Determinants of Public Knowledge, Attitude, and Practice on Antibiotic Use in Saudi Arabia: A Regional Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Questionnaire Development
2.3. Piloting the Questionnaire
2.4. Sample Size Calculation
2.5. Sample Recruitment and Data Collection
2.6. Statistical Analysis
2.7. Ethical Considerations
3. Results
3.1. Participants’ Demographic Characteristics
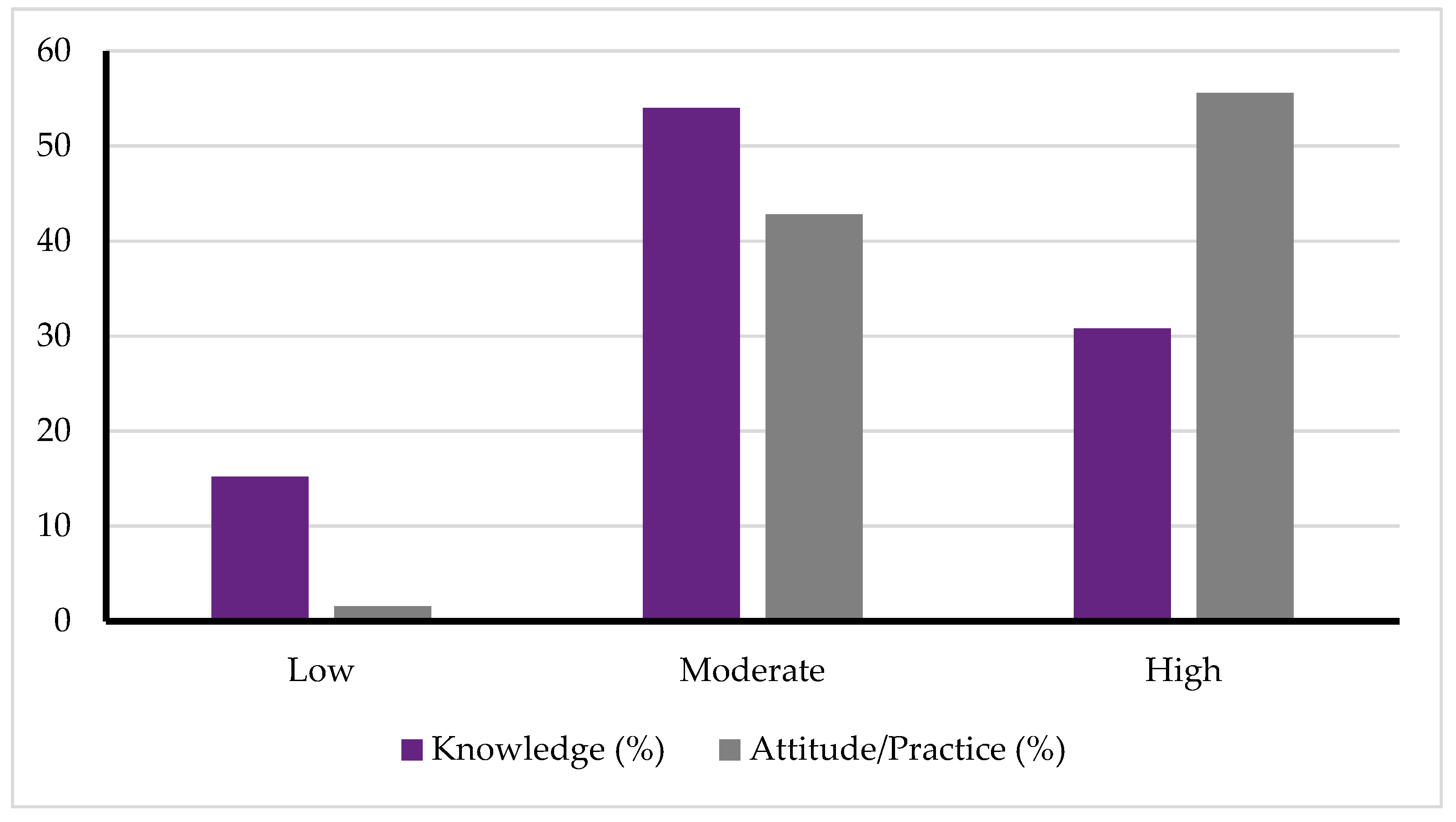
3.2. Levels of Knowledge and Attitude/Practice Toward Antibiotic Use
3.3. Association Between Knowledge Level and Attitude/Practice Toward Antibiotic Use
3.4. Predictors of High Knowledge Toward Antibiotic Use
3.5. Predictors of Good Attitude and Practice Toward Antibiotic Use
4. Discussion
4.1. Implications for Public Health and Policy
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- D’Amico, R.; Pifferi, S.; Torri, V.; Brazzi, L.; Parmelli, E. Antibiotic prophylaxis to reduce respiratory tract infections and mortality in adults receiving intensive care. Cochrane Database Syst. Rev. 2009, CD000022. [Google Scholar] [CrossRef] [PubMed]
- Carey, G.B.; Holleck, J.L.; Ein Alshaeba, S.; Jayakrishnan, R.; Gordon, K.S.; Grimshaw, A.A.; Gunderson, C.G. Estimated mortality with early empirical antibiotic coverage of methicillin-resistant Staphylococcus aureus in hospitalized patients with bacterial infections: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2023, 78, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Kudou, M.; Nakanishi, M.; Kuriu, Y.; Arita, T.; Shimizu, H.; Kiuchi, J.; Katsurahara, K.; Ikoma, H.; Kubota, T.; Fujiwara, H. The effect of preoperative oral antibiotics in the prevention of surgical site infection after laparoscopic colorectal cancer surgery: A propensity score matching study. J. Anus Rectum Colon. 2021, 5, 319–326. [Google Scholar] [CrossRef]
- Teillant, A.; Gandra, S.; Barter, D.; Morgan, D.J.; Laxminarayan, R. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: A literature review and modelling study. Lancet Infect. Dis. 2015, 15, 1429–1437. [Google Scholar] [CrossRef]
- Baquero, F. Threats of antibiotic resistance: An obliged reappraisal. Int. Microbiol. 2021, 24, 499–506. [Google Scholar] [CrossRef]
- Cars, O.; Nordberg, P. Antibiotic resistance–The faceless threat. Int. J. Risk Saf. Med. 2005, 17, 103–110. [Google Scholar] [CrossRef]
- Tangcharoensathien, V.; Chanvatik, S.; Sommanustweechai, A. Complex determinants of inappropriate use of antibiotics. Bull. World Health Organ. 2018, 96, 141. [Google Scholar] [CrossRef] [PubMed]
- Kotwani, A.; Joshi, J.; Lamkang, A.S.; Sharma, A.; Kaloni, D. Knowledge and behavior of consumers towards the non-prescription purchase of antibiotics: An insight from a qualitative study from New Delhi, India. Pharm. Pract. 2021, 19, 2206. [Google Scholar] [CrossRef]
- Do, N.T.; Vu, H.T.; Nguyen, C.T.; Punpuing, S.; Khan, W.A.; Gyapong, M.; Asante, K.P.; Munguambe, K.; Gómez-Olivé, F.X.; John-Langba, J. Community-based antibiotic access and use in six low-income and middle-income countries: A mixed-method approach. Lancet Glob. Health 2021, 9, e610–e619. [Google Scholar] [CrossRef]
- Hayes, J.F. Fighting back against antimicrobial resistance with comprehensive policy and education: A narrative review. Antibiotics 2022, 11, 644. [Google Scholar] [CrossRef]
- Sitotaw, B.; Philipos, W. Knowledge, Attitude, and Practices (KAP) on Antibiotic Use and Disposal Ways in Sidama Region, Ethiopia: A Community-Based Cross-Sectional Survey. Sci. World J. 2023, 2023, 8774634. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.I.; Aboud, E.A. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS ONE 2015, 10, e0117910. [Google Scholar] [CrossRef]
- Karuniawati, H.; Hassali, M.A.A.; Suryawati, S.; Ismail, W.I.; Taufik, T.; Hossain, M.S. Assessment of knowledge, attitude, and practice of antibiotic use among the population of Boyolali, Indonesia: A cross-sectional study. Int. J. Environ. Res. Public. Health 2021, 18, 8258. [Google Scholar] [CrossRef]
- Gillani, A.H.; Chang, J.; Aslam, F.; Saeed, A.; Shukar, S.; Khanum, F.; Jairoun, A.; Nicholson, A.; Mohamed Ibrahim, M.I.; Fang, Y. Public knowledge, attitude, and practice regarding antibiotics use in Punjab, Pakistan: A cross-sectional study. Expert. Rev. Anti-Infect. Ther. 2021, 19, 399–411. [Google Scholar] [CrossRef]
- Angelillo, S.; Paduano, G.; Sansone, V.; De Filippis, A.; Finamore, E.; Pelullo, C.P.; Di Giuseppe, G. Exploring Knowledge, Attitudes, and Behaviors Toward Antibiotics Use Among Adolescents in Southern Italy. Microorganisms 2025, 13, 290. [Google Scholar] [CrossRef] [PubMed]
- Ghaffoori Kanaan, M.H.; Tarek, A.M.; Abdullah, S.S. Knowledge and attitude among samples from community members, pharmacists and health care providers about antibiotic resistance in Al- Suwaria city/Wassit province/Iraq. IOP Conf. Ser. Earth Environ. Sci. 2021, 790, 012059. [Google Scholar] [CrossRef]
- Nafisah, S.B.; Nafesa, S.B.; Alamery, A.H.; Alhumaid, M.A.; AlMuhaidib, H.M.; Al-Eidan, F.A. Over-the-counter antibiotics in Saudi Arabia, an urgent call for policy makers. J. Infect. Public Health 2017, 10, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Al-Jedai, A.H.; Almogbel, Y.; Eljaaly, K.; Alqahtani, N.M.; Almudaiheem, H.Y.; Awad, N.; Alissa, D.A.; Assiri, A.; Alaama, T. Restriction on antimicrobial dispensing without prescription on a national level: Impact on the overall antimicrobial utilization in the community pharmacies in Saudi Arabia. PLoS ONE 2022, 17, e0271188. [Google Scholar] [CrossRef]
- Shatla, M.; Althobaiti, F.S.; Almqaiti, A.; Shatla Sr, M.; Almqaiti, A.A. Public knowledge, attitudes, and practices towards antibiotic use and antimicrobial resistance in the western region of Saudi Arabia. Cureus 2022, 14, e31857. [Google Scholar] [CrossRef]
- Zaidi, S.F.; Baroom, M.W.; Ibrahim Hanbashi, A.; Abdulaziz Alkhaibari, A.; Omar Yahya, A.; Alsalmi, M.; Alotaibi, R.; Nagro, A.; Anwar Khan, M.; Alshanberi, A.M. Cross-sectional survey among general population regarding knowledge and attitude toward antibiotic usage in Western Saudi Arabia. Pharmacy 2021, 9, 98. [Google Scholar] [CrossRef]
- Alshehri, A.A.; Khawagi, W.Y. Knowledge, Awareness, and Perceptions Towards Antibiotic Use, Resistance, and Antimicrobial Stewardship Among Final-Year Medical and Pharmacy Students in Saudi Arabia. Antibiotics 2025, 14, 116. [Google Scholar] [CrossRef]
- Singh, R.; Agarwal, T.M.; Al-Thani, H.; Al Maslamani, Y.; El-Menyar, A. Validation of a survey questionnaire on organ donation: An Arabic world scenario. J. Transplant. 2018, 2018, 9309486. [Google Scholar] [CrossRef] [PubMed]
- Makki, M.; Hassali, M.A.A.; Awaisu, A.; Chemaitelly, H.; Al Hail, M.; Mohammed ElMotasim, W.; Yousif Mohamed Ali Taha, M.; Mohd J Al-Khuzaei, N.; Salama, G.; Pallivalapila, A.; et al. Development, translation, and validation of a bilingual questionnaire on unused medications in homes. Saudi Pharm. J. 2021, 29, 648–655. [Google Scholar] [CrossRef]
- Kavookjian, J.; LaManna, J.B.; Davidson, P.; Davis, J.W.; Fahim, S.M.; McDaniel, C.C.; Ekong, G.; Todd, A.; Yehl, K.; Cox, C. Impact of diabetes self-management education/support on self-reported quality of life in youth with type 1 or type 2 diabetes. Sci. Diabetes Self-Manag. Care 2022, 48, 406–436. [Google Scholar] [CrossRef]
- Alfagih, S.A.; Albabtain, M.A.; Alfagih, M.; Alharbi, N. Evaluating Public Behavior toward Antibiotic Use in Riyadh: A Cross-Sectional Study. Pharmacoepidemiology (2813-0618) 2024, 3, 297. [Google Scholar] [CrossRef]
- Hejaz, H.A. Knowledge and Attitudes towards Antibiotic Usage. Jordan J. Pharm. Sci. 2023, 16, 447. [Google Scholar] [CrossRef]
- Hernández-Díaz, I.; Ayala-Meléndez, A.; González-González, E.; Rosario-Calderón, I.; Figueroa-Ríos, D.; Melin, K.; Hernández-Muñoz, J.J. Knowledge and beliefs, behaviors, and adherence among Latino parents or legal guardians related to antibiotic use for upper respiratory tract infections in children under 6 years of age. J. Am. Pharm. Assoc. 2019, 59, 506–513. [Google Scholar] [CrossRef]
- Chae, S.-M.; Park, E.-J.; Park, S. Consumers’ knowledge and attitudes toward antibiotic resistance. Health Policy Manag. 2011, 21, 365–380. [Google Scholar] [CrossRef]
- Henaine, A.-M.; Lahoud, N.; Abdo, R.; Shdeed, R.; Safwan, J.; Akel, M.; Fahs, I.; Zeenny, R.; Sacre, H.; Hallit, S. Knowledge of Antibiotics Use among Lebanese Adults: A study on the influence of sociodemographic characteristics. Sultan Qaboos Univ. Med. J. 2021, 21, 442. [Google Scholar] [CrossRef]
- Jimah, T.; Ogunseitan, O. Socio-demographic characteristics of the association between knowledge of antibiotic therapy and prudent use in Ghana. J. Glob. Health Rep. 2020, 4, e2020034. [Google Scholar] [CrossRef]
- Sun, R.; Yao, T.; Zhou, X.; Harbarth, S.; Lin, L. Non-biomedical factors affecting antibiotic use in the community: A mixed-methods systematic review and meta-analysis. Clin. Microbiol. Infect. 2022, 28, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Sabbatucci, M.; Furiozzi, F.; Iannazzo, S.; Maugeri, A.; Maraglino, F.; Prato, R.; Agodi, A.; Pantosti, A. Knowledge, attitudes and behaviors on antibiotic use and resistance among healthcare workers in Italy, 2019: Investigation by a clustering method. Antimicrob. Resist. Infect. Control 2021, 10, 134. [Google Scholar] [CrossRef] [PubMed]
- Shu, G.; Jayawardena, K.; Jayaweera Patabandige, D.; Tennegedara, A.; Liyanapathirana, V. Knowledge, perceptions and practices on antibiotic use among Sri Lankan doctors. PLoS ONE 2022, 17, e0263167. [Google Scholar] [CrossRef] [PubMed]
- Sulis, G.; Adam, P.; Nafade, V.; Gore, G.; Daniels, B.; Daftary, A.; Das, J.; Gandra, S.; Pai, M. Antibiotic prescription practices in primary care in low-and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020, 17, e1003139. [Google Scholar] [CrossRef]
- Machowska, A.; Stålsby Lundborg, C. Drivers of irrational use of antibiotics in Europe. Int. J. Environ. Res. Public Health 2019, 16, 27. [Google Scholar] [CrossRef]
- Al-Homaidan, H.T.; Barrimah, I.E. Physicians’ knowledge, expectations, and practice regarding antibiotic use in primary health care. Int. J. Health Sci. 2018, 12, 18. [Google Scholar]
- Alshehri, A.A.; Jalal, Z.; Cheema, E.; Haque, M.S.; Jenkins, D.; Yahyouche, A. Impact of the pharmacist-led intervention on the control of medical cardiovascular risk factors for the primary prevention of cardiovascular disease in general practice: A systematic review and meta-analysis of randomised controlled trials. Br. J. Clin. Pharmacol. 2020, 86, 29–38. [Google Scholar] [CrossRef]
- Boeni, F.; Arnet, I.; Hersberger, K.E. Adherence counseling during patient contacts in swiss community pharmacies. Patient Prefer. Adherence 2015, 9, 597–605. [Google Scholar] [CrossRef]
- Jones, L.F.; Owens, R.; Sallis, A.; Ashiru-Oredope, D.; Thornley, T.; Francis, N.A.; Butler, C.; McNulty, C.A. Qualitative study using interviews and focus groups to explore the current and potential for antimicrobial stewardship in community pharmacy informed by the Theoretical Domains Framework. BMJ Open 2018, 8, e025101. [Google Scholar] [CrossRef]
- Lee, Y.; Bradley, N. Antimicrobial stewardship practices in a subset of community pharmacies across the United States. Pharmacy 2023, 11, 26. [Google Scholar] [CrossRef]
- Tagum-Briones, J.M.; Romero, C.B.; De Villa, L.V.; Hisan, U.K. Knowledge, Attitudes, and Practices on Antibiotic Use: Inputs to the Development of Educational Materials on Antibiotics. J. Public Health Sci. 2023, 2, 1–19. [Google Scholar] [CrossRef]
- Geta, K.; Kibret, M. Knowledge, attitudes and practices of patients on antibiotic resistance and use in Public Hospitals of Amhara Regional State, Northwestern Ethiopia: A cross-sectional study. Infect. Drug Resist. 2022, 15, 193–209. [Google Scholar] [CrossRef] [PubMed]
- Zucco, R.; Lavano, F.; Anfosso, R.; Bianco, A.; Pileggi, C.; Pavia, M. Internet and social media use for antibiotic-related information seeking: Findings from a survey among adult population in Italy. Int. J. Med. Inform. 2018, 111, 131–139. [Google Scholar] [CrossRef]
- Wang, S.; Ogunseitan, O. Assessment of college students’ knowledge, attitudes, and practices regarding antibiotics stewardship. Int. J. Infect. Dis. 2022, 116, S14–S15. [Google Scholar] [CrossRef]
- Oyetunde, O.O.; Olugbake, O.A.; Famudehin, K.F. Evaluation of use of antibiotic without prescription among young adults. Afr. J. Pharm. Pharmacol. 2010, 4, 760–762. [Google Scholar]
- Lock, B.X.; Chong, C.P. Effects of pharmacist-led counseling on pediatric antibiotic suspension reconstitution knowledge and technique among rural parents: A multicenter study in Malaysia. J. Appl. Pharm. Sci. 2024, 14, 065–074. [Google Scholar] [CrossRef]
- Afzal, S.; Khan, F.U.; Aqeel, M.T.; Ullah, M.; Bajwa, M.; Akhtar, M.; Majid, M. Impact of a pharmacist-led educational intervention on knowledge, attitude, and practice toward the rational use of antibiotics among healthcare workers in a secondary care hospital in Punjab, Pakistan. Front. Pharmacol. 2024, 14, 1327576. [Google Scholar] [CrossRef]
- Bishop, C.; Yacoob, Z.; Knobloch, M.J.; Safdar, N. Community pharmacy interventions to improve antibiotic stewardship and implications for pharmacy education: A narrative overview. Res. Soc. Adm. Pharm. 2019, 15, 627–631. [Google Scholar] [CrossRef]
- Christian, J.G.; Byers, T.E.; Christian, K.K.; Goldstein, M.G.; Bock, B.C.; Prioreschi, B.; Bessesen, D.H. A computer support program that helps clinicians provide patients with metabolic syndrome tailored counseling to promote weight loss. J. Am. Diet. Assoc. 2011, 111, 75–83. [Google Scholar] [CrossRef]
- Smith, C.R.; Pogany, L.; Foley, S.; Wu, J.; Timmerman, K.; Gale-Rowe, M.; Demers, A. Canadian physicians’ knowledge and counseling practices related to antibiotic use and antimicrobial resistance: Two-cycle national survey. Can. Fam. Physician 2017, 63, e526–e535. [Google Scholar]
- Hebert, J.R.; Clemow, L.; Pbert, L.; Ockene, I.S.; Ockene, J.K. Social desirability bias in dietary self-report may compromise the validity of dietary intake measures. Int. J. Epidemiol. 1995, 24, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Klesges, L.M.; Baranowski, T.; Beech, B.; Cullen, K.; Murray, D.M.; Rochon, J.; Pratt, C. Social desirability bias in self-reported dietary, physical activity and weight concerns measures in 8-to 10-year-old African-American girls: Results from the Girls Health Enrichment Multisite Studies (GEMS). Prev. Med. 2004, 38, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Groenwold, R.H.; Nelson, D.B.; Nichol, K.L.; Hoes, A.W.; Hak, E. Sensitivity analyses to estimate the potential impact of unmeasured confounding in causal research. Int. J. Epidemiol. 2010, 39, 107–117. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) | |
|---|---|---|
| Gender | ||
| Male | 324 (36.4) | |
| Female | 567 (63.6) | |
| Age (years) | ||
| 18–30 | 501 (56.2) | |
| 31–40 | 142 (15.9) | |
| 41–50 | 170 (19.1) | |
| >50 | 78 (8.8) | |
| Education Level | ||
| Less than high school | 26 (2.9) | |
| High school | 205 (23.0) | |
| Bachelor’s degree | 593 (66.6) | |
| Postgraduate studies | 67 (7.5) | |
| Marital Status | ||
| Single | 472 (53.0) | |
| Married | 366 (41.1) | |
| Divorced | 37 (4.1) | |
| Widow | 16 (1.8) | |
| Residency City/Area | ||
| Taif | 478 (53.6) | |
| Makkah | 64 (7.2) | |
| Jeddah | 168 (18.9) | |
| Yanbu | 33 (3.7) | |
| Madinah | 45 (5.1) | |
| Other | 103 (11.6) | |
| Monthly Income (SAR) | ||
| Less than 3000 | 382 (42.9) | |
| 3000 to 10,000 | 255 (28.6) | |
| More than 10,000 | 254 (28.5) | |
| Antibiotic Use in the Past Year | ||
| 1–2 times | 369 (41.4) | |
| 3–5 times | 207 (23.2) | |
| More than 5 times | 122 (13.7) | |
| None | 193 (21.7) | |
| Source of Antibiotics | ||
| Government pharmacies | 514 (57.7) | |
| Private pharmacies | 377 (42.3) | |
| Employment in Healthcare Sector | ||
| Yes | 184 (20.7) | |
| No | 707 (79.3) | |
| Domain | Level | (n) | (%) | Mean ± SD |
|---|---|---|---|---|
| Knowledge | Low (<5) | 135 | 15.2 | 7.11 ± 2.59 |
| Moderate (5–8) | 481 | 54.0 | ||
| High (>8) | 275 | 30.8 | ||
| Attitude/Practice | Poor (<5) | 14 | 1.6 | 8.70 ± 2.19 |
| Average (5–8) | 381 | 42.8 | ||
| Good (>8) | 496 | 55.6 |
| Knowledge Level | n (%) | Poor Attitude/Practice | Average Attitude/Practice | Good Attitude/Practice | p-Value |
|---|---|---|---|---|---|
| Low (<5) | 135 (15.2%) | 4 (3.0%) | 85 (63.0%) | 46 (34.1%) | <0.001 |
| Moderate (5–8) | 481 (54.0%) | 9 (1.9%) | 240 (49.9%) | 232 (48.2%) | |
| High (>8) | 275 (30.8%) | 1 (0.4%) | 56 (20.4%) | 218 (79.3%) |
| Risk factors | Good Level of Knowledge (%) | COR (95% CI) | p Value | aOR (95% CI) | p Value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18–30 | 159 (31.7%) | 1 | 1 | |||
| 31–40 | 37 (26.1%) | 0.76 (0.50–1.15) | 0.195 | 1.67 (1.03–2.72) | 0.038 | |
| 41–50 | 52 (30.6%) | 0.95 (0.65–1.38) | 0.781 | 2.22 (1.42–3.48) | 0.001 | |
| More than 50 | 27 (34.6%) | 1.14 (0.69–1.88) | 0.613 | 2.13 (1.19–3.82) | 0.011 | |
| Gender | ||||||
| Male | 78 (24.1%) | 1 | ||||
| Female | 197 (34.7%) | 1.68 (1.23–2.28) | 0.001 | 1.90 (1.34–2.70) | <0.001 | |
| Education Level | ||||||
| Less than high school | 1 (3.8%) | 1 | 1 | |||
| High school | 40 (19.5%) | 6.06 (0.80–46.07) | 0.082 | 9.50 (1.18–76.44) | 0.034 | |
| Bachelor’s degree | 210 (35.4%) | 13.71 (1.84–101.88) | 0.011 | 14.48 (1.85–113.41) | 0.011 | |
| Postgraduate studies | 24 (35.8%) | 13.95 (1.78–109.50) | 0.012 | 15.37 (1.84–128.13) | 0.012 | |
| Marital Status | ||||||
| Single | 149 (31.6%) | 1 | ||||
| Married | 114 (31.1%) | 0.98 (0.73–1.32) | 0.897 | |||
| Divorced | 8 (21.6%) | 0.60 (0.27–1.34) | 0.211 | |||
| Widow | 4 (25.0%) | 0.72 (0.23–2.28) | 0.579 | |||
| Residence | ||||||
| Taif | 170 (35.6%) | 1 | ||||
| Makkah | 17 (26.6%) | 0.66 (0.37–1.18) | 0.157 | |||
| Jeddah | 49 (29.2%) | 0.75 (0.51–1.09) | 0.133 | |||
| Yanbu | 8 (24.2%) | 0.58 (0.26–1.31) | 0.191 | |||
| Madinah | 8 (17.8%) | 0.39 (0.18–0.86) | 0.020 | |||
| Other | 23 (22.3%) | 0.52 (0.32–0.86) | 0.011 | |||
| Monthly Income | ||||||
| Less than 3000 SAR | 105 (27.5%) | 1 | ||||
| 3000 to 10,000 SAR | 80 (31.4%) | 1.21 (0.85–1.71) | 0.290 | |||
| More than 10,000 SAR | 90 (35.4%) | 1.45 (1.03–2.04) | 0.034 | |||
| Antibiotic Use in the Past Year | ||||||
| 1–2 times | 139 (37.7%) | 1 | 1 | |||
| 3–5 times | 47 (22.7%) | 0.49 (0.33–0.72) | <0.001 | 0.59 (0.38–0.89) | 0.013 | |
| More than 5 times | 21 (17.2%) | 0.34 (0.21–0.58) | <0.001 | 0.37 (0.21–0.65) | 0.001 | |
| None | 68 (35.2%) | 0.90 (0.63–1.29) | 0.570 | 0.96 (0.64–1.45) | 0.856 | |
| Working in Healthcare | ||||||
| Yes | 116 (63.0%) | 1 | 1 | |||
| No | 159 (22.5%) | 0.17 (0.12–0.24) | <0.001 | 0.14 (0.09–0.20) | <0.001 | |
| Source of Information | ||||||
| The doctor | 135 (29.2%) | 1 | ||||
| The pharmacist | 88 (32.7%) | 1.18 (0.85–1.63) | 0.314 | |||
| Internet | 44 (37.6%) | 1.46 (0.96–2.24) | 0.078 | |||
| Family or friends | 5 (21.7%) | 0.68 (0.25–1.86) | 0.446 | |||
| Media (TV, newspapers) | 3 (15.8%) | 0.46 (0.13–1.59) | 0.217 | |||
| Doctor Counseling | ||||||
| Yes | 118 (24.3%) | 1 | 1 | |||
| No | 157 (38.8%) | 1.97 (1.48–2.63) | <0.001 | 1.78 (1.29–2.46) | <0.001 | |
| Pharmacist Counseling | ||||||
| Yes | 191 (30.2%) | 1 | ||||
| No | 84 (32.4%) | 1.11 (0.81–1.52) | 0.517 | |||
| Risk Factors | Good Level of Knowledge (%) | COR (95% CI) | p Value | AOR (95% CI) | p Value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| 18–30 | 228 (45.5%) | 1 | 1 | |||
| 31–40 | 66 (46.5%) | 1.04 (0.72–1.51) | 0.838 | |||
| 41–50 | 85 (50.0%) | 1.20 (0.85–1.70) | 0.311 | |||
| More than 50 | 41 (52.6%) | 1.33 (0.82–2.14) | 0.246 | |||
| Gender | ||||||
| Male | 111 (34.3%) | 1 | 1 | |||
| Female | 309 (54.5%) | 2.30 (1.73–3.05) | <0.001 | 2.32 (1.66–3.24) | <0.001 | |
| Education level | ||||||
| Less than high school | 8 (30.8%) | 1 | 1 | |||
| High school | 93 (45.4%) | 0.80 (0.30–2.10) | 0.646 | 2.78 (1.07–7.23) | 0.036 | |
| Bachelor’s degree | 295 (49.7%) | 1.49 (0.84–2.63) | 0.172 | 2.51 (0.99–6.31) | 0.051 | |
| Postgraduate studies | 24 (35.8%) | 1.77 (1.05–3.00) | 0.032 | 1.63 (0.55–4.71) | 0.380 | |
| Marital status | ||||||
| Single | 213 (45.1%) | 1 | 1 | |||
| Married | 193 (52.71%) | 1.36 (1.03–1.78) | 0.029 | 1.99 (1.43–2.77) | <0.001 | |
| Divorced | 8 (21.6%) | 0.34 (0.15–0.75) | 0.008 | 0.51 (0.21–1.27) | 0.147 | |
| Widow | 6 (37.5%) | 0.73 (0.26–2.04) | 0.548 | 1.08 (0.33–3.47) | 0.903 | |
| Residence | ||||||
| Taif | 258 (54.0%) | 1 | 1 | |||
| Makkah | 28 (43.8%) | 0.66 (0.39–1.12) | 0.126 | 0.75 (0.42–1.33) | 0.324 | |
| Jeddah | 86 (51.2%) | 0.89 (0.63–1.27) | 0.534 | 0.97 (0.65–1.44) | 0.867 | |
| Yanbu | 10 (30.3%) | 0.37 (0.17–0.80) | 0.011 | 0.72 (0.30–1.74) | 0.467 | |
| Madinah | 9 (20.0%) | 0.21 (0.10–0.45) | <0.001 | 0.36 (0.16–0.82) | 0.015 | |
| Other | 29 (28.2%) | 0.33 (0.21–0.53) | <0.001 | 0.37 (0.22–0.61) | <0.001 | |
| Monthly income | ||||||
| Less than 3000 SAR | 173 (45.3%) | 1 | ||||
| 3000 to 10,000 SAR | 120 (47.1%) | 1.07 (0.78–1.48) | 0.660 | |||
| More than 10,000 SAR | 127 (50.0%) | 1.21 (0.88–1.66) | 0.244 | |||
| Frequency of antibiotic use | ||||||
| 1–2 times | 203 (55.0%) | 1 | 1 | |||
| 3–5 times | 77 (37.2%) | 0.48 (0.34–0.69) | <0.001 | 0.52 (0.36–0.77) | 0.001 | |
| More than 5 times | 28 (23.0%) | 0.24 (0.15–0.39) | <0.001 | 0.26 (0.16–0.44) | <0.001 | |
| None | 112 (58.0%) | 1.13 (0.80–1.61) | 0.494 | 1.35 (0.92–1.99) | 0.125 | |
| Working in healthcare | ||||||
| Yes | 104 (56.5%) | 1 | 1 | |||
| No | 316 (44.7%) | 0.62 (0.45–0.86) | 0.004 | 0.58 (0.39–0.86) | 0.006 | |
| Source of information | ||||||
| The doctor | 239 (51.6%) | 1 | 1 | |||
| The pharmacist | 125 (46.5%) | 0.81 (0.60–1.10) | 0.179 | 0.77 (0.53–1.11) | 0.155 | |
| Internet | 46 (39.3%) | 0.61 (0.40–0.92) | 0.018 | 0.46 (0.28–0.74) | 0.001 | |
| Family or friends | 6 (26.1%) | 0.33 (0.13–0.85) | 0.022 | 0.58 (0.21–1.62) | 0.298 | |
| Media (TV, newspapers) | 4 (21.1%) | 0.25 (0.08–0.76) | 0.015 | 0.28 (0.09–0.89) | 0.033 | |
| Doctor counseling | ||||||
| Yes | 202 (41.6%) | 1 | 1 | |||
| No | 218 (53.8%) | 1.64 (1.26–2.14) | <0.001 | 1.89 (1.35–2.56) | <0.001 | |
| Pharmacist counseling | ||||||
| Yes | 302 (47.8%) | 1 | 1 | |||
| No | 118 (45.6%) | 0.91 (0.68–1.22) | 0.546 | 0.72 (0.50–1.04) | 0.078 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alruqayb, W.S.; Baali, F.H.; Althbiany, M.; Alharthi, A.; Alnefaie, S.; Alhaji, R.; Alshehri, R.; Khawagi, W.Y.; Alshahrani, M.A.; Arida, H.; et al. Determinants of Public Knowledge, Attitude, and Practice on Antibiotic Use in Saudi Arabia: A Regional Cross-Sectional Study. Healthcare 2025, 13, 1666. https://doi.org/10.3390/healthcare13141666
Alruqayb WS, Baali FH, Althbiany M, Alharthi A, Alnefaie S, Alhaji R, Alshehri R, Khawagi WY, Alshahrani MA, Arida H, et al. Determinants of Public Knowledge, Attitude, and Practice on Antibiotic Use in Saudi Arabia: A Regional Cross-Sectional Study. Healthcare. 2025; 13(14):1666. https://doi.org/10.3390/healthcare13141666
Chicago/Turabian StyleAlruqayb, Wadia S., Fahad H. Baali, Manar Althbiany, Alanoud Alharthi, Sara Alnefaie, Raghad Alhaji, Reem Alshehri, Wael Y. Khawagi, Monther A. Alshahrani, Hassan Arida, and et al. 2025. "Determinants of Public Knowledge, Attitude, and Practice on Antibiotic Use in Saudi Arabia: A Regional Cross-Sectional Study" Healthcare 13, no. 14: 1666. https://doi.org/10.3390/healthcare13141666
APA StyleAlruqayb, W. S., Baali, F. H., Althbiany, M., Alharthi, A., Alnefaie, S., Alhaji, R., Alshehri, R., Khawagi, W. Y., Alshahrani, M. A., Arida, H., & Alshehri, A. A. (2025). Determinants of Public Knowledge, Attitude, and Practice on Antibiotic Use in Saudi Arabia: A Regional Cross-Sectional Study. Healthcare, 13(14), 1666. https://doi.org/10.3390/healthcare13141666







