Prevalence and Determinants of Suicidal Ideation Among Physicians in Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Instrument
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Summers, R.F.; Gorrindo, T.; Hwang, S.; Aggarwal, R.; Guille, C. Well-being, burnout, and depression among North American psychiatrists: The state of our profession. Am. J. Psychiatry 2020, 177, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Ryan, E.; Hore, K.; Power, J.; Jackson, T. The relationship between physician burnout and depression, anxiety, suicidality and substance abuse: A mixed methods systematic review. Front. Public Health 2023, 11, 1133484. [Google Scholar] [CrossRef] [PubMed]
- Al-Humadi, S.; Bronson, B.; Muhlrad, S.; Paulus, M.; Hong, H.; Cáceda, R. Depression, suicidal thoughts, and burnout among physicians during the COVID-19 pandemic: A survey-based cross-sectional study. Acad. Psychiatry 2021, 45, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.S.; Bachu, R.; Adikey, A.; Malik, M.; Shah, M. Factors related to physician burnout and its consequences: A review. Behav. Sci. 2018, 8, 98. [Google Scholar] [CrossRef]
- Alomar, S.; Alosaimi, F.D.; Faden, M.; Alhaider, S.A.; Alsaywid, B.S.; Nakshabandi, Z.; Khamis, N. Towards a National System-Level Intervention: Characterization of Burnout Among Trainees of Saudi Postgraduate Healthcare Professions Programs. Healthcare 2025, 13, 473. [Google Scholar] [CrossRef]
- Fahrenkopf, A.M.; Sectish, T.C.; Barger, L.K.; Sharek, P.J.; Lewin, D.; Chiang, V.W.; Edwards, S.; Wiedermann, B.L.; Landrigan, C.P. Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ 2008, 336, 488–491. [Google Scholar] [CrossRef]
- Dong, M.; Zhou, F.C.; Xu, S.W.; Zhang, Q.; Ng, C.H.; Ungvari, G.S.; Xiang, Y.T. Prevalence of suicide-related behaviors among physicians: A systematic review and meta-analysis. Suicide Life-Threat. Behav. 2020, 50, 1264–1275. [Google Scholar] [CrossRef]
- Mata, D.A.; Ramos, M.A.; Bansal, N.; Khan, R.; Guille, C.; Di Angelantonio, E.; Sen, S. Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. JAMA 2015, 314, 2373–2383. [Google Scholar] [CrossRef]
- Ventriglio, A.; Watson, C.; Bhugra, D. Suicide among doctors: A narrative review. Indian J. Psychiatry 2020, 62, 114–120. [Google Scholar]
- Menon, N.K.; Shanafelt, T.D.; Sinsky, C.A.; Linzer, M.; Carlasare, L.; Brady, K.J.S.; Stillman, M.J.; Trockel, M.T. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw. Open 2020, 3, e2028780. [Google Scholar] [CrossRef]
- Klonsky, E.D.; May, A.M.; Saffer, B.Y. Suicide, suicide attempts, and suicidal ideation. Annu. Rev. Clin. Psychol. 2016, 12, 307–330. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, R.P. Theoretical Models of Suicide. In Ecological and Social Determinants of Suicidal Behavior; Springer: Singapore, 2025; pp. 1–46. [Google Scholar]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The hopelessness scale. J. Consult. Clin. Psychol. 1974, 42, 861. [Google Scholar] [CrossRef]
- Van Orden, K.A.; Witte, T.K.; Cukrowicz, K.C.; Braithwaite, S.R.; Selby, E.A.; Joiner, T.E., Jr. The interpersonal theory of suicide. Psychol. Rev. 2010, 117, 575. [Google Scholar] [CrossRef] [PubMed]
- Large, M.; Corderoy, A.; McHugh, C. Is suicidal behaviour a stronger predictor of later suicide than suicidal ideation? A systematic review and meta-analysis. Aust. N. Z. J. Psychiatry 2021, 55, 254–267. [Google Scholar] [CrossRef] [PubMed]
- Dutheil, F.; Aubert, C.; Pereira, B.; Dambrun, M.; Moustafa, F.; Mermillod, M.; Baker, J.S.; Trousselard, M.; Lesage, F.X.; Navel, V. Suicide among physicians and health-care workers: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0226361. [Google Scholar] [CrossRef]
- Khalil, M.A.; Khalifa, D.; Allam, R.M.; Abdalgeleel, S.A.; Khalaf, O.O. Suicide and depressive symptoms possible correlates among a sample of Egyptian physicians: Observational cross-sectional study (online survey). BMC Psychiatry 2024, 24, 408. [Google Scholar] [CrossRef]
- Iemmi, V.; Bantjes, J.; Coast, E.; Channer, K.; Leone, T.; McDaid, D.; Palfreyman, A.; Stephens, B.; Lund, C. Suicide and poverty in low-income and middle-income countries: A systematic review. Lancet Psychiatry 2016, 3, 774–783. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; Kazim, S.N.; Almufleh, A.S.; Aladwani, B.S.; Alsubaie, A.S. Prevalence of stress and its determinants among residents in Saudi Arabia. Saudi Med. J. 2015, 36, 605. [Google Scholar] [CrossRef]
- Altwaijri, Y.; Benjet, C.; Al-Habeeb, A.; Al-Subaie, A.; Akkad, M.; Alammar, S.; Bilal, L.; Naseem, T. Suicidal thoughts and behaviors in the Kingdom of Saudi Arabia. J. Affect. Disord. 2024, 352, 429–436. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; Alawad, H.S.; Alamri, A.K.; Saeed, A.I.; Aljuaydi, K.A.; Alotaibi, A.S.; Alotaibi, K.M.; Alfaris, E.A. Stress and coping among consultant physicians working in Saudi Arabia. Ann. Saudi Med. 2018, 38, 214–224. [Google Scholar] [CrossRef]
- Harvey, S.B.; Epstein, R.M.; Glozier, N.; Petrie, K.; Strudwick, J.; Gayed, A.; Dean, K.; Henderson, M. Mental illness and suicide among physicians. Lancet 2021, 398, 920–930. [Google Scholar] [CrossRef] [PubMed]
- Awaad, R.; Quadri, Y.; Suleiman, K.; Husain, A.; Hosseini, Z.; Rehman, O.; Elzamzamy, K.; Abdelrehim, A.; Rushdi, R.; Hill, T.; et al. Islam and suicide: An interdisciplinary scoping review. Spiritual. Clin. Pract. 2023, 10, 32. [Google Scholar] [CrossRef]
- Alosaimi, F.D.; AlAteeq, D.A.; Bin Hussain, S.I.; Alhenaki, R.S.; Bin Salamah, A.A.; AlModihesh, N.A. Public awareness, beliefs, and attitudes toward bipolar disorder in Saudi Arabia. Neuropsychiatr. Dis. Treat. 2019, 15, 2809–2818. [Google Scholar] [CrossRef]
- Carlisle, J. Mental health law in Saudi Arabia. BJPsych Int. 2018, 15, 17–19. [Google Scholar] [CrossRef] [PubMed]
- Chatterji, S. The Saudi National Mental Health Survey: Filling critical gaps in methodology and data in mental health epidemiology. Int. J. Methods Psychiatr. Res. 2020, 29, e1852. [Google Scholar] [CrossRef]
- Almadani, A.H.; Altheyab, E.S.; Alkheraiji, M.A.; Alfraiji, A.F.; Albrekkan, F.; Alkhamis, A.S.; AlBuqami, F.H.; Aljaffer, M.A. Perceptions and Attitudes of Mental Health Professionals toward the Mental Health Care Law in Saudi Arabia. Healthcare 2023, 11, 2784. [Google Scholar] [CrossRef] [PubMed]
- O’Carroll, P.W. Attempted suicide among young adults: Progress toward a meaningful estimate of prevalence. Am. J. Psychiatr. 1992, 149, 41. [Google Scholar]
- Jiraniramai, S.; Wongpakaran, T.; Angkurawaranon, C.; Jiraporncharoen, W.; Wongpakaran, N. Construct validity and differential item functioning of the PHQ-9 among health care workers: Rasch analysis approach. Neuropsychiatr. Dis. Treat. 2021, 17, 1035–1045. [Google Scholar] [CrossRef]
- Albougami, A. Resilient Coping Levels and Psychometric Properties of the Brief Resilient Coping Scale Among Nursing Professionals in Saudi Arabia. Healthcare 2024, 12, 2181. [Google Scholar] [CrossRef]
- Sharif, L.; Babhair, R.; Alzahrani, D.; Abuladel, A.; Kabli, A.; Alzahrani, R.; Alghamdi, L.; Mahsoon, A.; Sharif, K.; Alharazi, R.; et al. Unraveling the stigma: A qualitative descriptive exploration of the relationship between culture, religion, and mental disorders in Saudi Arabia. BMC Psychol. 2025, 13, 425. [Google Scholar] [CrossRef]
- Teoh, K.R.-H.; Dunning, A.; Taylor, A.K.; Gopfert, A.; Chew-Graham, C.A.; Spiers, J.; Appleby, L.; Van Hove, M.; Buszewicz, M.; Riley, R. Working conditions, psychological distress and suicidal ideation: Cross-sectional survey study of UK junior doctors. BJPsych Open 2024, 10, e14. [Google Scholar] [CrossRef]
- Hem, E.; Grønvold, N.; Aasland, O.G.; Ekeberg, Ø. The prevalence of suicidal ideation and suicidal attempts among Norwegian physicians. Results from a cross-sectional survey of a nationwide sample. Eur. Psychiatry 2000, 15, 183–189. [Google Scholar] [CrossRef]
- El-Haddad, Y. Major Trends Affecting Families in the Gulf Countries: 2003. Available online: https://www.un.org/esa/socdev/family/Publications/mtelhaddad.pdf (accessed on 1 January 2025).
- Zimmermann, C.; Strohmaier, S.; Herkner, H.; Niederkrotenthaler, T.; Schernhammer, E. Suicide rates among physicians compared with the general population in studies from 20 countries: Gender stratified systematic review and meta-analysis. BMJ 2024, 386, e078964. [Google Scholar] [CrossRef]
- Makhija, H.; Davidson, J.E.; Lee, K.C.; Barnes, A.; Choflet, A.; Zisook, S. National incidence of physician suicide and associated features. JAMA Psychiatry 2025, 82, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Causer, H.; Spiers, J.; Efstathiou, N.; Aston, S.; Chew-Graham, C.A.; Gopfert, A.; Grayling, K.; Maben, J.; van Hove, M.; Riley, R. The impact of colleague suicide and the current state of postvention guidance for affected co-workers: A critical integrative review. Int. J. Environ. Res. Public Health 2022, 19, 11565. [Google Scholar] [CrossRef] [PubMed]
- Ghozy, S.; Cross, W.M.; Islam, S.; Al-Mawali, A.H.; AlQurashi, A.A.; Hamza, A.; Joseph, B.; Banik, B.; Elsori, D.H.; Sultana, F.; et al. Psychological impact of COVID-19 on healthcare workers: Cross-sectional analyses from 14 countries. Glob. Ment. Health 2022, 9, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Shu, Z.; Chen, S.; Chen, H.; Chen, X.; Tang, H.; Zhou, J.; Tian, Y.; Wang, X.; Zhou, J. The effects of subjective family status and subjective school status on depression and suicidal ideation among adolescents: The role of anxiety and psychological resilience. PeerJ 2024, 12, e18225. [Google Scholar] [CrossRef]
- Abdel-Rahman, A.G.; Meky, F.; Halim, A.E.A.; Allam, M. Low job satisfaction among physicians in Egypt. TAF Prev. Med. Bull. 2008, 7, 91–96. [Google Scholar]
- Allebdi, A.A.; Ibrahim, H.M. Level and determinants of job satisfaction among Saudi physicians working in primary health-care facilities in Western Region, KSA. J. Fam. Med. Prim. Care 2020, 9, 4656–4661. [Google Scholar]
- Bondagji, D.; Fakeerh, M.; Alwafi, H.; Khan, A.A. The effects of long working hours on mental health among resident physicians in Saudi Arabia. Psychol. Res. Behav. Manag. 2022, 15, 1545–1557. [Google Scholar] [CrossRef]
- Lowry, R.; Crosby, A.E.; Brener, N.D.; Kann, L. Suicidal thoughts and attempts among US high school students: Trends and associated health-risk behaviors, 1991–2011. J. Adolesc. health 2014, 54, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Hwang, I.; Sampson, N.; Kessler, R.C.; Angermeyer, M.; Beautrais, A.; Borges, G.; Bromet, E.; Bruffaerts, R.; de Girolamo, G.; et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLoS Med. 2009, 6, e1000123. [Google Scholar] [CrossRef]
- Esfahani, M.; Hashemi, Y.; Alavi, K. Psychometric assessment of beck scale for suicidal ideation (BSSI) in general population in Tehran. Med. J. Islam. Repub. Iran 2015, 29, 268. [Google Scholar]
- van Spijker, B.A.J.; Batterham, P.J.; Calear, A.L.; Farrer, L.; Christensen, H.; Reynolds, J.; Kerkhof, A.J. The Suicidal Ideation Attributes Scale (SIDAS): Community-Based Validation Study of a New Scale for the Measurement of Suicidal Ideation. Suicide Life-Threat. Behav. 2014, 44, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Aldawsari, A.; Aldawsari, S.; Aldosari, H.; Alzahrani, M.Q.; Alzahrani, A.A.; Almalki, F.; Alzahrani, M.; Almutairi, B.M.; Alzahrani, N.; Alghamdi, S.M.; et al. Advancements Towards Better Mental Health in Saudi Arabia: A Narrative Review and Critical Analysis. J. Posit. Psychol. Wellbeing 2023, 7, 513–520. [Google Scholar]
- (SCFHS) SCfHS. DAEM. 2025. Available online: https://scfhs.org.sa/ar/training/daem (accessed on 1 January 2025).
| Characteristic | Total | Suicidal Ideation (in the Last Year) | p-Value | ||
|---|---|---|---|---|---|
| F (% of Total Participants) (n = 423) | Yes F (% of Participants) (n = 41) | No F (% of Participants) (n = 382) | |||
| Gender | Male | 302 (71.4%) | 26 (8.6%) | 276 (91.4%) | 0.234 |
| Female | 121 (28.6%) | 15 (12.4%) | 106 (87.6%) | ||
| Nationality | Saudi | 83 (19.7%) | 11 (13.3%) | 72 (86.7%) | 0.228 |
| Non-Saudi | 338 (80.3%) | 30 (8.9%) | 308 (91.1%) | ||
| Marital Status | Married | 372 (87.9%) | 35 (9.4%) | 337 (90.6%) | 0.594 |
| Not married | 51 (12.1%) | 6 (11.8%) | 45 (88.2%) | ||
| Have Children | Yes | 359 (92.5%) | 33 (9.2%) | 326 (90.8%) | 0.837 |
| No | 29 (7.5%) | 3 (10.3%) | 26 (89.7%) | ||
| Number of Children | 1–2 | 141 (39.3%) | 16 (11.3%) | 125 (88.7%) | 0.523 |
| 3–4 | 168 (46.8%) | 13 (7.7%) | 155 (92.3%) | ||
| ≥5 | 50 (13.9%) | 4 (8.0%) | 46 (92.0%) | ||
| Religion | Muslim | 396 (93.6%) | 41 (10.4%) | 355 (89.6%) | 0.094 |
| Non-Muslim | 27 (6.4%) | 0 (0.0%) | 27 (100.0%) | ||
| Income (Saudi Riyals) | Less than 20,000 | 231 (54.6%) | 29 (12.6%) | 202 (87.4%) | 0.029 |
| ≥20,000 | 192 (45.4%) | 12 (6.3%) | 180 (93.8%) | ||
| Age Group | <40 | 164 (39.0%) | 20 (12.2%) | 144 (87.8%) | 0.055 |
| 40–49 | 138 (32.8%) | 16 (11.6%) | 122 (88.4%) | ||
| ≥50 | 119 (28.3%) | 5 (4.2%) | 114 (95.8%) | ||
| Characteristic | Total | Suicidal Ideation (in the Last Year) | p-Value | ||
|---|---|---|---|---|---|
| F (% of Total Participants) | Yes F (% of Participants) | No F (% of Participants) | |||
| Average number of sleeping hours per day in the last year | ≤6 h | 315 (74.5%) | 32 (10.2%) | 283 (89.8%) | 0.589 |
| >6 h | 108 (25.5%) | 9 (8.3%) | 99 (91.7%) | ||
| In the last year, how much time do you spend on moderate-intensity aerobic physical activity per week? | <50 min/week | 251 (59.3%) | 28 (11.2%) | 223 (88.8%) | 0.219 |
| ≥50 min/week | 172 (40.7%) | 13 (7.6%) | 159 (92.4%) | ||
| Are you satisfied with your current income? | Satisfied or strongly satisfied | 203 (48.0%) | 17 (8.4%) | 186 (91.6%) | 0.466 |
| Not sure | 81 (19.1%) | 7 (8.6%) | 74 (91.4%) | ||
| Dissatisfied or very dissatisfied | 139 (32.9%) | 17 (12.2%) | 122 (87.8%) | ||
| Depression categories based on PHQ-9 score | Minimal to moderate depression | 332 (87.8%) | 28 (8.4%) | 304 (91.6%) | 0.005 |
| Moderately severe to severe depression | 46 (12.2%) | 10 (21.7%) | 36 (78.3%) | ||
| I have a history of major medical illness, including traumatic brain injury. | 3 (9.4%) | 29 (90.6%) | 0.950 | ||
| I have a current or past history of psychiatric illness. | 4 (18.2%) | 18 (81.8%) | 0.167 | ||
| I have received professional psychological help. | 2 (16.7%) | 10 (83.3%) | 0.840 | ||
| I have faced life stressors in the past year. | 31 (11.7%) | 233 (88.3%) | 0.066 | ||
| I have experienced childhood abuse, neglect, or parental separation. | 5 (12.8%) | 34 (87.2%) | 0.488 | ||
| I have access to guns, firearms, or other weapons. | 2 (15.4%) | 11 (84.6%) | 0.481 | ||
| I have been educated or trained in stress management and dealing with burnout phenomena among physicians. | 6 (6.8%) | 82 (93.2%) | 0.306 | ||
| I find it easy to access mental health treatment in my area. | 14 (8.6%) | 149 (91.4%) | 0.544 | ||
| Characteristic | Total | Suicidal Ideation (in the Last Year) | p-Value | ||
|---|---|---|---|---|---|
| F (% of Total Participants) | Yes F (% of Participants) | No F (% of Participants) | |||
| Region of practice | Central | 86 (20.3%) | 8 (9.3%) | 78 (90.7%) | 0.706 |
| Western | 76 (18.0%) | 10 (13.2%) | 66 (86.8%) | ||
| Eastern | 45 (10.6%) | 4 (8.9%) | 41 (91.1%) | ||
| Southern | 102 (24.1%) | 11 (10.8%) | 91 (89.2%) | ||
| Northern | 114 (27.0%) | 8 (7.0%) | 106 (93.0%) | ||
| Professional job title | General practitioner | 120 (30.2%) | 13 (10.8%) | 107 (89.2%) | 0.939 |
| Resident and trainee | 22 (5.5%) | 2 (9.1%) | 20 (90.9%) | ||
| Specialist or consultant | 256 (64.3%) | 25 (9.8%) | 231 (90.2%) | ||
| Medical specialty area | Medical | 271 (63.3%) | 26 (9.8%) | 240 (90.2%) | 0.714 |
| Surgical | 123 (28.7%) | 13 (10.6%) | 110 (89.4%) | ||
| Others (public health, dentistry, etc.) | 34 (7.9%) | 2 (5.9%) | 32 (94.1%) | ||
| Healthcare facility type | Public (government) | 406 (96.0%) | 38 (9.4%) | 368 (90.6%) | 0.234 |
| Private | 7 (1.7%) | 2 (28.6%) | 5 (71.4%) | ||
| Both | 10 (2.4%) | 1 (10.0%) | 9 (90.0%) | ||
| Monthly on-call shifts | None | 59 (13.9%) | 7 (11.9%) | 52 (88.1%) | 0.818 |
| 1–4 | 60 (14.2%) | 5 (8.3%) | 55 (91.7%) | ||
| 5–8 | 78 (18.4%) | 9 (11.5%) | 69 (88.5%) | ||
| >8 | 226 (53.4%) | 20 (8.8%) | 206 (91.2%) | ||
| Daily ward patient load | None | 66 (15.6%) | 3 (4.5%) | 63 (95.5%) | 0.477 |
| 1–10 | 107 (25.3%) | 11 (10.3%) | 96 (89.7%) | ||
| 11–20 | 86 (20.3%) | 10 (11.6%) | 76 (88.4%) | ||
| >20 | 164 (38.8%) | 17 (10.4%) | 147 (89.6%) | ||
| Weekly outpatient clinics | None | 51 (12.1%) | 5 (9.8%) | 46 (90.2%) | 0.797 |
| 1–4 | 66 (15.6%) | 6 (9.1%) | 60 (90.9%) | ||
| 5–8 | 43 (10.2%) | 6 (14.0%) | 37 (86.0%) | ||
| >8 | 263 (62.2%) | 24 (9.1%) | 239 (90.9%) | ||
| Do you agree that your work is stressful? | Agree or strongly agree | 309 (73.0%) | 37 (12.0%) | 272 (88.0%) | 0.024 |
| Not sure | 64 (15.1%) | 1 (1.6%) | 63 (98.4%) | ||
| Disagree or strongly disagree | 50 (11.8%) | 3 (6.0%) | 47 (94.0%) | ||
| During the last 12 months, have you regularly used any of the following: | None | 357 (86.7%) | 29 (8.1%) | 328 (91.9%) | 0.541 |
| Nicotine | 44 (10.7%) | 7 (15.9%) | 37 (84.1%) | ||
| Benzodiazepines | 1 (0.2%) | 0 (0.0%) | 1 (100.0%) | ||
| Analgesics | 5 (1.2%) | 0 (0.0%) | 5 (100.0%) | ||
| Stimulants | 4 (1.0%) | 0 (0.0%) | 4 (100.0%) | ||
| Opioids | 1 (0.2%) | 0 (0.0%) | 1 (100.0%) | ||
| Do you know a colleague (physician working in Saudi Arabia) who is seriously contemplating committing suicide in the future? | Yes | 11 (31.4%) | 24 (68.6%) | <0.001 | |
| No | 30 (7.7%) | 358 (92.3%) | |||
| Do you know a colleague (physician working in Saudi Arabia) who has attempted or died by suicide? | Yes | 8 (22.9%) | 27 (77.1%) | 0.006 | |
| No | 33 (8.5%) | 355 (91.5%) | |||
| Do you have plans for your future (career, family, finances, etc.)? | Yes | 30 (8.5%) | 323 (91.5%) | 0.062 | |
| No | 11 (15.7%) | 59 (84.3%) | |||
| Characteristic | Total | Suicidal Ideation (in the Last Year) | p-Value | ||
|---|---|---|---|---|---|
| F (% of Total Participants) | Yes F (% of Participants) | No F (% of Participants) | |||
| I look for creative ways to alter difficult situations. | Does not describe me at all | 48 (11.3%) | 8 (16.7%) | 40 (83.3%) | 0.344 |
| Does not describe me | 27 (6.4%) | 4 (14.8%) | 23 (85.2%) | ||
| Neutral | 161 (38.1%) | 12 (7.5%) | 149 (92.5%) | ||
| Describes me | 134 (31.7%) | 12 (9.0%) | 122 (91.0%) | ||
| Describes me very well | 53 (12.5%) | 5 (9.4%) | 48 (90.6%) | ||
| Regardless of what happens to me, I believe I can control my reaction to it. | Does not describe me at all | 25 (5.9%) | 3 (12.0%) | 22 (88.0%) | 0.418 |
| Does not describe me | 27 (6.4%) | 4 (14.8%) | 23 (85.2%) | ||
| Neutral | 149 (35.2%) | 18 (12.1%) | 131 (87.9%) | ||
| Describes me | 163 (38.5%) | 13 (8.0%) | 150 (92.0%) | ||
| Describes me very well | 59 (13.9%) | 3 (5.1%) | 56 (94.9%) | ||
| I believe that I can grow in positive ways by dealing with difficult situations. | Does not describe me at all | 25 (5.9%) | 4 (16.0%) | 21 (84.0%) | <0.001 |
| Does not describe me | 17 (4.0%) | 7 (41.2%) | 10 (58.8%) | ||
| Neutral | 135 (31.9%) | 16 (11.9%) | 119 (88.1%) | ||
| Describes me | 182 (43.0%) | 11 (6.0%) | 171 (94.0%) | ||
| Describes me very well | 64 (15.1%) | 3 (4.7%) | 61 (95.3%) | ||
| I actively look for ways to replace the losses I encounter in life. | Does not describe me at all | 25 (5.9%) | 4 (16.0%) | 21 (84.0%) | 0.045 |
| Does not describe me | 20 (4.7%) | 4 (20.0%) | 16 (80.0%) | ||
| Neutral | 146 (34.5%) | 19 (13.0%) | 127 (87.0%) | ||
| Describes me | 181 (42.8%) | 12 (6.6%) | 169 (93.4%) | ||
| Describes me very well | 51 (12.1%) | 2 (3.9%) | 49 (96.1%) | ||
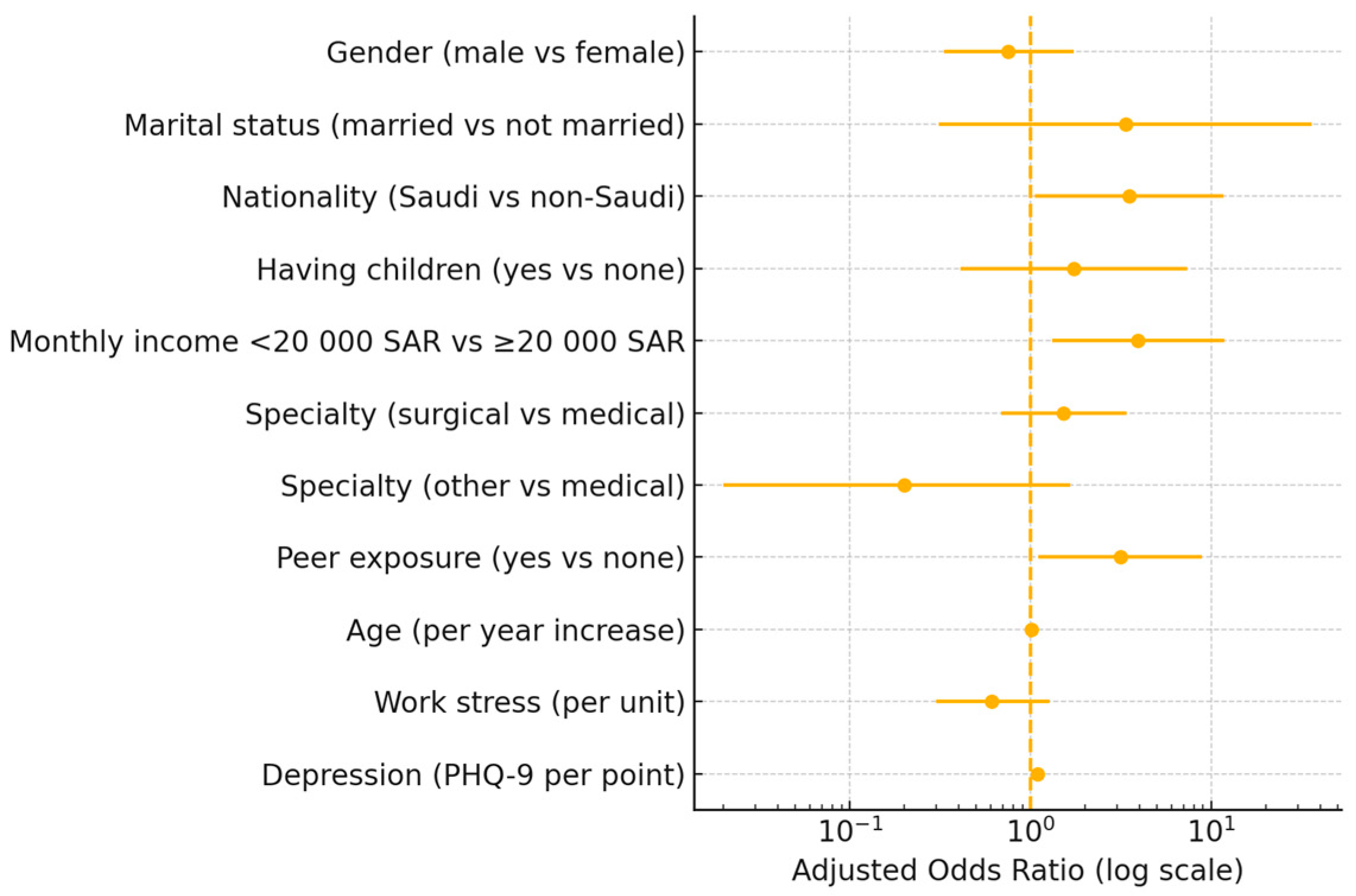
| Predictor | Reference Category | OR (95% CI) * | p-Value |
|---|---|---|---|
| Gender (male) | Female | 0.75 (0.33–1.73) | 0.501 |
| Marital status (married) | Not married | 3.36 (0.31–35.97) | 0.316 |
| Nationality (Saudi) | Non-Saudi | 3.50 (1.05–11.73) | 0.042 |
| Having children (yes) | No children | 1.73 (0.41–7.38) | 0.457 |
| Monthly income < SAR 20,000 * | ≥SAR 20,000 | 3.94 (1.32–11.76) | 0.014 |
| Specialty (surgical) | Medical | 1.52 (0.69–3.38) | 0.300 |
| Specialty (other) | Medical | 0.20 (0.02–1.66) | 0.134 |
| Peer exposure to suicidal ideation (yes) | No exposure | 3.13 (1.10–8.88) | 0.032 |
| Age (per year increase) | — | 1.01 (0.97–1.06) | 0.559 |
| Perceived work stress (per unit) | — | 0.61 (0.30–1.28) | 0.193 |
| Depression score (PHQ-9 per point) | — | 1.09 (1.02–1.16) | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alghamdi, A.H.; Aljaffer, M.A.; Almadani, A.H.; Alghamdi, S.A.; Alshehri, H.R.; Alyateem, A.A.; Hashim, R.T.; Alosaimi, F.D. Prevalence and Determinants of Suicidal Ideation Among Physicians in Saudi Arabia. Healthcare 2025, 13, 1632. https://doi.org/10.3390/healthcare13131632
Alghamdi AH, Aljaffer MA, Almadani AH, Alghamdi SA, Alshehri HR, Alyateem AA, Hashim RT, Alosaimi FD. Prevalence and Determinants of Suicidal Ideation Among Physicians in Saudi Arabia. Healthcare. 2025; 13(13):1632. https://doi.org/10.3390/healthcare13131632
Chicago/Turabian StyleAlghamdi, Ayedh H., Mohammed A. Aljaffer, Ahmad H. Almadani, Saleh A. Alghamdi, Hasan R. Alshehri, Akeel A. Alyateem, Refan T. Hashim, and Fahad D. Alosaimi. 2025. "Prevalence and Determinants of Suicidal Ideation Among Physicians in Saudi Arabia" Healthcare 13, no. 13: 1632. https://doi.org/10.3390/healthcare13131632
APA StyleAlghamdi, A. H., Aljaffer, M. A., Almadani, A. H., Alghamdi, S. A., Alshehri, H. R., Alyateem, A. A., Hashim, R. T., & Alosaimi, F. D. (2025). Prevalence and Determinants of Suicidal Ideation Among Physicians in Saudi Arabia. Healthcare, 13(13), 1632. https://doi.org/10.3390/healthcare13131632





