Abstract
Background/Objectives: The role of environmental modifications and design in mitigating behavioural symptoms is increasingly being recognised as a way to address the psychosocial needs of individuals with dementia. This study aims to investigate various nature-based interventions for reducing agitation in people with dementia in long-term residential care environments. Methods: Database searches were conducted on MEDLINE, PsycINFO, Scopus, and Web of Science. A literature search was conducted with the following inclusion criteria: (i) peer-reviewed journal publication written in English; (ii) random controlled trials (RCTs) and quasi-experimental design with results for pre- and post-testing reported; (iii) interventions using natural elements, where the effectiveness of the reduction in agitation was measured using a validated instrument; and (iv) participants aged 65 and older with dementia residing in long-term care facilities. Results: This meta-analysis included 29 studies with 733 participants. The results showed that such interventions had a significant negative mean effect on lowering agitation in this population. Additionally, intervention settings (indoor vs. outdoor) and the presence of social interaction were significant predictors of the effect size for agitation reduction. At the same time, no significant differences in effect size were observed between the types of experiences with nature (indirect vs. direct) or the duration of the interventions. Conclusions: This study demonstrates that, when thoughtfully applied, nature-based interventions can significantly alleviate agitation in patients with dementia residing in long-term residential care facilities. This review lays the groundwork for future research aimed at developing design guidelines and planning strategies to integrate natural elements into dementia-friendly environments effectively.
1. Introduction
As a person’s dementia progresses, they may experience agitation, psychosis, anxiety, depression, and apathy [1]. The behavioural symptoms of dementia may also include patients’ inappropriate physical and verbal actions towards family members and caregivers. Due to the challenging and disruptive behaviours that characterise dementia, nearly every person with dementia is eventually placed in a nursing home at some point during the illness [2]. However, behavioural symptoms are often exacerbated or triggered by a mismatch between individuals’ needs or excessive stressors and the environment [3]. Therefore, modifying the environment to accommodate the needs of dementia patients could be an important strategy to mitigate agitation and other behavioural symptoms.
To date, a number of studies have examined and reviewed the relationship between people with dementia and their environments. For example, a systematic review by Marquardt et al. [4] categorised 169 studies into four main areas: basic design decisions, environmental attributes, ambience, and environmental information, and illustrated how these design interventions impact the behaviours, functions, well-being, social engagement, and orientations of people with dementia. Chaudhury et al. [5] also reviewed 103 studies and identified the influence of several factors, including environmental characteristics of social spaces, unit size, spatial layout, homelike character, and sensory stimulation, on residents’ behaviours and well-being in care facilities. Furthermore, Barrett et al. [6] provided a synthesis of diverse evidence leading to the formulation of three design principles (manageable cognitive load, clear sequencing, and an appropriate level of stimulation), backed up by more in-depth design parameters. The findings from the reviews indicated that the environment could have a therapeutic effect on people with dementia, helping them improve and preserve their well-being, behaviour, functionality, and independence. In particular, the reviews have shown that sensory stimulation approaches, which are abundant in nature, can serve as effective interventions. Although individuals with dementia respond differently to natural stimuli, studies have shown certain benefits, including reduced agitation and depression, improved mood, positive interactions with staff, and enhanced well-being [7,8,9]. Therefore, designing interventions and environments that provide opportunities for people with dementia to interact with nature could be crucial in promoting their health, well-being, and quality of life.
The design discourse has increasingly recognised and promoted those physical living environments with natural elements as essentially therapeutic. For example, Wilson [10] introduced the term ‘biophilia’, which describes the inherent connection humans have with nature. When individuals encounter nonthreatening natural stimuli, their emotional state improves, resulting in positive changes in physiological activity, enhanced attention and memory, and reduced negative emotions [11,12,13]. For individuals with dementia, nature offers a stimulating environment with sensory experiences and opportunities for engaging in social activities, which in turn have a positive impact on their health and well-being. A qualitative review by Orr et al. [14] examined how older people with dementia described their sensory experiences and connectedness with the natural world. The authors reported that older adults found significant pleasure and enjoyment from observing and interacting with nature and that these activities appeared to have therapeutic effects on their mood and quality of life. Similarly, Bennett et al. [15] found that continued engagement with outdoor activities improved associated support for self and identity among people with dementia. In their review of 16 studies on sensory gardens and horticultural activities with participants with dementia living in care homes, Gonzalez and Kirkevold [16] reported that nature-based activities reduced agitation and restlessness, increased social engagement, and improved the sleep and well-being of people with dementia. Murroni et al. [17] also reviewed 16 quantitative studies on the benefits that garden visits and gardening therapy have on people with dementia. The review revealed that the most significant effects were engagement, agitation, stress, positive emotions, and improved medication use. Motealleh’s narrative review [18] of the effectiveness of outdoor natural landscapes focused on the behavioural and psychological symptoms of dementia, including agitation, apathy, and engagement. Furthermore, some studies have focused on specific natural elements within designs, such as images of nature, light, sound, and smell—also known as ‘biophilic design’. As an application of the concept of ‘biophilia’, biophilic design offers a sustainable design strategy that fosters connections between humans and nature in built environments [19]. This design concept involves direct experiences of nature, such as natural light, air, plants, animals, and water; indirect experiences of nature, including images of nature, natural materials, and naturalistic shapes and forms; and the simulation of light and smell, all of which evoke and mimic natural elements. A review of Goudriaan et al. [20] examined the influence of daylight and indoor lighting on older adults with dementia in care facilities. Although they found no conclusive evidence to suggest that indoor light reduces challenging behaviours, positive effects were observed in improving depressive symptoms and quality of life. Another review by D’Andrea et al. [21] synthesised the evidence regarding the efficacy of interventions involving olfactory stimulation (e.g., lavender or orange) for individuals with dementia. They demonstrated that exposure to scents can trigger memories of personal past experiences and autobiographical memory, thereby evoking positive emotions. More recently, Huang and Yuan [22] examined 11 studies on the health benefits aromatic scents have on older people with dementia. They indicated that herbs and aromatic plants had comprehensive health benefits, such as reduced agitated behaviour and enhanced cognitive functions and overall well-being.
Nevertheless, a key finding of the abovementioned reviews is the limited empirical evidence identifying the beneficial effects of nature-based applications on people with dementia. To date, insufficient attention has been given to the application of design and its role in enhancing long-term residential care environments. Furthermore, there is still a lack of systematic understanding of how nature-based interventions affect specific symptoms in long-term residents with dementia in their care settings. To address this research gap, this paper builds on earlier reviews and analyses and examines experimental studies that assess the impact of nature-based interventions on agitation in people with dementia. The focus is on studies involving interventions that aim to enhance sensory experiences and reduce agitation by utilising natural elements in long-term residential care environments. For this review, agitation is defined as ‘a response to either internal or external stimuli or both, described by behavioural or verbal disruptiveness, inappropriateness, aggressiveness and repetitiveness’ [23]. To systematically explore the relative impact of nature-based interventions on reducing residents’ agitation, the effects of the intervention settings (indoor vs. outdoor), the presence of social interaction, the types of experiences with nature (indirect vs. direct), and the duration of the interventions are examined. This review and meta-analysis focus on studies conducted in long-term residential care settings, aiming to serve as a valuable resource for those seeking to advance knowledge in this field and to identify effective dementia care practices across various contexts. Based on the conclusions drawn from existing studies, a research and practice agenda is proposed.
2. Materials and Methods
2.1. Inclusion Criteria
A literature search was conducted with the following inclusion criteria: (i) peer-reviewed journal publications written in English; (ii) random controlled trials (RCTs) and quasi-experimental design with results for pre- and post-testing reported; (iii) interventions using natural elements, where the effectiveness of the reduction in agitation was measured using a validated instrument, including the Cohen–Mansfield Agitation Inventory (CMAI), Agitated Behaviour Scale (ABS), and Neuropsychiatric Inventory (NPI); and (iv) participants aged 65 and older with dementia residing in long-term care facilities. Furthermore, following Kellert and Calabrese’s key principles of biophilic design, only the studies that examined interventions involving ‘repeated and sustained engagement with nature’ [19] were considered.
2.2. Search Strategy
This meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMAs) guidelines. Database searches were conducted on MEDLINE, PsycINFO, Scopus, and Web of Science. The final search was completed in July 2024. Four sets of filters were applied to the database search, all of which were set to search for terms in the titles or abstracts. The first filter was used to identify studies about natural elements: Title (natur* OR garden* OR green* OR farm* OR plant* OR biophilic OR sound OR light OR scent OR olfactory). The second filter was applied to identify studies on the dementia population: Abstract (dementia), whilst the third filter was used to identify studies on built environments: Abstract (design OR environment* OR setting). Additional papers were identified through manual searches of review papers and Google searches.
2.3. Data Collection Process and Data Items
The data comprised (i) the basic study information (author, year of publication, and country), (ii) study design, (iii) the sample information (number and mean age), (iv) intervention details (intervention content and duration), and (v) outcome measurement.
2.4. Quality Assessment of Eligible Studies
Two independent reviewers assessed all the studies meeting the inclusion criteria for external and internal validity using the JBI standardised appraisal tools for RCTs and quasi-experimental studies (see Appendix A). The questions in the appraisal tool were rated ‘Yes’, ‘No’, ‘Unclear’, or ‘Not applicable’. The overall methodological quality of each study was then calculated by adding all ‘Yes’ ratings and dividing them by the number of applicable questions to obtain a percentage [24]. The studies were rated ‘low methodological quality’, ‘adequate’, ‘moderate’ and ‘strong’ if they received a rating of less than 50%, between 50% and 69%, between 70% and 85%, and between 86% and 100%, respectively. Given that studies of ‘low methodological quality’ may compromise the quality of systematic review practice recommendations, all studies with such a rating were excluded.
2.5. Data Synthesis and Analysis
The software package Meta Essentials (www.erim.eur.nl/research-support (accessed on 5 April 2025) was used to analyse the data. Meta Essentials is a useful tool that automatically calculates effect sizes from different types of data and supports various meta-analysis tasks, such as subgroup analysis, moderator analysis, and checking for publication bias [25]. All outcomes included in the analyses were continuous. The extracted data included pre—post mean values and Cohen’s d and Hedges’ g effect sizes, as well as mean change scores, including the standard deviation (SD) and/or confidence interval (CI) values. A key eligibility criterion for inclusion was that studies must include a specific measure of agitation, which could be any of the validated measures with the available constituent subscales. Where missing data were found, the corresponding authors were contacted to request further information. In cases where the correlation coefficient (r) was not provided or available, data from other sources were used to estimate this correlation and a sensitivity analysis was conducted to determine how this affected the results.
Due to the variation in the samples analysed, the random effects model was chosen as the most appropriate analytical approach. Uncertainty about the findings was expressed in the form of a 95% CI. This was followed by the evaluation of effect sizes [26], with 0.2, 0.5, and 0.8 representing small, medium, and large effects, respectively. Heterogeneity amongst effect sizes was determined by a significant Q value (p < 0.10). The I2 statistic is indicative of the degree of variability in effect sizes, with the ranges of 1–49, 50–74, and 75–100 signifying low, moderate, and high heterogeneity, respectively.
Moreover, in instances of high heterogeneity, three subgroup analyses were performed to assess whether (i) the intervention settings (indoor vs. outdoor), (ii) the presence of social interaction, (iii) the types of experiences with nature (indirect vs. direct), and (iv) the duration of interventions contributed to the variability in the effects. Finally, publication bias was examined using funnel plots and associated statistics. Assessing the impact of publication bias involved estimating the effect if the bias were absent using trim-and-fill analysis [27]. This method eliminated the most extreme effect sizes from the funnel plot and subsequently recalculated the effect size to enhance the symmetry of the funnel plots around the newly suggested effect size.
2.6. Sensitivity Analysis
Sensitivity analyses were applied to examine the robustness of the synthesised results. Following the guidance provided by Higgins and Green [28], in cases where there was an estimated substantial or considerable risk of heterogeneity, further subgroup and/or sensitivity analysis was conducted and reported alongside the main analysis to provide more detailed insights. Subgroup analysis involved stratifying the findings by the intensity of the intervention and, where appropriate, reporting results only for the studies that were assessed as having high or moderate methodological quality. Furthermore, in instances where forest plots indicated clear outliers within the sample, the removal of these items from the main model was considered, after which the resulting change in the overall main effect and I2 values was reported.
3. Results
3.1. Study Selection
Our database search protocol identified 1193 citations. After removing 594 duplicated items, our initial pool consisted of 599 publications. Of these, 507 articles were excluded because they did not meet the inclusion criteria. The list was further refined to 92 entries by discarding those that were irrelevant. A total of 35 articles were excluded as they did not contain the statistical information needed for our analyses—it was not available in the published document and could not be obtained from the authors. A total of 57 studies underwent a full-text analysis. Studies that lacked essential statistical information (e.g., means, standard deviations, or sample sizes), presented data in incompatible formats, or were identified as having significant methodological flaws were excluded. This resulted in 31 articles in the final publication pool. Figure 1 presents the PRISMA flowchart.

Figure 1.
PRISMA flowchart of study selection.
3.2. Study Characteristics
The initial analysis included 31 studies (11 RCTs and 20 quasi-experimental studies) with 826 participants. Nine papers were published before 2009, 13 between 2010 and 2019, and 9 between 2020 and 2023. In terms of study design, 11 studies used a randomised controlled design, and 20 studies used a quasi-experimental design. This increased rate of publication illustrates the establishment and acceptance of nature as a supportive design intervention for older people with dementia residing in long-term residential care environments. The studies were conducted in such care environments in the following different countries: 11 studies were carried out in North America, 8 studies in Asia, 7 studies in Europe, and 5 studies in Australia. The mean age of participants ranged from 71.14 to 86.90 years. In terms of interventions, 7 studies used naturalistic lighting for circadian stimulus, 10 studies used olfactory stimulation, 4 studies used the sound of nature, and 10 studies used indoor and outdoor gardens. In terms of outcome measures, the most widely used scale to measure the participants’ agitation was the CMAI (n = 23), followed by the NPI (n = 7) and the ABS (n = 1). There was a wide range in the duration over which the intervention was delivered, ranging between just 3 days and several months. Only four studies included follow-up measures at 3 weeks [18], 4 weeks [29,30], and 6 weeks [31] upon completion of the study. The detailed characteristics of each study are summarised in Table 1.

Table 1.
Characteristics of the studies included in the meta-analysis.
3.3. Immediate Effects of Interventions
The total sample size for interventions assessing nature connectedness pre- and post-intervention was 826 (range 5–82) from 31 studies. A large negative mean effect was observed (g = −1.04 [95% CI −1.43, −0.65]), which was significant (p < 0.001). The heterogeneity of effects was also significant (Q = 324.56, p < 0.001) and had high inconsistency (I2 = 90.76%).
Through the sensitivity analysis, inadequate studies were systematically removed to improve statistical consistency, resulting in 29 remaining studies. Two studies were identified as outliers due to effect sizes being substantially different from the others. Accordingly, the total sample size for interventions assessing agitation pre- and post-intervention was 733 (range 5–82) from 29 studies. A large negative mean effect was observed (g = −0.86 [95% CI −1.15, −0.57]), which was significant (p < 0.001). The heterogeneity of effects was also significant (Q = 215.61, p < 0.001) and had a moderate inconsistency (I2 = 87.01%). Subgroup analyses were then conducted on 29 studies.
3.4. Subgroup Analyses
Subgroup analyses were carried out to investigate the factors affecting the effectiveness of natural contact and engagement on the following nature connection dimensions: (i) intervention settings (indoor vs. outdoor), (ii) the presence of social interaction, (iii) the types of experiences with nature (indirect vs. direct), and (iv) the duration of interventions.
3.4.1. Intervention Settings
Twenty studies were coded as indoor interventions and eleven as outdoor interventions. In this review, only outdoor interventions within care facilities (e.g., outdoor gardens directly accessible from living areas) were included to minimise selection bias. The test for subgroup differences suggested that there was a statistically significant subgroup effect (p = 0.040), indicating that the intervention settings statistically significantly affected the effectiveness of the interventions. For indoor settings, a large effect was observed (g = −1.00 [95% CI −1.38, −0.62], I2 = 90.34%), whilst a medium effect was found for outdoor settings (g = −0.76 [95% CI −1.19, −0.33], I2 = 49.38%), as shown in Figure 2.
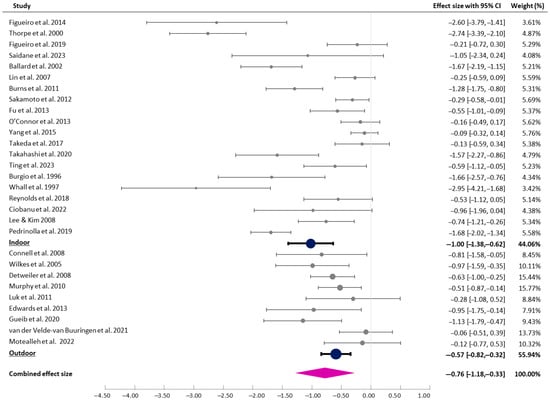
Figure 2.
Forest plot of pre–post effects and CIs (indoor vs. outdoor interventions) [7,8,9,29,30,31,32,33,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56].
3.4.2. The Presence of Social Interaction
For the subgroup analysis, studies were categorised based on whether the interventions applied involved social interaction. The majority of the studies (n = 23) were individual interventions, whilst only 6 involved social interaction. The studies coded as ‘social interaction’ involved various interventions and activities to encourage social contact with caregivers, friends, or family members in natural environments. Those studies that required minimal contact to set up the intervention, such as applying oil to the skin or accompanying someone from the bedroom to the garden, were coded as ‘individual interventions’. The test for subgroup differences indicated a statistically significant subgroup effect (p = 0.028), indicating that the presence of social interaction statistically significantly modified the effect of the interventions. For the individual interventions, a medium effect (g = −0.73 [95% CI −1.02, −0.44], I2 = 85.44%) was found, whilst the interventions involving social interaction provided more significant outcomes (g = −0.99 [95% CI −1.59, −0.78], I2 = 68.62%), as shown in Figure 3.

Figure 3.
Forest plot of pre–post effects and CIs (individual vs. social interaction) [7,8,9,29,30,31,32,33,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56].
3.4.3. Types of Experiences with Nature
Following Richardson and Butler [57], indirect experiences of nature were identified in 18 studies, which involved contact with images of nature and natural materials (e.g., recorded sounds and smells) that evoked and mimicked nature. Furthermore, 11 studies were coded as ‘direct experiences of nature’, where participants engaged with natural environmental features, including air, natural light, vegetation, water bodies, landscapes, and ecosystems. The test for subgroup differences suggested that there was no statistically significant subgroup effect (p = 0.300), indicating that the types of experiences with nature did not modify the effect of the interventions (Figure 4).
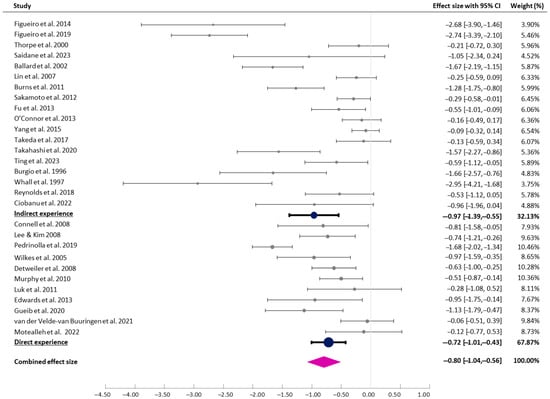
Figure 4.
Forest plot of pre–post effects and CIs (indirect vs. direct experiences) [7,8,9,29,30,31,32,33,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56].
3.4.4. Duration of Interventions
Studies were categorised based on the duration of the intervention. The studies examined the impact of the intervention on participants’ agitation levels over periods ranging from 3 days to 12 months. The durations of 17 studies were less than 1 month, those of 7 studies were between 1 and 6 months, and those of 5 studies lasted more than 6 months. The test for subgroup differences suggested that there was no statistically significant subgroup effect (p = 0.970), indicating that the duration of intervention did not modify the effect of the interventions (Figure 5).

Figure 5.
Forest plot of pre–post effects and CIs (duration of intervention) [7,8,9,29,30,31,32,33,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56].
4. Discussion
This meta-analysis included 29 studies with 733 participants to investigate the application of various nature-based strategies for reducing agitation in people with dementia housed in long-term residential care environments. Overall, it was found that such interventions had a significant effect on reducing agitation in people with dementia. Furthermore, intervention settings (indoor vs. outdoor) and the presence of social interaction were significant predictors of the effect size for agitation reduction. No effect size differences were observed between the types of experiences with nature (indirect vs. direct) or the duration of interventions. However, only a few studies measured sustained changes. With only 4 out of 29 studies available, it is not possible to draw firm conclusions about the longevity of the effect on agitation.
4.1. The Effect of Intervention Settings
The results suggested that indoor interventions were more effective than outdoor interventions in reducing agitation in long-term residential care environments. Most interventions involving circadian or olfactory stimulation were conducted inside care homes, such as the participants’ bedrooms or in common areas (e.g., dining room). While Figueiro et al. [29] installed luminaires in a subject’s room for the lighting intervention, Saidane et al. [36] and Figueiro et al. [34] placed the floor lamps in both the participants’ bedrooms and common areas for those who spent most of the day outside their bedrooms. No differences in effects were observed between different indoor locations.
In recent years, there has been an increasing interest in incorporating outdoor gardens or patios in nursing facilities. Whilst previous studies have shown the benefits of multisensory experiences [14,16], there is less agreement regarding the value of the provision of outdoor spaces. A review by Fleming and Purandare [58] revealed that people with dementia have difficulty dealing with high levels of stimulation. They also tend to have a reduced ability to screen out unwanted stimuli and can easily become more confused, anxious, and agitated when overstimulated. Thus, for these individuals, there is a need to control sensory stimulation to avoid the reverse effect [4].
Moreover, Barrett et al. [6] proposed a model showing the links between design principles and the negative symptoms of dementia. The model indicated that moderate levels of stimulation would contribute to reduced apathy and agitation, whilst excessive stimulation was likely to lead to agitation and aggression. Thus, the authors suggested that environmental design should seek to find a balance where the individual remains engaged without being overwhelmed, making them stimulated, but not disturbed. Additionally, several studies have indicated barriers to the use of outdoor spaces. A lack of safety features (e.g., no handrails or poor surface materials), insufficient resting spaces, limited access to bathroom facilities and drinking fountains, and weather-related issues in outdoor environments could also diminish the benefits of natural experiences [3]. Thus, careful optimisation of stimulation levels and the provision of proper facilities are crucial to enhancing the positive effects of outdoor natural environments for people with dementia residing in long-term residential care.
4.2. The Effect of Social Interaction
It was found that nature-based interventions involving social interaction were more effective at reducing agitation than those that did not. In this study, the research identified as ‘social interaction’ involved the interventions designed to promote social contact with caregivers, friends, or family members in natural environments. For example, Edwards et al. [56] studied the impact of outdoor gardens as social spaces for a wide range of activities where individuals can meet friends and family members. Connell et al. [37] investigated the effects of 1 h recreational activities performed in small groups of 4–6 people to help them receive bright light exposure. The study of Whall et al. [48] also involved interactions between residents and staff during showers with natural simulations.
Whilst these studies demonstrated that social interaction might be a useful tool for enhancing the impact of nature-based applications in people with dementia, much uncertainty still exists regarding the impact of interactions with people on agitation in people with dementia. For instance, Burgio et al. [47] showed that staff touch and verbal interaction elicit agitation in some subjects but reduce it for others. Kolanowski and Litaker [59] observed that individuals who were more extraverted demonstrated significantly less agitation, whilst more introverted individuals showed greater agitation during high levels of social interaction. Thus, responses to social interactions seem to vary on an individual basis. Therefore, monitoring social interaction is crucial, as insufficient interaction can result in functional decline, whilst intensive human interaction may cause increased agitation. In this regard, further research is needed to identify the most effective methods for facilitating social interactions among residents without causing agitation.
This meta-analysis also tested the relative effects of the types of experiences with nature (indirect vs. direct) and the duration of interventions. For subgroup analysis, some studies identified indirect experiences of nature through contact with images and materials that evoked and mimicked nature. For example, Lin et al. [39] placed aroma diffusers near the participant’s bedside during nighttime sleep. In contrast, other studies were identified as ‘direct experiences of nature’, in which participants actively engaged with natural environmental features. Connell et al. [37] conducted the recreational program with small groups of 4–6 people in outdoor spaces to expose participants to natural light. However, the test for subgroup differences did not show a statistically significant subgroup effect. Moreover, the subgroup analysis of the duration of interventions also found no significant difference between subgroups (i.e., 1 month vs. 1–6 months vs. more than 6 months). Although some studies [33,37,39] were carried out over less than 1 month, the effects were large. In this review, coding experiences with nature are particularly challenging, as publications are often unable to capture the full scope of activities in which participants engage. Given that the focus was on the reported study methodology rather than on the participants’ actual experiences, this categorisation should be approached with caution.
4.3. Limitations of This Study
This study has potential limitations. The effect estimates in this analysis are based on the existing interventional studies. Differences in study designs, participant characteristics, and intervention types could affect the consistency of the results. Moreover, the scope of subgroup analyses was limited due to insufficient data or incomplete reporting, which restricted the ability to explore factors influencing the intervention’s effectiveness. Notwithstanding these limitations, this study provides some insights into the importance of considering nature-based interventions as an acceptable therapeutic intervention for agitation, particularly in efforts to enhance their environmental and social settings to cater to the needs of people with dementia.
4.4. Recommendations for Future Research and Practice
It is now widely recognised that providing environmental support can mitigate behavioural symptoms and improve the quality of life of persons with dementia by addressing their psychosocial needs. Several studies have shown the benefits of natural stimuli, but these have also indicated that individuals with dementia respond differently based on their cognitive load capacities and degrees of stimulation [6]. Getting to know the individual is crucial for identifying the underlying factors that trigger certain behaviours so that the potential for them to occur can be eliminated or minimised [60]. Therefore, further research is necessary to fully comprehend individual differences in the impact of biophilic design applications in care facilities. It involves understanding the environmental preferences, experiences, and activities that people with dementia respond to, which in turn promotes these aspects of health and helps them achieve a good quality of life.
Moreover, there has been little agreement on which optimum level of stimulation can reduce agitation in people with dementia. This review showed different outcomes in environmental stimulation (indoor vs. outdoor) and social interaction. In particular, relatively greater environmental stimulation had a negative effect on the benefits of nature-based applications, whilst human interaction had a positive effect on their benefits. These findings reveal the difficulty in distinguishing the contribution of the physical environment from that of social contact and engagement. Thus, further investigations and experimentation into the optimum level of stimulation for reducing agitation in people with dementia are strongly recommended.
More broadly, research is also needed to explore the combination of proper environmental stimulation with other care practice manipulations. Some studies that combine reduced stimulation with other manipulations have been shown to lessen behavioural disturbances [61]. For example, interventions in nursing homes aimed at reducing night-time noise have not succeeded in improving sleep duration, whereas a combination of increased daytime physical activity and decreased night-time noise levels can help alleviate agitation in nursing home residents [62,63]. A further study could assess the impact of combining nonpharmacological interventions with natural elements on agitation or other behavioural symptoms in older people with dementia. Clinicians and caregivers might also need some targeted education and training on the impact of nature-based interventions, which can be tailored to suit the care planning and management needs of behavioural symptoms in dementia. Finally, healthcare professionals working in facilities providing dementia care services could use nature-based interventions when undertaking environmental modifications to reduce risks related to falls and other health outcomes.
5. Conclusions
This study is among the first to conduct a meta-analysis of nature-based interventions as a strategy to reduce agitation in older people with dementia in institutional settings. This review shows the importance of considering nature-based applications as an acceptable therapeutic intervention for agitation in efforts to modify environments and enhance their environmental features to cater to the needs of people with dementia. More importantly, this work highlights that, when thoughtfully applied, natural elements can significantly alleviate agitation in dementia patients living in long-term residential care facilities. The intervention setting and the presence of social interaction were significant factors influencing the effectiveness of the intervention in reducing agitation. This review lays the groundwork for future research aimed at developing design guidelines and planning strategies to integrate natural elements into dementia-friendly environments.
Author Contributions
Conceptualisation, E.Y.C. and J.Y.L.; methodology and validation, E.Y.C. and J.Y.L.; formal analysis, E.Y.C.; data curation, J.Y.L.; writing—original draft preparation, E.Y.C. and J.Y.L.; writing—review and editing, J.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Hong Kong Polytechnic University, P0046676.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analysed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A. Quality Assessment of Methodological Quality

Table A1.
Quality assessment of methodological quality using JBIs’ checklist of randomised controlled trials.
Table A1.
Quality assessment of methodological quality using JBIs’ checklist of randomised controlled trials.
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Total (%) | Methodological Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Figueiro et al., 2019 [32] | Y | U | Y | Y | N/A | N/A | U | Y | Y | Y | Y | Y | Y | 69 | Adequate |
| Ballard et al., 2002 [38] | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 92 | Strong |
| Lin et al., 2007 [39] | Y | U | Y | Y | U | Y | U | Y | Y | Y | Y | Y | Y | 77 | Moderate |
| Burns et al., 2011 [40] | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | 85 | Moderate |
| Sakamoto et al., 2012 [41] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | Strong |
| Fu et al., 2013 [31] | Y | U | U | Y | U | Y | U | Y | Y | Y | N | Y | Y | 62 | Adequate |
| O’Connor et al., 2013 [42] | Y | Y | Y | Y | N | Y | N | Y | Y | Y | N | Y | Y | 77 | Moderate |
| Yang et al., 2015 [43] | Y | Y | N | Y | U | Y | U | Y | Y | Y | Y | Y | Y | 77 | Moderate |
| Takahashi et al., 2020 [45] | U | U | Y | Y | N/A | Y | U | Y | Y | Y | Y | Y | U | 62 | Adequate |
| Pedrinolla et al., 2019 [51] | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 92 | Strong |
| Luk et al., 2011 [55] | U | U | Y | Y | U | U | N | Y | Y | Y | Y | Y | Y | 62 | Adequate |
N, no; N/A, not applicable; U, unclear; Y, yes; 0–49%: low methodological quality; 50–69%: adequate methodological quality; 70–85: moderate methodological quality; 86–100%: strong methodological quality. Q1. Was true randomisation used for the assignment of participants to the treatment groups? Q2. Was the allocation to the treatment groups concealed? Q3. Were the treatment groups similar at baseline? Q4. Were the participants blind to the treatment assignment? Q5. Were those delivering the treatment blind to the treatment assignment? Q6. Were the treatment groups treated identically, other than the intervention of interest? Q7. Were the outcomes assessors blind to the treatment assignment? Q8. Were the outcomes measured in the same way for the treatment groups? Q9. Were the outcomes measured in a reliable way? Q10. Was the follow-up complete and, if not, were differences between the groups in terms of their follow-up adequately described and analysed? Q11. Were the participants analysed in the groups to which they were randomised? Q12. Was the appropriate statistical analysis used? Q13. Was the trial design appropriate, and were any deviations from the standard RCT design (individual randomisation and parallel groups) accounted for in the conduct and analysis of the trial?

Table A2.
Quality assessment of methodological quality using JBIs’ checklist of quasi-experimental studies.
Table A2.
Quality assessment of methodological quality using JBIs’ checklist of quasi-experimental studies.
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Total (%) | Methodological Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Figueiro et al., 2014 [29] | Y | N | Y | Y | Y | Y | Y | Y | Y | 89 | Strong |
| Saidane et al., 2023 [36] | Y | N | Y | N | Y | Y | Y | Y | Y | 78 | Moderate |
| Thorpe et al., 2000 [33] | Y | N | Y | Y | Y | Y | Y | Y | Y | 89 | Strong |
| Figueiro et al., 2020 [34] | Y | N | Y | Y | Y | Y | Y | Y | Y | 89 | Strong |
| Figueiro and Kales 2021 [35] | Y | Y | Y | N | Y | Y | U | Y | Y | 78 | Moderate |
| Connell et al., 2007 [37] | Y | Y | Y | Y | Y | Y | U | Y | Y | 89 | Strong |
| Takeda et al., 2017 [44] | Y | N | Y | Y | Y | Y | Y | Y | Y | 89 | Strong |
| Ting et al., 2023 [46] | Y | Y | Y | Y | Y | Y | U | Y | Y | 89 | Strong |
| Burgio et al., 1996 [47] | Y | N | Y | Y | Y | Y | Y | Y | Y | 89 | Strong |
| Whall et al., 1997 [48] | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100 | Strong |
| Reynolds et al., 2018 [49] | Y | N | Y | U | Y | Y | Y | Y | Y | 78 | Moderate |
| Ciobanu et al., 2022 [30] | Y | N | Y | U | Y | Y | U | Y | Y | 67 | Adequate |
| Lee & Kim 2008 [50] | Y | N | Y | U | Y | Y | Y | Y | Y | 78 | Moderate |
| Wilkes et al., 2005 [52] | Y | N | Y | N | Y | Y | U | Y | Y | 67 | Adequate |
| Detweiler et al., 2008 [53] | Y | N | Y | Y | Y | Y | Y | Y | Y | 89 | Moderate |
| Murphy et al., 2010 [54] | Y | N | Y | U | Y | Y | U | Y | Y | 67 | Adequate |
| Edwards et al., 2012 [56] | Y | N | Y | N | Y | Y | Y | Y | Y | 78 | Moderate |
| Gueib et al., 2020 [7] | Y | Y | Y | Y | Y | Y | U | Y | Y | 89 | Strong |
| van der Velde-van Buuringen et al., 2021 [8] | Y | N | Y | Y | Y | Y | Y | Y | Y | 89 | Moderate |
| Motealleh et al., 2022 [9] | Y | N | Y | Y | Y | Y | U | Y | Y | 78 | Moderate |
N, no; U, unclear; Y, yes; 0–49%: low methodological quality; 50–69%: adequate methodological quality; 70–85: moderate methodological quality; 86–100%: strong methodological quality. Q1 = Is it clear in the study what the ‘cause’ is and what the ‘effect’ (i.e., there is no confusion about which variable comes first) is? Q2 = Was there a control group? Q3 = Were the participants included in any similar comparisons? Q4 = Were the participants included receiving any comparable or similar treatment/care, other than the exposure or the intervention of interest? Q5 = Were there multiple measurements of the outcome, both pre and post the intervention/exposure? Q6 = Were the outcomes of the participants included in any comparisons measured in the same way? Q7 = Were the outcomes measured in a reliable way? Q8 = Was the follow-up complete, and if not, were differences between the groups in terms of their follow-up adequately described and analysed? Q9 = Was appropriate statistical analysis used? A simplified version of this technique could also involve the use of simple cutoff scores (e.g., studies with 7 or more yes responses are included). Available online: https://journals.lww.com/jbisrir/fulltext/2024/03000/the_revised_jbi_critical_appraisal_tool_for_the.4.aspx#T1 (accessed on 5 April 2025).
References
- Cerejeira, J.; Lagarto, L.; Mukaetova-Ladinska, E.B. Behavioral and psychological symptoms of dementia. Front. Neurol. 2012, 3, 73. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, H.; Abey-Nesbit, R.; Nishtala, P.S.; Allore, H.; Han, L.; Deely, J.M.; Pickering, J.W. Predictors of residential care admission in community-dwelling older people with dementia. J. Am. Med. Dir. Assoc. 2020, 21, 1665–1670. [Google Scholar] [CrossRef] [PubMed]
- Bossen, A. The importance of getting back to nature for people with dementia. J. Gerontol. Nurs. 2010, 36, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Marquardt, G.; Bueter, K.; Motzek, T. Impact of the design of the built environment on people with dementia: An evidence-based review. Health Environ. Res. Des. J. 2014, 8, 127–157. [Google Scholar] [CrossRef] [PubMed]
- Chaudhury, H.; Cooke, H.A.; Cowie, H.; Razaghi, L. The Influence of the Physical Environment on Residents with Dementia in Long-Term Care Settings: A Review of the Empirical Literature. Gerontologist 2018, 58, e325–e337. [Google Scholar] [CrossRef] [PubMed]
- Barrett, P.; Sharma, M.; Zeisel, J. Optimal spaces for those living with dementia: Principles and evidence. Build. Res. Inf. 2019, 47, 734–746. [Google Scholar] [CrossRef]
- Gueib, C.; Pop, A.; Bannay, A.; Nassau, E.; Fescharek, R.; Gil, R.; Luc, A.; Rivasseau Jonveaux, T. Impact of a healing garden on self-consciousness in patients with advanced Alzheimer’s disease: An exploratory study. J. Alzheimer’s Dis. 2020, 75, 1283–1300. [Google Scholar] [CrossRef] [PubMed]
- van der Velde-van Buuringen, M.; Achterberg, W.P.; Caljouw, M.A.A. Daily garden use and quality of life in persons with advanced dementia living in a nursing home: A feasibility study. Nurs. Open 2021, 8, 1243–1253. [Google Scholar] [CrossRef] [PubMed]
- Motealleh, P.; Moyle, W.; Jones, C.; Dupre, K. The Impact of a Dementia-Friendly Garden Design on People With Dementia in a Residential Aged Care Facility: A Case Study. Health Environ. Res. Des. J. 2022, 15, 196–218. [Google Scholar] [CrossRef] [PubMed]
- Wilson, E.O. Biophilia; Harvard University Press: London, UK, 1986. [Google Scholar]
- Choe, E.Y.; Jorgensen, A.; Sheffield, D. Does a natural environment enhance the effectiveness of Mindfulness-Based Stress Reduction (MBSR)? Examining the mental health and wellbeing, and nature connectedness benefits. Landsc. Urban Plan. 2020, 202, 103886. [Google Scholar] [CrossRef]
- Hartig, T.; Mitchell, R.; De Vries, S.; Frumkin, H. Nature and health. Annu. Rev. Public Health 2014, 35, 207–228. [Google Scholar] [CrossRef] [PubMed]
- Maller, C.; Townsend, M.; Pryor, A.; Brown, P.; St Leger, L. Healthy nature healthy people:‘contact with nature’as an upstream health promotion intervention for populations. Health Promot. Int. 2006, 21, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Orr, N.; Wagstaffe, A.; Briscoe, S.; Garside, R. How do older people describe their sensory experiences of the natural world? A systematic review of the qualitative evidence. BMC Geriatr. 2016, 16, 116. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.; Wolverson, E.; Price, E. Me, myself, and nature: Living with dementia and connecting with the natural world—More than a breath of fresh air? A literature review. Dementia 2022, 21, 2351–2376. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.T.; Kirkevold, M. Benefits of sensory garden and horticultural activities in dementia care: A modified scoping review. J. Clin. Nurs. 2014, 23, 2698–2715. [Google Scholar] [CrossRef] [PubMed]
- Murroni, V.; Cavalli, R.; Basso, A.; Borella, E.; Meneghetti, C.; Melendugno, A.; Pazzaglia, F. Effectiveness of therapeutic gardens for people with dementia: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 9595. [Google Scholar] [CrossRef] [PubMed]
- Motealleh, P.; Moyle, W.; Jones, C.; Dupre, K. Creating a dementia-friendly environment through the use of outdoor natural landscape design intervention in long-term care facilities: A narrative review. Health Place 2019, 58, 102148. [Google Scholar] [CrossRef] [PubMed]
- Kellert, S.; Calabrese, E. The Practice of Biophilic Design; Terrapin Bright LLC: London, UK, 2015; Volume 3. [Google Scholar]
- Goudriaan, I.; van Boekel, L.C.; Verbiest, M.E.A.; van Hoof, J.; Luijkx, K.G. Dementia enlightened?! a systematic literature review of the influence of indoor environmental light on the health of older persons with dementia in long-term care facilities. Clin. Interv. Aging 2021, 16, 909–937. [Google Scholar] [CrossRef] [PubMed]
- D’Andrea, F.; Tischler, V.; Dening, T.; Churchill, A. Olfactory stimulation for people with dementia: A rapid review. Dementia 2022, 21, 1800–1824. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yuan, X. Smellscape as a healing factor in institutional gardens to enhance health and well-being for older people with dementia: A scoping review. J. Clin. Nurs. 2024, 33, 454–468. [Google Scholar] [CrossRef] [PubMed]
- Al Ghassani, A.; Rababa, M.; Abu Khait, A. Agitation in people with dementia: A concept analysis. Nurs. Forum 2021, 56, 1015–1023. [Google Scholar] [CrossRef] [PubMed]
- Barker, T.H.; Stone, J.C.; Sears, K.; Klugar, M.; Leonardi-Bee, J.; Tufanaru, C.; Aromataris, E.; Munn, Z. Revising the JBI quantitative critical appraisal tools to improve their applicability: An overview of methods and the development process. JBI Evid. Synth. 2023, 21, 478–493. [Google Scholar] [CrossRef] [PubMed]
- Suurmond, R.; van Rhee, H.; Hak, T. Introduction, comparison, and validation of Meta-Essentials: A free and simple tool for meta-analysis. Res. Synth. Methods 2017, 8, 537–553. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical power analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and Fill: A Simple Funnel-Plot-Based Method. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Cochrane: London, UK, 2011. [Google Scholar]
- Figueiro, M.G.; Plitnick, B.A.; Lok, A.; Jones, G.E.; Higgins, P.; Hornick, T.R.; Rea, M.S. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin. Interv. Aging 2014, 9, 1527–1537. [Google Scholar] [CrossRef] [PubMed]
- Ciobanu, I.; Draghici, R.; Marin, A.G.; Zamfir, M.V.; Iliescu, A.; Zamfir, M.; Goodall, G.; Popescu, M.N.; Serrano, J.; Berteanu, M. Case series of an ICT-based multimodal intervention program for people with major neurocognitive disorders: The SENSE-GARDEN project. J. Gerontol. Geriatr. Med. 2022, 8, 2. [Google Scholar]
- Fu, C.Y.; Moyle, W.; Cooke, M. A randomised controlled trial of the use of aromatherapy and hand massage to reduce disruptive behaviour in people with dementia. BMC Complement. Altern. Med. 2013, 13, 165. [Google Scholar] [CrossRef] [PubMed]
- Figueiro, M.G.; Plitnick, B.; Roohan, C.; Sahin, L.; Kalsher, M.; Rea, M.S. Effects of a Tailored Lighting Intervention on Sleep Quality, Rest—Activity, Mood, and Behavior in Older Adults With Alzheimer Disease and Related Dementias: A Randomized Clinical Trial. J. Clin. Sleep Med. 2019, 15, 1757–1767. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, L.; Middleton, J.; Russell, G.; Stewart, N. Bright light therapy for demented nursing home patients with behavioral disturbance. Am. J. Alzheimers Dis. Other Demen 2000, 15, 18–26. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Sahin, L.; Kalsher, M.; Plitnick, B.; Rea, M.S. Long-Term, All-Day Exposure to Circadian-Effective Light Improves Sleep, Mood, and Behavior in Persons with Dementia. J. Alzheimers Dis. Rep. 2020, 4, 297–312. [Google Scholar] [CrossRef] [PubMed]
- Figueiro, M.G.; Kales, H.C. Lighting and Alzheimer’s disease and related dementias: Spotlight on sleep and depression. Light. Res. Technol. 2021, 53, 405–422. [Google Scholar] [CrossRef] [PubMed]
- Saidane, H.A.; Rasmussen, T.; Andersen, K.; Iversen, H.K.; West, A.S. An Explorative Investigation of the Effect of Naturalistic Light on Agitation-Associated Behavior in Nursing Home Residents With Dementia: A Pilot Study. Health Environ. Res. Des. J. 2023, 16, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Connell, B.R.; Sanford, J.A.; Lewis, D. Therapeutic effects of an outdoor activity program on nursing home residents with Dementia. Outdoor Environ. People Dement. 2007, 21, 194–209. [Google Scholar] [CrossRef]
- Ballard, C.G.; O’Brien, J.T.; Reichelt, K.; Perry, E.K. Aromatherapy as a safe and effective treatment for the management of agitation in severe dementia: The results of a double-blind, placebo-controlled trial with Melissa. J. Clin. Psychiatry 2002, 63, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.W.K.; Chan, W.C.; Ng, B.F.L.; Lam, L.C.W. Efficacy of aromatherapy (Lavandula angustifolia) as an intervention for agitated behaviours in Chinese older persons with dementia: A cross-over randomized trial. Int. J. Geriatr. Psychiatry 2007, 22, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Burns, A.; Perry, E.; Holmes, C.; Francis, P.; Morris, J.; Howes, M.J.R.; Chazot, P.; Lees, G.; Ballard, C. A double-blind placebo-controlled randomized trial of melissa officinalis oil and donepezil for the treatment of agitation in Alzheimer’s disease. Dement. Geriatr. Cogn. Disord. 2011, 31, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, Y.; Ebihara, S.; Ebihara, T.; Tomita, N.; Toba, K.; Freeman, S.; Arai, H.; Kohzuki, M. Fall prevention using olfactory stimulation with lavender odor in elderly nursing home residents: A randomized controlled trial. J. Am. Geriatr. Soc. 2012, 60, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, D.W.; Eppingstall, B.; Taffe, J.; van der Ploeg, E.S. A randomized, controlled cross-over trial of dermally-applied lavender (Lavandula angustifolia) oil as a treatment of agitated behaviour in dementia. BMC Complement. Altern. Med. 2013, 13, 315. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.H.; Lin, L.C.; Wu, S.C.; Chiu, J.H.; Wang, P.N.; Lin, J.G. Comparison of the efficacy of aroma-acupressure and aromatherapy for the treatment of dementia-associated agitation. BMC Complement. Altern. Med. 2015, 15, 93. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Watanuki, E.; Koyama, S. Effects of inhalation aromatherapy on symptoms of sleep disturbance in the elderly with dementia. Evid.-Based Complement. Altern. Med. 2017, 2017, 1902807. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Shindo, S.; Kanbayashi, T.; Takeshima, M.; Imanishi, A.; Mishima, K. Examination of the influence of cedar fragrance on cognitive function and behavioral and psychological symptoms of dementia in Alzheimer type dementia. Neuropsychopharmacol. Rep. 2020, 40, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Ting, Y.Y.; Tien, Y.; Huang, H.P. Effects of aromatherapy on agitation in patients with dementia in the community: A quasi-experimental study. Geriatr. Nurs. 2023, 51, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Burgio, L.D.; Butler, F.R.; Roth, D.L.; Michael Hardin, J.; Hsu, C.C.; Ung, K. Agitation in nursing home residents: The role of gender and social context. Int. Psychogeriatr. 2000, 12, 495–511. [Google Scholar] [CrossRef] [PubMed]
- Whall, A.L.; Black, M.E.; Groh, C.J.; Yankou, D.J.; Kupferschmid, B.J.; Foster, N.L. Aggression. The effect of natural environments upon agitation and aggression in late stage dementia patients. Am. J. Alzheimer’s Dis. 1997, 12, 216–220. [Google Scholar] [CrossRef]
- Reynolds, L.; Rodiek, S.; Lininger, M.; Mcculley, M.A. Can a Virtual Nature Experience Reduce Anxiety and Agitation in People With Dementia? J. Hous. Elder. 2018, 32, 176–193. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, S. Effects of indoor gardening on sleep, agitation, and cognition in dementia patients—A pilot study. Int. J. Geriatr. Psychiatry 2008, 23, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Pedrinolla, A.; Tamburin, S.; Brasioli, A.; Sollima, A.; Fonte, C.; Muti, E.; Smania, N.; Schena, F.; Venturelli, M. An Indoor Therapeutic Garden for Behavioral Symptoms in Alzheimer’s Disease: A Randomized Controlled Trial. J. Alzheimer’s Dis. 2019, 71, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Wilkes, L.; Fleming, A.; Wilkes, B.L.; Cioffi, J.M.; Le Miere, J. Environment in reducing agitation in dementia Environmental approach to reducing agitation in older persons with dementia in a nursing home. Australas. J. Ageing 2005, 24, 141–145. [Google Scholar] [CrossRef]
- Detweiler, M.B.; Murphy, P.F.; Myers, L.C.; Kim, K.Y. Does a wander garden influence inappropriate behaviors in dementia residents? Am. J. Alzheimers Dis. Other Demen. 2008, 23, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Murphy, P.F.; Miyazaki, Y.; Detweiler, M.B.; Kim, K.Y. Longitudinal analysis of differential effects on agitation of a therapeutic wander garden for dementia patients based on ambulation ability. Dementia 2010, 9, 355–373. [Google Scholar] [CrossRef]
- Luk, K.Y.; Lai, K.Y.C.; Li, C.C.; Cheung, W.H.; Lam, S.M.R.; Li, H.Y.; Ng, K.P.; Shiu, W.H.; So, C.Y.; Wan, S.F. The effect of horticultural activities on agitation in nursing home residents with dementia. Int. J. Geriatr. Psychiatry 2011, 26, 435–436. [Google Scholar] [CrossRef] [PubMed]
- Edwards, C.A.; McDonnell, C.; Merl, H. An evaluation of a therapeutic garden’s influence on the quality of life of aged care residents with dementia. Dementia 2012, 12, 494–510. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M.; Butler, C.W. Nature connectedness and biophilic design. Build. Res. Inf. 2022, 50, 36–42. [Google Scholar] [CrossRef]
- Fleming, R.; Purandare, N. Long-term care for people with dementia: Environmental design guidelines. Int. Psychogeriatr. 2010, 22, 1084–1095. [Google Scholar] [CrossRef] [PubMed]
- Kolanowski, A.; Litaker, M. Social interaction, premorbid personality, and agitation in nursing home residents with dementia. Arch. Psychiatr. Nurs. 2006, 20, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Zeisel, J.; Silverstein, N.M.; Hyde, J.; Levkoff, S.; Lawton, M.P.; Holmes, W. Environmental correlates to behavioral health outcomes in Alzheimer’s special care units. Gerontologist 2003, 43, 697–711. [Google Scholar] [CrossRef] [PubMed]
- Bellelli, G.; Frisoni, G.B.; Bianchetti, A.; Boffelli, S.; Guerrini, G.B.; Scotuzzi, A.; Ranieri, P.; Ritondale, G.; Guglielmi, L.; Fusari, A.; et al. Special care units for demented patients: A multicenter study. Gerontologist 1998, 38, 456–462. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alessi, C.A.; Yoon, E.J.; Schnelle, J.F.; Al-Samarrai, N.R.; Cruise, P.A. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: Do sleep and agitation improve? J. Am. Geriatr. Soc. 1999, 47, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Alessi, C.A.; Martin, J.L.; Webber, A.P.; Cynthia Kim, E.; Harker, J.O.; Josephson, K.R. Randomized, controlled trial of a nonpharmacological intervention to improve abnormal sleep/wake patterns in nursing home residents. J. Am. Geriatr. Soc. 2005, 53, 803–810. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).