1. Introduction
In recent decades, Computed Tomography (CT) has become one of the most vital diagnostic imaging techniques in the medical field [
1]. It provides fast, non-invasive, and highly detailed images, which are essential for screening, diagnosing, and monitoring various health conditions [
2,
3]. CT imaging is used extensively for both adults and paediatric patients due to its ability to assess multiple organs and structures, helping doctors make more informed decisions [
4]. Currently, the increased utilization of CT scans in both developed and developing countries poses great concerns about the radiation hazards associated with these CT examinations [
5]. Despite its tremendous clinical value, the reports have demonstrated that CT examinations can promote cancer risk due to associated ionizing radiation [
6,
7]. As the utility of the CT has been greatly increasing over the years, the sharp increase in the volume of CT imaging examinations was found to be the major source of radiation exposure in the medical field [
1]. A study by UNSCEAR on overall effective doses related to diagnostic medical exposures revealed that CT examinations represent 9.6% of total radiological investigations and contribute to 61.6% of total effective doses [
6]. While the benefits of CT scans are undeniable, concerns about patient radiation exposure, especially for children, have raised significant challenges in healthcare practices [
8]. Paediatric patients, being more sensitive to ionizing radiation, are at a higher risk of potential radiation-induced harm, necessitating the implementation of strategies that limit exposure while maintaining diagnostic effectiveness [
9].
The International Commission on Radiological Protection (ICRP) introduced the concept of Diagnostic Reference Levels (DRLs) as a tool to optimize radiation doses in medical imaging procedures [
10,
11,
12]. DRLs are used globally to ensure that the radiation doses administered to patients are neither excessively high nor low, serving as a benchmark for optimal radiation exposure [
13,
14]. In the last two decades, paediatric DRLs have been established in various countries for the most common CT examinations, including CT Head, CT Chest, CT Chest Abdomen Pelvis (CAP), and CT Abdomen Pelvis (AP) [
15,
16,
17,
18]. DRLs have been proven to be effective tools in monitoring radiation exposure and optimizing patient safety during diagnostic imaging [
19].
Several studies have focused on establishing and updating DRLs for paediatric CT imaging. In the UK, a review in 2011 updated national DRLs, showing a reduction in radiation doses over time, with a 17–47% decrease by 2019 due to advances in CT technology [
20]. In France and Ireland, studies revealed significant variations in radiation doses, highlighting the need for standardization [
21]. The American College of Radiology also updated DRLs in 2021 for the top 10 paediatric CT exams [
22,
23]. These studies show the importance of regularly updating DRLs to ensure patient safety and diagnostic effectiveness.
The recommended DRL quantities for CT imaging examinations are CT dose-index volume (CTDI
vol) and dose-length product (DLP). The CTDI
vol value represents the radiation dose resulting from a single rotation of the X-ray tube, while DLP indicates the total radiation exposure of the patient, and is highly affected by length of imaged area, called scan length or imaging range [
23,
24,
25,
26]. Additionally, regular review of local DRLs for CT imaging examinations is essential to maintain compliance with radiation safety policies, and ensure that DRLs are not systematically exceeded, thereby enhancing radiology practice [
25,
27]. The fast growth of CT technology, such as spectral CT and high-slice scanners, further reinforces the importance of establishing DRLs, considered as one of the hottest topics in current radiology practice, as an efficient and valuable tool for radiation dose optimization [
12,
26].
However, while DRLs have been widely established in many regions, specific attention to paediatric CT imaging remains limited. Children are more susceptible to radiation damage due to their growing tissues, smaller size, and longer expected lifespan. Therefore, it is imperative to develop and evaluate DRLs specifically for paediatric patients to ensure that their radiation exposure is minimized without compromising diagnostic quality [
11,
28]. Existing studies on DRLs for paediatric CT have often been generalized from adult populations or focused on specific diagnostic procedures.
Oman has made significant strides in improving healthcare services, ensuring the safe use of diagnostic imaging for children remains a priority. The Sultan Qaboos University Hospital (SQUH) and Royal Hospital (RH), two of the largest healthcare facilities in Oman, provide a wide range of imaging services, including paediatric CT scans. However, the absence of locally established DRLs for paediatric patients necessitates the development of these reference levels to improve the local radiation protection practice and ensure compliance with international safety standards.
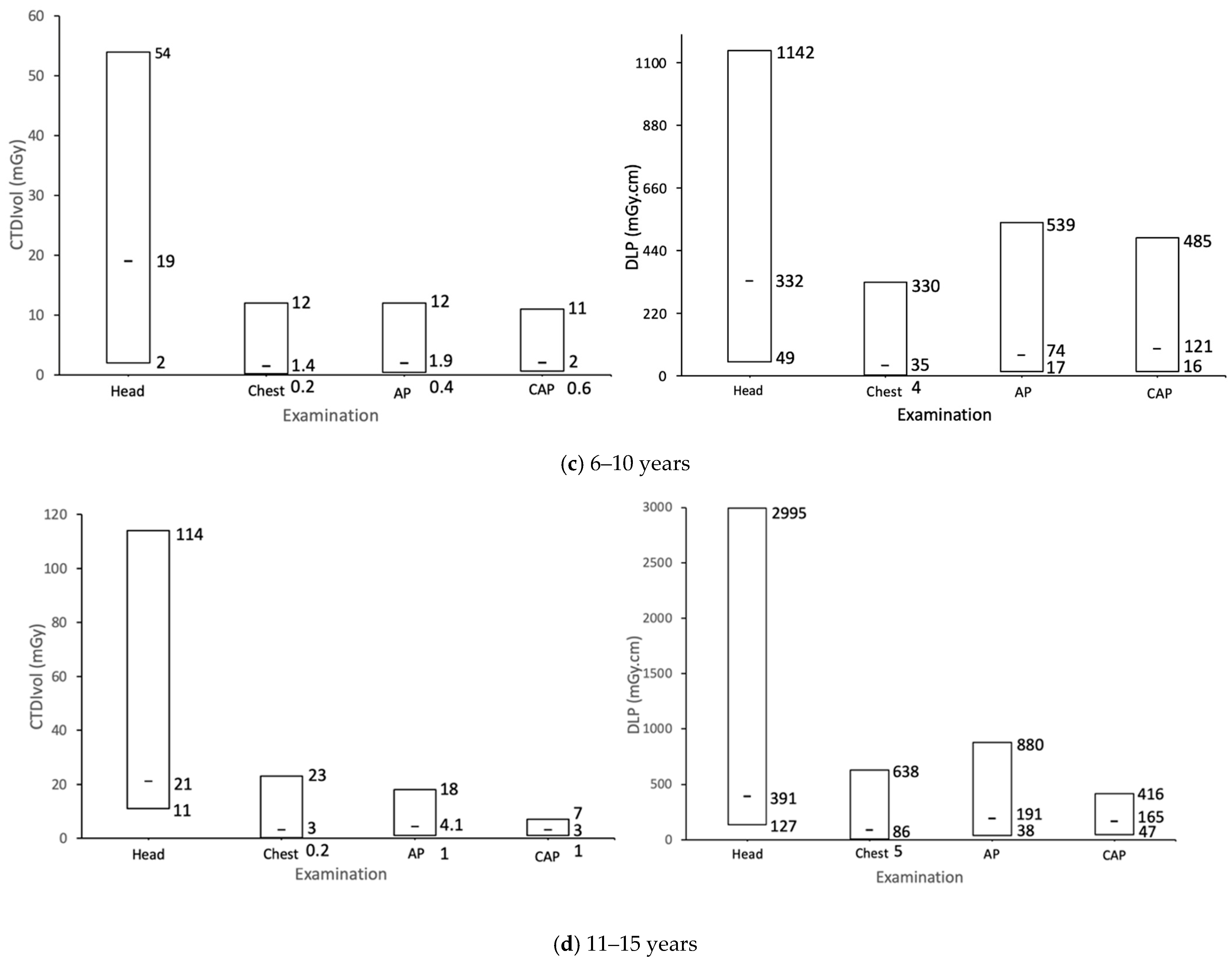
This study aimed to establish DRLs for paediatric CT imaging by evaluating the radiation doses from routine paediatric CT examinations. The main goal was to estimate DRL values for the four most common paediatric CT examinations, including CT Head, CT Chest, CT Abdomen Pelvis (AP), and CT Chest Abdomen Pelvis (CAP), as well as compare and discuss the derived DRLs with the most recently published DRLs in other countries.
2. Materials & Methods
2.1. Data Collection
In this retrospective study, dosimetric data were collected from CT paediatric patients’ scans available on the picture archiving and communication systems (PACS) at Sultan Qaboos University Hospital (SQUH; namely, Centre 1) and Royal Hospital (RH; namely, Centre 2). The radiation dose monitoring (RDM) and Al-Shifa hospital information system were used to extract the CT dosimetric data from Centre 1 and Centre 2, respectively. All patients’ scans were performed over the period from 2020 to 2024. Radiologists and medical physicists identified the four most common CT imaging examinations. These included CT Head, CT Chest, CT Abdomen Pelvis (AP), and CT Chest Abdomen Pelvis (CAP). Paediatric CT scans were all performed either on the Siemens SOMATOM Force 256 slice or Siemens SOMATOM Force 64 slice or Siemens SOMATOM Definition Flash (Siemens Healthineers, Erlangen, Germany). Dosimetric CT data were obtained from routine diagnostic scans performed on SOMATOM Force scanners at Centre 1, whereas Centre 2 operated both the Force 256 and the Definition Flash scanners. The use of CT dosimetric dose data acquired on different scanner models is an added value in terms of reliability and robustness in DRL studies and is expected to reflect local practice. All scanners were subject to strict quality assurance programs, including planned maintenance by the manufacturer, as well as daily, weekly, and annual quality control (QC) tests, along with post-repair QCs performed by local medical physicists. Additionally, despite both centres following quality control procedures, differences in the implemented scanning protocols such as scan length and automatic exposure control features may contribute to the variation in radiation dose across hospitals.
The total number of CT dosimetry records was collected from 5956 patient scans across both hospitals. The collected paediatric CT imaging was categorized into four paediatric age groups as recommended by ICRP 135 [
12]: <1 year, 1–5 years, 6–10 years, and 11–15 years. Additionally, patients were classified into four weight groups according to the recommendations of “Radiation Protection N
o 185: European Guidelines on Diagnostic Reference Levels for Paediatric Imaging” [
28]: <15 kg, 15–<30 kg, 30–50 kg, and >50 kg.
CT dosimetric data were collected from the dose reports generated by the CT acquisition and processing workstation at the completion of the patient study. To ensure the estimation of reliable and relevant DRLs, only diagnostic CT scans carried out using standard of care scanning protocols and approved by the quality management committee were considered in this study. This facilitates the comparison of the results with similar studies performed in other countries. A structured Excel form was developed and used by the researchers to collect data at both hospitals. CT dosimetry quantities (CTDIvol, DLP, exposure settings (kVp and mAs)) and patient demographics (age and weight) that were documented on the PACS or RIS radiology systems were collected from all patients’ scans.
2.2. Data Analysis
Microsoft Excel (Office 365), Minitab Statistical Software—Web App and OriginPro 2019 were used for data processing, statistical analysis, and charts generation presented in the ‘Results’ and ‘Discussion’ sections. Initially, Andreson–Darling normality tests were performed using Minitab to assess the distribution of continuous data. The normality tests identified that non-parametric tests were appropriate. Descriptive statistics, including minimum, median, maximum, interquartile ranges (IQRs), and 95% confidence intervals (CIs), for CTDIvol and DLP values across all CT imaging examinations were estimated. These median values were considered as local ‘typical values for DRLs’ and were subsequently compared to DRLs reported in recent studies. The Mann–Whitney U and Kruskal–Wallis tests were used to assess differences between the DRL values of the two centres and differences between age- and weight-based DRLs, respectively. These statistical indicators enhance transparency and allow a more robust comparison of dose distributions and paediatric scanning protocols between institutions. A significance level of 0.05 was applied for all statistical tests.