Integrating Acupuncture and Herbal Medicine into Assisted Reproductive Technology: A Systematic Review and Meta-Analysis of East Asian Traditional Medicine
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Strategy and Selection Criteria
2.3. Inclusion Criteria
- P (population): This is defined as infertile couples undergoing ART treatment (IVF and ICSI). ART refers to medical procedures and interventions that assist individuals or couples in achieving pregnancy, typically involving techniques such as IVF and ICSI.
- I (intervention): EATM therapies, including acupuncture (classic acupuncture, electro-acupuncture, laser acupuncture, and auricular acupuncture) and HM (herbal powders, pills, granules, decoctions, and ointments), were examined. The intervention protocols in ART cycles primarily focused on three aspects: duration, frequency, and timing. The duration ranged from 1 to 12 weeks. Acupuncture was administered once daily or every other day, while HM was taken two to three times per day. Interventions were implemented before and during IVF, as well as after embryo transfer (ET).
- C (comparison): Sham or placebo EATM therapies and conventional IVF/ICSI treatment (long protocol, GnRH antagonist protocol, Frozen ET protocol, IVF-ET microstimulation).
- O (outcome): A total of 4 outcome indices were analyzed in the meta-analysis (i.e., CPR, LBR, IR and AE). The CPR is defined as the presence of an intrauterine gestational sac. The LBR is defined as the ratio between the number of patients with live-born babies and the number of embryo transfers performed. The IR is defined as the percentage of embryos that were transferred that developed at least to the stage of fetal heart activity, as documented by pregnancy ultrasound. An AE is any unfavorable and unintended sign, symptom, or disease temporally associated with the use of an EATM treatment.
- S (study design): Only English-language RCTs were included.
2.4. Definitions of Control, Sham, and Placebo Groups
- Control Group: Participants received standard ART treatments (e.g., IVF or ICSI) without any additional EATM intervention, providing a baseline for comparison.
- Sham Acupuncture Group: Used in six trials, sham acupuncture involved needling at nonacupuncture points (nonacupoints) or using noninvasive needles that did not penetrate the skin. This method mimicked the acupuncture procedure while minimizing specific therapeutic effects, serving as an active control to account for placebo responses.
- Placebo Group: In six HM trials, the placebo consisted of pills made from a mixture of starch and glucose, shaped to resemble real herbal medicine pills. This ensured blinding and allowed for an assessment of the specific effects of herbal medicine beyond psychological or expectancy-driven responses.
2.5. Exclusion Criteria
2.6. Data Extraction
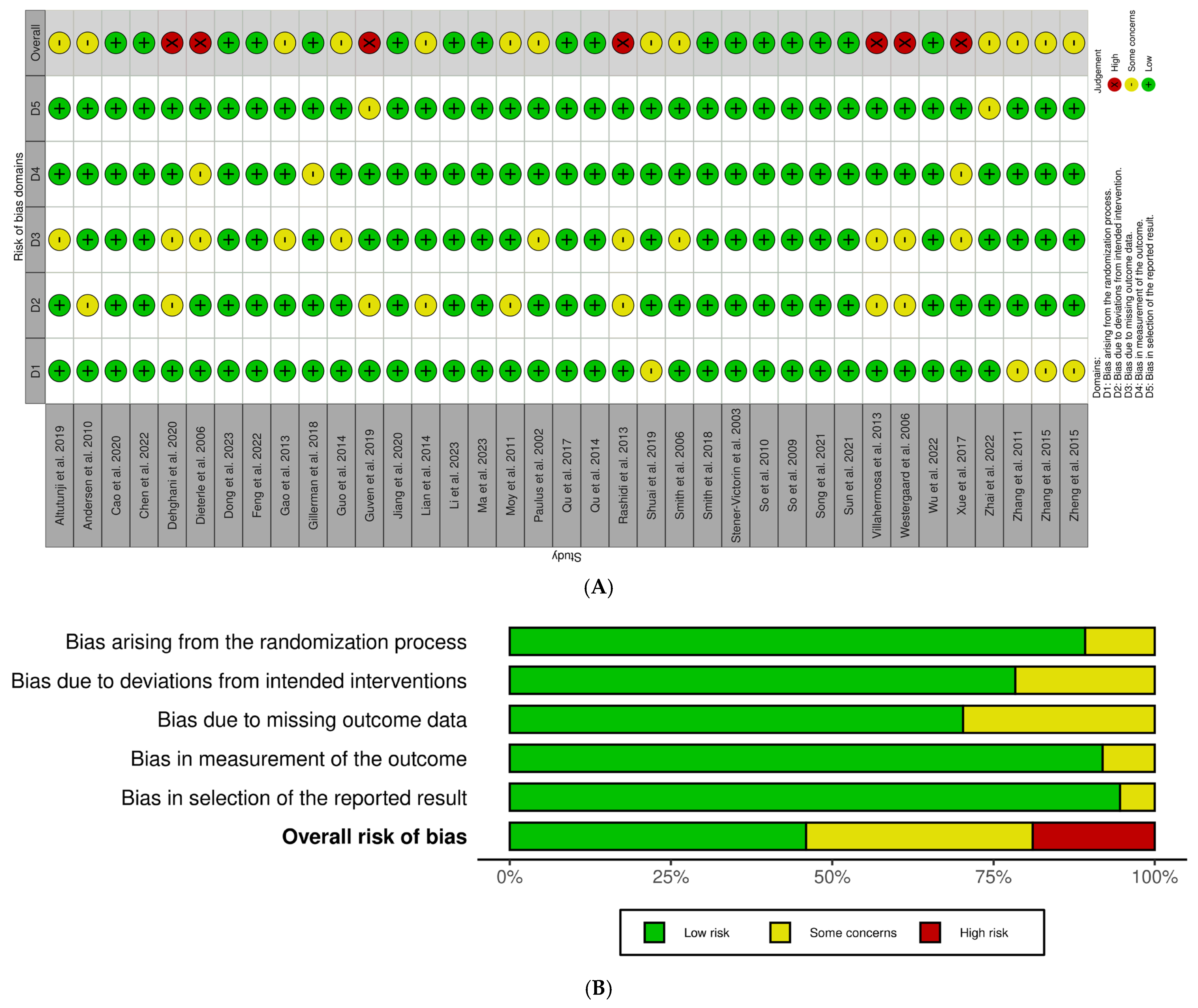
2.7. Risk of Bias Assessment
- Studies rated low-risk (e.g., 7, 11, 33, 39, 41–44, 46–49, 52–55) showed robust randomization, effective blinding, and full outcome reporting.
- Studies showing some concerns (e.g., 9, 10, 12, 29–32, 36–38, 40, 45) typically reflected minor uncertainties that did not compromise study validity.
- High-risk studies (e.g., 50, 51, 56–60) had serious methodological issues such as inadequate randomization, a lack of blinding, or selective reporting.
2.8. Data Synthesis and Statistical Analysis
- 0–40%: no heterogeneity.
- 30–60%: moderate heterogeneity.
- 50–90%: substantial heterogeneity.
- 75–100%: considerable heterogeneity.
- 75–90% falls into both classifications, meaning it is at the higher end of substantial heterogeneity and the lower end of considerable heterogeneity.
- Sample size: Larger studies may yield more precise results than smaller trials.
- EATM intervention types: Distinguishing between acupuncture and HM allows us to isolate their unique effects. This is essential, as each intervention type may influence reproductive outcomes differently due to their distinct physiological mechanisms.
2.9. Publication Bias
2.10. Assessment of Evidence Quality
- Risk of Bias: Studies were downgraded if there were concerns about randomization, blinding, or selective reporting.
- Inconsistency: Evidence was downgraded if studies showed conflicting results across trials.
- Indirectness: Evidence was considered indirect if populations or interventions differed significantly from those relevant to the research question.
- Imprecision: Studies with wide confidence intervals or small sample sizes were downgraded.
- Publication Bias: We assessed whether smaller studies with negative results might not have been published, which could skew findings.
2.11. Impact on Study Findings
3. Results
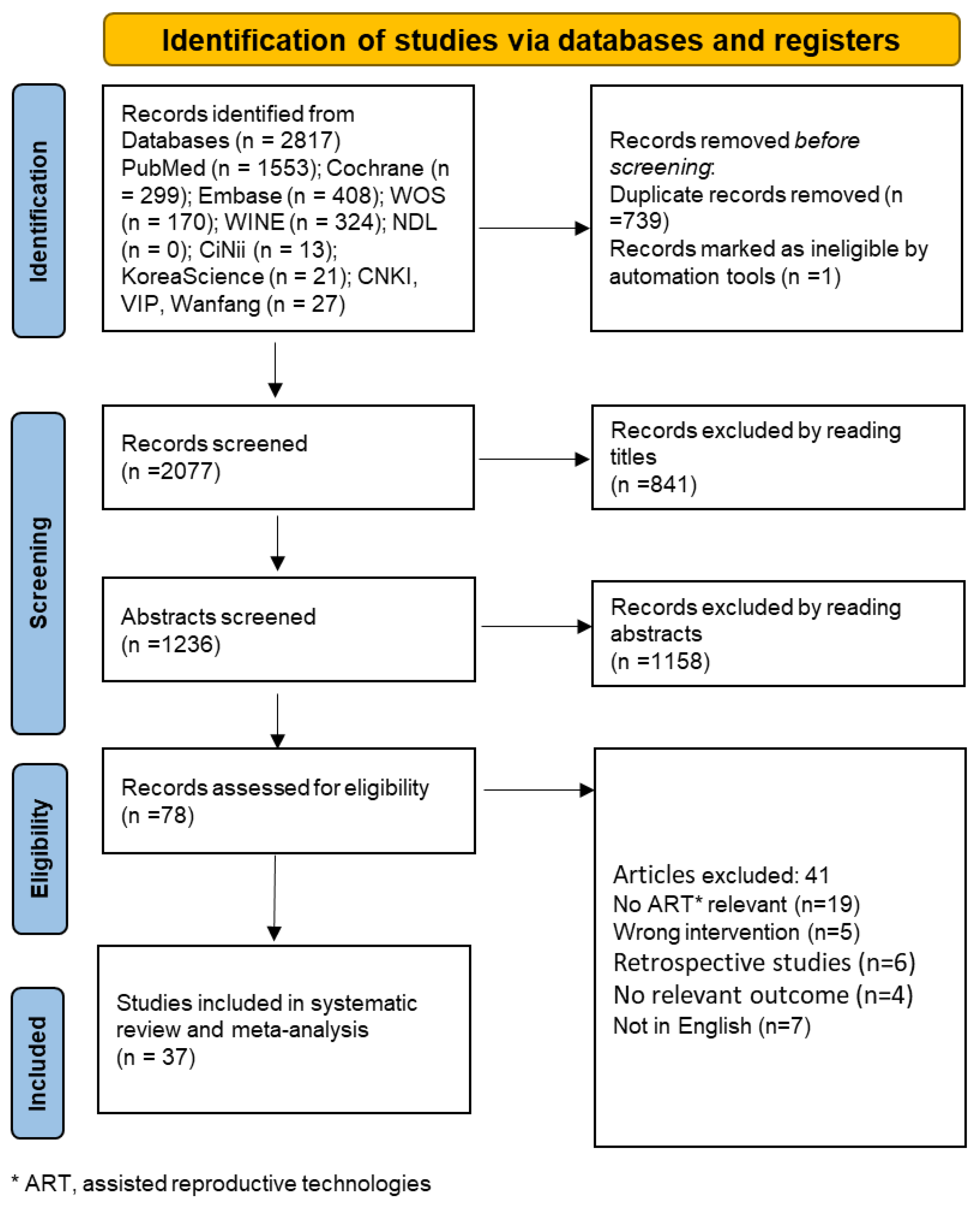
3.1. Results of the Search
3.2. Characteristics of Included Studies
3.3. Risk of Bias
3.4. Outcomes
3.4.1. Primary Outcomes
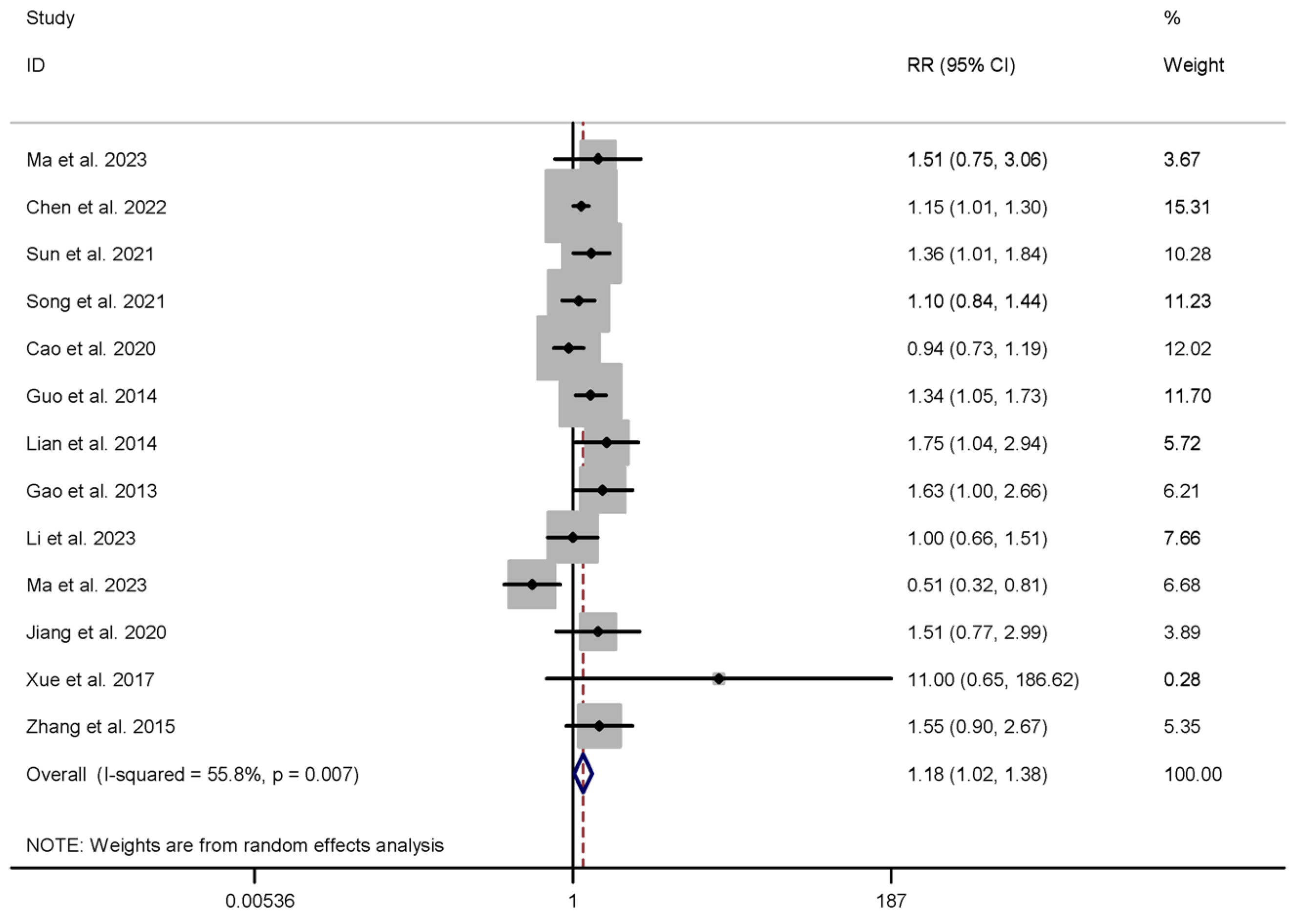
3.4.2. Secondary Outcomes
3.4.3. Safety of Outcomes
3.4.4. Adherence
3.5. Subgroup Analyses
3.6. Sensitivity Analysis
- Acupuncture vs. Sham: The CPR showed a significant increase (RR = 1.218, 95% CI 1.019–1.455, p = 0.030), while the LBR did not show a significant improvement (RR = 1.152, 95% CI 0.892–1.488, p = 0.277), suggesting a moderate effect on clinical pregnancy but not on live birth rates.
- HM vs. Sham: The CPR was significantly higher in the HM group compared to placebo (RR = 1.211, 95% CI 1.071–1.370, p = 0.002), reinforcing the potential benefits of HM interventions.
- Acupuncture vs. Control: Both the CPR (RR = 1.416, 95% CI 1.231–1.629, p < 0.001) and LBR (RR = 1.465, 95% CI 1.163–1.846, p = 0.001) were significantly higher, indicating the positive effect of acupuncture when compared to a no-treatment control.
- HM vs. Control: No significant difference was observed in the CPR (RR = 1.101, 95% CI 0.646–1.876, p = 0.724), suggesting that HM did not outperform standard IVF treatment.
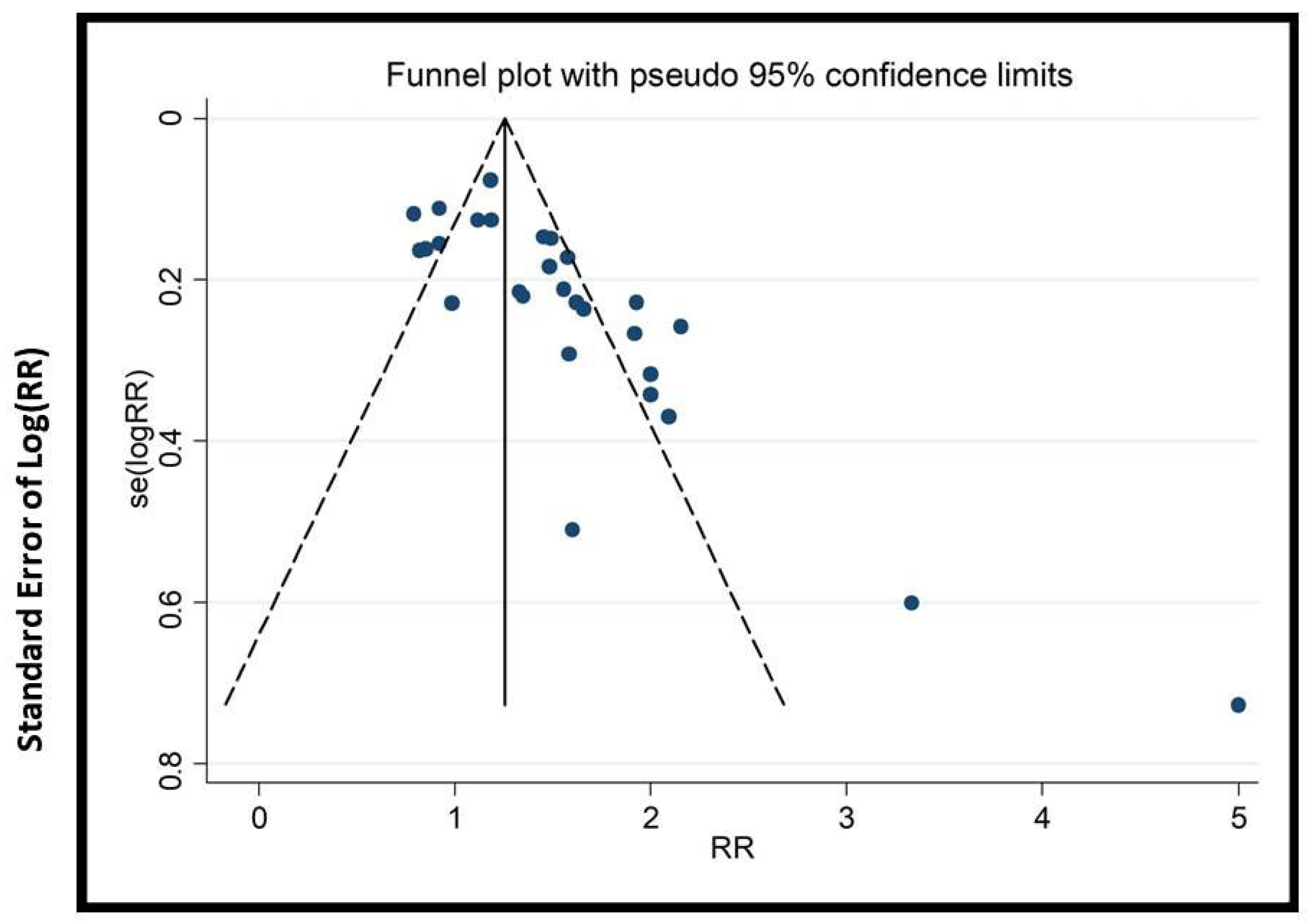
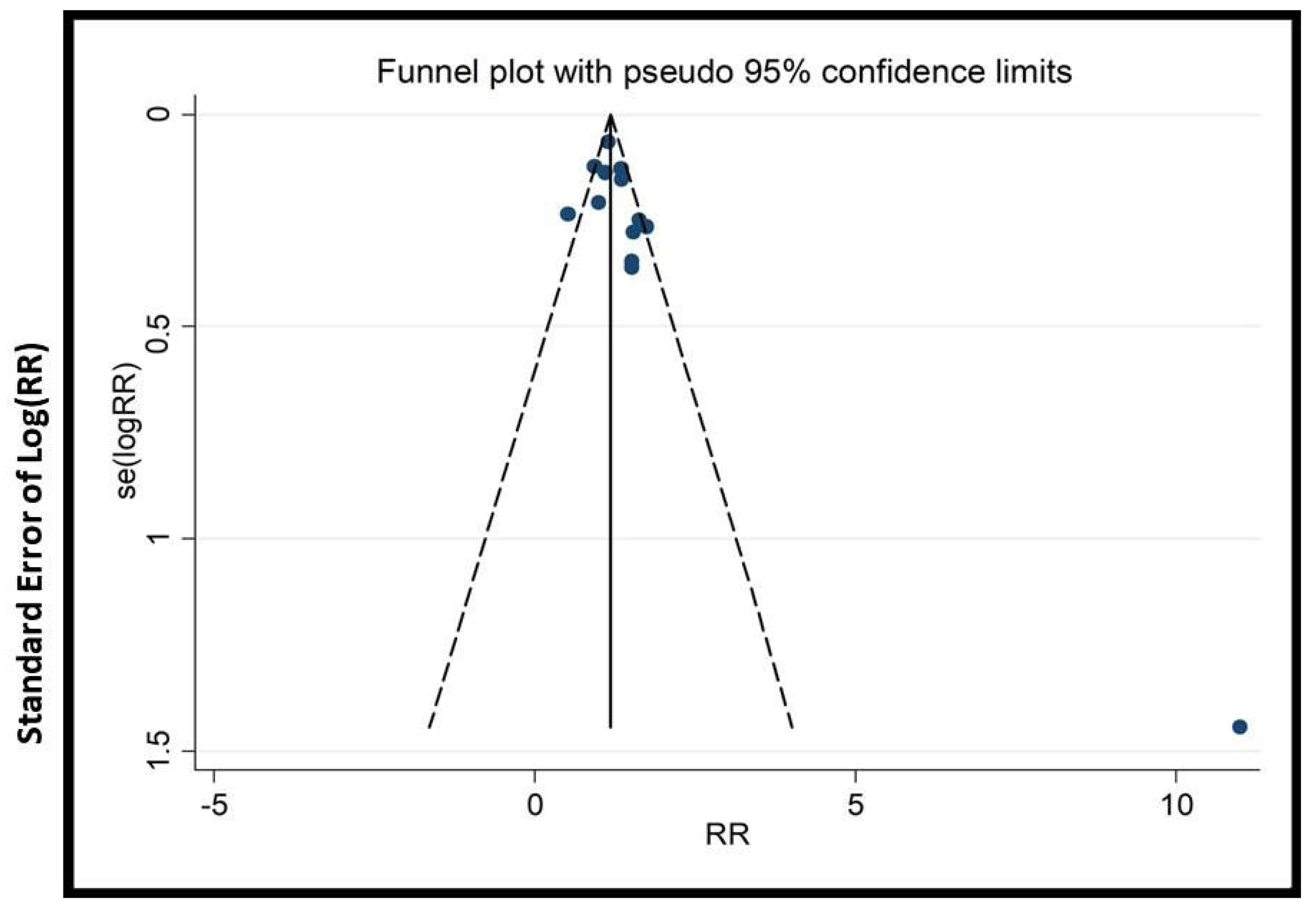
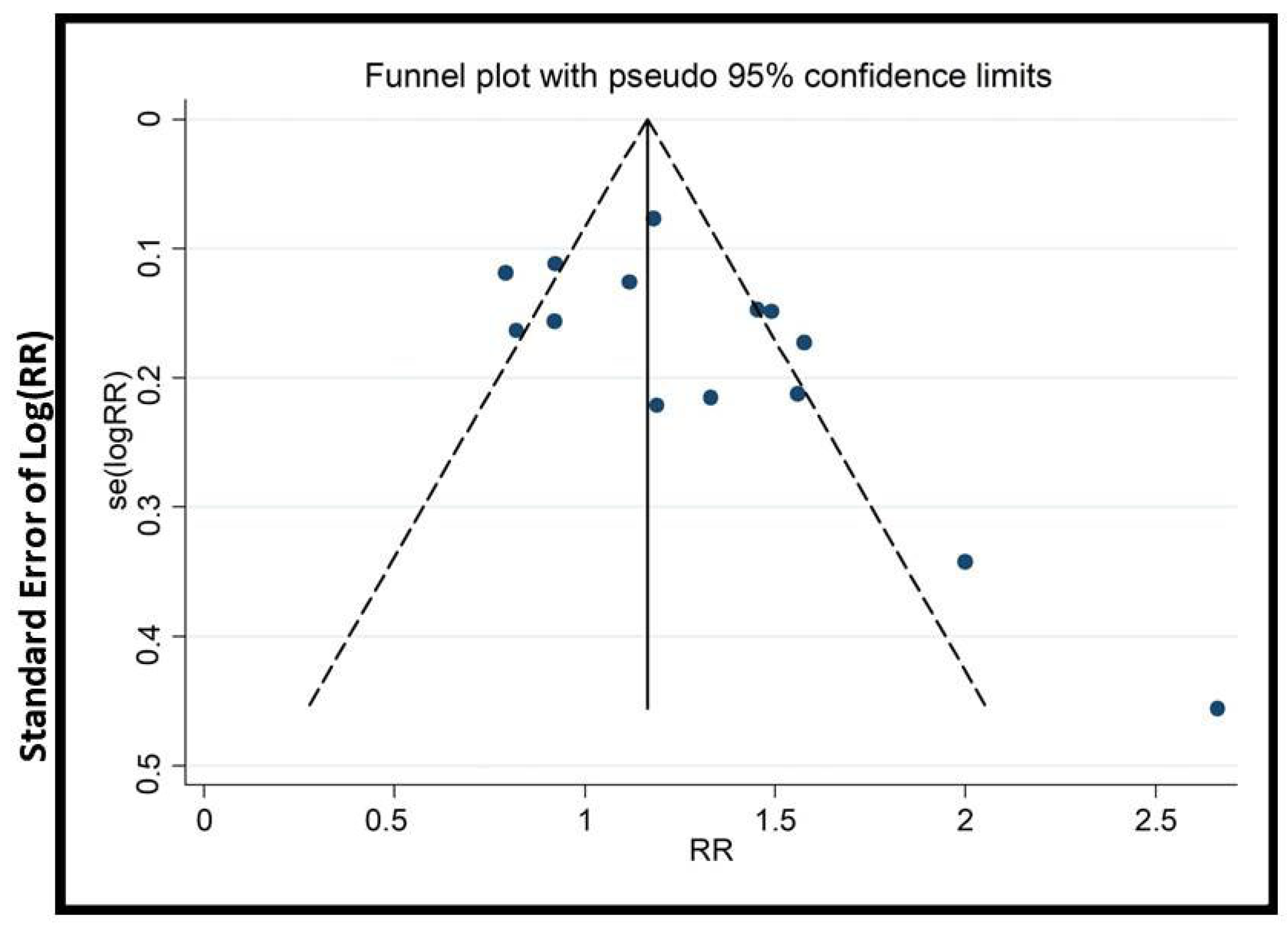
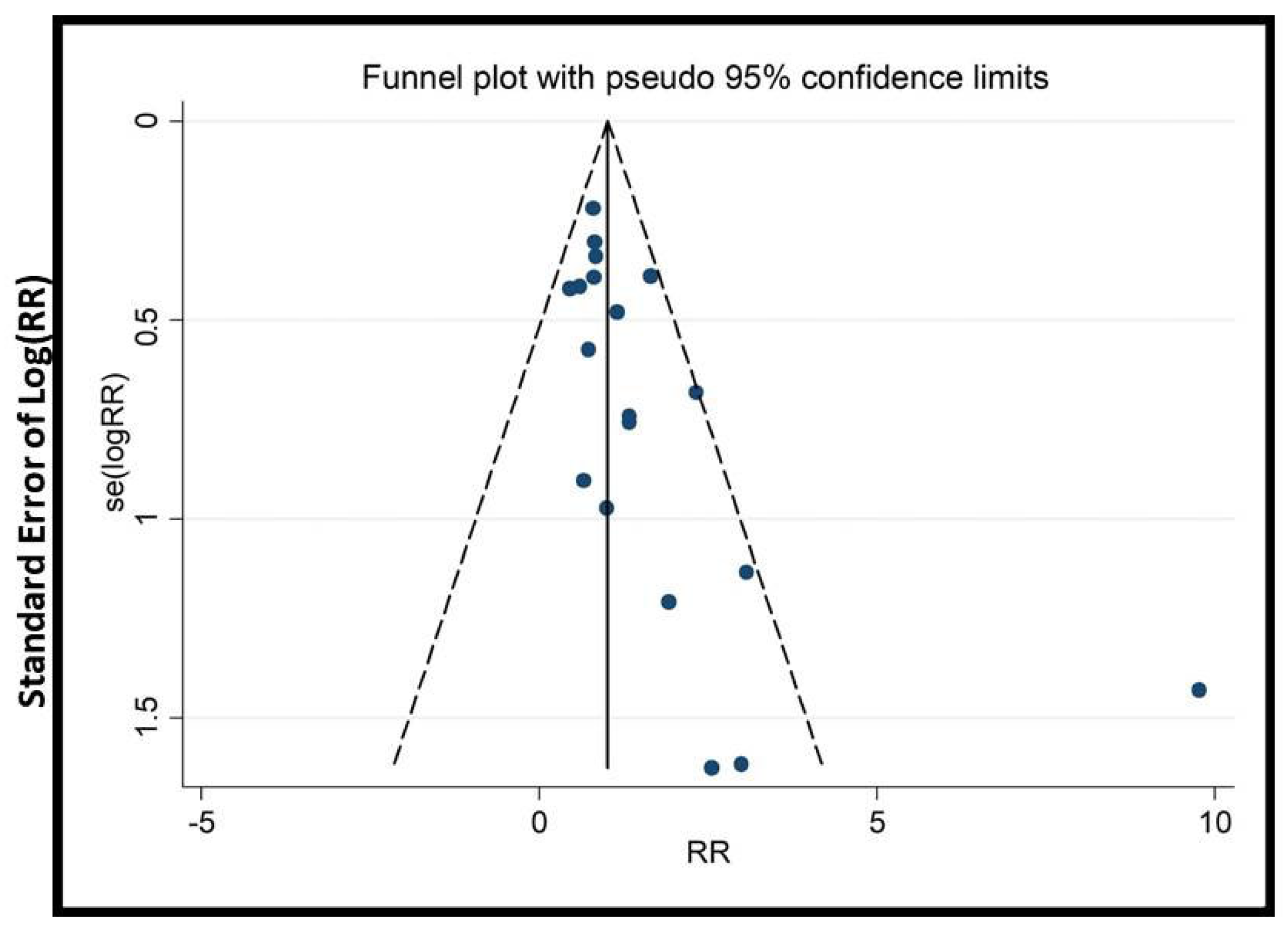
3.7. Publication Bias
3.8. Quality of Evidence by GRADE
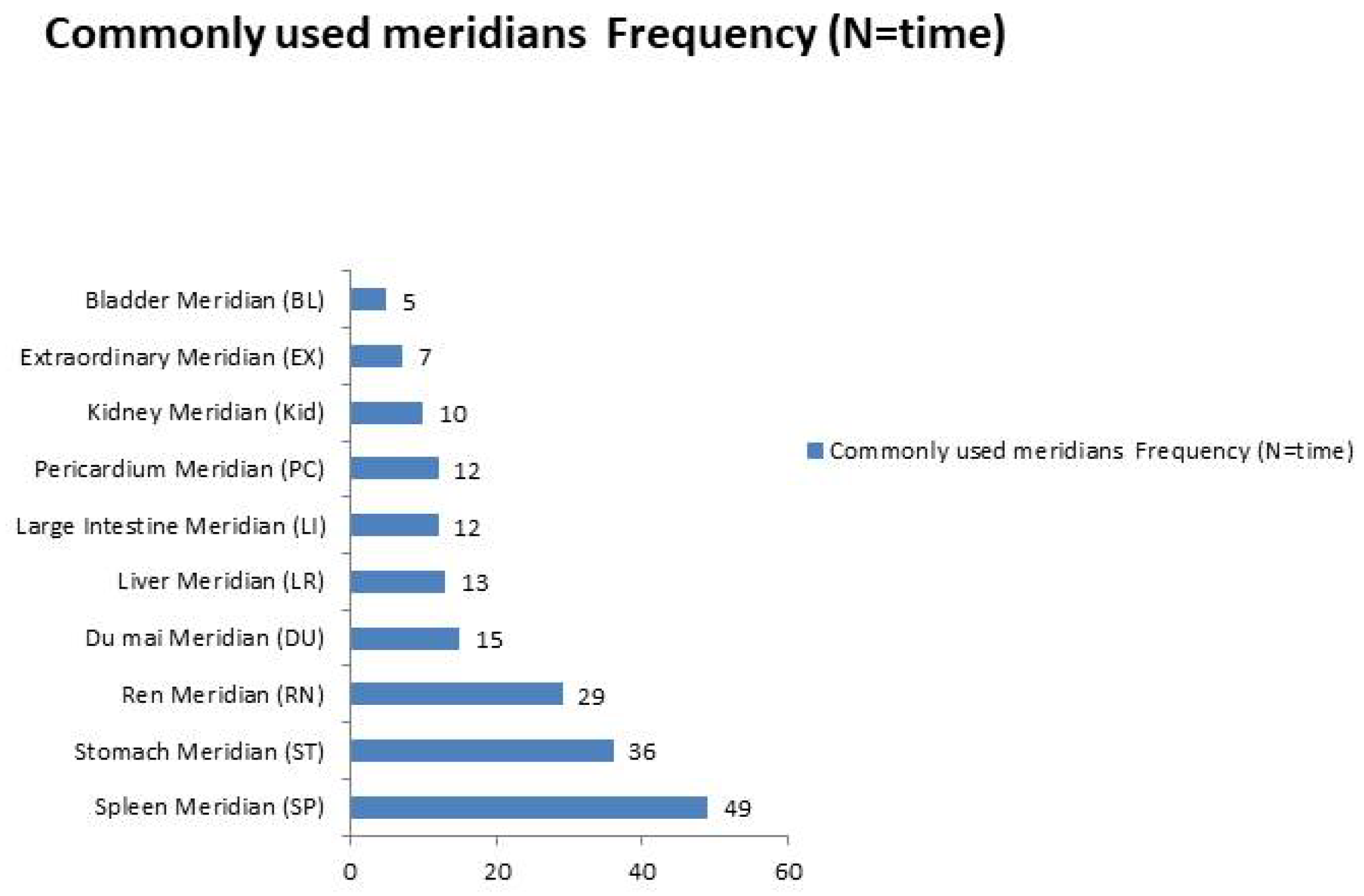
3.9. Key Acupoints and Meridians
HM Intervention
4. Discussion
4.1. Summary of Main Results
4.2. EATM Mechanisms on Reproductive Outcomes
4.2.1. Acupuncture Mechanisms on ART Outcomes
4.2.2. HM Mechanisms on ART Outcomes
4.3. Strengths and Limitations
4.4. The Gaps in the Literature
4.5. Variability in Acupuncture and HM
- Different Acupuncture Techniques: Variations in types of acupuncture (e.g., body, electro-acupuncture, auricular), stimulation methods (manual vs. electrical), needle placement, and treatment duration introduce inconsistencies in administration, leading to variable outcomes across studies.
- Sham Acupuncture Impact: The range of sham techniques used affects control comparisons and complicates efficacy evaluation. Some sham methods may cause physiological responses, skewing results and making it difficult to assess the true effects of acupuncture.
- HM Diversity: The wide variety of herbal formulas (e.g., powders, pills, decoctions), dosages, and timing (before, during, or after IVF) complicates comparisons. These variations prevent clear conclusions about the efficacy of specific EATM interventions.
4.6. Practice and Future Research Implications
4.7. The Potential Policy Implications
- Standardization of EATM Treatments in ART: Policymakers should develop unified guidelines for the application of acupuncture and HM in ART. This includes standardizing treatment protocols to improve consistency, reproducibility, and clinical outcomes across settings.
- Practitioner Training and Certification: Establishing specialized training and certification programs for EATM practitioners working in ART settings can ensure safe, high-quality, and evidence-informed care.
- Insurance and Accessibility: Expanding insurance coverage to include evidence-based EATM therapies can improve accessibility and reduce financial barriers for patients seeking integrative ART support.
- Interdisciplinary Collaboration: Fostering collaboration between reproductive endocrinologists and EATM practitioners may promote comprehensive and patient-centered care, leading to better clinical outcomes and patient satisfaction.
4.8. Integration of EATM in Clinical Practice
- Preparation Phase (3 months before IVF)
- 2.
- Ovarian Stimulation to Egg Retrieval
- 3.
- Embryo Transfer (ET) Day
- 4.
- Post-Transfer to Beta-hCG Test
- 5.
- Post-Pregnancy Confirmation (up to 12 weeks)
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Graham, M.E.; Jelin, A.; Hoon, A.H.; Wilms Floet, A.M.; Levey, E.; Graham, E.M. Assisted reproductive technology: Short- and long-term outcomes. Dev. Med. Child. Neurol. 2023, 65, 38–49. [Google Scholar] [CrossRef] [PubMed]
- Raymo, J.M.; Park, H.; Xie, Y.; Yeung, W.J.J. Marriage and family in East Asia: Continuity and change. Annu. Rev. Sociol. 2015, 41, 471–492. [Google Scholar] [CrossRef] [PubMed]
- Nomura, K.; Karita, K.; Araki, A.; Nishioka, E.; Muto, G.; Iwai-Shimada, M.; Nishikitani, M.; Inoue, M.; Tsurugano, S.; Kitano, N.; et al. For making a declaration of countermeasures against the falling birth rate from the Japanese Society for Hygiene: Summary of discussion in the working group on academic research strategy against an aging society with low birth rate. Environ. Health Prev. Med. 2019, 24, 14. [Google Scholar] [CrossRef]
- Wyns, C.; Bergh, C.; Calhaz-Jorge, C.; De Geyter, C.; Kupka, M.S.; Motrenko, T.; Rugescu, I.; Smeenk, J.; Tandler-Schneider, A.; Vidakovic, S. ART in Europe, 2016: Results generated from European registries by ESHRE. Hum. Reprod. Open 2020, 2020, hoaa032. [Google Scholar] [CrossRef] [PubMed]
- Wyns, C.; De Geyter, C.; Calhaz-Jorge, C.; Kupka, M.S.; Motrenko, T.; Smeenk, J.; Bergh, C.; Tandler-Schneider, A.; Rugescu, I.A.; Goossens, V. ART in Europe, 2018: Results generated from European registries by ESHRE. Hum. Reprod. Open 2022, 2022, hoac022. [Google Scholar]
- Cheong, Y.; Nardo, L.G.; Rutherford, T.; Ledger, W. Acupuncture and herbal medicine in in vitro fertilisation: A review of the evidence for clinical practice. Hum. Fertil. 2010, 13, 3–12. [Google Scholar] [CrossRef]
- So, E.W.S.; Ng, E.H.Y.; Wong, Y.Y.; Lau, E.Y.L.; Yeung, W.S.B.; Ho, P.C. A randomized double blind comparison of real and placebo acupuncture in IVF treatment. Hum. Reprod. 2009, 24, 341–348. [Google Scholar] [CrossRef]
- Stener-Victorin, E.; Wu, X. Effects and mechanisms of acupuncture in the reproductive system. Auton. Neurosci. 2010, 157, 46–51. [Google Scholar] [CrossRef]
- Paulus, W.E.; Zhang, M.; Strehler, E.; El-Danasouri, I.; Sterzik, K. Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy. Fertil. Steril. 2002, 77, 721–724. [Google Scholar] [CrossRef]
- Dieterle, S.; Ying, G.; Hatzmann, W.; Neuer, A. Effect of acupuncture on the outcome of in vitro fertilization and intracytoplasmic sperm injection: A randomized, prospective, controlled clinical study. Fertil. Steril. 2006, 85, 1347–1351. [Google Scholar] [CrossRef]
- Smith, C.; Coyle, M.; Norman, R.J. Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Fertil. Steril. 2006, 85, 1352–1358. [Google Scholar] [CrossRef] [PubMed]
- Westergaard, L.G.; Mao, Q.; Krogslund, M.; Sandrini, S.; Lenz, S.; Grinsted, J. Acupuncture on the day of embryo transfer significantly improves the reproductive outcome in infertile women: A prospective, randomized trial. Fertil. Steril. 2006, 85, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Manheimer, E.; Zhang, G.; Udoff, L.; Haramati, A.; Langenberg, P.; Berman, B.M.; Bouter, L.M. Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: Systematic review and meta-analysis. BMJ 2008, 336, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Xia, W.; Huang, J.; Zhang, X.; Li, F.; Yu, X.; Ma, J.; Zeng, Q. Effects of acupuncture on the pregnancy outcomes of frozen-thawed embryo transfer: A systematic review and meta-analysis. Front. Public Health 2022, 10, 987276. [Google Scholar] [CrossRef]
- Zhu, F.; Zhao, B.; Wu, J.; Yin, S.; Ma, T.; Li, Z.; Zhu, X.; Wang, T.; Yang, B.; Che, D. Effect of transcutaneous electrical acupoint stimulation on pregnancy outcomes in women with in vitro fertilization-embryo transfer: A systematic review and meta-analysis. Front. Cell Dev. Biol. 2022, 10, 1068894. [Google Scholar] [CrossRef]
- Quan, K.; Yu, C.; Wen, X.; Lin, Q.; Wang, N.; Ma, H. Acupuncture as treatment for female infertility: A systematic review and meta-analysis of randomized rontrolled trials. Evid. Based Complement. Alternat. Med. 2022, 2022, 3595033. [Google Scholar] [CrossRef]
- Lee, J.W.; Hyun, M.K.; Kim, H.J.; Kim, D.I. Acupuncture and herbal medicine for female infertility: An overview of systematic reviews. Integr. Med. Res. 2021, 10, 100694. [Google Scholar] [CrossRef]
- Kwon, C.Y.; Lee, B.; Lee, S.H.; Jo, J. Herbal medicine in women undergoing in vitro fertilization/intracytoplasmic sperm injection: A systematic review and meta-analysis. Complement. Ther. Med. 2020, 53, 102528. [Google Scholar] [CrossRef]
- Cao, H.; Han, M.; Ng, E.H.Y.; Wu, X.; Flower, A.; Lewith, G.; Liu, J.-P. Can Chinese herbal medicine improve outcomes of in vitro fertilization? A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2013, 8, e81650. [Google Scholar] [CrossRef]
- Song, J.Y.; Dong, F.Y.; Wu, Z.J.; Ma, Y.X.; Sun, Z.G. Impact of whole-systems traditional Chinese medicine therapy on in vitro fertilization and embryo transfer outcomes: A retrospective cohort study. Eur. J. Integr. Med. 2023, 60, 102246. [Google Scholar] [CrossRef]
- Jo, J.; Kang, M.J.; Lee, J.M.; Kim, H.; Jerng, U.M. Effects of traditional Korean medicine on anti-Müllerian hormone in patients with diminished ovarian reserve: A retrospective study. Complement. Ther. Med. 2016, 24, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Lee, H.W.; Kim, N.; Park, Y.H.; Choi, T.Y.; Lee, M.S. Characteristics and outcomes of herbal medicine for female infertility: A retrospective analysis of data from a Korean medicine clinic during 2010–2020. Int. J. Womens Health 2022, 14, 575–582. [Google Scholar] [CrossRef]
- Li, X.; Lee, H.W.; Zhou, T.; Robinson, N.; Hu, X.-Y.M.; Dunjić, M.; Wang, F.; Zhang, R.; Panel, C.; Zhu, Y.; et al. Non-pharmacological interventions involving traditional Chinese medicine for assisted reproductive technology: A group consensus. Integr. Med. Res. 2025, 14, 101137. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Savović, J.; Page, M.J.; Elbers, R.G.; Sterne, J.A.C. Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2019; pp. 205–228. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- Schünemann, H.J.; Oxman, A.D.; Brozek, J.; Glasziou, P.; Jaeschke, R.; Vist, G.E.; Williams, J.W., Jr.; Kunz, R.; Craig, J.; Montori, V.M.; et al. Grading quality of evidence and strength of recommendations for diagnostic tests and strategies. BMJ 2008, 336, 1106–1110. [Google Scholar] [CrossRef]
- Altutunji, A.Z.; Liu, L.; Cai, J.; Wang, Z.; Gao, Y. The effect of acupuncture on anti-mullerian hormone and assisted reproduction outcome in Polycystic Ovary Syndrome patients undergoing in vitro fertilization. J. Pak. Med. Assoc. 2019, 69 (Suppl. S3), S4–S8. [Google Scholar]
- Dehghani, A.S.; Homayouni, K.; Kanannejad, Z.; Kanannejad, Z. The effect of acupuncture on the day of embryo transfer on the in vitro fertilization outcomes: An RCT. Int. J. Reprod. Biomed. 2020, 18, 209–214. [Google Scholar] [CrossRef]
- Qu, F.; Zhang, D.; Chen, L.T.; Wang, F.-F.; Pan, J.-X.; Zhu, Y.-M.; Ma, C.-M.; Huang, Y.-T.; Ye, X.-Q.; Sun, S.-J.; et al. Auricular acupressure reduces anxiety levels and improves outcomes of in vitro fertilization: A prospective, randomized and controlled study. Sci. Rep. 2014, 4, 5028. [Google Scholar] [CrossRef]
- Di Villahermosa, D.I.M.; dos Santos, L.G.; Nogueira, M.B.; Vilarino, F.L.; Barbosa, C.P. Influence of acupuncture on the outcomes of in vitro fertilisation when embryo implantation has failed: A prospective randomised controlled clinical trial. Acupunct. Med. 2013, 31, 157–161. [Google Scholar] [CrossRef]
- Zhang, R.; Feng, X.J.; Guan, Q.; Cui, W.; Zheng, Y.; Sun, W.; Han, J.-S. Increase of success rate for women undergoing embryo transfer by transcutaneous electrical acupoint stimulation: A prospective randomized placebo-controlled study. Fertil. Steril. 2011, 96, 912–916. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Song, J.; Cao, X.; Sun, Z. Mechanism of Guilu Erxian ointment based on targeted metabolomics in intervening in vitro fertilization and embryo transfer outcome in older patients with poor ovarian response of kidney-qi deficiency type. Front. Endocrinol. 2023, 14, 1045384. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.L.; Fu, Y.L.; Kang, Y.; Qi, C.; Zhang, Q.H.; Kuang, Y.P. Clinical observations of sequential therapy with Chinese medicine and hysteroscopic mechanical stimulation of the endometrium in infertile patients with repeated implantation failure undergoing frozen-thawed embryo transfer. Chin. J. Integr. Med. 2015, 21, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Qu, F.; Wang, F.F.; Wu, Y.; Zhou, J.; Robinson, N.; Hardiman, P.J.; Pan, J.-X.; He, Y.-J.; Zhu, Y.-H.; Wang, H.-Z.; et al. Transcutaneous electrical acupoint stimulation improves the outcomes of in vitro fertilization: A prospective, randomized and controlled study. Explore 2017, 13, 306–312. [Google Scholar] [CrossRef]
- Zheng, Y.; Feng, X.; Mi, H.; Yao, Y.; Zhao, Y.; Li, J.; Jiao, J.; Gong, A.; Sun, W.; Deng, X. Effects of transcutaneous electrical acupoint stimulation on ovarian reserve of patients with diminished ovarian reserve in in vitro fertilization and embryo transfer cycles. J. Obstet. Gynaecol. Res. 2015, 41, 1905–1911. [Google Scholar] [CrossRef]
- Zhai, Z.J.; Liu, J.E.; Lei, L.L.; Wang, S.Y. Effects of transcutaneous electrical acupoint stimulation on ovarian responses and pregnancy outcomes in patients undergoing IVF-ET: A randomized controlled trial. Chin. J. Integr. Med. 2022, 28, 434–439. [Google Scholar] [CrossRef]
- Dong, H.X.; Wu, X.; Zhou, Q.; Huang, D.-M.; Zhang, M.-M.; Huang, G.-Y.; Yang, W. Effect of acupuncture on endometrial blood flow in women undergoing in vitro fertilization embryo transfer: A single blind, randomized controlled trial. Chin. J. Integr. Med. 2024, 30, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Ning, Y.; Ye, Y.Y.; Liu, Y.-L.; Tang, M.; Hu, S.; Zhuo, Y.-Y. Effects of acupuncture on endometrium and pregnancy outcomes in patients with polycystic ovarian syndrome undergoing in vitro fertilization-embryo transfer: A randomized clinical trial. Chin. J. Integr. Med. 2022, 28, 736–742. [Google Scholar] [CrossRef]
- Feng, X.; Zhu, N.; Yang, S.; Wang, L.; Sun, W.; Li, R.; Gong, F.; Han, S.; Zhang, R.; Han, J. Transcutaneous electrical acupoint stimulation improves endometrial receptivity resulting in improved IVF-ET pregnancy outcomes in older women: A multicenter, randomized, controlled clinical trial. Reprod. Biol. Endocrinol. 2022, 20, 127. [Google Scholar] [CrossRef]
- Shuai, Z.; Li, X.; Tang, X.; Lian, F.; Sun, Z. Transcutaneous electrical acupuncture point stimulation improves pregnancy outcomes in patients with recurrent implantation failure undergoing in vitro fertilisation and embryo transfer: A prospective, randomised trial. Acupunct. Med. 2019, 37, 33–39. [Google Scholar] [CrossRef]
- So, E.W.S.; Ng, E.H.Y.; Wong, Y.Y.; Yueng, W.S.B.; Ho, P.C. Acupuncture for frozen-thawed embryo transfer cycles: A double-blind randomized controlled trial. Reprod. Biomed. Online 2010, 20, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Andersen, D.; Løssl, K.; Andersen, A.N.; Fürbringer, J.; Bach, H.; Simonsen, J.; Larsen, E.C. Acupuncture on the day of embryo transfer: A randomized controlled trial of 635 patients. Reprod. Biomed. Online 2010, 21, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Stener-Victorin, E.; Waldenström, U.; Wikland, M.; Nilsson, L.; Hägglund, L.; Lundeberg, T. Electro-acupuncture as a peroperative analgesic method and its effects on implantation rate and neuropeptide Y concentrations in follicular fluid. Hum. Reprod. 2003, 18, 1454–1460. [Google Scholar] [CrossRef] [PubMed]
- Gillerman, K.; Kulkarni, A.; Shah, A.; Gudi, A.; Homburg, R. The impact of acupuncture on IVF success rates: A randomised controlled trial. Fertil. Sci. Res. 2018, 5, 48–54. [Google Scholar]
- Rashidi, B.H.; Tehrani, E.S.; Hamedani, N.A.; Pirzadeh, L. Effects of acupuncture on the outcome of in vitro fertilisation and intracytoplasmic sperm injection in women with polycystic ovarian syndrome. Acupunct. Med. 2013, 31, 151–156. [Google Scholar] [CrossRef]
- Smith, C.A.; de Lacey, S.; Chapman, M.; Ratcliffe, J.; Norman, R.J.; Johnson, N.P.; Boothroyd, C.; Fahey, P. Effect of acupuncture vs sham acupuncture on live births among women undergoing in vitro fertilization: A randomized clinical trial. JAMA 2018, 319, 1990–1998. [Google Scholar] [CrossRef]
- Moy, I.; Milad, M.P.; Barnes, R.; Confino, E.; Kazer, R.R.; Zhang, X. Randomized controlled trial: Effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization. Fertil. Steril. 2011, 95, 583–587. [Google Scholar] [CrossRef]
- Guven, P.G.; Cayir, Y.; Borekci, B. Effectiveness of acupuncture on pregnancy success rates for women undergoing in vitro fertilization: A randomized controlled trial. Taiwan. J. Obstet. Gynecol. 2020, 59, 282–286. [Google Scholar] [CrossRef]
- Li, X.F.; Wang, Z.Q.; Xu, H.Y.; Liu, H.; Sheng, Y.; Xu, J.; Li, Y.-M.; Lian, F. Effects of Zishen Yutai pills on in vitro fertilization-embryo transfer outcomes in patients with diminished ovarian reserve: A prospective, open-labeled, randomized and controlled study. Chin. J. Integr. Med. 2023, 29, 291–298. [Google Scholar] [CrossRef]
- Chen, X.; Hao, C.; Deng, W.; Bai, H.; Li, Y.; Wang, Z.; Shi, Y.; Zhang, H.; Zhu, Y.; Zhang, H.; et al. Effects of the Zishen Yutai pill Compared with placebo on live births among women in a fresh embryo transfer cycle: A aandomized controlled trial. Obstet. Gynecol. 2022, 139, 192–201. [Google Scholar] [CrossRef]
- Sun, J.; Song, J.Y.; Dong, Y.; Xiang, S.; Guo, Q. Erzhi Tiangui granules improve in vitro fertilization outcomes in infertile women with advanced age. Evid. Based Complement. Alternat Med. 2021, 2021, 9951491. [Google Scholar] [CrossRef] [PubMed]
- Song, J.Y.; Gao, D.D.; Cao, X.L.; Xiang, S.; Chen, Y.-H.; Teng, Y.-L.; Li, X.-F.; Liu, H.-P.; Wang, F.-X.; Zhang, B.; et al. The role of traditional Chinese formula Ding-Kun Pill (DKP) in expected poor ovarian response women (POSEIDON Group 4) undergoing in vitro fertilization-embryo transfer: A multicenter, randomized, double-blind, placebo-controlled trial. Front. Endocrinol. 2021, 12, 675997. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.L.; Song, J.Y.; Zhang, X.X.; Chen, Y.H.; Teng, Y.L.; Liu, H.P.; Deng, T.Y.; Sun, Z.G. Effects of a Chinese patent medicine Gushen’antai pills on ongoing pregnancy rate of hormone therapy FET cycles: A multi-center, randomized, double-blind, placebo-controlled clinical trial. Front. Endocrinol. 2020, 11, 581719. [Google Scholar] [CrossRef]
- Jiang, X.; Yan, H.; Zhong, X.; Tong, G.; Zhang, W. Effect of Bushen Yutai recipe on IVF patients subjected to mild ovarian stimulation. Front. Med. 2020, 7, 541537. [Google Scholar] [CrossRef]
- Xue, H.; Dong, J.; Xu, H.; Huang, X.; Dai, H.; Hao, C. Tiaogeng Yijing decoction improves the pregnancy outcomes of patients with poor ovarian response undergoing in vitro fertilization-embryo transfer. Exp. Ther. Med. 2017, 14, 3935–3941. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guo, J.; Li, D.; Liu, C.; Ji, X.; Li, R.; Du, X. Effects of Chinese herbs combined with in vitro fertilization and embryo transplantation on infertility: A clinical randomized controlled trial. J. Trad. Chin. Med. 2014, 34, 267–273. [Google Scholar] [CrossRef]
- Lian, F.; Wu, H.C.; Sun, Z.G.; Guo, Y.; Shi, L.; Xue, M.Y. Effects of Liuwei Dihuang Granule on the outcomes of in vitro fertilization pre-embryo transfer in infertility women with Kidney-yin deficiency syndrome and the proteome expressions in the follicular fluid. Chin. J. Integr. Med. 2014, 20, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Chang, X.; Du, H.; Zhang, M.; Zhang, J.; Zhu, A. Effect of soothing liver therapy on oocyte quality and growth differentiation factor-9 in patients undergoing in vitro fertilization and embryo transfer. J. Trad. Chin. Med. 2013, 33, 597–602. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 12; StataCorp LP: College Station, TX, USA, 2011. [Google Scholar]
- Singh, J. International conference on harmonization of technical requirements for registration of pharmaceuticals for human use. J. Pharmacol. Pharmacother. 2015, 6, 185–187. [Google Scholar] [CrossRef]
- Freites-Martinez, A.; Santana, N.; Arias-Santiago, S.; Viera, A. Using the common terminology criteria for adverse events (CTCAE—Version 5.0) to evaluate the severity of adverse events of anticancer therapies. Actas Dermo-Sifiliográficas (Engl. Ed.) 2020, 112, 90–92. [Google Scholar] [CrossRef]
- Zia, F.Z.; Olaku, O.; Bao, T.; Berger, A.; Deng, G.; Fan, A.Y.; Garcia, M.K.; Herman, P.M.; Kaptchuk, T.J.; Ladas, E.J.; et al. The National Cancer Institute’s Conference on Acupuncture for Symptom Management in Oncology: State of the Science, Evidence, and Research Gaps. J. Natl. Cancer Inst. Monogr. 2017, 2017, lgx005. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Altman, D.G.; Hammerschlag, R.; Youping, L.; Taixiang, W.; White, A.; Moher, D. Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT Statement. PLoS Med. 2010, 7, e1000261. [Google Scholar] [CrossRef] [PubMed]
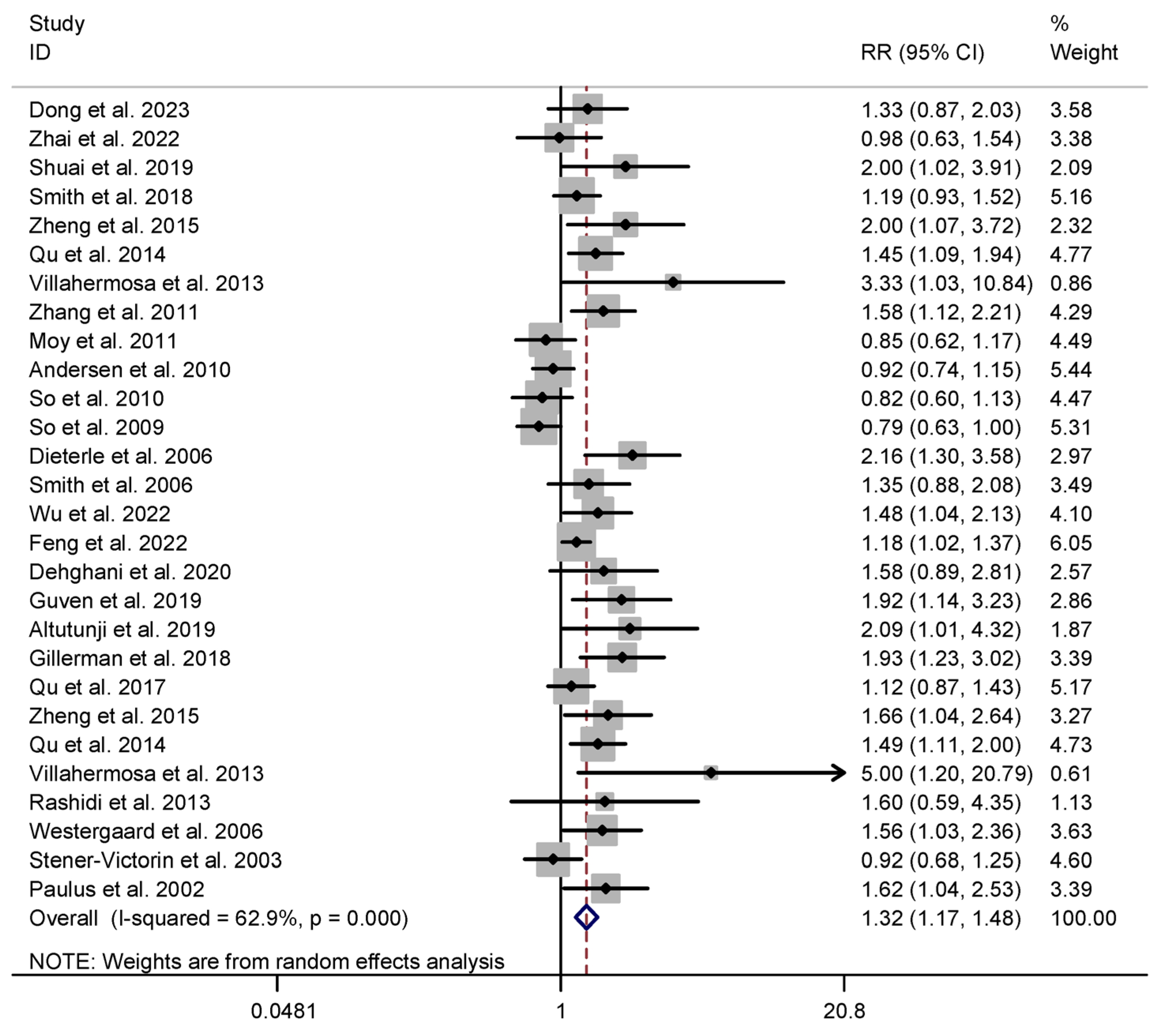





| Outcomes | No. of Studies | No. of IG Patients | No. of CG Patients | RR (95% CI) | Study Heterogeneity | ||
|---|---|---|---|---|---|---|---|
| χ2 | df | I2 (%) | |||||
| Primary outcomes | |||||||
| Acupuncture vs. Sham+ No intervention | |||||||
| Clinical pregnancy rate | 25 | 3565 | 3045 | 1.316 (1.171, 1.480) | 72.68 | 27 | 62.9% |
| Live birth rate | 14 | 2517 | 2096 | 1.287 (1.081, 1.533) | 46.48 | 14 | 69.9% |
| Herbal medicine vs. Sham+ No intervention | |||||||
| Clinical pregnancy rate | 12 | 2142 | 2201 | 1.184 (1.017, 1.379) | 27.14 | 12 | 55.8% |
| Live birth rate | 3 | 1407 | 1411 | 1.147 (1.010, 1.303) | 0.32 | 2 | 0.0% |
| Secondary outcomes | |||||||
| Acupuncture vs. Sham+ No intervention | |||||||
| Implantation rate | 13 | 2302 | 1871 | 1.183 (1.028, 1.363) | 37.57 | 13 | 65.4% |
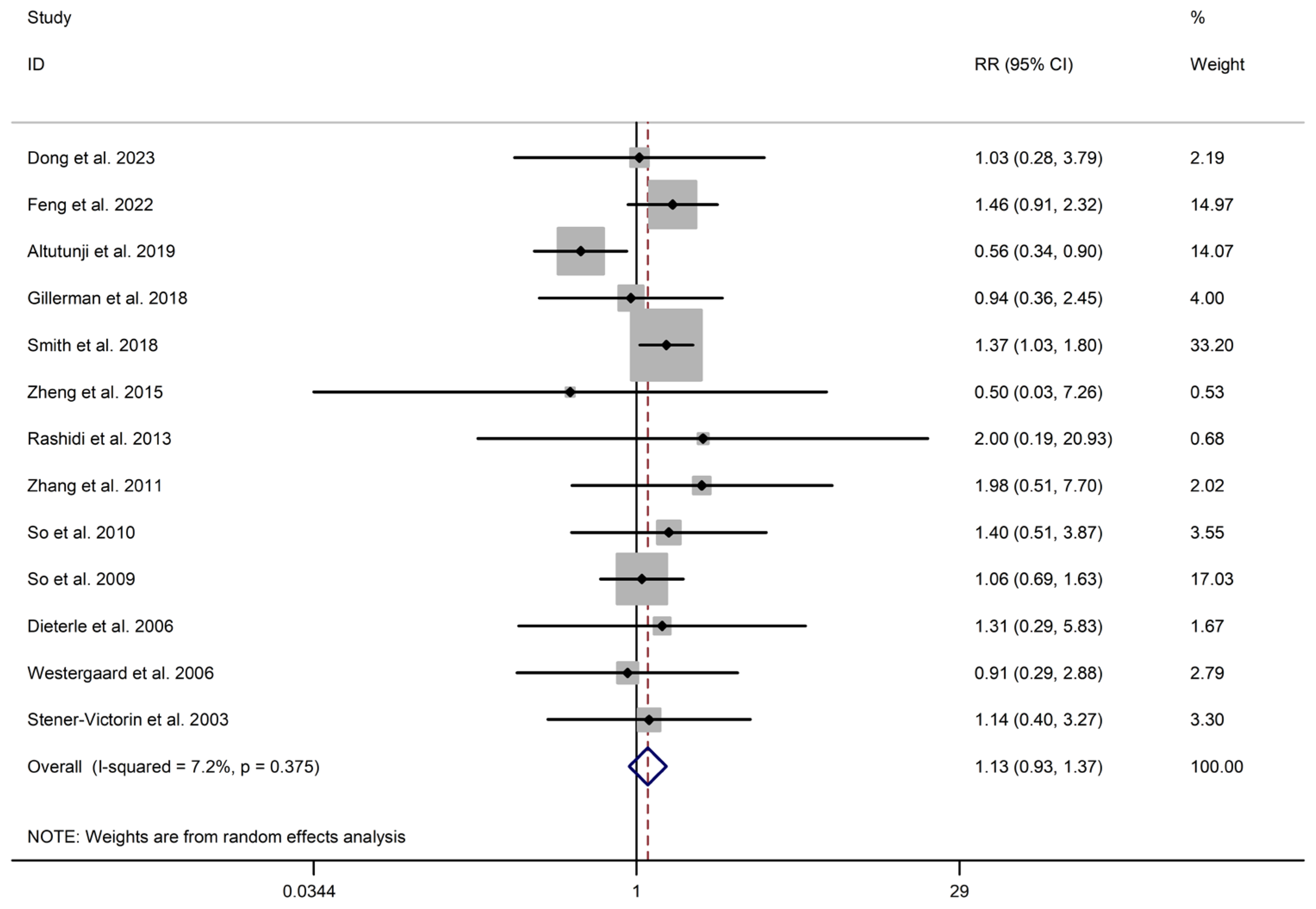
| Adverse events * | 13 | 1064 | 1092 | 1.125 (0.926, 1.367) | 12.92 | 12 | 7.2% |
| Herbal medicine vs. Sham+ No intervention | |||||||
| Implantation rate | 5 | 1488 | 1547 | 1.106 (0.968, 1.264) | 4.65 | 4 | 14.0% |
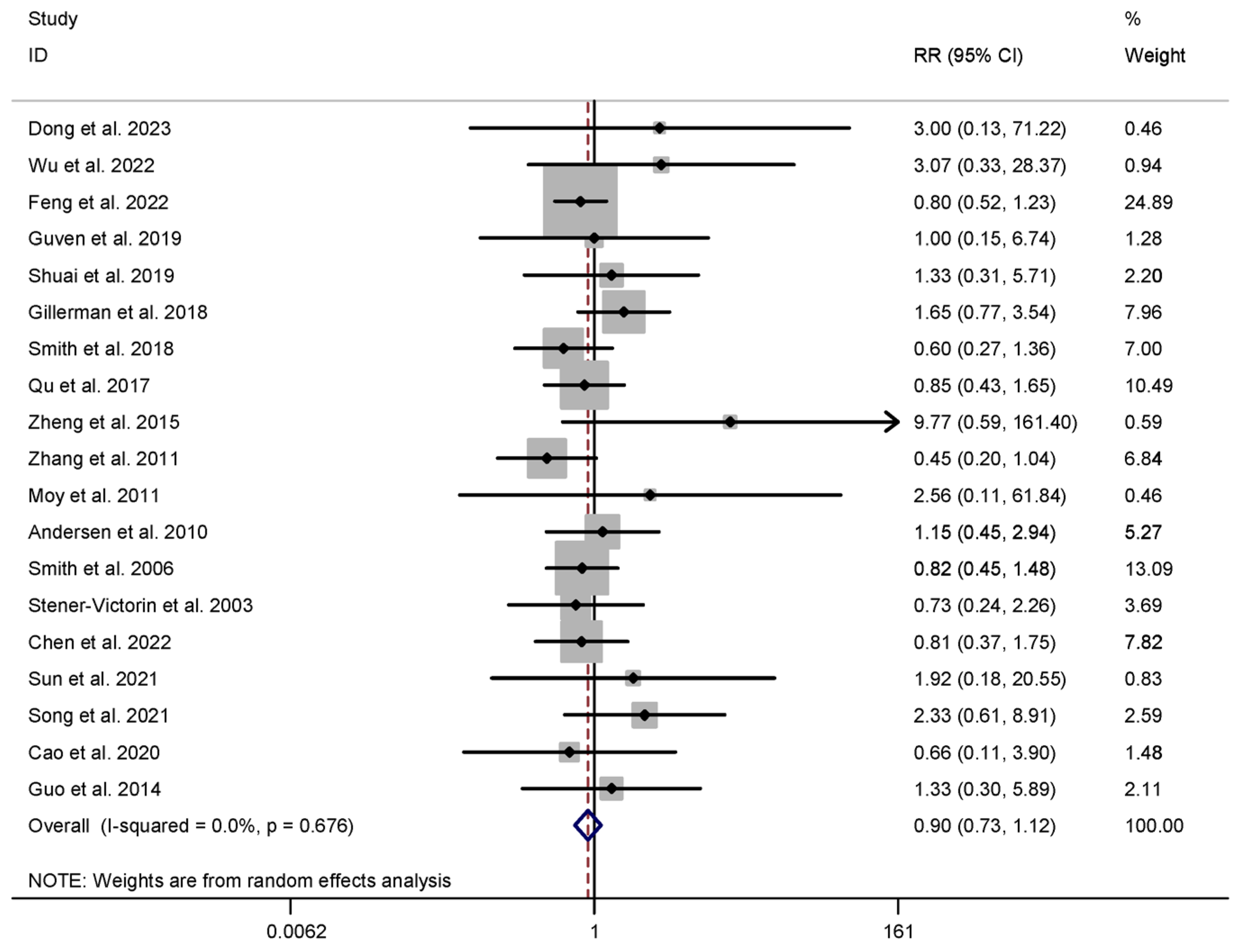
| Adverse events | 6 | 771 | 706 | 0.916 (0.726, 1.157) | 1.98 | 5 | 0.0% |
| Factor | Outcome or Subgroup | No. of Studies | No. of Patients | RR (95% CI) | I2 | p Value |
|---|---|---|---|---|---|---|
| IG vs. CG CPR | ||||||
| Type of CG | Sham Ac | 14 | 3730 | 1.218 (1.019, 1.455) | 69.7% | 0.030 |
| No acupuncture | 14 | 2880 | 1.416 (1.231, 1.629) | 42.9% | 0.000 | |
| Placebo HM | 8 | 3727 | 1.211 (1.071, 1.370) | 32.2% | 0.002 | |
| No HM | 5 | 616 | 1.101 (0.646, 1.876) | 72.7% | 0.724 | |
| LBR | ||||||
| Type of CG | Sham Ac | 8 | 2743 | 1.152 (0.892, 1.488) | 74.4% | 0.277 |
| No acupuncture | 7 | 1870 | 1.465 (1.163, 1.846) | 57.7% | 0.001 | |
| Placebo HM+ No HM | 3 | 2818 | 1.147 (1.010, 1.303) | 0.0% | 0.035 | |
| IR | ||||||
| Type of CG | Sham Ac | 9 | 2317 | 1.192 (0.952, 1.493) | 72.3% | 0.125 |
| No acupuncture | 5 | 1856 | 1.201 (1.031, 1.400) | 41.6% | 0.019 | |
| Placebo HM+ No HM | 5 | 3035 | 1.106 (0.968, 1.264) | 14.0% | 0.137 | |
| AE | ||||||
| Type of CG | Sham Ac+ No acupuncture | 13 | 2156 | 1.125 (0.926, 1.367) | 7.2% | 0.236 |
| Placebo HM+ No HM | 6 | 1477 | 0.916 (0.726, 1.157) | 0.0% | 0.463 | |
| Outcomes | No. of Studies | Sample Size | RR | Effects Model | 95% CI | I2 Value | Z Value | p Value |
|---|---|---|---|---|---|---|---|---|
| Vs. sham Ac/placebo HM | ||||||||
| LBR (Ac) | 8 | 2743 | 1.152 | Random | 0.892, 1.488 | 74.4% | 1.09 | 0.277 |
| CPR (Ac) | 14 | 3730 | 1.218 | Random | 1.019, 1.455 | 69.7% | 2.17 | 0.030 |
| CPR (HM) | 8 | 3727 | 1.211 | Random | 1.071, 1.370 | 32.2% | 3.04 | 0.002 |
| Vs. CG | ||||||||
| LBR (Ac) | 7 | 1870 | 1.465 | Random | 1.163, 1.846 | 57.7% | 3.24 | 0.001 |
| CPR (Ac) | 14 | 2880 | 1.416 | Random | 1.231, 1.629 | 42.9% | 4.88 | 0.000 |
| CPR (HM) | 5 | 616 | 1.101 | Random | 0.646, 1.876 | 72.7% | 0.35 | 0.724 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, X.; Wu, B.; Zhou, S.; Xu, Y.; Ogihara, A.; Nishimura, S.; Jin, Q.; Litscher, G. Integrating Acupuncture and Herbal Medicine into Assisted Reproductive Technology: A Systematic Review and Meta-Analysis of East Asian Traditional Medicine. Healthcare 2025, 13, 1326. https://doi.org/10.3390/healthcare13111326
Peng X, Wu B, Zhou S, Xu Y, Ogihara A, Nishimura S, Jin Q, Litscher G. Integrating Acupuncture and Herbal Medicine into Assisted Reproductive Technology: A Systematic Review and Meta-Analysis of East Asian Traditional Medicine. Healthcare. 2025; 13(11):1326. https://doi.org/10.3390/healthcare13111326
Chicago/Turabian StylePeng, Xiangping, Bo Wu, Siyu Zhou, Yinghan Xu, Atsushi Ogihara, Shoji Nishimura, Qun Jin, and Gerhard Litscher. 2025. "Integrating Acupuncture and Herbal Medicine into Assisted Reproductive Technology: A Systematic Review and Meta-Analysis of East Asian Traditional Medicine" Healthcare 13, no. 11: 1326. https://doi.org/10.3390/healthcare13111326
APA StylePeng, X., Wu, B., Zhou, S., Xu, Y., Ogihara, A., Nishimura, S., Jin, Q., & Litscher, G. (2025). Integrating Acupuncture and Herbal Medicine into Assisted Reproductive Technology: A Systematic Review and Meta-Analysis of East Asian Traditional Medicine. Healthcare, 13(11), 1326. https://doi.org/10.3390/healthcare13111326


_MD__MPH_PhD.png)





