Impact of the COVID-19 Pandemic on Emergency Air Medical Transport of Pediatric Patients in the Penghu Islands
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.C.; Chang, Y.C.; Fan Chiang, Y.L.; Chien, Y.C.; Cheng, M.; Yang, C.H.; Huang, C.H.; Hsu, Y.N. First case of coronavirus disease 2019 (COVID-19) pneumonia in Taiwan. J. Formos. Med. Assoc. 2020, 119, 747–751. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.C.; Lee, P.I.; Hsueh, P.R. How Taiwan has responded to COVID-19 and how COVID-19 has affected Taiwan, 2020–2022. J. Microbiol. Immunol. Infect. 2023, 56, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.T.; Lin, C.Y.; Tsai, M.J.; Hung, C.T.; Hsu, C.W.; Lu, P.L.; Hou, M.F. Infection control measures of a Taiwanese hospital to confront the COVID-19 pandemic. Kaohsiung J. Med. Sci. 2020, 36, 296–304. [Google Scholar] [CrossRef]
- Lee, Y.T.; Lai, Y.W.; Chen, J.H.; Chen, W.L.; Wu, M.Y.; Chung, J.Y. Assessing the impact of the COVID-19 pandemic on pediatric emergency department visits in Taiwan. Medicina 2024, 60, 288. [Google Scholar] [CrossRef]
- Wu, M.Y.; Li, C.J.; Hou, Y.T.; Chen, Y.L.; Chang, F.W.; Yiang, G.T. Analysis of emergency air medical services over 9 years in the Penghu archipelago of Taiwan. Tzu Chi Med. J. 2020, 32, 82–87. [Google Scholar] [CrossRef]
- Li, S.P.; Hsu, P.C.; Huang, C.Y.; Wu, P.W.; Fang, H.H. Air transportation impact on a late preterm neonate. Aerosp. Med. Hum. Perform. 2024, 95, 219–222. [Google Scholar] [CrossRef]
- Frakes, M.A.; Denison, T.; Leisten, D.C.; Wheeler, J.; Boomhower, J.; Cohen, J.E.; Wilcox, S. Operational policies and procedures for critical care transport during a respiratory pandemic. Air Med. J. 2022, 41, 252–256. [Google Scholar] [CrossRef]
- Abe, T.; Takahashi, O.; Saitoh, D.; Tokuda, Y. Association between helicopter with physician versus ground emergency medical services and survival of adults with major trauma in Japan. Crit. Care 2014, 18, R146. [Google Scholar] [CrossRef]
- Grines, C.L.; Westerhausen, D.R.; Grines, L.L., Jr.; Hanlon, J.T.; Logemann, T.L.; Niemela, M.; Weaver, W.D.; Graham, M.; Boura, J.; O’Neill, W.W.; et al. A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction: The Air Primary Angioplasty in Myocardial Infarction study. J. Am. Coll. Cardiol. 2002, 39, 1713–1719. [Google Scholar] [CrossRef] [PubMed]
- Silliman, S.L.; Quinn, B.; Huggett, V.; Merino, J.G. Use of a field-to-stroke center helicopter transport program to extend thrombolytic therapy to rural residents. Stroke 2003, 34, 729–733. [Google Scholar] [CrossRef] [PubMed]
- Tsai, S.-H.; Kraus, J.; Wu, H.-R.; Chen, W.-L.; Chiang, M.-F.; Lu, L.-H.; Chang, C.-E.; Chiu, W.-T. The effectiveness of video-telemedicine for screening of patients requesting emergency air medical transport (EAMT). J. Trauma 2007, 62, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Dewhurst, A.T.; Farrar, D.; Walker, C.; Mason, P.; Beven, P.; Goldstone, J.C. Medical repatriation via fixed-wing air ambulance: A review of patient characteristics and adverse events. Anaesthesia 2001, 56, 882–887. [Google Scholar] [CrossRef]
- Wills, V.L.; Eno, L.; Walker, C.; Gani, J.S. Use of an ambulance-based helicopter retrieval service. Aust. N. Z. J. Surg. 2000, 70, 506–510. [Google Scholar] [CrossRef]
- Stroud, M.H.; Miquel-Verges, F.F.; Rozenfeld, R.A.; Holcomb, R.G.; Brown, C.C.; Meyer, K. The state of neonatal and pediatric interfacility transport during the coronavirus disease 2019 pandemic. Air Med. J. 2021, 40, 331–336. [Google Scholar] [CrossRef]
- Bogli, J.; Gusewell, S.; Strassle, R.; Kahlert, C.R.; Albrich, W.C. Pediatric hospital admissions, case severity, and length of hospital stay during the first 18 months of the COVID-19 pandemic in a tertiary children’s hospital in Switzerland. Infection 2023, 51, 439–446. [Google Scholar] [CrossRef]
- Gill, P.J.; Mahant, S.; Hall, M.; Berry, J.G. Reasons for admissions to US children’s hospitals during the COVID-19 pandemic. JAMA 2021, 325, 1676–1679. [Google Scholar] [CrossRef]
- Pelletier, J.H.; Rakkar, J.; Au, A.K.; Fuhrman, D.; Clark, R.S.B.; Horvat, C.M. Trends in US pediatric hospital admissions in 2020 compared with the decade before the COVID-19 pandemic. JAMA Netw. Open 2021, 4, e2037227. [Google Scholar] [CrossRef]
- Bodilsen, J.; Nielsen, P.B.; Sogaard, M.; Dalager-Pedersen, M.; Speiser, L.O.Z.; Yndigegn, T.; Nielsen, H.; Larsen, T.B.; Skjøth, F. Hospital admission and mortality rates for non-covid diseases in Denmark during COVID-19 pandemic: Nationwide population based cohort study. BMJ 2021, 373, n1135. [Google Scholar] [CrossRef]
- Chen, H.H.; Kao, J.H.; Chen, J.S.; Ni, Y.H. What we have learned from COVID-19 pandemic? J. Formos. Med. Assoc. 2021, 120 (Suppl. S1), S1–S5. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.F.; Huang, Y.H.; Cheng, C.Y.; Wu, K.H.; Tang, K.S.; Chiu, I.M. Public Health Interventions for the COVID-19 pandemic reduce respiratory tract infection-related visits at pediatric emergency departments in Taiwan. Front. Public Health 2020, 8, 604089. [Google Scholar] [CrossRef] [PubMed]
- Fuse, T.; Ikuse, T.; Aizawa, Y.; Fuse, M.; Goto, F.; Okazaki, M.; Iwaya, A.; Saitoh, A. Decline in pediatric admission on an isolated island in the COVID-19 pandemic. Pediatr. Int. 2022, 64, e15326. [Google Scholar] [CrossRef] [PubMed]
- Wilder, J.L.; Parsons, C.R.; Growdon, A.S.; Toomey, S.L.; Mansbach, J.M. Pediatric hospitalizations during the COVID-19 pandemic. Pediatrics 2020, 146, e2020005983. [Google Scholar] [CrossRef]
- Hatoun, J.; Correa, E.T.; Donahue, S.M.A.; Vernacchio, L. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics 2020, 146, e2020006460. [Google Scholar] [CrossRef]
- Rush, M.; Khan, A.; Barber, J.; Bloom, M.; Anspacher, M.; Fratantoni, K.; Parikh, K. Length of stay and barriers to discharge for technology-dependent children during the COVID-19 Pandemic. Hosp. Pediatr. 2023, 13, 80–87. [Google Scholar] [CrossRef]
- Wu, J.H.; Wang, C.C.; Lu, F.L.; Huang, S.C.; Liu, Y.P.; Lu, C.Y.; Chang, L.-Y.; Wu, E.-T. The impact of the coronavirus disease 2019 epidemic and national public restrictions on Pediatric intensive care units in Taiwan. J. Formos. Med. Assoc. 2023, 122, 113–120. [Google Scholar] [CrossRef]
| Demographics | All Cases (n = 40) | Before COVID-19 (n = 20) | During COVID-19 (n = 20) | p-Value |
|---|---|---|---|---|
| Age, median (Q1–Q3) | ||||
| <6 year | 1 (0–3.00) | 2 (0–3.00) | 1 (0–1.50) | 0.322 |
| 6 to <18 years | 10 (7.50–16.50) | 9 (8.25–16.25) | 12.5 (8.00–16.00) | 0.804 |
| All ages | 2 (0–5.00) | 3 (0–5.00) | 1 (0–5.00) | 0.362 |
| Gender, n (%) | ||||
| Male | 28 (70.00) | 15 (75.00) | 13 (65.00) | 0.731 |
| Female | 12 (30.00) | 5 (25.00) | 7 (35.00) | |
| Aircraft, n (%) | ||||
| rotary-wing | 36 (90.00) | 20 (100.00) | 16 (80.00) | 0.106 |
| fixed-wing | 4 (10.00) | 0 (0.00) | 4 (20.00) | |
| Hospital stay, median (Q1–Q3) | 12.5 (8.00–26.50) | 11 (6.00–16.50) | 17 (9.00–31.00) | 0.098 |
| Reason, n (%) | ||||
| Insufficient medical equipment | 26 (65.00) | 15 (75.00) | 11 (55.00) | 0.320 |
| Lack of specialist doctors | 19 (47.50) | 6 (30.00) | 13 (65.00) | 0.056 |
| Family request | 10 (25.00) | 5 (25.00) | 5 (25.00) | 1.000 |
| No beds | 1 (2.50) | 0 (0.00) | 1 (5.00) | 1.000 |
| Disease, n (%) | ||||
| Burn injury | 2 (5.00) | 1 (5.00) | 1 (5.00) | 1.000 |
| Traumatic injury | 9 (22.50) | 5 (25.00) | 4 (20.00) | 1.000 |
| Neurological disease | 11 (27.50) | 6 (30.00) | 5 (25.00) | 1.000 |
| Neonatal disease | 12 (30.00) | 6 (30.00) | 6 (30.00) | 1.000 |
| Cardiovascular disease | 6 (15.00) | 4 (20.00) | 2 (10.00) | 0.661 |
| Infectious disease | 7 (17.50) | 4 (20.00) | 3 (15.00) | 1.000 |
| Genetics and Metabolism | 5 (12.50) | 3 (15.00) | 2 (10.00) | 1.000 |
| Gastroenterology | 1 (2.50) | 0 (0.00) | 1 (5.00) | 1.000 |
| Nephrology | 3 (7.50) | 1 (5.00) | 2 (10.00) | 1.000 |
| Pulmonology | 1 (2.50) | 0 (0.00) | 1 (5.00) | 1.000 |
| Hematologic disease | 1 (2.50) | 1 (1.00) | 0 (0.00) | 1.000 |
| Critical care medicine | 14 (35.00) | 6 (30.00) | 8 (40.00) | 0.741 |
| Year | Subspecialty 1 | Subspecialty 2 | Subspecialty 3 | Subspecialty 4 |
|---|---|---|---|---|
| 2017 | Endocrinology | Cardiology | Neurology | |
| 2018 | Endocrinology | Cardiology | Neurology | |
| 2019 | Endocrinology | Cardiology | Neonatology | GI |
| 2020 | Endocrinology | Cardiology | Neonatology | GI |
| 2021 | Endocrinology | Cardiology | Neonatology | GI |
| 2022 | Endocrinology | Cardiology | Neonatology | Neurology |
| Demographics | All Cases (n = 27) | Before COVID-19 (n = 13) | During COVID-19 (n = 14) | p-Value |
|---|---|---|---|---|
| Age, median (Q1–Q3) | 1 (0–2.00) | 2 (0–3.00) | 0.5 (0–1.00) | 0.300 |
| Gender, n (%) | ||||
| Male | 17 (62.96) | 9 (69.23) | 8 (57.14) | 0.695 |
| Female | 10 (37.04) | 4 (30.77) | 6 (42.86) | |
| Aircraft, n (%) | ||||
| rotary-wing | 24 (88.89) | 13 (100.00) | 11 (78.57) | 0.222 |
| fixed-wing | 3 (11.11) | 0 (0.00) | 3 (21.43) | |
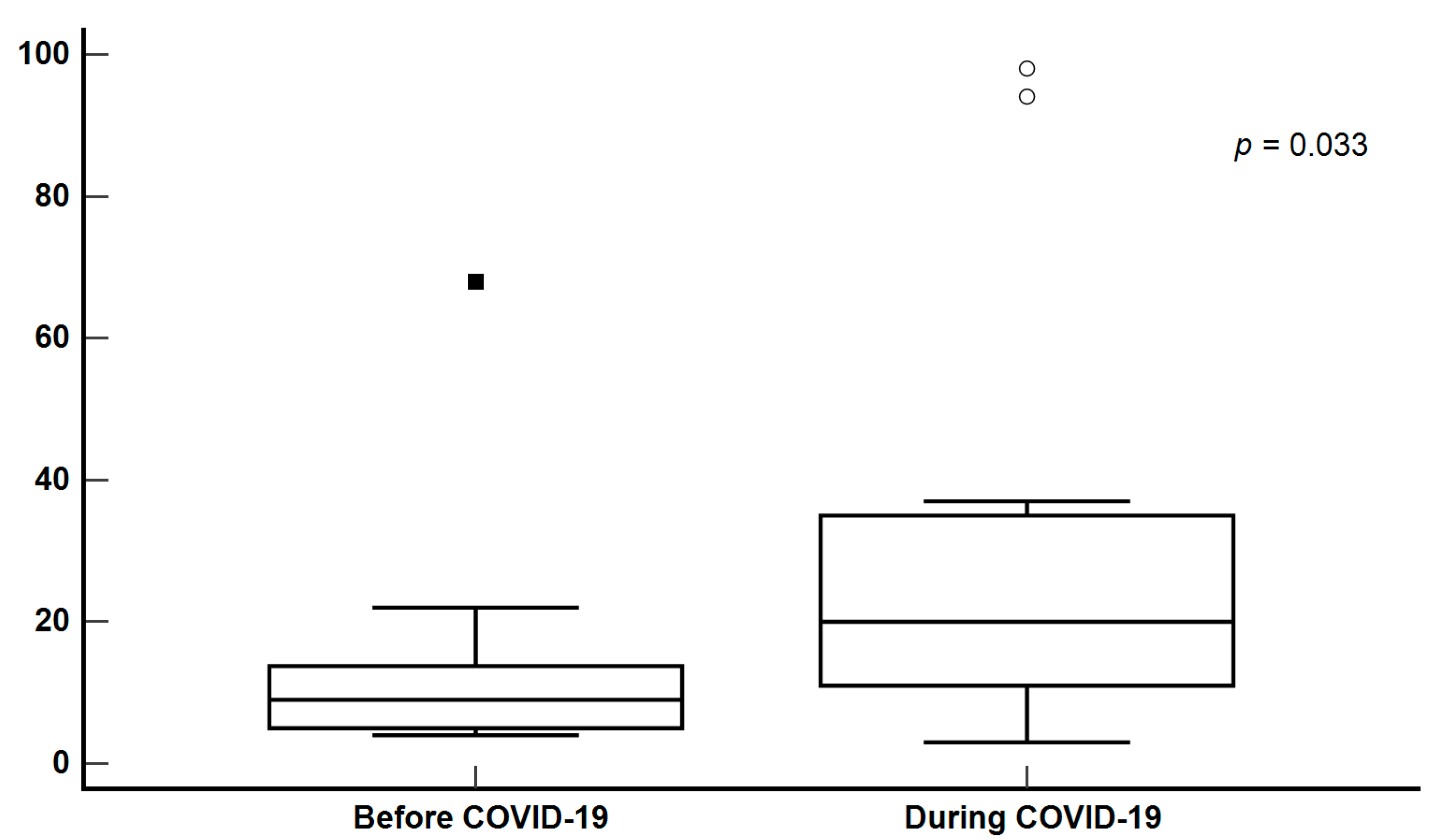
| Hospital stay, median (Q1–Q3) | 13 (8.00–26.50) | 9 (5.00–13.75) | 20 (11.00–35.00) | 0.033 |
| Reason, n (%) | ||||
| Insufficient medical equipment | 21 (77.78) | 12 (92.31) | 9 (64.29) | 0.165 |
| Lack of specialist doctors | 14 (51.85) | 4 (30.77) | 10 (71.43) | 0.057 |
| Family request | 5 (18.52) | 2 (15.38) | 3 (21.43) | 1.000 |
| No beds | 0 (0.00) | 0 (0.00) | 0 (0.00) | - |
| Disease, n (%) | ||||
| Neurological disease | 10 (37.04) | 6 (46.15) | 4 (28.57) | 0.440 |
| Neonatal disease | 12 (44.44) | 6 (46.15) | 6 (42.86) | 1.000 |
| Cardiovascular disease | 5 (18.52) | 3 (23.08) | 2 (14.29) | 0.648 |
| Infectious disease | 6 (22.22) | 3 (23.08) | 3 (21.43) | 1.000 |
| Genetics and Metabolism | 5 (18.52) | 3 (23.08) | 2 (14.29) | 0.648 |
| Gastroenterology | 1 (3.70) | 0 (0.00) | 1 (7.14) | 1.000 |
| Nephrology | 2 (7.41) | 1 (7.69) | 1 (7.14) | 1.000 |
| Pulmonology | 1 (3.70) | 0 (0.00) | 1 (7.14) | 1.000 |
| Hematologic disease | 0 (0.00) | 0 (0.00) | 0 (0.00) | - |
| Critical care medicine | 9 (33.33) | 5 (38.46) | 4 (28.57) | 0.695 |
| Seasons, n (%) | All Cases (n = 27) | Before COVID-19 (n = 13) | During COVID-19 (n = 14) | p-Value |
|---|---|---|---|---|
| Spring | 7 (25.93) | 5 (38.46) | 2 (14.29) | 0.209 |
| Summer | 11 (40.74) | 4 (30.77) | 7 (50.00) | 0.440 |
| Fall | 5 (18.52) | 1 (7.69) | 4 (28.57) | 0.326 |
| Winter | 4 (14.81) | 3 (23.08) | 1 (7.14) | 0.326 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fang, H.-H.; Huang, C.-Y.; Hsu, P.-C.; Sung, C.-C.; Li, S.-P.; Lai, C.-Y. Impact of the COVID-19 Pandemic on Emergency Air Medical Transport of Pediatric Patients in the Penghu Islands. Healthcare 2025, 13, 1450. https://doi.org/10.3390/healthcare13121450
Fang H-H, Huang C-Y, Hsu P-C, Sung C-C, Li S-P, Lai C-Y. Impact of the COVID-19 Pandemic on Emergency Air Medical Transport of Pediatric Patients in the Penghu Islands. Healthcare. 2025; 13(12):1450. https://doi.org/10.3390/healthcare13121450
Chicago/Turabian StyleFang, Hung-Hsiang, Chuang-Yen Huang, Po-Chang Hsu, Chia-Cheng Sung, Sheng-Ping Li, and Chung-Yu Lai. 2025. "Impact of the COVID-19 Pandemic on Emergency Air Medical Transport of Pediatric Patients in the Penghu Islands" Healthcare 13, no. 12: 1450. https://doi.org/10.3390/healthcare13121450
APA StyleFang, H.-H., Huang, C.-Y., Hsu, P.-C., Sung, C.-C., Li, S.-P., & Lai, C.-Y. (2025). Impact of the COVID-19 Pandemic on Emergency Air Medical Transport of Pediatric Patients in the Penghu Islands. Healthcare, 13(12), 1450. https://doi.org/10.3390/healthcare13121450







