The Determinants of Coexisting Anemia and Undernutrition Among Pregnant Women in Southern Ethiopia: A Multi-Level Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Study Design, Period, Population and Sample Size
2.3. Study Variables
2.4. Data Collection Tools and Techniques
2.5. Blood Collection and Serum Preparation Procedures
2.6. Data Quality Assurance
2.7. Ethics Statement
2.8. Data Analysis Techniques
3. Results
3.1. Socio-Demographic Characteristics of Research Subjects
3.2. Study Participants’ Reproductive Health Characteristics
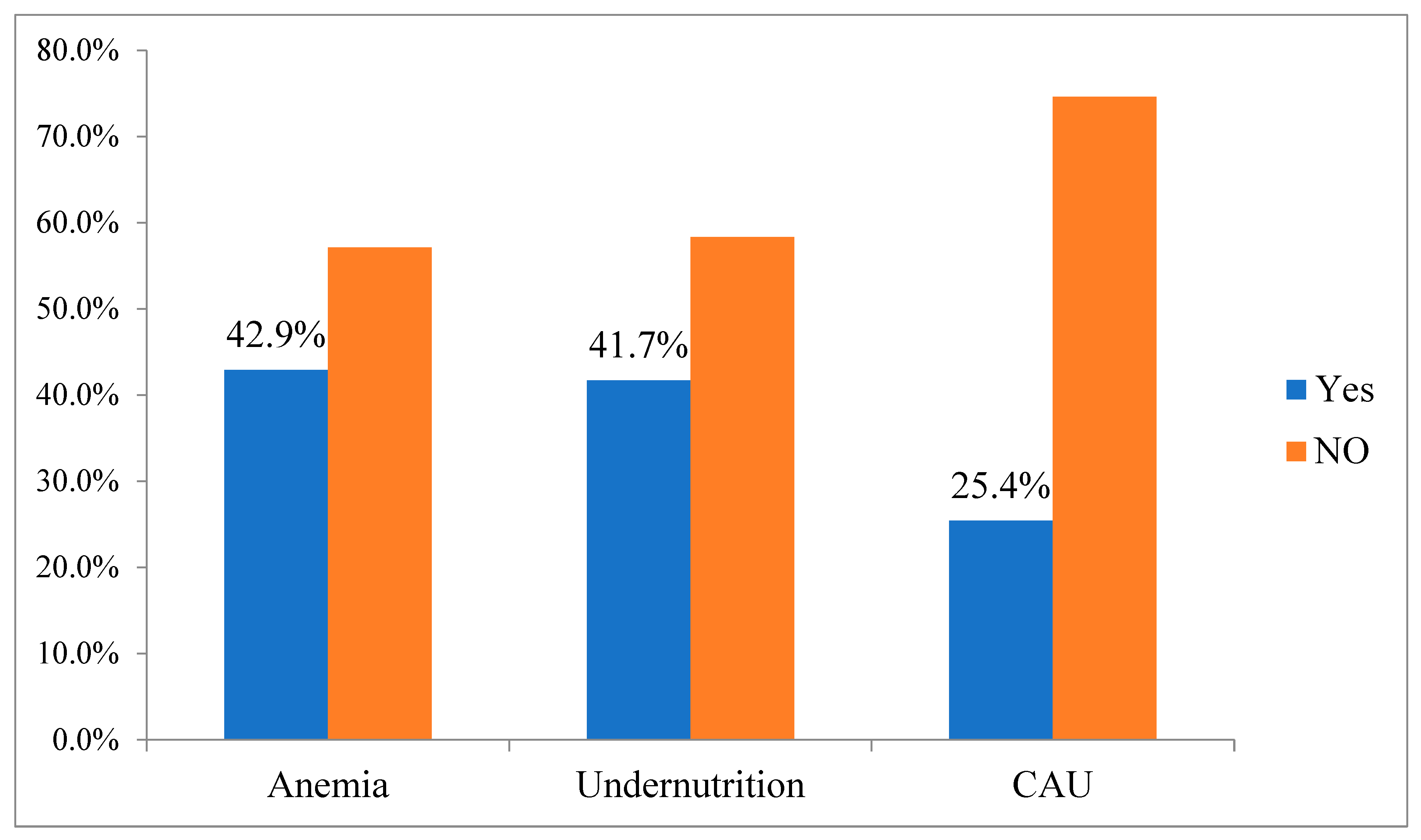
3.3. Prevalence of Coexisting Anemia and Undernutrition
3.4. Determinants of Coexisting Anemia and Undernutrition
3.5. Random Effect Model and Model Fitness Information on CAU Prevalence
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AIC | Akaike information criteria |
| APR | Adjusted prevalence ratio; |
| BIC | Bayesian information criteria |
| CI | Confidence interval; |
| CPR | Crude prevalence ratio |
| EDHS | Ethiopian Demographic and Health Survey |
| FANTA | Food and nutrition technical assistance |
| FAO | Food and agriculture organization |
| HCPs | Health Care Providers |
| HEW | Health extension worker |
| ICC | Intra-class correlation coefficient |
| IRB | Institutional review board |
| IUGR | Intrauterine growth retardation |
| MPR | Median prevalence ratio |
| NGO | Non-governmental organization |
| PI | Principal Investigator |
| SD | Standard deviation |
| VIF | Variance inflation factor |
| WHO | World Health Organization |
| WRA | Women of reproductive age |
References
- Ververs, M.-T.; Antierens, A.; Sackl, A.; Staderini, N.; Captier, V. Which anthropometric indicators identify a pregnant woman as acutely malnourished and predict adverse birth outcomes in the humanitarian context? PLoS Curr. 2013, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.M.; Dong, K.; Deitchler, M.; Chung, M.; Maalouf-Manasseh, Z.; Tumilowicz, A.; Wanke, C. Use of Cutoffs for Mid-Upper Arm Circumference (MUAC) as an Indicator or Predictor of Nutritional and Health-Related Outcomes in Adolescents and Adults: A Systematic Review; FHI: Washington, DC, USA, 2013; p. 360. [Google Scholar]
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; WHO: Geneva, Switzerland, 2011.
- World Health Organization. World Health Organization (2021) Anemia in Women and Children. Available online: https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children (accessed on 3 May 2025).
- CSA I. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF. 2016. Available online: https://dhsprogram.com/pubs/pdf/fr328/fr328.pdf (accessed on 21 June 2025).
- Derso, T.; Abera, Z.; Tariku, A. Magnitude and associated factors of anemia among pregnant women in Dera District: A cross-sectional study in northwest Ethiopia. BMC Res. Notes 2017, 10, 359. [Google Scholar] [CrossRef] [PubMed]
- Hemming, K.; Eldridge, S.; Forbes, G.; Weijer, C.; Taljaard, M. How to design efficient cluster randomised trials. BMJ 2017, 358, j3064. [Google Scholar] [CrossRef] [PubMed]
- Hussein, K.L.; Mogren, I.; Lindmark, G.; Massawe, S.; Nystrom, L. Risks for preterm delivery and low birth weight are independently increased by severity of maternal anaemia. S. Afr. Med. J. 2009, 99, 98–102. [Google Scholar] [PubMed]
- Moench-Pfanner, R.; Silo, S.; Laillou, A.; Wieringa, F.; Hong, R.; Hong, R.; Poirot, E.; Bagriansky, J. The Economic Burden of Malnutrition in Pregnant Women and Children under 5 Years of Age in Cambodia. Nutrients 2016, 8, 292. [Google Scholar] [CrossRef]
- World Health Organization. Nutritional Anaemias: Tools for Effective Prevention and Control Geneva: World Health Organization. 2017. Available online: https://apps.who.int/iris/handle/10665/259425 (accessed on 3 May 2025).
- Ruel, M.T.; Alderman, H. Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet 2013, 382, 536–551. [Google Scholar] [CrossRef] [PubMed]
- MoFED Health Sector Growth and Transformation Plan (GTP), The Federal Democratic Republic of Ethiopia. 2010. Available online: https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/ethiopia/ethiopia_gtp_2010-2015.pdf (accessed on 3 May 2025).
- Federal Democratic Republic of Ethiopia, National Nutrition Program Multi-sectoral Implementation Guide. Addis Ababa: 2016. Available online: https://scalingupnutrition.org/sites/default/files/2022-06/national-multi-stakeholder-platform-ethiopia.pdf (accessed on 3 May 2025).
- Dessalegn, F.N.; Wanamo, T.E.; Wordofa, D. Prevalence of Iron Deficiency Anemia and Associated Factors among Pregnant Women Attending Antenatal Care Follow-up at Dodola General Hospital, West Arsi Zone, Oromia Region, South East Ethiopia. Arch. Med. 2021, 13, 40. Available online: https://www.itmedicalteam.pl/articles/prevalence-of-iron-deficiency-anemia-and-associated-factors-among-pregnant-women-attending-antenatal-care-follow-up-at-dodola-gene.pdf (accessed on 3 May 2025).
- Laelago, F.; Paulos, W.; Halala Handiso, Y. Prevalence and predictors of iron deficiency anemia among pregnant women in Bolosso Bomibe district, Wolaita Zone, Southern Ethiopia Community-based cross-sectional study. Cogent Public Health 2023, 10, 2183562. [Google Scholar] [CrossRef]
- Woldegebriel, A.G.; Gebrehiwot, G.G.; Desta, A.A.; Ajemu, K.F.; Berhe, A.A.; Woldearegay, T.W.; Bezabih, N.M. Determinants of Anemia in Pregnancy: Findings from the Ethiopian Health and Demographic Survey. Anemia 2020, 2020, 2902498. [Google Scholar] [CrossRef]
- Patel, A.; Prakash, A.A.; Das, P.K.; Gupta, S.; Pusdekar, Y.V.; Hibberd, P.L. Maternal anemia and underweight as determinants of pregnancy outcomes: Cohort study in eastern rural Maharashtra, India. BMJ Open 2018, 8, e021623. [Google Scholar] [CrossRef]
- Deriba, B.S.; Bala, E.T.; Bulto, G.A.; Geleta, T.A.; Ayalew, A.F.; Gebru, A.A.; Desta, H.O.; Shiferaew, M.B.; Sahile, L.Z. Determinants of Anemia among Pregnant Women at Public Hospitals in West Shewa, Central Ethiopia: A Case-Control Study. Anemia 2020, 2020, 2865734. [Google Scholar] [CrossRef]
- Alene, K.A.; Dohe, A.M. Prevalence of Anemia and Associated Factors among Pregnant Women in an Urban Area of Eastern Ethiopia. Anemia 2014, 2014, 561567. [Google Scholar] [CrossRef]
- Bekele, A.; Tilahun, M.; Mekuria, A. Prevalence of Anemia and Its Associated Factors among Pregnant Women Attending Antenatal Care in Health Institutions of Arba Minch Town, Gamo Gofa Zone, Ethiopia: A Cross-Sectional Study. Anemia 2016, 2016, 1073192. [Google Scholar] [CrossRef] [PubMed]
- Teshome, M.S.; Meskel, D.H.; Wondafrash, B. Determinants of Anemia Among Pregnant Women Attending Antenatal Care Clinic at Public Health Facilities in Kacha Birra District, Southern Ethiopia. J. Multidiscip. Healthc. 2020, 13, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Lesage, J.; Hahn, D.; Leonhardt, M.; Blondeau, B.; Breant, B.; Dupouy, J.P. Maternal undernutrition during late gestation-induced intrauterine growth restriction in the rat is associated with impaired placental GLUT3 expression, but does not correlate with endogenous corticosterone levels. J. Endocrinol. 2002, 174, 37–43. [Google Scholar] [CrossRef]
- Muze, M.; Yesse, M.; Kedir, S.; Mustefa, A. Prevalence and associated factors of undernutrition among pregnant women visiting ANC clinics in Silte zone, Southern Ethiopia. BMC Pregnancy Childbirth 2020, 20, 707. [Google Scholar] [CrossRef] [PubMed]
- Nigatu, M.; Gebrehiwot, T.T.; Gemeda, D.H. Household food insecurity, low dietary diversity, and early marriage were predictors for undernutrition among pregnant women residing in Gambella, Ethiopia. Adv. Public Health. 2018, 2018, 1350195. [Google Scholar] [CrossRef]
- Shiferaw, A.; Husein, G. Acute Under Nutrition and Associated Factors among Pregnant Women in Gumay District, Jimma Zone, South West Ethiopia. J. Women’s Health Care 2019, 8, 459. [Google Scholar] [CrossRef]
- Tadesse, A.; Hailu, D.; Bosha, T. Nutritional status and associated factors among pastoralist children aged 6–23 months in Benna Tsemay Woreda, South Omo Zone, Southern Ethiopia. Int. J. Nutr. Food Sci. 2017, 7, 11–23. [Google Scholar] [CrossRef]
- Tikuye, H.H.; Gebremedhin, S.; Mesfin, A.; Whiting, S. Prevalence and Factors Associated with Undernutrition among Exclusively Breastfeeding Women in Arba Minch Zuria District, Southern Ethiopia: A Cross-sectional Community-Based Study. Ethiop. J. Health Sci. 2019, 29, 913–922. [Google Scholar] [CrossRef]
- Zewdie, S.; Fage, S.G.; Tura, A.K.; Weldegebreal, F. Undernutrition among Pregnant Women in Rural Communities in Southern Ethiopia. Int. J. Womens Health. 2021, 13, 73–79. [Google Scholar] [CrossRef]
- Donner, A.; Birkett, N.; Buck, C. Randomization by cluster. Sample size requirements and analysis. Am. J. Epidemiol. 1981, 114, 906–914. [Google Scholar] [CrossRef]
- Federal Ministry of Health [Ethiopia]. National Guideline for Family Planning Services in Ethiopia; FMoH: Addis Ababa, Ethiopia, 2011.
- Federal Democratic Republic of Ethiopia Ministry of Health. Federal Democratic Republic of Ethiopia Ministry of Health. National Nutrition Program: 2016–2020; FMoH: Addis Ababa, Ethiopia, 2016. Available online: https://www.moh.gov.et (accessed on 3 May 2025).
- Federal Ministry of Health [Ethiopia]. Community-Based Nutrition Program Training Manual for Health Extension Workers; FMoH: Addis Ababa, Ethiopia, 2013.
- Federal Ministry of Health (FMoH), Ethiopia. Health Extension Program in Ethiopia: Profile; FMoH: Addis Ababa, Ethiopia, 2010.
- Teklehaimanot, H.D.; Teklehaimanot, A. Human resource development for a community-based health extension program: A case study from Ethiopia. Hum. Resour. Health 2013, 11, 1–12. [Google Scholar] [CrossRef]
- Banteyerga, H. Ethiopia’s health extension program: Improving health through community involvement. MEDICC Rev. 2011, 13, 46–49. [Google Scholar] [CrossRef]
- Demilew, Y.M.; Alene, G.D.; Belachew, T. Dietary practices and associated factors among pregnant women in West Gojjam Zone, Northwest Ethiopia. BMC Pregnancy Childbirth 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Abute, L.; Beyamo, A.; Erchafo, B.; Tadesse, T.; Sulamo, D.; Sadoro, T. Dietary Practice and Associated Factors among Pregnant Women in Misha Woreda, South Ethiopia: A Community-Based Cross-Sectional Study. J. Nutr. Metab. 2020, 2020, 5091318. [Google Scholar] [CrossRef] [PubMed]
- Alem, M.; Enawgaw, B.; Gelaw, A.; Kena, T.; Seid, M.; Olkeba, Y. Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Azezo Health Center Gondar town, Northwest Ethiopia. J. Interdiscipl Histopathol. 2013, 1, 137–144. [Google Scholar] [CrossRef]
- Getachew, M.; Yewhalaw, D.; Tafess, K.; Getachew, Y.; Zeynudin, A. Anaemia and associated risk factors among pregnant women in Gilgel Gibe dam area, Southwest Ethiopia. Parasit Vectors 2012, 5, 296. [Google Scholar] [CrossRef]
- World Health Organization. Improving Nutrition Outcomes with Better Water, Sanitation and Hygiene: Practical Solutions for Policies and Programmes. 2015. Available online: https://www.who.int/publications/i/item/9789241565103 (accessed on 3 May 2025).
- Bull, B.S.; National Committee for Clinical Laboratory Standards. Reference and Selected Procedures for the Quantitative Determination of Hemoglobin in Blood: Approved Standard, 2nd ed.; National Committee for Clinical Laboratory Standards: Villanova, PA, USA, 1994. [Google Scholar]
- Gwatkin, D.R.; Gwatkin, D.R. Health inequalities and the health of the poor: What do we know? What can we do? Bull. World Health Organ. 2000, 78, 3–18. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC2560590/pdf/10686729.pdf (accessed on 3 May 2025). [PubMed]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007. [Google Scholar]
- Kleiman, E. Understanding and Analyzing Multilevel Data from Real-Time Monitoring Studies: An Easily-Accessible Tutorial Using R. 2017. Available online: https://osf.io/preprints/psyarxiv/xf2pw_v1 (accessed on 3 May 2025).
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression; Wiley: New York, NY, USA, 2000. [Google Scholar]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163, Erratum in J. Chiropr. Med. 2017, 16, 346. [Google Scholar] [CrossRef]
- Lee, S.E.; Talegawkar, S.A.; Merialdi, M.; Caulfield, L.E. Dietary intakes of women during pregnancy in low- and middle-income countries. Public Health Nutr. 2013, 16, 1340–1353. [Google Scholar] [CrossRef] [PubMed]
- Adem, H.A.; Usso, A.A.; Hebo, H.J.; Workicho, A.; Ahmed, F. Determinants of acute undernutrition among pregnant women attending primary healthcare unit in Chinaksen District, Eastern Ethiopia: A case-control study. PeerJ 2023, 11, e15416. [Google Scholar] [CrossRef]
- World Health Organization. Nutrition in Adolescence–Issues and Challenges for the Health Sector. Available online: https://iris.who.int/bitstream/handle/10665/43342/92;jsessionid=268FA3727B4187B66A6232E6FC093BD5?sequence=1 (accessed on 20 August 2024).
- Sserwanja, Q.; Mutisya, L.M.; Musaba, M.W. Exposure to different types of mass media and timing of antenatal care initiation: Insights from the 2016 Uganda Demographic and Health Survey. BMC Womens Health. 2022, 22, 10. [Google Scholar] [CrossRef]
- Shah, N.; Zaheer, S.; Safdar, N.F.; Turk, T.; Hashmi, S. Women’s awareness, knowledge, attitudes, and behaviours towards nutrition and health in Pakistan: Evaluation of kitchen gardens nutrition program. PLoS ONE 2023, 18, e0291245. [Google Scholar] [CrossRef]
- Masters, W.A.; Eggersdorfer, M.; Cordaro, J.; Fanzo, J.; Gibney, M.; Kennedy, E.; Labrique, A.; Steffen, J. The Economic Causes of Malnutrition. In Good Nutrition: Perspectives for the 21st Century; Karger Publishers: Basel, Switzerland, 2016; pp. 92–104. [Google Scholar]
- Ver Ploeg, M.; Breneman, V.; Dutko, P.; Williams, R.; Snyder, S.; Dicken, C.; Kaufman, P. Access to Affordable and Nutritious Food: Updated Estimates of Distance to Supermarkets Using 2010 Data; Economic Research Report No. 262227; United States Department of Agriculture, Economic Research Service: Washington, DC, USA, 2012. [CrossRef]
- French, S.A.; Tangney, C.C.; Crane, M.M.; Wang, Y.; Appelhans, B.M. Nutrition quality of food purchases varies by household income: The SHoPPER study. BMC Public Health. 2019, 19, 231. [Google Scholar] [CrossRef] [PubMed]
- Zegeye, K.; Gebeyehu, A.; Melese, T. The role of geographical access in the Utilization of institutional delivery service in rural Jimma Horro District, Southwest Ethiopia. Prim Health Care 2014, 4, 2167-1079. [Google Scholar]
- Ahmed, R.; Sultan, M.; Abose, S.; Assefa, B.; Nuramo, A.; Alemu, A.; Demelash, M.; Eanga, S.; Mosa, H. Levels and associated factors of the maternal healthcare continuum in Hadiya zone, Southern Ethiopia: A multilevel analysis. PLoS ONE 2022, 17, e0275752. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Singh, K.K.; Singh, P. Maternal health care service utilization among young married women in India, 1992–2016: Trends and determinants. BMC Pregnancy Childbirth 2021, 21, 122. [Google Scholar] [CrossRef]
- Fatema, K. Impact of Mass Media on the Utilization of Maternal Healthcare Services in South Asia. Available online: https://digitalcommons.memphis.edu/etd/2031/ (accessed on 3 May 2025).
- Yoseph, A.; Teklesilasie, W.; Guillen-Grima, F.; Astatkie, A. Individual-and community-level determinants of maternal health service utilization in southern Ethiopia: A multilevel analysis. Women’s Health 2023, 19, 17455057231218195. [Google Scholar] [CrossRef]
- Shudura, E.; Yoseph, A.; Tamiso, A. Utilization and predictors of maternal health care services among women of reproductive age in Hawassa University Health and Demographic Surveillance System Site, South Ethiopia: A cross-sectional study. Adv. Public Health 2020, 2020, 5865928. [Google Scholar] [CrossRef]
- Asefa, A.; Gebremedhin, S.; Messele, T.; Letamo, Y.; Shibru, E.; Alano, A.; Morgan, A.; Kermode, M. Mismatch between antenatal care attendance and institutional delivery in south Ethiopia: A multilevel analysis. BMJ Open 2019, 9, e024783. [Google Scholar] [CrossRef]
- Kennedy, G.; Ballard, T.; Dop, M. Guidelines for Measuring Household and Individual Dietary Diversity. FAO. 2011. Available online: https://openknowledge.fao.org/server/api/core/bitstreams/86ee19ca-4fab-4547-b837-44cf2a7d6927/content (accessed on 3 May 2025).
- Castell, G.S.; Rodrigo, C.P.; de la Cruz, J.N.; Bartrina, J.A. Household food insecurity access scale (HFIAS). Nutr. Hosp. 2015, 31, 272–278. [Google Scholar]
- Negash, W.D.; Fetene, S.M.; Shewarega, E.S.; Fentie, E.A.; Asmamaw, D.B.; Teklu, R.E.; Aragaw, F.M.; Belay, D.G.; Alemu, T.G.; Eshetu, H.B. Multilevel analysis of quality of antenatal care and associated factors among pregnant women in Ethiopia: A community based cross-sectional study. BMJ Open 2022, 12, e063426. [Google Scholar] [CrossRef] [PubMed]
- Huda, T.M.; Chowdhury, M.; El Arifeen, S.; Dibley, M.J. Individual and community level factors associated with health facility delivery: A cross sectional multilevel analysis in Bangladesh. PLoS ONE 2019, 14, e0211113. [Google Scholar] [CrossRef] [PubMed]
- Liyew, A.M.; Teshale, A.B. Individual and community level factors associated with anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health survey, 2016; a multilevel analysis. BMC Public Health 2020, 20, 775. [Google Scholar] [CrossRef]
- Tessema, Z.T.; Animut, Y. Spatial distribution and determinants of an optimal ANC visit among pregnant women in Ethiopia: Further analysis of 2016 Ethiopia demographic health survey. BMC Pregnancy Childbirth 2020, 20, 137. [Google Scholar] [CrossRef]
- Yoseph, A.; Teklesilasie, W.; Guillen-Grima, F.; Astatkie, A. Effect of community health education on mothers’ knowledge of obstetric danger signs and birth preparedness and complication readiness practices in southern Ethiopia: A cluster randomized controlled trial. PLoS ONE 2024, 19, e0312267. [Google Scholar] [CrossRef]
- Yoseph, A.; Teklesilasie, W.; Guillen-Grima, F.; Astatkie, A. Community-based health education led by women’s groups significantly improved maternal health service utilization in Southern Ethiopia: A cluster randomized controlled trial. Healthcare 2024, 12, 1045. [Google Scholar] [CrossRef]
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef]
- Fry, K.; Firestone, R.; Chakraborty, N.M. Measuring Equity with Nationally Representative Wealth Quintiles; psi: Washington, DC, USA, 2014; Available online: https://media.psi.org/wp-content/uploads/2020/02/31012157/Wealth-Quintile-Guide.pdf (accessed on 3 May 2025).
- Manaloor, V.A.; Radhakrishnan, K.; Raghu, P.T.; Nambi, V.A. Measuring the economic status of different caste groups in rural India: An application of principal component analysis. Indian J. Econ. Dev. 2021, 9, 1–9. [Google Scholar] [CrossRef]
- Sartipi, M.; Nedjat, S.; Mansournia, M.A.; Baigi, V.; Fotouhi, A. Assets as a socioeconomic status index: Categorical principal components analysis vs. latent class analysis. Arch. Iran. Med. 2016, 19, 791–796. [Google Scholar] [PubMed]
- Zhang, Z.; Sangsawang, T.; Vipahasna, K.; Pigultong, M. A mixed-methods data approach integrating importance-performance analysis (IPA) and Kaiser-Meyer-Olkin (KMO) in applied talent cultivation. J. Appl. Data Sci. 2024, 5, 256–267. [Google Scholar]

| Variables | Coexisting Anemia and Undernutrition | CPR (95% CI) | APR (95% CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Individual-level determinants | ||||
| Women’s education | ||||
| Have formal education | 80 (23.2) | 265 (76.8) | Ref | Ref |
| No formal education | 51 (30.0) | 119 (70.0) | 1.14 (0.85, 1.54) | 0.87 (0.75, 1.01) |
| Family size | ||||
| Small | 97 (23.9) | 309 (76.1) | Ref | Ref |
| Large | 34 (31.2) | 75 (68.8) | 1.12 (0.83, 1.50) | 0.92 (0.64, 1.31) |
| Women’s occupation status | ||||
| Housewife | 113 (24.4) | 350 (75.4) | Ref | |
| Merchant | 11 (36.7) | 19 (63.3) | 0.99 (0.55, 1.77) | 0.98 (0.59, 1.62) |
| Government employee | 7 (31.8) | 15 (68.2) | 0.73 (0.19, 2.78) | 0.78 (0.31, 1.95) |
| Decision-making power of women | ||||
| Autonomous | 66 (20.9) | 250 (79.1) | Ref | Ref |
| Non-autonomous | 65 (32.7) | 134 (67.3) | 2.26 (0.89, 5.78) | 1.37 (0.41, 4.54) |
| Model family training | ||||
| Not obtained | 45 (29.8) | 106 (70.2) | Ref | Ref |
| Obtained | 86 (23.6) | 278 (76.4) | 0.63 (0.37, 1.06) | 0.66 (0.45, 0.96) * |
| Food security status | ||||
| Secure households | 46 (14.4) | 274 (85.6) | Ref | Ref |
| Insecure households | 85 (43.6) | 110 (56.4) | 2.89 (1.50, 5.57) | 2.17 (1.43, 3.28) ** |
| Dietary diversity status | ||||
| Adequate | 39 (15.9) | 206 (84.1) | Ref | Ref |
| Inadequate | 92 (34.1) | 178 (65.9) | 1.91 (1.50, 2.42) | 1.51 (1.18, 1.95) ** |
| Women’s knowledge about nutrition | ||||
| Good | 36 (13.6) | 228 (86.4) | Ref | Ref |
| Poor | 95 (37.8) | 156 (62.2) | 2.40 (1.59, 3.61) | 1.55 (1.06, 2.26) * |
| Food security status | ||||
| Secure households | 46 (14.4) | 274 (85.6) | Ref | Ref |
| Insecure households | 85 (43.6) | 110 (56.4) | 2.89 (1.50, 5.57) | 2.17 (1.43, 3.28) ** |
| Dietary diversity status | ||||
| Adequate | 39 (15.9) | 206 (84.1) | Ref | Ref |
| Inadequate | 92 (34.1) | 178 (65.9) | 1.91 (1.50, 2.42) | 1.51 (1.18, 1.95) ** |
| Women’s knowledge about nutrition | ||||
| Good | 36 (13.6) | 228 (86.4) | Ref | Ref |
| Poor | 95 (37.8) | 156 (62.2) | 2.40 (1.59, 3.61) | 1.55 (1.06, 2.26) * |
| Women’s attitude towards nutrition | ||||
| Positive | 92 (26.7) | 252 (73.3) | Ref | Ref |
| Negative | 39 (22.8) | 132 (77.2) | 0.87 (0.50, 1.52) | 0.78 (0.30, 2.01) |
| Community-level determinants | ||||
| Place of residence | ||||
| Urban | 10 (11.0) | 81 (89.0) | Ref | Ref |
| Rural | 121 (28.5) | 303 (71.5) | 3.13 (0.36, 26.95) | 3.53 (0.33, 37.40) |
| Community-level wealth status | ||||
| High | 50 (16.4) | 255 (83.6) | Ref | Ref |
| Low | 81 (38.6) | 129 (61.4) | 1. 68 (0.67, 4.17) | 1.25 (0.76, 2.06) |
| Community-level distance | ||||
| Not big problem | 77 (23.6) | 249 (76.4) | Ref | Ref |
| Big problem | 54 (28.6) | 135 (71.4) | 0.96 (0.45, 2.06) | 0.78 (0.30, 2.02) |
| Community-level literacy | ||||
| High | 13 (8.8) | 134 (91.2) | Ref | Ref |
| Low | 118 (32.1) | 250 (67.9) | 4.28 (0.83, 21.98) | 2.16 (0.49, 9.54) |
| Community-level road access | ||||
| Inaccessible | 18 (36.0) | 32 (64.0) | Ref | Ref |
| Accessible | 113 (24.3) | 352 (75.7) | 0.73 (0.45, 1.17) | 0.65 (0.43, 0.98) * |
| Community-level autonomy | ||||
| High | 16 (8.2) | 178 (91.8) | Ref | Ref |
| Low | 115 (35.8) | 206 (64.2) | 7.75 (3.52, 17.05) | 6.19 (3.42,11.22) ** |
| Measure of Variation | Model 0 (95% CI) | Model 1 (95% CI) | Model 2 (95% CI) | Model 3 (95% CI) |
|---|---|---|---|---|
| Variance of intercept | 0.69 (0.16, 3.02) | 0.58 (0.08, 3.92) | 0.57 (0.20, 1.58) | 0.49 (0.14, 1.73) |
| ICC percentage | 27.23 (10.49–54.40) | |||
| MPR | 2.20 (1.46–5.21) | 1.95 (1.42, 3.49) | ||
| Model fitness | ||||
| Log-likelihood ratio | −293.10 | −257.72 | −245.67 | −228.15 |
| AIC | 590.21 | 533.45 | 505.35 | 474.30 |
| BIC | 598.70 | 571.64 | 535.06 | 512.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoseph, A.; Mussie, L.; Belayineh, M.; Aguinaga-Ontoso, I.; Guillen-Grima, F.; Mutwiri, G. The Determinants of Coexisting Anemia and Undernutrition Among Pregnant Women in Southern Ethiopia: A Multi-Level Analysis. Healthcare 2025, 13, 1495. https://doi.org/10.3390/healthcare13131495
Yoseph A, Mussie L, Belayineh M, Aguinaga-Ontoso I, Guillen-Grima F, Mutwiri G. The Determinants of Coexisting Anemia and Undernutrition Among Pregnant Women in Southern Ethiopia: A Multi-Level Analysis. Healthcare. 2025; 13(13):1495. https://doi.org/10.3390/healthcare13131495
Chicago/Turabian StyleYoseph, Amanuel, Lakew Mussie, Mehretu Belayineh, Ines Aguinaga-Ontoso, Francisco Guillen-Grima, and G. Mutwiri. 2025. "The Determinants of Coexisting Anemia and Undernutrition Among Pregnant Women in Southern Ethiopia: A Multi-Level Analysis" Healthcare 13, no. 13: 1495. https://doi.org/10.3390/healthcare13131495
APA StyleYoseph, A., Mussie, L., Belayineh, M., Aguinaga-Ontoso, I., Guillen-Grima, F., & Mutwiri, G. (2025). The Determinants of Coexisting Anemia and Undernutrition Among Pregnant Women in Southern Ethiopia: A Multi-Level Analysis. Healthcare, 13(13), 1495. https://doi.org/10.3390/healthcare13131495




_MD__MPH_PhD.png)



