Effects of Hypopressive Techniques on the CORE Complex: A Systematic Review
Abstract
1. Introduction
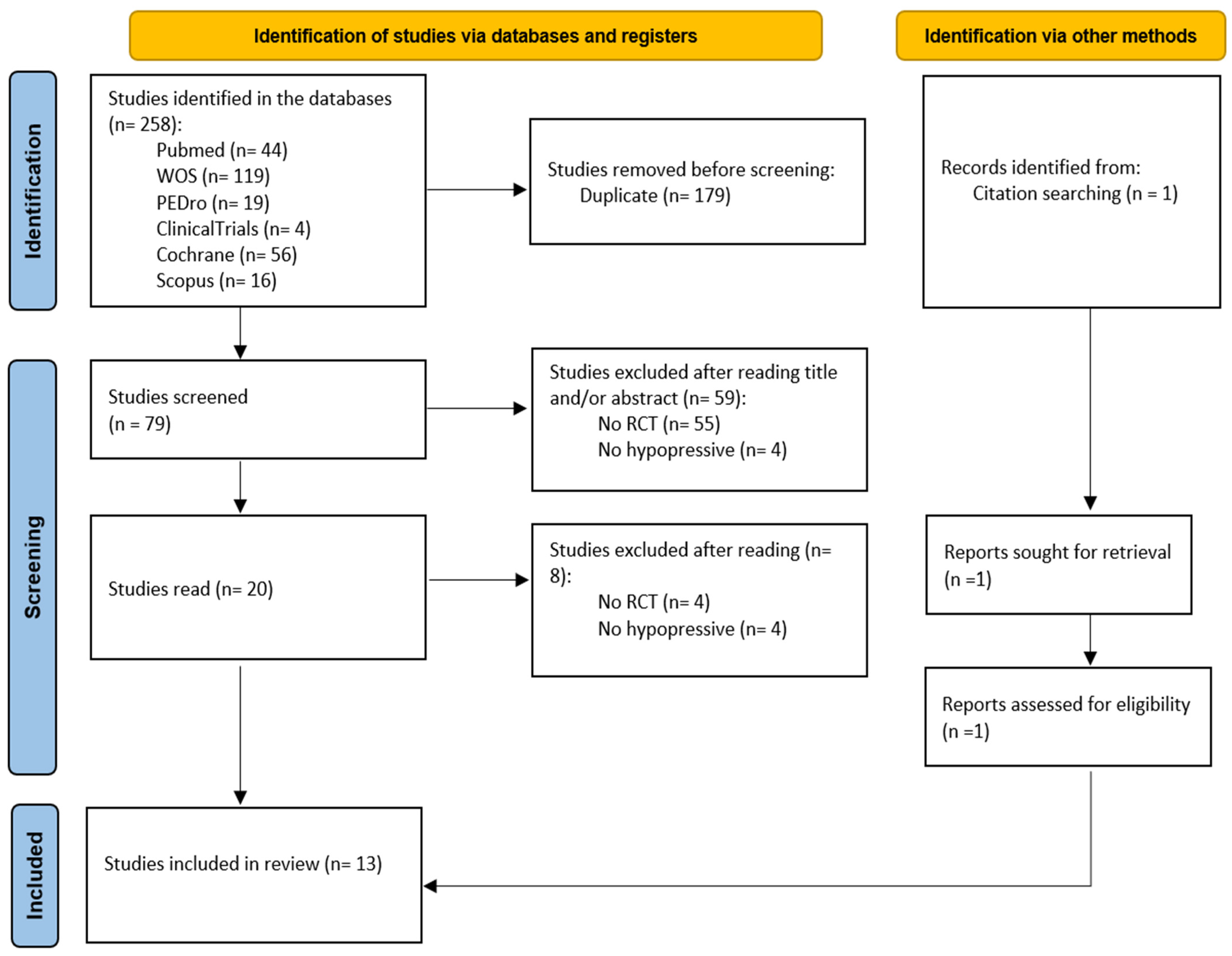
2. Materials and Methods
2.1. Design
2.2. Study Selection
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Methodological Quality of the Studies and Risk of Bias
3.2. Participants
3.3. Interventions
3.4. Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CORE | Lumbo-Pelvi Coxal Complex |
| PF | Pelvic Floor |
| AHT | Abdominal Hypopressive Techniques |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-analyses |
| RoB | Risk of Bias |
| PFMX | Pelvic Floor Muscle Exercise |
| UI | Urinary Incontinence |
| TrA | Abdominis Transversus |
Appendix A
| Database | Search Equations |
|---|---|
| PUBMED | ((“Pelvic Floor” [Mesh]) OR (“Pelvic Floor Disorders” [Mesh])) AND ((“hypopressive exercise”) OR (“hypopressive abdominals”) OR (“hypopressive method”)) ((“Abdominal Muscles” [Mesh]) OR (“Abdominal CORE” [Mesh])) AND ((“hypopressive exercise”) OR (“hypopressive abdominals”) OR (“hypopressive method”)) ((“Low Back Pain” [Mesh]) OR (“Back Pain” [Mesh]) AND ((“hypopressive exercise”) OR (“hypopressive abdominals”) OR (“hypopressive method”)) (“Diaphragm” [Mesh]) AND ((“hypopressive exercise”) OR (“hypopressive abdominals”) OR (“hypopressive method”)) |
| WOS | (((((TS = (hypopressive method)) OR TS = (hypopressive exercise)) OR TS = (hypopressive abdominals))) AND (((TS = (pelvic floor)) OR TS = (pelvic floor disorders)))) (((((TS = (abdominal CORE)) OR TS = (abdominal muscles))) AND (TS=(hypopressive exercise)) OR TS = (hypopressive abdominals)) OR TS = (hypopressive method)) ((((TS = (low back)) OR TS = (low back pain)) AND (((TS=(hypopressive exercise)) OR TS = (hypopressive method)) AND TS = (hypopressive abdominals)))) (((TS = (diaphragm)) AND (((TS = (hypopressive exercise)) OR TS = (hypopressive method)) OR TS = (hypopressive abdominals)))) |
| PEDro | hypopressive* “pelvic floor*” “pelvic floor disorders*” hypopressive* “low back pain*” “low back*” hypopressive* “abdominal CORE*” “abdominal wall*” hypopressive* diaphragm* |
| CLINICALTRIALS | hypopressive exercise, hypopressive abdominals, hypopressive method|Pelvic Floor Disorders hypopressive exercise, hypopressive abdominals, hypopressive method|abdominal CORE hypopressive exercise, hypopressive abdominals, hypopressive method|Low Back Pain hypopressive exercise, hypopressive abdominals, hypopressive method|Diaphragm |
| Cochrane | “HYPOPRESSIVE” AND “PELVIC FLOOR” “HYPOPRESSIVE” AND (“ABDOMINAL MUSCLES” MESH) “HYPOPRESSIVE” AND (“LOW BACK PAIN” MESH) “HYPOPRESSIVE” AND “DIAPHRAGM” |
| Scopus | (TITLE-ABS-KEY ((“Pelvic Floor” OR “Pelvic Floor Disorders“) AND (“hypopressive abdominals” OR “hypopressive method”)) TITLE-ABS-KEY (((“Abdominal muscles” OR “Abdominal core”) AND (“hypopressive abdominals” OR “hypopressive AND method”))) TITLE-ABS-KEY (((“Low Back Pain” OR “Low Back”) AND (“hypopressive abdominals” OR “hypopressive AND method”))) TITLE-ABS-KEY TITLE-ABS-KEY (((“Diaphragm”) AND (“hypopressive abdominals” OR “hypopressive AND method”))) |
References
- Akuthota, V.; Nadler, S.F. Core strengthening. Arch. Phys. Med. Rehabil. 2004, 85, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.E.; Nyland, J.; Caudill, P.; Brosky, J.; Caborn, D.N. Dynamic trunk stabilization: A conceptual back injury prevention program for volleyball athletes. J. Orthop. Sports Phys. Ther. 2008, 38, 703–720. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.M. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J. Spinal Disord. 1992, 5, 383–397. [Google Scholar] [CrossRef]
- Panjabi, M.M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J. Spinal Disord. 1992, 5, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Rami-Colás, C.; Martín-Nogueras, A.M. Physiotherapy treatment of idiopathic scoliosis: Schroth versus hypopressive gymnastics. Fisioterapia 2016, 38, 28–37. [Google Scholar] [CrossRef]
- Soto González, M.; Da Cuña Carrera, I.; Gutiérrez Nieto, M.; López García, S.; Ojea Calvo, A.; Lantarón Caeiro, E.M. Early 3-month treatment with comprehensive physical therapy program restores continence in urinary incontinence patients after radical prostatectomy: A randomized controlled trial. Neurourol. Urodyn. 2020, 39, 1529–1537. [Google Scholar] [CrossRef]
- Caufriez, M.; Fernández, J.C.; Guignel, G.; Heimann, A. Comparación de las variaciones de presión abdominal en medio acuático y aéreo durante la realización de cuatro ejercicios abdominales hipopresivos. Rev. Iberoam. Fisioter. Kinesiol. 2007, 10, 12–23. [Google Scholar] [CrossRef]
- Navarro Brazález, B.; Sánchez Sánchez, B.; Prieto Gómez, V.; De La Villa Polo, P.; McLean, L.; Torres Lacomba, M. Pelvic floor and abdominal muscle responses during hypopressive exercises in women with pelvic floor dysfunction. Neurourol. Urodyn. 2020, 39, 793–803. [Google Scholar] [CrossRef]
- Stüpp, L.; Resende, A.P.; Petricelli, C.D.; Nakamura, M.U.; Alexandre, S.M.; Zanetti, M.R. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourol. Urodyn. 2011, 30, 1518–1521. [Google Scholar] [CrossRef]
- Da Cuña-Carrera, I.; Alonso-Calvete, A.; Lantarón-Caeiro, E.M.; Soto-González, M. Are There Any Differences in Abdominal Activation between Women and Men during Hypopressive Exercises? Int. J. Environ. Res. Public Health 2021, 18, 6984. [Google Scholar] [CrossRef]
- Katz, C.M.S.; Barbosa, C.P. Effects of hypopressive exercises on pelvic floor and abdominal muscles in adult women: A systematic review of randomized clinical trials. J. Bodyw. Mov. Ther. 2024, 37, 38–45. [Google Scholar] [CrossRef] [PubMed]
- de Viñaspre-Hernández, R.R. Efficacy of hypopressive abdominal gymnastics in rehabilitating the pelvic floor of women: A systematic review. Actas Urol. Esp. 2018, 42, 557–566. [Google Scholar] [CrossRef]
- Bellido-Fernández, L.; Jiménez-Rejano, J.; Chillón-Martínez, R.; Gómez-Benítez, M.; De-La-Casa-Almeida, M.; Rebollo-Salas, M. Effectiveness of Massage Therapy and Abdominal Hypopressive Gymnastics in Nonspecific Chronic Low Back Pain: A Randomized Controlled Pilot Study. Evid.-Based Complement. Alternat. Med. 2018, 2018, 3684194. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Ardem, C.L.; Büttner, F.; Andrade, R.; Weir, A.; Ashe, M.C.; Holden, S.; Impellizzeri, F.M.; Delahunt, E.; Dijkstra, H.P.; Mathieson, S.; et al. Implementing the 27 PRISMA 2020 Statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: The PESiST. Br. J. Sports Med. 2022, 56, 175–195. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Jose-Vaz, L.A.; Andrade, C.L.; Cardoso, L.C.; Bernardes, B.T.; Pereira-Baldon, V.S.; Resende, A.P.M. Can abdominal hypopressive technique improve stress urinary incontinence? An assessor-blinded randomized controlled trial. Neurourol. Urodyn. 2020, 39, 2314–2321. [Google Scholar] [CrossRef]
- Resende, A.P.; Stüpp, L.; Bernardes, B.T.; Oliveira, E.; Castro, R.A.; Girão, M.J.; Sartori, M.G. Can hypopressive exercises provide additional benefits to pelvic floor muscle training in women with pelvic organ prolapse? Neurourol. Urodyn. 2012, 31, 121–125. [Google Scholar] [CrossRef]
- Dierick, F.; Galtsova, E.; Lauer, C.; Buisseret, F.; Bouché, A.F.; Martin, L. Clinical and MRI changes of puborectalis and iliococcygeus after a short period of intensive pelvic floor muscles training with or without instrumentation: A prospective randomized controlled trial. Eur. J. Appl. Physiol. 2018, 118, 1661–1671. [Google Scholar] [CrossRef] [PubMed]
- Bellido-Fernández, L.; Jiménez-Rejano, J.J.; Chillón-Martínez, R.; Lorenzo-Muñoz, A.; Pinero-Pinto, E.; Rebollo-Salas, M. Clinical relevance of massage therapy and abdominal hypopressive gymnastics on chronic nonspecific low back pain: A randomized controlled trial. Disabil. Rehabil. 2022, 44, 4233–4240. [Google Scholar] [CrossRef] [PubMed]
- Collado, S.A.; Pellicer, C.M.; Ramirez, B.M.; Dominguez-Escrig, J.; Rubio-Briones, J.; Gomez-Ferrer, A.; Iborra, J.I.; Casanova, R.-B.J.; Ricos, T.J.; Monros, L.J.; et al. Intensive preoperatory Pelvic Floor Muscle Training reduce duration and severity of stress urinary incontinence after radical prostatectomy: A randomized controlled trial. Eur. Urol. Suppl. 2013, 12, e1007–e1008. [Google Scholar] [CrossRef]
- Resende, A.P.M.; Stüpp, L.; Bernardes, B.T.; Oliveria, E.; Castro, R.A.; Girão, M.J.B.C.; Sartori, M.G.F. Pelvic floor muscle training alone or in combination with hypopressive exercises: Randomized controlled trial. Neurourol. Urodyn. 2010, 29, 973–975. [Google Scholar]
- Au, D.; Matthew, A.G.; Alibhai, S.M.; Jones, J.M.; Fleshner, N.E.; Finelli, A.; Elterman, D.; Singal, R.K.; Jamnicky, L.; Faghani, N.; et al. Pfilates and hypopressives for the treatment of urinary incontinence after radical prostatectomy: Results of a feasibility randomized controlled trial. PM&R 2020, 12, 55–63. [Google Scholar] [CrossRef]
- Moreno-Muñoz, M.D.M.; Hita-Contreras, F.; Estudillo-Martínez, M.D.; Aibar-Almazán, A.; Castellote-Caballero, Y.; Bergamin, M.; Gobbo, S.; Cruz-Díaz, D. The Effects of Abdominal Hypopressive Training on Postural Control and Deep Trunk Muscle Activation: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 2741. [Google Scholar] [CrossRef]
- Molina-Torres, G.; Moreno-Muñoz, M.; Rebullido, T.R.; Castellote-Caballero, Y.; Bergamin, M.; Gobbo, S.; Hita-Contreras, F.; Cruz-Diaz, D. The effects of an 8-week hypopressive exercise training program on urinary incontinence and pelvic floor muscle activation: A randomized controlled trial. Neurourol. Urodyn. 2023, 42, 500–509. [Google Scholar] [CrossRef]
- Vicente-Campos, D.; Sanchez-Jorge, S.; Terrón-Manrique, P.; Guisard, M.; Collin, M.; Castaño, B.; Rodríguez-Sanz, D.; Becerro-de-Bengoa-Vallejo, R.; Chicharro, J.L.; Calvo-Lobo, C. The Main Role of Diaphragm Muscle as a Mechanism of Hypopressive Abdominal Gymnastics to Improve Non-Specific Chronic Low Back Pain: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 4983. [Google Scholar] [CrossRef] [PubMed]
- Mitova, S.; Avramova, M.; Gramatikova, M. Effectiveness of hypopressive gymnastics in women with pelvic floor dysfunction. J. Phys. Educ. Sport 2022, 22, 416–422. [Google Scholar] [CrossRef]
- Navarro-Brazález, B.; Prieto-Gómez, V.; Prieto-Merino, D.; Sánchez-Sánchez, B.; McLean, L.; Torres-Lacomba, M. Effectiveness of Hypopressive Exercises in Women with Pelvic Floor Dysfunction: A Randomised Controlled Trial. J. Clin. Med. 2020, 9, 1149. [Google Scholar] [CrossRef]
- Caufriez, M.; Fernández, J.C.; Fanzel, R.; Snoeck, T. Efectos de un programa de entrenamiento estructurado de Gimnasia Abdominal Hipopresiva sobre la estática vertebral cervical y dorsolumbar. Fisioterapia 2006, 28, 205–216. [Google Scholar] [CrossRef]
- Ithamar, L.; de Moura Filho, A.G.; Benedetti Rodrigues, M.A.; Duque Cortez, K.C.; Machado, V.G.; de Paiva Lima, C.R.O.; Moretti, E.; Lemos, A. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J. Bodyw. Mov. Ther. 2018, 22, 159–165. [Google Scholar] [CrossRef]
- Rial, T.; Pinsach, P. Principios técnicos de los ejercicios hipopresivos del Dr. Caufriez. Educ. Fís. Deport. Rev. Digit. 2012, 17, 172. [Google Scholar]
- Sussman, R.D.; Syan, R.; Brucker, B.M. Guideline of guidelines: Urinary incontinence in women. BJU Int. 2020, 125, 638–655. [Google Scholar] [CrossRef]
- Cortell-Tormo, J.M.; García-Jaén, M.; Chulvi-Medrano, I.; Hernández-Sánchez, S.; Lucas-Cuevas, Á.G.; Tortosa-Martínez, J. Influence of scapular position on the core musculature activation in the prone plank exercise. J. Strength Cond. Res. 2017, 31, 2255–2262. [Google Scholar] [CrossRef]
- Hodges, P.W.; Richardson, C.A. Contraction of the abdominal muscles associated with movement of the lower limb. Phys. Ther. 1997, 77, 132–144. [Google Scholar] [CrossRef]
- Rial, T.; Sousa, L.; García, E.; Pinsach, P. Efectos inmediatos de una sesión de ejercicios hipopresivos en diferentes parámetros corporales. Cuest. Fisioter. 2014, 43, 13–21. [Google Scholar]
- Álvarez-Sáez, M.M.; Rial-Rebullido, T.R.; Chulvi-Medrano, I.; García-Soidán, J.L.; Cortell-Tormo, J. Can an eight-week program based on the hypopressive technique produce changes in pelvic floor function and body composition in female rugby players? Retos 2016, 30, 26–29. [Google Scholar]
- Barresi-Leloutre, I.M.; Hernández-Vian, Ó. Efectos de un programa de entrenamiento de Hypopressive RSF Reprogramación Sistémica Funcional en mujeres sanas. Retos Nuevas Tend. Educ. Fís. Deporte Recreación 2021, 39, 120–124. [Google Scholar]
- Shiri, R.; Falah-Hassani, K.; Heliövaara, M.; Solovieva, S.; Amiri, S.; Lallukka, T.; Burdorf, A.; Husgafvel-Pursiainen, K.; Viikari-Juntura, E. Risk Factors for Low Back Pain: A Population-Based Longitudinal Study. Arthritis Care Res. 2019, 71, 290–299. [Google Scholar] [CrossRef]
- Santiago-Bazan, C.; Alvarado-Perez, J.R.; Ludeña-Ambukka, S.T. Hypopressive exercises in patients with chronic lower back pain at a rehabilitation center in Lima. Rev. Cient. Cienc. Méd. 2023, 26, 8–15. [Google Scholar]
- Ishida, H.; Kobara, K.; Osaka, H.; Suehiro, T.; Ito, T.; Kurozumi, C.; Watanabe, S. Correlation between Peak Expiratory Flow and Abdominal Muscle Thickness. J. Phys. Ther. Sci. 2014, 26, 1791–1793. [Google Scholar] [CrossRef] [PubMed]


| Author | 1 * | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Au et al. (2020) [25] | N | Y | Y | Y | N | N | N | N | Y | Y | Y | 6 |
| Bellido-Fdez et al. (2022) [22] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Caufriez et al. (2006) [31] | Y | Y | Y | N | Y | N | Y | Y | N | Y | Y | 7 |
| Collado-Serra et al. (2013) [23] | Y | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Dierick et al. (2018) [21] | Y | Y | N | Y | N | Y | Y | Y | N | Y | Y | 7 |
| Jose-Vaz et al. (2020) [19] | Y | Y | Y | Y | N | N | Y | N | N | Y | Y | 6 |
| Mitova et al. (2022) [29] | N | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Molina-Torres et al. (2023) [27] | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | 8 |
| Moreno-Muñoz et al. (2021) [26] | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 |
| Navarro-Brazález et al. (2020) [30] | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 |
| Resende et al. (2010) [24] | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 |
| Resende et al. (2012) [20] | N | Y | N | Y | N | N | Y | Y | N | Y | Y | 6 |
| Vicente-Campos et al. (2021) [28] | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7 |
| Authors | Observed Area | Sample | Intervention | Supervisor | Age | Period | Measures | Results |
|---|---|---|---|---|---|---|---|---|
| Jose-Vaz et al. (2020) [19] | EUI | 130 | G1 (n = 36): AHT G2 (n = 37): PFMX | PST PF | G1: 56.9 ± 11.5 G2: 53.4 ± 11.6 | 12 weeks G1: 3 phases/4 weeks each; training 50′ G2: 3 series 8–12 contraction max/session 6” contraction | 7-day voiding diary, ICIQ-SF, MogS, manometry. | Significant improvements in both groups, in PF strength variables compared to baseline values. G2 significant improvements in strength variables compared to G1. G1 significantly improves EUI compared to baseline values. G2 significantly improves EUI compared to baseline values. G2 improves EUI results significantly compared to G1. |
| Resende et al. (2012) [20] | PF | 58 | G1 (n = 21): PFMX G2 (n = 21): APMFX G3 (n = 16): control | PST urogynecological | G1: 56.7 ± 10.7 G2: 51.9 ± 7.4 G3: 58.7 ± 0.4 | 12 weeks Daily | PF Strength: MOGS endurance. SEMG muscle activity. | G1 and G2 improved significantly in the PF strength variables compared to baseline values and compared to G3. There were no significant differences in muscle strength or activity between G1 and G2. The resistance in G1 was significantly higher than G2. G1 was significantly greater tan G3 in strength resistance and SEMG. G2 was significantly superior to G3 at the 3-month evaluation in all strength variables. |
| Dierick et al. (2018) [21] | Puborectal and iliococcygeal | 24 | G1 (n = 9): APMFX G2: (n = 8): BFB PFEE | PST PF | G1: 22.9 ± 1.2 G2: 23 ± 2 | 10–11months 270′ (9sessions/30′) 3 sessions/week for 3 weeks | MOGS: PF strength. rPR.iPR. PB idle tone. DA PDFI-20 and PDIQ-7. MRI: signal intensity straight-media vagina-media vagina at 3 and 9 volumes | Significant improvements in iPR and PB strength in both groups compared to baseline values. There were no differences in strength. PF resting tone nor in diaphragmatic aspiration in both groups compared to baseline values. G2 significantly improves dPR compared to baseline values. G1 did not obtain differences in rPR compared to baseline values. G2 significant improvement in dPR strength compared to G1. On MRI, the volumen of the IL and the signal intensity of the PR decreased significantly compared to baseline values in both groups. In the rest of the variables there were no significant differences. |
| Bellido-Fdez et al. (2021) [22] | NSLBP | 60 | G1 (n = 20): massotherapyG2 (n = 20): AHT G3 (n = 20): massotherapy + AHT | PST | G1: IQR 43 G2: IQR 27 G3: IQR 34 | 5 weeks 8 interventions of 30′ | ODI. NRS. SF-12 and Schober’s test | There were significant improvements in all groups 4 weeks pre/post intervention compared to baseline values in disability; pain; lumbar mobility and the physical component of quality of life. G2: significant improvements in the mental component of quality of life compared to baseline values at the end of the intervention. G3 significantly improved disability compared to G1 and G2. In the rest of variables there were no significant differences. |
| Caufriez et al. (2006) [31] | Back | 29 | G1: AHT G2: posture training | - | - | 10 weeks 1h weekly | Shöber test; occipital axis. Cervical arrow. Lumbar and dorsal; flexion and extension of spine; Sorensen-Biering test; lateral inclination measurement; measurement of the height of the ASIS and PSIS. Popliteal angle and psoas extensibility. | Sorensen-Biering test: significant improvements in G1 compared to baseline values. Occipital axis: significant difference for G1 compared to baseline values. Measurement of the height of the ASIS and PSIS. Popliteal angle and psoas extensibility: significant improvements in both groups compared to baseline values. In the resto of the variables there were no significant differences. |
| Navarro-Brazález et al. (2020) [30] | PFD | 96 | G1 (n = 32): PFMXG2 (n = 32): AHT G3 (n = 32): APFX | PST PF | G1: 48 ± 12 G2: 48 ± 8 G3: 46 ± 8 | 8 weeks 2 sessions: 45′/week | PFID-20. PDIQ-7. PFM measurement with manometer and dynamometer | G1, G2 and G3 significantly improved the strength of the PFM compared to baseline values. There were no statistically significant differences between groups. |
| Collado Serra (2014) [23] | EUI and RP | 179 | G1 (n = 87): APFX G2 (n = 92): control | - | - | G1: 3 weeks before operation/3 months after. Daily PFMT and weekly AHT. G2: 3 months after operation, daily kegels. | 24h-PW. ICIQ-QI SF. continence. | Both significantly reduce the duration and severity of SUI after RP compared to baseline values. G1 significantly reduces the duration and severity of SUI after RP compared to G2. |
| Resende et al. (2010) [24] | PFM and activation TrA | 58 | G1 (n = 21): PFMX G2 (n = 21): AHT G3 (n = 16): Control | PST | G1: 56.7 ± 10.7 G2: 51.9 ± 7.4 G3: 58.7 ± 0.4) | 3 months daily home exercises | MOGS. PERFECT. MVC by SEMG | G1 and G2 there were no significant differences comparing maximum force and contraction with respect to baseline values. IG1 and G2 resistance improved compared to baseline values. G1 and G2 improved significantly in all variables compared to G3. |
| Au et al. (2019) [25] | PF | 37 | G1 (n = 19): PFMX control G2 (n = 18): APFX | PST | G1: 61.3 ± 7.3 G2: 63.0 ± 8.5 | 26 weeks daily. | HRQOL: FACT-P y PORPUS. IPSS y IIEF-5. VD | Week 26. G1 and G2 improved significantly in continence compared to baseline values. There were no significant differences between groups in functional assessment and quality of life. There were no significant differences in erectile function compared to baseline values or between groups. |
| Moreno-Muñoz et al. (2021) [26] | Postural control and Deep trunk muscles | 117 | G1 (n = 62): AHT G2 (n = 55): Control | Independent consultant | G1: 44.54 ± 10.4 G2: 46.89 ± 6.59 | 8 weeks 2 sessions/week | Stabilometric platform based on the Romberg test. Ultrasound image for TrA activation | G1 improved in all variables related to postural control and TrA activation compared to baseline values and compared to G2. G2 did not obtain significant differences compared to baseline values. |
| Molina-Torres et al. (2022) [27] | UI + PF activation | 117 | G1 (n = 62): AHT G2 (n = 55): control | Independent consultant | G1: 44.54 ± 10.4 G2: 46.89 ± 6.59 | 8 weeks G1: 2 sessions/weekG2: NL | MOGS. PFDI-20. PFIQ-7. ICIQ | In week 26, G1 + G2 improved significantly in continence compared to baseline values. There were no significant differences between groups when measuring UI functional assessment and quality of life. There were no significant differences in erectile function compared to baseline values or between groups. |
| Vicente-Campos et al. (2021) [28] | Diaphragm in NSLBP | 40 | G1 (n = 20): AHT G2 (n = 20): control | PST | G1: 23.25 ± 4.52 G2: 23.90 ± 7.36 | 8 weeks G1: 2 HAG training for week. G2: NL G2 (control): NL | Diaphragm thickness. PImax. NRS. Pain threshold. IPAQ. RMDQ. CSI. TSK-11 | G1 improved significantly compared to G2 in diaphragm thickness, forced inspiration and decreased scores or central sensitization, disability and pain. There were no significant differences between groups in the rest of the variables. Pre-test and post-test measures were not specified. |
| Mitova et al. (2022) [29] | PFD | 47 | G1: Kegel G2: AHT G3: AHT + Kegel | - | G1: 38.53 ± 2.92 G2:39.13 ± 3.09 G3: 39.44 ± 3.12 | 12 weeks G1: Kegel twice daily. G2: AHT 5 times a week G3: combination of both | UDI-6. IIQ-7 and Kiel test for abdominal, back and hip extensor muscles. | All 3 groups obtained improvements in abdominal strength and resistance, gluteal and back muscles with respect to baseline values. Significant improvements in G2 and G3 in abdominal strength and endurance, gluteal and back with respect to g1. There were no significant differences between G2 and G3. Regarding quality of life all groups improved compared to baseline values, but there were no significant differences between groups. 3 groups obtained improvements in continence compared to baseline values, but only G3 obtained significant improvements both with respect to baseline values as with respect to G1 and G2. |
| Authors | Duration | Groups | Learning | Exercise | ||
|---|---|---|---|---|---|---|
| Jose-Vaz et al. (2020) [19] | 24 sess/12 weeks—50′ | AHT |
| First Phase (4 week) | 3 sets of 8 repetitions. 3′ between sets Exercises: 1 SD with flx legs + 1 STG with hands on hips, chest and head + 1 cat position | |
| Second Phase (4 week) | 3 sets of 10 reps. 3′ between sets. Exercises: SD with alternating leg flx + 1 STG with legs in front. Hands on hips, chest and overhead + 1 BPD against Wall. Hands on hips, chest and overhead. | |||||
| Third Phase (4 week) | 3 sets of 12 reps. 3′ between sets. Exercises: 1 on knees+ 1 BPD without support+ 1BPD with flexing the trunk and hand on the Knee. All with hands on hips, chest and above head. | |||||
| EMS | Series of 8/12 contractions close to the maximum PFM holding each one for 6” with ¾ contractions at the top. | First Phase (4 week) | 3 sets of 8 reps, 6” duration and 3 contractions at the top, 1′ between sets. Exercises: 2 SD + 1 STG | |||
| Second Phase (4 week) | 3 sets of 10 reps, 6” duration and 3 contractions at the top, 1′ between sets. Exercises: 1 DS +1 SDT+ 1 BPD | |||||
| Third Phase (4 week) | 3 sets of 12 reps, 6” duration and 4 contractions at the top, 1′ between sets. Exercises: 3 STG + BPD | |||||
| Resende et al. (2012) [20] | 3 month | APFX | 1st date | Information on PF and TrA localization and function. SD with knees in flex., PF localization with a mirror and palpation of the perineum. PF contraction is taught. | 2 sets of 8–10 reps daily, contraction held for 6–8” SD and BPD voluntary contraction of the PF with diaphragmatic aspiration. Daily exercises at home for 3 months. Calls every 2 weeks and monthly appointments. | |
| 2nd date | AHT Learning. Slow DFG inspiration followed by total expiration. Glottic closure and abdominal Wall contraction with diaphragmatic aspiration. | |||||
| 3rd date | Home exercise training. | |||||
| EMSPF | 1st date | Information on PF localization and function. SD with knees in flx, PF localization with a mirror and palpation of the perineum. PF contraction is taught in the expiratory phase. | 3 sets of 8–12 voluntary contractions max held for 6” with 12“of rest between contractions. Then 3 fast contractions in a row. Calls every 2 weeks and monthly appointments. | |||
| 2nd date | Increased PF awareness with vaginal cone; avoiding extraction with voluntary contraction. Stretch reflex by vaginal palpation associated with voluntary PF contraction. | |||||
| 3rd date | Home exercise training. | |||||
| Dierick et al. (2018) [21] | 3 sessions 30′-week for 3 weeks | APFX |
| 3 sets of 8–12 repetitions, BPD exercise, quadruped and SD, with active movements. The sequence of postures is t the discretion of the PST | ||
| BFB EMSPF | Transvaginal electrical stimulation (excitomotor, bidirectional, rectangular, symmetrical current) through vaginal probes, 15′ (450” in right RP and 450” in left RP) BFB lasting 15′ (6” of muscle contraction and 12” of rest). EMS frequency between 20 and 50 Hz Biphasic pulses of 1 ms Intensity at maximum will up to a maximum of 100 mA. | |||||
| Bellido-Fdez et al. (2022) [22] | 8 sessions 30′ in 5 weeks | Masotherapy | Spine-focused massage therapy protocol designed for the soft tissues of the thoracic, lumbar and cervical systems, the entire fascial system and vertebral joints. | |||
| AHT | 6 AHT static abdominals. Each exercise is repeated 3 times in addition to a previous Learning phase and a rest period. | |||||
| AHT + Masotherapy | 4 massage therapy sessions. 4AHT sessions in alternating sessions. | |||||
| Caufriez et al. (2006) [31] | 1 a week for 1hour for 10 weeks | AHT | Self-elongation is requested. The patient must bring the elbows outwards in the direction of the longitudinal axis of the arm. While the hands remain at the level of the iliac crests. The patient is instructed to take a lower costal inhalation in such a way that the lower ribs are raised. Then, a full exhalation is requested. Maintaining self-elongation, and finally, perform an inspiratory movement with the glottis closed, emphasizing the abduction of the shoulder blades. Self-elongation and elevation of the lower ribs. | Each posture is held for 15–30” and repeated 3 times, with 20” rest between exercises. Exercises: BPT with hands pointing forward, BPT trunk inclination, semi-sitting, seated-tailor, knees with hands lateral to the iliac crests, quadruped. SD hands lateral to the iliac crests seated-genupectoral. | ||
| Control | Same positions as AHT but without muscle activation to reduce abdominal pressure. | |||||
| Navarro-Brazález et al. (2020) [30] | 2 sessions of 45’/week—8weeks | EMSPF | PFMX based on Perfect scheme. 10 fast max contractions of 1” each. Hold contraction for 10”. Repeat sequence 10 times. Manual resistance to improve strength and palpation-based feedback. | If a score of <3 was achieved, intravaginal EEM was used for 15’ to improve awareness and PF contraction. SD exercises with manometric probe. | ||
| If a score > 3 was achieved or with a large urogenital hiatus, the dynamometry probe was used. They progressed to manometry once they were able to generate pressure while performing the exercises. If the women progressed sufficiently, the last 2 BFB sessions were performed in a more functional standing position. | ||||||
| The biofeedback system offered different displays to support concentric, isometric and eccentric exercises; specific exercises and timing were adjusted based on the women’s ability and progressed when appropriate. | ||||||
| AHT | Exhale to your expiratory reserve volumen. Then hold your breath (apnea) and expand your rib cage to draw the abdominal Wall inward and cranially without inhaling. Maintain the apnea and expansion of the rib cage for approximately 10”. | 3 reps with a breath rest between reps. 3 times rest between reps. 5–10 exercises within each session. Exercises: BPT, kneeling, kneeling on all fours, STG and SD. Using a variety of upper and lower extremity positions. | ||||
| APFX | Same Learning as in the other groups- | Half of the session in EMSPF and half in AHT. Exercises: 2 SD postures, 1 four-point kneeling and 2 BPT. | ||||
| Collado-Serra (2013) [23] | 3 weeks before prostatectomy and 3 months after. | APFX | AHT: with assessed BFB (with Surface electrodes, periodic PF contractions, 1–3–5”, fast contractions, intense and max strength contractions) and TrA activation. Daily PFMX at home. | |||
| Control | Oral instructions for Kegel exercises. | |||||
| Resende et al. (2010) [24] | 12 weeks | AHT | 1st date | Lifestyle counseling. Information on PF and TrA location and function. Activation of TrA in SD during full expiration. PF contraction is taught. | 2 sets of 8–10 reps daily. Contraction held for 5–8”, 40′ each session. SD and BPT voluntary contraction of the PF with diaphragmatic aspiration. Daily exercises at home for 3 months. | |
| 2nd date | AHT Learning. SD with knees flx., slow DFG inspiration followed by total expiration. Glottic closure and abdominal Wall contraction with DFG aspiration. | |||||
| 3rd date | Home exercise training. | |||||
| EMSPF | 1st date | Lifestyle counseling. Information on PF SD location and function with flexed knees. PF localization with a mirror and palpation of the perineum. PF contraction is taught in the expiratory phase. | 3 sets of 8–12 voluntary contractions of 6” max with 12” rest between contractions. Followed by 3 fast contractions. SD, STG and BPT exercises. | |||
| 2nd date | Increased PF awareness with vaginal cone; avoiding extraction with voluntary contraction. Stretch reflex by vaginal palpation associated with voluntary PF contraction. | |||||
| 3rd date | Home exercise training. | |||||
| Au et al. (2019) [25] | 26 weeks | AHT + FPilates + EMSPF | Protocol published | Increasing progression every 2 weeks. 30 reps/day during weeks 1–2 up to 180 reps during weeks 7–26. | ||
| EMSPF | Instructions to isolate and contract the PF muscles to the maximum. | Increasing progression every 2 weeks. 30 reps per day during weeks 1–2 up to 180 reps in weeks 7–26. | ||||
| Moreno-Muñoz et al. (2021) [26] | 2 sessions of 30′/week—8 weeks. | AHT | First 2 sessions | Low-PressureFitness Protocol Learning respiratory and postural techniques: self-elongation + decoaptation of the glenohumeral + dorsal ankle flexor + overflow of the gravity axis + DGD+ expiratory apnea + costal opening | 3 reps with each posture, changing during the expiratory phase. Expiratory apnea with each posture and after 3 respiratory cycles. | |
| Rest of sessions | Complete progression of postures from BPT to SD. | |||||
| Molina-Torres et al.,(2022) [23] | 2 weekly sessions, 20′/8 weeks | AHT | Postural breathing patterns. Rib cage proprioception, familiarization with apnea and abdominal vaccum. Postural indications: axial lengthening + neutral pelvis + projection of the center of gravity + ankle dorsiflexion + activation of the shoulder girdle. | Dynamic progression of AHT in BPD, STG, quadruped and SD. | ||
| Vicente-Campos et al.,(2021) [28] | 2 sessions/week, 30–40′/8 weeks | AHT |
| 6 AHT separated by 2′ of recovery between them. Each exercise was repeat 3 times. | ||
| Mitova et al. (2022) [29] | 12 weeks Kegel: twice daily. AHT: 45′, 5 times/week. AHT + Kegel: both protocols | Kegel | Kegel Methd. Specific exercises were performed starting from initial positions. | Not specified. | ||
| AHT | Deep breathing in 3 phases. In third, called expiratory apnea, a strong contraction of the abdominal muscles is performed. | |||||
| AHT + Kegel | Both methods were applied. | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernandez-Lucas, P.; Escobio-Prieto, I.; Moro López-Menchero, P. Effects of Hypopressive Techniques on the CORE Complex: A Systematic Review. Healthcare 2025, 13, 1443. https://doi.org/10.3390/healthcare13121443
Hernandez-Lucas P, Escobio-Prieto I, Moro López-Menchero P. Effects of Hypopressive Techniques on the CORE Complex: A Systematic Review. Healthcare. 2025; 13(12):1443. https://doi.org/10.3390/healthcare13121443
Chicago/Turabian StyleHernandez-Lucas, Pablo, Isabel Escobio-Prieto, and Paloma Moro López-Menchero. 2025. "Effects of Hypopressive Techniques on the CORE Complex: A Systematic Review" Healthcare 13, no. 12: 1443. https://doi.org/10.3390/healthcare13121443
APA StyleHernandez-Lucas, P., Escobio-Prieto, I., & Moro López-Menchero, P. (2025). Effects of Hypopressive Techniques on the CORE Complex: A Systematic Review. Healthcare, 13(12), 1443. https://doi.org/10.3390/healthcare13121443






