Abstract
Background: Individuals receiving intensive care are particularly vulnerable to developing pressure sores. This heightened risk necessitates a thorough understanding of relevant risk factors and the time at which these injuries manifest, facilitating effective prevention. Objective: This investigation, structured as a retrospective cohort study, aimed to assess the duration until pressure sore onset and identify contributing risk factors among 50 adult patients in an intensive care unit (ICU), observed over 12 weeks. Methodology: Our analysis employed the Kaplan–Meier approach for survival analysis. We then used the log-rank test to determine significant differences in survival curves. We utilized COX proportional regression analysis to explore the associations between various factors and the development of pressure injuries during the ICU stay. Results: Data from 50 adult ICU patients showed that 29 patients developed pressure sores. Coccyx (44%) and back (6%) were most affected. The median survival time from ICU admission to the final skin examination for pressure sore development was 3 days. The multivariable Cox regression analysis revealed that males with a high BMI, increased systolic blood pressure, elevated albumin levels, and a more extended ICU stay were at a significantly higher risk of developing pressure ulcers (p-value < 0.05). Conclusions: The research highlights the need to prioritize males with high BMI, high blood pressure, and high albumin patients in preventing pressure sores in the ICU, with an extended ICU stay significantly increasing the risk. This information can be utilized to develop clinical guidelines for reducing pressure sore incidence and improving patient care.
1. Introduction
Pressure injuries—also known as pressure ulcers or pressure sores—are areas of localized damage to the skin and underlying tissues, typically caused by prolonged pressure, shear, or friction, especially over bony prominences [1,2]. They are multifactorial in origin, influenced by limited mobility, poor nutrition, moisture imbalance, impaired circulation, and mechanical devices that apply sustained pressure to the skin [3,4]. Contrary to the belief that these injuries develop gradually, they can occur within 2 h of continuous pressure application [5]. The internationally recognized staging system classifies pressure injuries from Stage I to Stage IV, including unstageable lesions and suspected deep tissue injuries, based on the depth and severity of tissue damage [6].
Among hospitalized populations, patients in intensive care units (ICUs) face the highest risk of developing pressure injuries due to immobility, hemodynamic instability, reduced tissue perfusion, impaired oxygenation, and prolonged exposure to medical devices [7,8,9,10]. The increased longevity and complexity of care among critically ill and geriatric patients have also contributed to higher rates of pressure injuries in ICUs globally [11,12,13]. Within the nursing practice domain, pressure sores act as a significant benchmark reflecting the standard of care provided by nurses and the overall proficiency of healthcare practitioners. Nurses are instrumental in proactively averting these lesions and ensuring a swift intervention upon their appearance [14,15,16].
A growing body of literature has explored the epidemiology, risk factors, and outcomes of pressure injuries in ICU settings. Most existing studies have adopted retrospective designs or cross-sectional analyses, often focusing on the prevalence and incidence rates or evaluating isolated risk factors using logistic regression models [6,8,10]. While these studies have provided important insights, they often lack a comprehensive investigation into the cumulative effect of multiple interacting variables, such as survival duration, medical device exposure, and physiological instability, on pressure injury development in critically ill patients. Furthermore, few studies have incorporated time-dependent factors or survival analysis approaches to predict pressure injury risk throughout ICU stay.
This study aimed to address these gaps by investigating the relationship between survival duration and pressure injury development in ICU patients through a robust analytical framework. By integrating clinical and device-related risk factors using multivariate modeling and survival analysis, this research provides a more dynamic understanding of pressure injury risk over time. The findings inform proactive, individualized prevention strategies and enhance nursing care quality in high-risk populations. The study has been built upon existing literature by employing a longitudinal approach that captures the temporal dynamics of pressure injury development. The originality of this research lies in its methodological emphasis on survival duration as a predictive factor, its consideration of multiple coexisting risk factors, and its application within an ICU context. These elements provide a novel contribution to the field and directly support the study’s aim to identify and quantify the effects of survival duration and other risk factors on developing pressure injuries among ICU patients.
2. Materials and Methods
2.1. Study Design and Participants
This retrospective cohort study aimed to investigate the occurrence of pressure injuries among 595 critically ill patients admitted to the adult intensive care unit (ICU) at Mahasarakham Hospital, Thailand, between 1 January 2023 and 31 October 2024. Following the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines, the study was designed and reported to ensure methodological transparency and reproducibility. Data was collected on a single study day, capturing baseline clinical and demographic information. Patients were subsequently followed for 12 weeks to assess the development of pressure injuries, survival status, and length of hospital stay.
The sample size was calculated using G*Power version 3.1, assuming a large effect size of 0.25, an alpha level of 0.05, and a power of 0.95. The required sample size was 49 patients. Sample selection was conducted using simple random sampling by the lottery method from a list of patients who met the eligibility criteria.
Fifty eligible participants included adult patients aged 18 and older admitted to the ICU between 00:00 and 23:59:59 on the designated study day. Inclusion criteria required a minimum ICU stay of three days and the provision of informed consent by either the patient or a legally authorized representative. Patients were excluded if they had severe clinical conditions that precluded participation, if consent was declined, or if the patient died during the study period.
2.2. Data Collection
Data collection was conducted on 1 January 2023. Anonymous patient information was obtained using standardized case report forms, which included data extracted from electronic medical records from HOSxP (Hospital Information System) within the first three days of ICU admission. Collected variables encompassed demographic characteristics, admission details, and physiological parameters relevant to the study day. Disease severity was assessed using the Simplified Acute Physiology Score II (SAPS II) (AUC = 0.85) [17,18]. Pressure injuries were systematically recorded through direct clinical observation, following internationally recognized staging definitions [6]. Pressure injury risk was evaluated using the Braden Scale, which consists of six subscales—mobility, activity, sensory perception, skin moisture, nutritional status, and friction/shear—with lower scores indicating higher risk (AUC = 0.82) [19,20]. While the SAPS II and Braden Scale are widely used internationally, their use in this study included content validation by three experts for relevance and appropriateness in the Thai clinical context. However, formal cross-cultural validation or psychometric testing in the Thai population was not established and is acknowledged as a limitation.
This study’s staging of pressure ulcers followed the classification system established by the National Pressure Ulcer Advisory Panel (NPUAP), which categorizes pressure injuries into six stages, including device-related and mucosal membrane pressure injuries. Assessments were conducted collaboratively by experienced ICU nurses and attending physicians to ensure accuracy and consistency. Follow-up data were collected on survival status, length of ICU stay, and overall hospital stay, either until discharge or up to 12 weeks post-admission. To ensure consistency and accuracy in pressure injury assessment, a training module—accompanied by a self-assessment tool based on international staging definitions [6]—was developed and included in the official study guidelines. This module underwent content validation by three experts before the study’s commencement. All registered data collectors were instructed and encouraged to thoroughly review the training materials before participating in the data collection process.
2.3. Data Management
The reported data underwent a thorough evaluation for its quality and integrity. Any missing values that appeared extreme or seemed unlikely were cross-referenced directly with the patients’ medical records. If the data still raised concerns, the principal investigator made the final decision regarding its inclusion in the study, reaching a consensus with the team. Missing values deemed suitable for inclusion through this agreement were either filled in using median values or inferred from other existing variables. Any remaining missing values were then excluded from the final analyses.
2.4. Statistical Analysis
The statistical analyses were conducted at the individual patient level. To determine the proportion of pressure sores occurring in the ICU on the study day, we calculated the percentage of patients with at least one pressure injury. Continuous data were summarized using the median and interquartile range (IQR), while categorical data were presented as counts (n) and percentages (%). Univariate analyses were conducted using appropriate statistical tests, including the Chi-square test, Exact test, Mann–Whitney U test, and Kruskal–Wallis test. Survival analysis was conducted using the Kaplan–Meier procedure, and the log-rank test was used to assess differences in survival curves. COX proportional regression analysis was employed to examine associations with ICU-acquired pressure injuries. All variables were included in the analysis, regardless of their results in the univariate analysis. The results are reported as hazard ratios (HRs) with corresponding 95% confidence intervals (CIs). The statistical analysis was performed using IBM SPSS version 25.0, licensed by Mahasarakham University.
2.5. Ethical Considerations and Informed Consent
This research was approved by the Human Research Ethics Committee at Mahasarakham University, with accreditation number 419-383/2565. Before inclusion in the study, the relatives of patients in the sample were informed about the study’s objectives. They were asked to provide voluntary informed consent to participate, with the option to decline participation at any time. The collected data will be treated confidentially, ensuring that respondents remain anonymous, and the results will be presented in a manner that preserves their anonymity. All research procedures were conducted in compliance with relevant guidelines and regulations.
3. Results
3.1. Demographic Characteristics and Health Condition
The study’s participant pool was predominantly male, accounting for 76.00% of the cohort, with an average age of 56.74 ± 11.53 years. Their mean body mass index (BMI) was 22.16 ± 4.53 kg/m2. A key characteristic was that every participant (100.00%) required mechanical ventilation and received complete medical and nursing care. Clinical observations showed an average temperature of 37.89 ± 0.94 °C. Blood pressure readings indicated a mean systolic pressure of 126.00 ± 27.91 mmHg and a mean diastolic pressure of 72.70 ± 16.39 mmHg. The mean arterial pressure (MAP) averaged 87.26 ± 16.10 mmHg, with a remarkable 98.00% of individuals falling within the typical normal range of 65.00–110.00 mmHg. Beyond physiological measures, the participants generally exhibited good health habits and functional status. Most reported good sleep quality (60.00%), and all were non-smokers (100.00%). Regular bowel movements, specifically once per day, were reported by 76.00% of participants. A significant majority received standard inotropic support (58.0%), displayed normal respiratory mechanics (86.0%), and maintained complete independence in their activities of daily living (ADLs) (100.0%). Regarding pre-existing health conditions, diabetes mellitus (DM) was the most common, affecting 30.00% of participants, followed by hypertension (HT) at 24.00%. Importantly, no cases of edema, urinary incontinence, additional comorbidities, or any alterations in the level of consciousness (LOC) were found in this study group.
An assessment of pressure sore classification using the Barden score indicated that most were grade 2 (28.00%), followed by grade 1 (22.00%) and grade 3 (8.00%). The average duration of ICU admission was 7.60 ± 8.03 days. Most participants (74.00%) had an ICU stay of less than 9 days. The average time for a pressure sore to develop was 3.66 ± 4.90 days. Furthermore, most participants presented with abnormal albumin levels (92.00%), either above 5.00 gm/dL or below 3.50 gm/dL. Abnormal hemoglobin levels (below 11.00 g/dL) were also noted in 58.00% of cases. Detailed information is presented in Table 1.

Table 1.
Characteristics and health conditions of the participants.
3.2. Location of Pressure Sore
An analysis of pressure sore locations showed the coccyx was most frequently affected, appearing in 44% of patients. Less common sites for these lesions included the back (6%) and the hip (2%), as detailed in Figure 1.
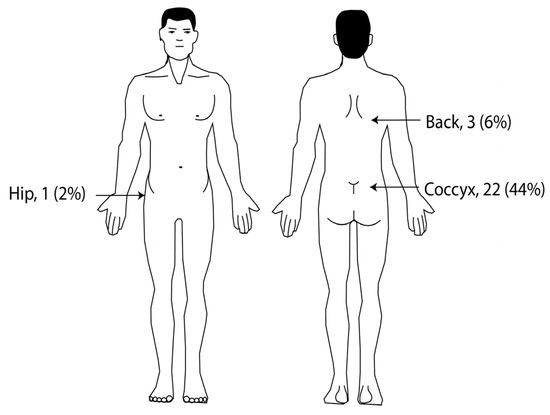
Figure 1.
Anatomical locations of pressure sores in ICU patients (n = 50).
3.3. Survival Time of Pressure Sore Development
The comprehensive survival analysis for pressure sore development in ICU patients indicated a median survival time of 3 days (95% CI = 2.04 to 3.96). While males exhibited a shorter median time to pressure sore development at 3 days (95% CI = 2.28 to 3.72), compared to females at 5 days (95% CI = 4.18 to 5.82), this difference was not statistically significant (p-value = 0.389) at the α ≤ 0.05 level, as illustrated in Table 2 and Figure 2.

Table 2.
Survival time comparison between males and females.
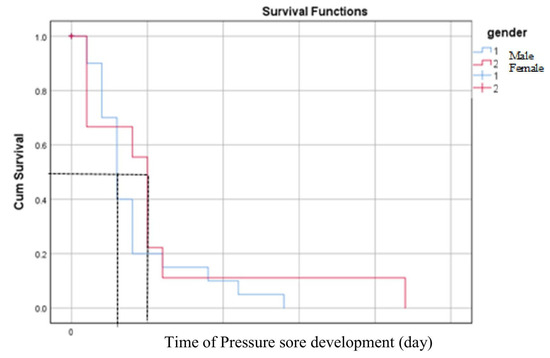
Figure 2.
Medians for survival time of pressure sore development comparison between male and female. The black dashed lines indicate the median day of survival time for pressure sore development.
3.4. Comparative Analysis of Survival Time for Pressure Sore Development at the Mean of Covariates
The results showed that pressure sore stage 3 has a longer median survival time of 5 days, stage 2 exhibited a median survival time of 4 days, while stage 1 had a shorter median survival time (3 days, 95% CI, 1.49 to 4.51 days). However, this difference is not statistically significant at a p-value ≤ 0.05, as shown in Figure 3.
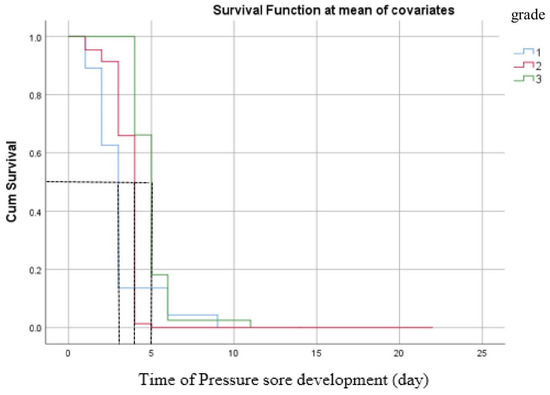
Figure 3.
Survival time of pressure sore development at the mean of covariates. The black dashed lines indicate the median day of survival time for pressure sore development.
3.5. Multivariable Analysis of Risk Factors for Pressure Sores Development
The study employed multivariable Cox proportional regression with the Backward method to assess the risk factors associated with pressure sore development in adult ICU patients. Several of the fourteen factors analyzed differed significantly between the two groups, with p-values ≤ 0.25. These factors included age (years), gender, body mass index (BMI, kg/m2), temperature (°C), systolic blood pressure (mmHg), diastolic blood pressure (mmHg), mean arterial pressure (MAP, mmHg), presence of diabetes mellitus (DM), hypertension (HT), serum albumin (g/dL), hemoglobin level (g/dL), and length of ICU stay (<9 days vs. ≥9 days).
The results indicated that males exhibited a statistically significant hazard ratio for pressure sore development, which was four times higher (95% CI = 1.25 to 12.10) than that of females. BMI also demonstrated a statistically significant hazard ratio for pressure sore development, with a 1 kg/m2 increase associated with a 0.22 times higher hazard ratio at a p-value of 0.001. Systolic blood pressure showed a statistically significant hazard ratio for pressure sore development; a 1 mmHg increase was associated with a 0.04 times lower hazard ratio at a p-value of 0.003. Albumin displayed a statistically significant hazard ratio for pressure sore development, with a 1 gm/dL increase associated with a 1.15 times higher hazard ratio at a p-value of 0.001. Moreover, a length of stay in the ICU of 9 days or more exhibited a statistically significant hazard ratio for pressure sore development, which was 8.27 times higher (95% CI = 2.42 to 28.28) compared to those with a length of stay in the ICU of less than 9 days (p-value = 0.001). However, age, diastolic blood pressure, mean arterial pressure (MAP), diabetes (DM), hypertension (HT), and hemoglobin were not statistically significant for pressure sore development in ICU patients, as presented in Table 3.

Table 3.
Hazard factors of pressure sores among ICU patients by multivariable Cox proportional regression.
4. Discussion
This retrospective cohort study evaluated the time to onset of pressure sores and associated risk factors in a cohort of 50 adult ICU patients over a 12-week interval. We found that most ICU patients with pressure ulcers were older, which was not statistically significant compared to prior studies, potentially due to varied patient populations and care. Secondly, incomplete data on comorbidities limited the study, but being male significantly increased pressure sore risk, and surprisingly, higher BMI showed a slight increase in risk, opposing previous findings. Thirdly, longer ICU stays and albumin were significant risk factors for pressure sores, though diabetes and hypertension did not show a direct, independent effect on development time. Fourthly, despite prior research linking prolonged mechanical ventilation to pressure sores, this study, where all patients were ventilated, found no statistically significant association. Lastly, pressure sores developed in a median of 3 days, with a non-significant trend towards faster development in males and stage 1 ulcers, contrasting with a larger study’s significant stage-based differences.
This study showed that most ICU patients with pressure ulcers were older adults, although this difference was not statistically significant compared to those without pressure ulcers. This finding contradicts previous studies that reported older age as a risk factor for pressure sores in ICU patients [3,19,21]. These discrepancies in results may stem from the inclusion of younger patients in this study, variations in patient care procedures, cultural factors, and differences in study sizes. Older age independently correlated with the occurrence of pressure sores. The progressively rising proportion of very old residents represents a conspicuous influx of high-risk patients, characterized by the accumulation of chronic comorbidities, nutritional deficiencies, immobility, and aging skin [22,23]. However, this study’s documentation of comorbidities, dietary deficiencies, and immobility was incomplete. Males exhibited a statistically significant hazard ratio for pressure sore development, four times higher than females. This result was similar to the previous study. However, this study showed that a 1 kg/m2 increase in BMI increased the risk of pressure sore development by 0.22 times; this result was in contrast to previous studies, which reported that lower or decreased body weight was significantly associated with pressure sore development [3,19].
These findings concerning the health condition of ICU patients indicated that the length of ICU stays exceeding 9 days, increases in BMI, systolic blood pressure, and albumin levels, as well as masculinity, were statistically significant risk factors for pressure sore development. This outcome aligns with prior studies that highlighted that an extended ICU stay, along with factors such as diabetes, hypertension, and cardiovascular disease, increased the likelihood of pressure sore development among ICU patients [24,25]. However, this study did not establish a direct association between underlying conditions such as diabetes mellitus (DM) and hypertension (HT) and the development of pressure ulcers, as all patients with DM and HT developed pressure sores. Nevertheless, after adjusting for confounding factors using multivariable Cox regression analysis, neither DM nor HT emerged as significant hazards influencing the time to pressure sore development.
The treatment of critical patients in the ICU, including mechanical ventilation, the use of vasopressors, and sedative drugs, has been identified as a potential risk factor for pressure sore development, as reported in previous studies [26,27]. Research on mechanical ventilation has highlighted that using a ventilator for 10 h significantly impacts the occurrence of pressure sores [27]. However, this study’s results indicated that all ICU patients were on ventilators and did not show a statistically significant association with pressure sore development. This discrepancy could stem from patient conditions or variations in patient care procedures.
The overall median survival time for the development of pressure sores was 3 days. Males exhibited a shorter survival time for the development of pressure sores than females, although this difference was not statistically significant. The Kaplan–Meier analysis revealed that the survival time for pressure sore development in stage 1 was shorter than in other stages; however, this difference did not reach statistical significance. This contrasts with a more extensive previous study, which reported statistically significant differences in survival time for pressure sores across different stages using a log-rank test [19]. These variations in results may be attributed to differences in patient care procedures, cultural factors, and variations in study sizes.
5. The Strengths and Limitations of the Study
This study has several limitations. First, the data represent only a single point in time [20] and do not account for potentially influential factors such as staffing levels. Second, the generalizability of the findings is limited, as the study was conducted in a single hospital in Northeastern Thailand, which may not represent other geographic areas. Third, assessing pressure sore staging is inherently challenging; reliance on medical records and assistant nurses’ documentation may introduce uncertainty in tissue assessments. Although efforts were made to ensure consistency through standardized data collection procedures and training, some variability and bias may have occurred. Lastly, the small sample size and single-center design limit the ability to generalize the findings and preclude causal inference.
The strength of this study lies in its identification of foundational risk factors associated with the development of pressure sores. The findings provide essential evidence to support initiatives to address this critical patient safety issue and offer baseline data relevant for local and regional quality improvement efforts. Importantly, pressure sore staging was assessed through direct skin inspection—the gold standard—by trained outcome assessors, ensuring the reliability of outcome classification. The study was conducted following a rigorous protocol, with meticulous attention to standardization of data collection procedures. These results contribute valuable insight into risk stratification among ICU patients and may inform the development of clinical practice guidelines. Further studies involving larger and more heterogeneous populations are warranted to explore potential causal relationships.
6. Conclusions
Overall, this study offers several notable benefits. It precisely identifies that pressure sores typically develop within a median of just 3 days for ICU patients. This finding provides vital intelligence, allowing medical staff to address and manage this complication preemptively. The finding that males face a heightened risk, evidenced by a gender-based disparity in pressure sore development time, provides critical guidance for tailoring prevention strategies. Furthermore, pinpointing the coccyx as the most common site for these sores helps healthcare providers concentrate their preventative actions more effectively. Finally, the finding that patients staying in the ICU for nine days or longer have a significantly higher likelihood of developing pressure sores informs the deployment of more focused and proactive care strategies.
Author Contributions
Conceptualization, W.P. and S.K.; methodology, W.P., S.K., T.S., C.S., K.S., J.R., L.K.N., and K.T.; software, W.P., S.K., T.S., C.S., K.S., and K.T.; validation, W.P., S.K., T.S., C.S., K.S., J.R., L.K.N., and K.T.; formal analysis, W.P., S.K., T.S., C.S., K.S., and J.R.; investigation, W.P., S.K., T.S., C.S., K.S., J.R., L.K.N., and K.T.; resources, W.P., S.K., T.S., C.S., K.S., and J.R.; data curation, W.P., S.K., T.S., C.S., K.S., J.R., L.K.N., and K.T.; writing—original draft preparation, W.P. and S.K.; writing—review and editing, W.P., S.K., T.S., C.S., K.S., J.R., L.K.N., and K.T.; visualization, W.P. and K.T.; supervision, S.K.; project administration, W.P. and S.K.; funding acquisition, S.K. and K.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research project was financially supported by Mahasarakham University: Fast track 2025.
Institutional Review Board Statement
The study was conducted in accordance with the principles of human research ethics. Ethical approval was obtained from the Human Research Ethics Committee at Mahasarakham University, with accreditation number 419-383/2565, 28 December 2022.
Informed Consent Statement
Written informed consent has been obtained from the participants to publish this paper.
Data Availability Statement
Data are available upon request.
Acknowledgments
We extend our heartfelt gratitude to all the participants who contributed to this study. The support for this research was graciously provided by Mahasarakham Hospital and Faculty of Public Health, Mahasarakham University, Thailand.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gefen, A.; Brienza, D.M.; Cuddigan, J.; Haesler, E.; Kottner, J. Our contemporary understanding of the aetiology of pressure ulcers/pressure injuries. Int. Wound J. 2022, 19, 692–704. [Google Scholar] [CrossRef]
- Zaidi, S.R.H.; Sharma, S. Pressure Ulcer. In StatPearls; National Institutes of Health: Treasure Island, FL, USA, 2025. [Google Scholar]
- Chung, M.-L.; Widdel, M.; Kirchhoff, J.; Sellin, J.; Jelali, M.; Geiser, F.; Muecke, M.; Conrad, R. Risk factors for pressure injuries in adult patients: A narrative synthesis. Int. J. Environ. Res. Public Health 2022, 19, 761. [Google Scholar] [CrossRef] [PubMed]
- Williams, L. At a glance: Pressure injuries. Br. J. Nurs. 2024, 33, S24–S30. [Google Scholar] [CrossRef]
- Rochester, A. Quality improvement project to reduce the incidence of nasal bridge pressure sores in adults requiring acute non-invasive ventilation (NIV) and continuous positive airway pressure (CPAP). BMJ Open Qual. 2025, 14, e003238. [Google Scholar] [CrossRef] [PubMed]
- Headlam, J.; Illsley, A. Pressure ulcers: An overview. Br. J. Hosp. Med. 2020, 81, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.K.; Hahn, H.M.; Park, D.H. Factors influencing the severity of medical device-related pressure injuries: Pressure injury staging comparison. Int. Wound J. 2023, 20, 2735–2741. [Google Scholar] [CrossRef]
- Ziegler, S.; Schmoor, C.; Scholer, L.M.; Schepputat, S.; Takem, E.; Grotejohann, B.; Steinbrenner, I.; Feuchtinger, J. Potential for reducing immobility times of a mobility monitor in-bed sensor system—A stepped-wedge cluster-randomised trial. BMC Nurs. 2023, 22, 478. [Google Scholar] [CrossRef]
- Efteli, E.; Gunes, U. Assessing the Validity and Reliability of a New Pressure Ulcer Risk Assessment Scale for Patients in Intensive Care Units. Wound Manag. Prev. 2020, 66, 24–33. [Google Scholar] [CrossRef]
- Ribeiro, R.N.; Oliveira, D.V.; Paiva, W.S.; Sousa, R.M.C.; Vieira, R.C.A. Incidence of pressure injury in patients with moderate and severe traumatic brain injury: A systematic review. BMJ Open 2024, 14, e089243. [Google Scholar] [CrossRef]
- Alshahrani, B.; Middleton, R.; Rolls, K.; Sim, J. Pressure injury prevalence in critical care settings: An observational pre-post intervention study. Nurs. Open 2024, 11, e2110. [Google Scholar] [CrossRef]
- Gökdemir, S.; Aslan, M. Main Factors Regarding Pressure Injury in Intensive Care Unit Patients and the Effects of Nursing Interventions. Turk. J. Intensive Care 2024, 22, 31–40. [Google Scholar] [CrossRef]
- Fulbrook, P.; Lovegrove, J.; Hay, K.; Coyer, F. State-wide prevalence of pressure injury in intensive care versus acute general patients: A five-year analysis. J. Clin. Nurs. 2023, 32, 4947–4961. [Google Scholar] [CrossRef] [PubMed]
- Al-Qudimat, A.R.; Maabreh, A.H.; Shtayat, H.; Khaleel, M.A.; Allatayfeh, J.M.; Iblasi, A.S. Prevention of pressure injuries and nursing interventions in critical care settings: A synthesis without Meta-analysis (SWiM). Chronic Wound Care Manag. Res. 2024, 11, 13–30. [Google Scholar] [CrossRef]
- Tervo-Heikkinen, T.; Heikkilä, A.; Koivunen, M.; Kortteisto, T.; Peltokoski, J.; Salmela, S.; Sankelo, M.; Ylitörmänen, T.; Junttila, K. Nursing interventions in preventing pressure injuries in acute inpatient care: A cross-sectional national study. BMC Nurs. 2023, 22, 198. [Google Scholar] [CrossRef]
- Alshahrani, B.; Sim, J.; Middleton, R. Nursing interventions for pressure injury prevention among critically ill patients: A systematic review. J. Clin. Nurs. 2021, 30, 2151–2168. [Google Scholar] [CrossRef]
- Auriant, I.; Vinatier, I.; Thaler, F.; Tourneur, M.; Loirat, P. Simplified acute physiology score II for measuring severity of illness in intermediate care units. Crit. Care Med. 1998, 26, 1368–1371. [Google Scholar] [CrossRef] [PubMed]
- Sala, J.J.; Mayampurath, A.; Solmos, S.; Vonderheid, S.C.; Banas, M.; D’Souza, A.; LaFond, C. Predictors of pressure injury development in critically ill adults: A retrospective cohort study. Intensive Crit. Care Nurs. 2021, 62, 102924. [Google Scholar] [CrossRef]
- Labeau, S.O.; Afonso, E.; Benbenishty, J.; Blackwood, B.; Boulanger, C.; Brett, S.J.; Calvino-Gunther, S.; Chaboyer, W.; Coyer, F.; Deschepper, M.; et al. Prevalence, associated factors and outcomes of pressure injuries in adult intensive care unit patients: The DecubICUs study. Intensive Care Med. 2021, 47, 160–169. [Google Scholar] [CrossRef]
- Huang, C.; Ma, Y.; Wang, C.; Jiang, M.; Yuet Foon, L.; Lv, L.; Han, L. Predictive validity of the braden scale for pressure injury risk assessment in adults: A systematic review and meta-analysis. Nurs. Open 2021, 8, 2194–2207. [Google Scholar] [CrossRef]
- Cremasco, M.F.; Whitaker, I.Y. Risk factors for pressure ulcers development in intensive care unit patients. Rev. Cuid. 2021, 12, e1196. [Google Scholar]
- Brunker, L.B.; Boncyk, C.S.; Rengel, K.F.; Hughes, C.G. Elderly Patients and Management in Intensive Care Units (ICU): Clinical Challenges. Clin. Interv. Aging 2023, 18, 93–112. [Google Scholar] [CrossRef] [PubMed]
- Feng, M.; Liu, Y.; Li, Q.; Yang, X.; Wei, F.; Cheng, H.; Lyu, J.; Lin, Q. Association between geriatric nutritional risk index and adverse outcomes in critical ill patients with chronic obstructive pulmonary disease: A cohort study of 2824 older adults. BMC Pulm. Med. 2024, 24, 634. [Google Scholar] [CrossRef]
- Oliveira, B.A.d.; Zanchetta, F.C.; Barbieri, B.; Falcioni, C.A.S.; Araújo, E.P.D.; Lima, M.H.M. Point prevalence and risk factors for pressure ulcers in hospitalized adult patients: A cross-sectional study. Einstein 2024, 22, eAO0811. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhou, W.; Du, H. Association between hypertension and pressure ulcer: A systematic review and meta-analysis. Int. Wound J. 2024, 21, e14829. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Fan, J.; Chen, L.; Xie, L.; Huang, L.; Ruan, Y.; Xu, X.; Liang, Z. Strategies to preventing pressure injuries among intensive care unit patients mechanically ventilated in prone position: A systematic review and a Delphi study. Front. Med. 2023, 10, 1131270. [Google Scholar] [CrossRef]
- Karahan, E.; Çelik, S.; Uçar, Ö. Incidence of pressure ulcers in the patients on mechanical ventilation: A prospective study. J. Contemp. Med. 2020, 10, 62–69. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).