Identifying Areas with Low Access to the COVID-19 Vaccine: A New Objective Framework Incorporating Mobility Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Population and Vaccine Provider Data
2.2. Road Network Data
2.3. SafeGraph Mobility Data
2.4. Adapted USDA Low-Access Definition
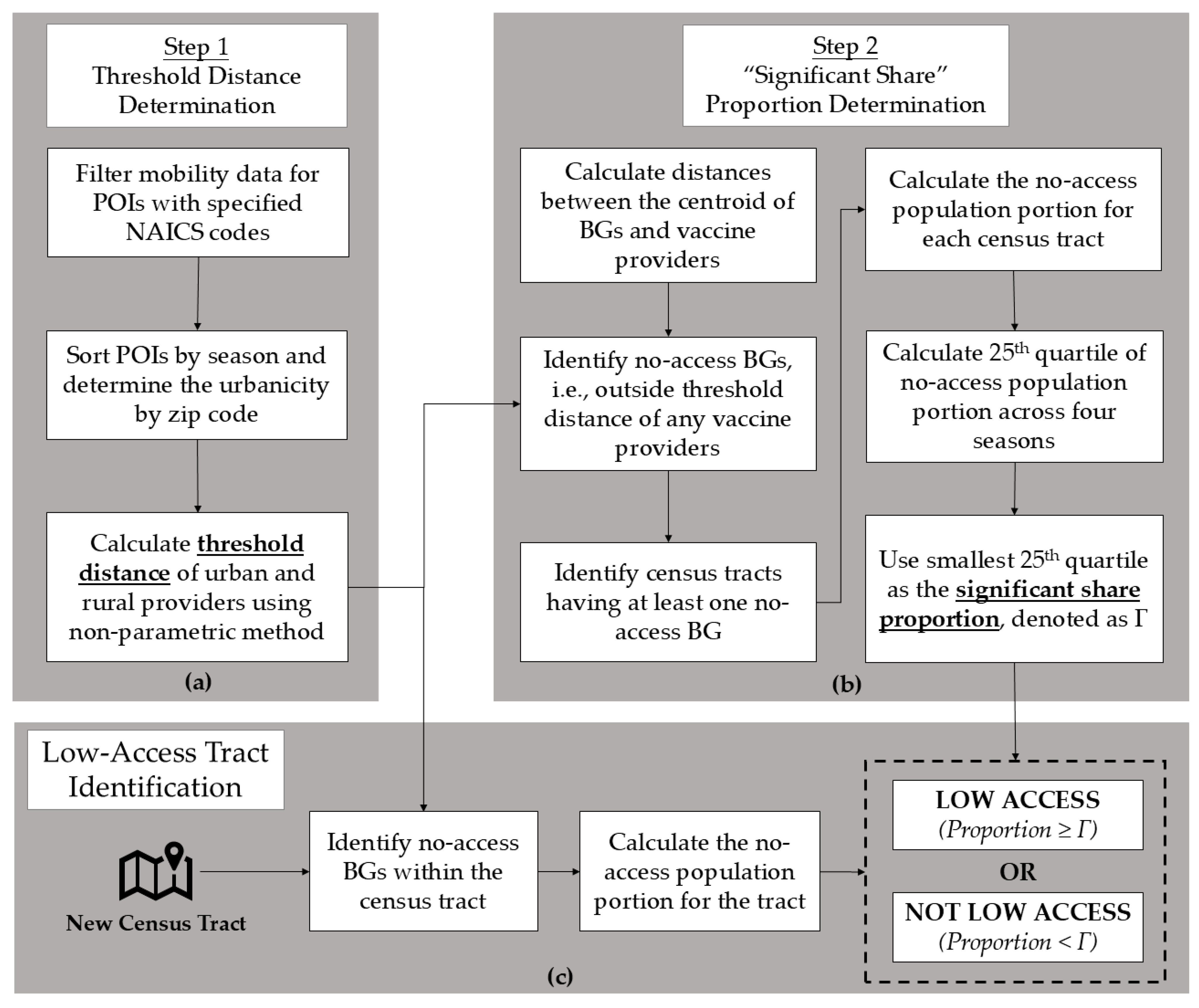
2.5. Mobility Data-Driven Definition
- Step 1: Calculate the threshold distance
- Step 2: Determine the “significant share” of a population
2.6. Evaluation Metrics
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- COVID-19 Cases|WHO COVID-19 Dashboard. Datadot 2023. Available online: https://data.who.int/dashboards/covid19/cases (accessed on 1 March 2025).
- COVID-19 Deaths|WHO COVID-19 Dashboard. Datadot 2023. Available online: https://data.who.int/dashboards/covid19/deaths?n=o (accessed on 1 March 2025).
- COVID-19 Vaccine Effectiveness Monthly Update. Centers for Disease Control and Prevention. 2022. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccine-effectiveness (accessed on 13 February 2023).
- DiRago, N.V.; Li, M.; Tom, T.; Schupmann, W.; Carrillo, Y.; Carey, C.M.; Gaddis, S.M. COVID-19 Vaccine Rollouts and the Reproduction of Urban Spatial Inequality: Disparities Within Large US Cities in March and April 2021 by Racial/Ethnic and Socioeconomic Composition. J. Urban Health 2022, 99, 191–207. [Google Scholar] [CrossRef] [PubMed]
- Jean-Jacques, M.; Bauchner, H. Vaccine Distribution—Equity Left Behind? JAMA 2021, 325, 829–830. [Google Scholar] [CrossRef] [PubMed]
- Hardeman, A.; Wong, T.; Denson, J.L.; Postelnicu, R.; Rojas, J.C. Evaluation of Health Equity in COVID-19 Vaccine Distribution Plans in the United States. JAMA Netw. Open 2021, 4, e2115653. [Google Scholar] [CrossRef] [PubMed]
- Murthy, B.P.; Sterrett, N.; Weller, D.; Zell, E.; Reynolds, L.; Toblin, R.L.; Murthy, N.; Kriss, J.; Rose, C.; Cadwell, B.; et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, December 14, 2020–April 10, 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 759–764. [Google Scholar] [CrossRef]
- Pressman, A.R.; Lockhart, S.H.; Shen, Z.; Azar, K.M.J. Measuring and Promoting SARS-CoV-2 Vaccine Equity: Development of a COVID-19 Vaccine Equity Index. Health Equity 2021, 5, 476–483. [Google Scholar] [CrossRef]
- Saelee, R.; MStat, E.; Murthy, B.; Castro-Roman, P.; Fast, H.; Meng, L. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, December 14, 2020–January 31, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 335–340. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Food Access Research Atlas Documentation. U.S. Department of Agriculture. Economic Research Service. 2022. Available online: https://www.ers.usda.gov/data-products/food-access-research-atlas/documentation/ (accessed on 13 February 2023).
- Wisseh, C.; Hildreth, K.; Marshall, J.; Tanner, A.; Bazargan, M.; Robinson, P. Social Determinants of Pharmacy Deserts in Los Angeles County. J. Racial Ethn. Health Disparities 2021, 8, 1424–1434. [Google Scholar] [CrossRef]
- Qato, D.M.; Daviglus, M.L.; Wilder, J.; Lee, T.; Qato, D.; Lambert, B. ‘Pharmacy Deserts’ Are Prevalent in Chicago’s Predominantly Minority Communities, Raising Medication Access Concerns. Health Aff. 2014, 33, 1958–1965. [Google Scholar] [CrossRef]
- Pednekar, P.; Peterson, A. Mapping pharmacy deserts and determining accessibility to community pharmacy services for elderly enrolled in a State Pharmaceutical Assistance Program. PLoS ONE 2018, 13, e0198173. [Google Scholar] [CrossRef]
- Tao, Z.; Cheng, Y.; Zheng, Q.; Li, G. Measuring spatial accessibility to healthcare services with constraint of administrative boundary: A case study of Yanqing District, Beijing, China. Int. J. Equity Health 2018, 17, 7. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measures of Spatial Accessibility to Health Care in a GIS Environment: Synthesis and a Case Study in the Chicago Region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 1100–1107. [Google Scholar] [CrossRef]
- Dai, D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place 2010, 16, 1038–1052. [Google Scholar] [CrossRef]
- Bemanian, A.; Mosser, J.F. Investigating the Spatial Accessibility and Coverage of the Pediatric COVID-19 Vaccine: An Ecologic Study of Regional Health Data. Vaccines 2024, 12, 545. [Google Scholar] [CrossRef] [PubMed]
- Xia, Y.; Chen, H.; Zuo, C.; Zhang, N. The impact of traffic on equality of urban healthcare service accessibility: A case study in Wuhan, China. Sustain. Cities Soc. 2022, 86, 104130. [Google Scholar] [CrossRef]
- Luo, W.; Whippo, T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place 2012, 18, 789–795. [Google Scholar] [CrossRef]
- Cao, Y.; Li, T.; Chen, H.; Zhao, Q.; Sun, J.; Grépin, K.A.; Kang, J.-Y. Evaluating geographic accessibility to COVID-19 vaccination across 54 countries/regions. BMJ Glob. Health 2025, 10, e017761. [Google Scholar] [CrossRef]
- Rader, B.; Astley, C.M.; Sewalk, K.; Delamater, P.L.; Cordiano, K.; Wronski, L.; Rivera, J.M.; Hallberg, K.; Pera, M.F.; Cantor, J.; et al. Spatial modeling of vaccine deserts as barriers to controlling SARS-CoV-2. Commun. Med. 2022, 2, 141. [Google Scholar] [CrossRef]
- Brenner, P.S.; DeLamater, J. Lies, Damned Lies, and Survey Self-Reports? Identity as a Cause of Measurement Bias. Soc. Psychol. Q. 2016, 79, 333–354. [Google Scholar] [CrossRef]
- Allan, D.P. Catchments of general practice in different countries—A literature review. Int. J. Health Geogr. 2014, 13, 32. [Google Scholar] [CrossRef]
- Census Bureau Data. US Census Bureau. 2017. Available online: https://data.census.gov/ (accessed on 13 February 2023).
- TIGER/Line® Shapefiles. US Census Bureau. 2022. Available online: https://www.census.gov/cgi-bin/geo/shapefiles/index.php (accessed on 13 February 2023).
- Rural-Urban Commuting Area Codes. U.S. Department of Agriculture. Economic Research Service. 2020. Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx (accessed on 13 February 2023).
- Oregon Rural-Urban Commuting Areas. Oregon Health & Science University. 2014. Available online: https://www.ohsu.edu/oregon-office-of-rural-health/about-rural-and-frontier-data (accessed on 13 February 2023).
- ALERT Immunization Information System. Oregon Health Authority. 2020. Available online: https://www.alertiis.org/ORPRD/portalInfoManager.do (accessed on 13 February 2023).
- Grabenstein, J.D. Essential services: Quantifying the contributions of America’s pharmacists in COVID-19 clinical interventions. J. Am. Pharm. Assoc. 2022, 62, 1929–1945.e1. [Google Scholar] [CrossRef] [PubMed]
- Management of Anaphylaxis at COVID-19 Vaccination Sites|CDC. 2025. Available online: https://www.cdc.gov/vaccines/covid-19/clinical-considerations/managing-anaphylaxis.html (accessed on 30 May 2025).
- Oregon Health Authority. OHA Powerpoint for Press Conference 2021. Available online: https://www.oregon.gov/oha/ERD/Documents/OHA%20Powerpoint%20for%20Press%20Conference%202.26.21.pdf (accessed on 20 May 2025).
- OSRM API Documentation. Open Source Routing Machine. 2017. Available online: http://project-osrm.org/docs/v5.24.0/api/# (accessed on 13 February 2023).
- Juhász, L.; Hochmair, H. Studying Spatial and Temporal Visitation Patterns of Points of Interest Using SafeGraph Data in Florida. GIForum 2020, 8, 119–136. [Google Scholar] [CrossRef]
- Weekly Patterns|SafeGraph Docs. SafeGraph n.d. Available online: https://docs.safegraph.com/docs/weekly-patterns (accessed on 19 May 2025).
- Klise, K.; Beyeler, W.; Finley, P.; Makvandi, M. Analysis of mobility data to build contact networks for COVID-19. PLoS ONE 2021, 16, e0249726. [Google Scholar] [CrossRef] [PubMed]
- Moreland, A.; Christine, H.; Michael, T.; Gregory, S.; McCord, R.F.; Hilton, C. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement—United States, March 1–May 31, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1198–1203. [Google Scholar] [CrossRef]
- Gottumukkala, R.; Katragadda, S.; Bhupatiraju, R.T.; Kamal, A.M.; Raghavan, V.; Chu, H.; Kolluru, R.; Ashkar, Z. Exploring the relationship between mobility and COVID− 19 infection rates for the second peak in the United States using phase-wise association. BMC Public Health 2021, 21, 1669. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.; Newberger, N.; Smalling, S. The spread of social distancing. Econ. Lett. 2020, 196, 109511. [Google Scholar] [CrossRef] [PubMed]
- North American Industry Classification System (NAICS). US Census Bureau. 2022. Available online: https://www.census.gov/naics/ (accessed on 13 February 2023).
- Boddy, R.; Smith, G. Statistical Methods in Practice: For Scientists and Technologists; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2009; ISBN 978-0-470-74664-6. [Google Scholar]
- Gade, K. A Non-singular Horizontal Position Representation. J. Navig. 2010, 63, 395–417. [Google Scholar] [CrossRef]
- Lopez, L.; Hart, L.H.; Katz, M.H. Racial and Ethnic Health Disparities Related to COVID-19. JAMA 2021, 325, 719. [Google Scholar] [CrossRef]
- Webb Hooper, M.; Nápoles, A.M.; Pérez-Stable, E.J. COVID-19 and Racial/Ethnic Disparities. JAMA 2020, 323, 2466. [Google Scholar] [CrossRef]
- Mackey, K.; Ayers, C.K.; Kondo, K.K.; Saha, S.; Advani, S.M.; Young, S.; Spencer, H.; Rusek, M.; Anderson, J.; Veazie, S.; et al. Racial and Ethnic Disparities in COVID-19–Related Infections, Hospitalizations, and Deaths. Ann. Intern. Med. 2021, 174, 362–373. [Google Scholar] [CrossRef]
- COVID-19 Vaccine Equity for Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. 2022. Available online: https://archive.cdc.gov/#/details?url=https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/vaccine-equity.html (accessed on 13 February 2023).
- Weiss, A.; Pickens, G.; Roemer, M. Methods for Calculating Patient Travel Distance to Hospital in HCUP Data. Available online: https://hcup-us.ahrq.gov/reports/methods/MS2021-02-Distance-to-Hospital.jsp (accessed on 13 February 2023).
- Akinlotan, M.; Primm, K.; Khodakarami, N.; Bolin, J.; Ferdinand, A.; Rural-Urban Variations in Travel Burdens for Care: Findings from the 2017 National Household Travel Survey. Southwest Rural Health Research Center. 2021. Available online: https://oaktrust.library.tamu.edu/server/api/core/bitstreams/bdb2f5a7-627b-4bb9-bc86-fb4890cfc9db/content#:~:text=On%20average%2C%20U.S.%20residents%20spent,%2C%20(p%3C0.0001) (accessed on 13 February 2023).
- Shahid, R.; Bertazzon, S.; Knudtson, M.L.; Ghali, W.A. Comparison of distance measures in spatial analytical modeling for health service planning. BMC Health Serv. Res. 2009, 9, 200. [Google Scholar] [CrossRef]
- Grech, V.; Borg, M. Influenza vaccination in the COVID-19 era. Early Hum. Dev. 2020, 148, 105116. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.; Kassens-Noor, E.; Kuljanin, G.; Vertalka, J. A geographic analysis of population density thresholds in the influenza pandemic of 1918–19. Int. J. Health Geogr. 2013, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Bonabeau, E.; Toubiana, L.; Flahault, A. The geographical spread of influenza. Proc. R. Soc. Lond. B Biol. Sci. 1998, 265, 2421–2425. [Google Scholar] [CrossRef]
- Attonito, J.; Van Arsdale, W.; Fishman, K.; Darya, M.; Jacomino, M.; Luck, G. Sociodemographic Disparities in Access to COVID-19 Vaccines upon Initial Rollout in Florida. Health Aff. Proj. Hope 2021, 40, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- Liao, T.F. Social and economic inequality in coronavirus disease 2019 vaccination coverage across Illinois counties. Sci. Rep. 2021, 11, 18443. [Google Scholar] [CrossRef]
- Williams, A.M.; Clayton, H.B.; Singleton, J.A. Racial and Ethnic Disparities in COVID-19 Vaccination Coverage: The Contribution of Socioeconomic and Demographic Factors. Am. J. Prev. Med. 2022, 62, 473–482. [Google Scholar] [CrossRef]
- Coronavirus (COVID-19). Indian Health Service. 2020. Available online: https://mcc-covid.crc.pitt.edu/COVID19_official_websites/United%20States%20of%20America%20(the)/ihs_situation_update/2020-12-15_092153.html (accessed on 13 February 2023).
- Coston, A.; Guha, N.; Ouyang, D.; Lu, L.; Chouldechova, A.; Ho, D.E. Leveraging Administrative Data for Bias Audits: Assessing Disparate Coverage with Mobility Data for COVID-19 Policy. In Proceedings of the 2021 ACM Conference on Fairness, Accountability, and Transparency, Virtual Event Canada, 3–10 March 2021; Association for Computing Machinery: New York, NY, USA, 2021; pp. 173–184. [Google Scholar]


| Metrics | MDD—Spring | MDD—Summer | MDD—Fall | MDD—Winter | USDA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MED | IQR | MED | IQR | MED | IQR | MED | IQR | MED | IQR | ||
| Calculated Metrics | |||||||||||
| G2SFCA score | 20 | 0.00 | 0.08 | 0.00 | 0.02 | 0.00 | 0.08 | 0.00 | 0.15 | 0.24 | 0.23 |
| 30 | 0.00 | 0.13 | 0.00 | 0.09 | 0.00 | 0.13 | 0.01 | 0.19 | 0.25 | 0.24 | |
| 40 | 0.04 | 0.14 | 0.02 | 0.09 | 0.04 | 0.14 | 0.04 | 0.17 | 0.29 | 0.23 | |
| 50 | 0.05 | 0.14 | 0.03 | 0.08 | 0.05 | 0.14 | 0.06 | 0.19 | 0.32 | 0.22 | |
| 60 | 0.08 | 0.15 | 0.04 | 0.11 | 0.08 | 0.15 | 0.09 | 0.18 | 0.33 | 0.19 | |
| 70 | 0.09 | 0.17 | 0.06 | 0.13 | 0.09 | 0.17 | 0.11 | 0.18 | 0.33 | 0.16 | |
| 80 | 0.12 | 0.17 | 0.09 | 0.15 | 0.12 | 0.17 | 0.13 | 0.17 | 0.34 | 0.13 | |
| 90 | 0.15 | 0.16 | 0.09 | 0.13 | 0.15 | 0.16 | 0.16 | 0.16 | 0.35 | 0.11 | |
| Population-to-facility ratio | 20 | 4954 | 4133 | 4954 | 3815 | 4954 | 4133 | 4954 | 4176 | 50 | 243 |
| 30 | 4954 | 4653 | 4954 | 4648 | 4954 | 4653 | 1386 | 4647 | 23 | 65 | |
| 40 | 449 | 2258 | 472 | 2295 | 449 | 2258 | 450 | 2290 | 14 | 31 | |
| 50 | 260 | 1498 | 413 | 1506 | 260 | 1498 | 252 | 1365 | 11 | 20 | |
| 60 | 151 | 3180 | 181 | 3176 | 151 | 3180 | 143 | 896 | 8 | 15 | |
| 70 | 122 | 919 | 122 | 2417 | 122 | 919 | 111 | 399 | 6 | 12 | |
| 80 | 91 | 306 | 106 | 451 | 91 | 306 | 75 | 234 | 5 | 10 | |
| 90 | 60 | 223 | 66 | 305 | 60 | 223 | 50 | 189 | 4 | 9 | |
| Non-calculated Metrics | Indicator | ||||||||||
| Socioeconomic Status | Poverty Rate (%) | 13.30 | 8.20 | 13.00 | 7.10 | 13.30 | 8.20 | 13.50 | 8.03 | 9.65 | 8.00 |
| No High School Diploma Rate (%) | 8.56 | 4.29 | 8.39 | 3.69 | 8.56 | 4.29 | 8.66 | 4.60 | 7.59 | 6.70 | |
| Unemployment Rate (%) | 6.80 | 4.60 | 6.60 | 4.80 | 6.80 | 4.60 | 6.80 | 4.48 | 4.90 | 3.60 | |
| Uninsured Rate (%) | 6.50 | 2.80 | 6.50 | 3.10 | 6.50 | 2.80 | 6.50 | 2.73 | 5.65 | 4.10 | |
| Per Capita Income | 27.5 K | 7.7 K | 28.7 K | 8.5 K | 27.6 K | 7.7 K | 27.6 K | 7.3 K | 34.0 K | 13.9 K | |
| All Oregon | Low-Vaccine-Accessibility Areas by Definition | |||||
|---|---|---|---|---|---|---|
| USDA | MDD—Spring | MDD—Summer | MDD—Fall | MDD—Winter | ||
| Age (years) | ||||||
| Under 5 | 5.58% | 5.49% | 4.45% | 4.66% | 4.45% | 4.56% |
| 5 to 19 | 17.80% | 18.51% | 15.60% | 16.55% | 15.60% | 15.57% |
| 20 to 64 | 59.43% | 57.29% | 54.58% | 54.70% | 54.58% | 54.41% |
| 65+ | 17.18% | 18.71% | 25.37% | 24.09% | 25.37% | 25.47% |
| Race | ||||||
| White alone | 84.29% | 86.51% | 88.77% | 87.83% | 88.77% | 89.23% |
| Black or African American alone | 1.91% | 1.24% | 0.71% | 0.78% | 0.71% | 0.62% |
| American Indian and Alaska Native alone | 1.16% | 0.96% | 4.50% | 5.74% | 4.50% | 4.28% |
| Asian alone | 4.37% | 4.01% | 0.78% | 0.76% | 0.78% | 0.69% |
| Native Hawaiian and Other Pacific Islander alone | 0.40% | 0.29% | 0.14% | 0.14% | 0.14% | 0.11% |
| Some other race alone | 3.07% | 2.52% | 1.27% | 1.44% | 1.27% | 1.11% |
| Two or more races | 4.80% | 4.47% | 3.84% | 3.31% | 3.84% | 3.95% |
| Ethnicity | ||||||
| Hispanic or Latino | 13.01% | 11.25% | 7.25% | 7.45% | 7.25% | 6.76% |
| Non-Hispanic or Latino | 86.99% | 88.75% | 92.75% | 92.55% | 92.75% | 93.24% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tao, D.; Agor, J.; McGregor, J.; Douglass, T.; Gibler, A.; Vergara, H.A. Identifying Areas with Low Access to the COVID-19 Vaccine: A New Objective Framework Incorporating Mobility Data. Healthcare 2025, 13, 1368. https://doi.org/10.3390/healthcare13121368
Tao D, Agor J, McGregor J, Douglass T, Gibler A, Vergara HA. Identifying Areas with Low Access to the COVID-19 Vaccine: A New Objective Framework Incorporating Mobility Data. Healthcare. 2025; 13(12):1368. https://doi.org/10.3390/healthcare13121368
Chicago/Turabian StyleTao, Defeng, Joseph Agor, Jessina McGregor, Trevor Douglass, Andrew Gibler, and Hector A. Vergara. 2025. "Identifying Areas with Low Access to the COVID-19 Vaccine: A New Objective Framework Incorporating Mobility Data" Healthcare 13, no. 12: 1368. https://doi.org/10.3390/healthcare13121368
APA StyleTao, D., Agor, J., McGregor, J., Douglass, T., Gibler, A., & Vergara, H. A. (2025). Identifying Areas with Low Access to the COVID-19 Vaccine: A New Objective Framework Incorporating Mobility Data. Healthcare, 13(12), 1368. https://doi.org/10.3390/healthcare13121368






