What Shapes Quality of Life in Youth? A Multidimensional Approach from Lifestyle to Residential Context—Cor-School Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Instruments and Variables
2.3.1. Quality of Life
2.3.2. Anthropometric Variables
2.3.3. Biochemical Variables
2.3.4. Lifestyle Variables
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HRQoL | Health-related quality of life |
| WtH | Waist-to-height ratio |
| HDL | High-density lipoprotein |
| LDL | Low-density lipoprotein |
References
- Ravens-Sieberer, U.; Bullinger, M. Assessing health-related quality of life in chronically ill children with the German KINDL: First psychometric and content analytical results. Qual. Life Res. 1998, 7, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Villalonga-Olives, E.; Kawachi, I.; Almansa, J.; Witte, C.; Lange, B.; Kiese-Himmel, C.; Von Steinbüchel, N. Pediatric Health-Related Quality of Life: A Structural Equation Modeling Approach. PLoS ONE 2014, 9, e113166. [Google Scholar] [CrossRef] [PubMed]
- Haile, S.R.; Peralta, G.P.; Raineri, A.; Rueegg, S.; Ulytė, A.; Puhan, M.A.; Radtke, T.; Kriemler, S. Determinants of health-related quality of life in healthy children and adolescents during the COVID-19 pandemic: Results from a prospective longitudinal cohort study. Eur. J. Pediatr. 2024, 183, 2273–2283. [Google Scholar] [CrossRef] [PubMed]
- The BELLA study group; Ravens-Sieberer, U.; Erhart, M.; Wille, N.; Bullinger, M. Health-related quality of life in children and adolescents in Germany: Results of the BELLA study. Eur. Child Adolesc. Psychiatry 2008, 17, 148–156. [Google Scholar] [CrossRef]
- The KIDSCREEN group; Michel, G.; Bisegger, C.; Fuhr, D.C.; Abel, T. Age and gender differences in health-related quality of life of children and adolescents in Europe: A multilevel analysis. Qual. Life Res. 2009, 18, 1147–1157. [Google Scholar] [CrossRef]
- Meixner, L.; Cohrdes, C.; Schienkiewitz, A.; Mensink, G.B.M. Health-related quality of life in children and adolescents with overweight and obesity: Results from the German KIGGS survey. BMC Public Health 2020, 20, 1722. [Google Scholar] [CrossRef]
- Wang, J.; Jin, W.; Shi, L.; Geng, Y.; Zhu, X.; Hu, W. Health-Related Quality of Life in Children: The Roles of Age, Gender and Interpersonal Trust. Int. J. Environ. Res. Public Health 2022, 19, 15408. [Google Scholar] [CrossRef]
- Mikkelsen, H.T.; Småstuen, M.C.; Haraldstad, K.; Helseth, S.; Skarstein, S.; Rohde, G. Changes in health-related quality of life in adolescents and the impact of gender and selected variables: A two-year longitudinal study. Health Qual. Life Outcomes 2022, 20, 123. [Google Scholar] [CrossRef]
- Ventriglio, A.; Sancassiani, F.; Contu, M.P.; Latorre, M.; Di Slavatore, M.; Fornaro, M.; Bhugra, D. Mediterranean Diet and its Benefits on Health and Mental Health: A Literature Review. Clin. Pract. Epidemiol. Ment. Health 2020, 16, 156–164. [Google Scholar] [CrossRef]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef]
- Korkutata, A.; Korkutata, M.; Lazarus, M. The impact of exercise on sleep and sleep disorders. NPJ Biol. Timing Sleep 2025, 2, 5. [Google Scholar] [CrossRef]
- Jiménez-López, E.; Mesas, A.E.; Bizzozero-Peroni, B.; Fernández-Rodríguez, R.; Garrido-Miguel, M.; Victoria-Montesinos, D.; López-Bueno, R.; López-Gil, J.F. Clustering of Mediterranean dietary patterns linked with health-related quality of life in adolescents: The EHDLA study. Eur. J. Pediatr. 2023, 182, 4113–4121. [Google Scholar] [CrossRef]
- Lubans, D.; Richards, J.; Hillman, C.; Faulkner, G.; Beauchamp, M.; Nilsson, M.; Kelly, P.; Smith, J.; Raine, L.; Biddle, S. Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. Pediatrics 2016, 138, e20161642. [Google Scholar] [CrossRef] [PubMed]
- Shochat, T.; Cohen-Zion, M.; Tzischinsky, O. Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Med. Rev. 2014, 18, 75–87. [Google Scholar] [CrossRef]
- Grasaas, E.; Rohde, G.; Haraldstad, K.; Helseth, S.; Småstuen, M.C.; Skarstein, S.; Mikkelsen, H.T. Sleep duration in schooldays is associated with health-related quality of life in norwegian adolescents: A cross-sectional study. BMC Pediatr. 2023, 23, 473. [Google Scholar] [CrossRef]
- Ukegbu, T.E.; Wylie-Rosett, J.; Groisman-Perelstein, A.E.; Diamantis, P.M.; Rieder, J.; Ginsberg, M.; Lichtenstein, A.H.; Matthan, N.R.; Shankar, V. Waist-to-height ratio associated cardiometabolic risk phenotype in children with overweight/obesity. BMC Public Health 2023, 23, 1549. [Google Scholar] [CrossRef]
- Ezzatvar, Y.; Izquierdo, M.; Ramírez-Vélez, R.; Del Pozo Cruz, B.; García-Hermoso, A. Accuracy of different cutoffs of the waist-to-height ratio as a screening tool for cardiometabolic risk in children and adolescents: A systematic review and meta-analysis of diagnostic test accuracy studies. Obes. Rev. 2022, 23, e13375. [Google Scholar] [CrossRef] [PubMed]
- Buttitta, M.; Iliescu, C.; Rousseau, A.; Guerrien, A. Quality of life in overweight and obese children and adolescents: A literature review. Qual. Life Res. 2014, 23, 1117–1139. [Google Scholar] [CrossRef]
- Fiorentino, R.; Chiarelli, F. Treatment of Dyslipidaemia in Children. Biomedicines 2021, 9, 1078. [Google Scholar] [CrossRef]
- Ministerio de Vivienda y Agenda Urbana. Áreas Urbanas en España 2024; Secretaría General Técnica: Madrid, Spain, 2024. [Google Scholar]
- Tillmann, S.; Clark, A.F.; Gilliland, J.A. Children and Nature: Linking Accessibility of Natural Environments and Children’s Health-Related Quality of Life. Int. J. Environ. Res. Public Health 2018, 15, 1072. [Google Scholar] [CrossRef]
- Villanueva, K.; Badland, H.; Kvalsvig, A.; O’Connor, M.; Christian, H.; Woolcock, G.; Giles-Corti, B.; Goldfeld, S. Can the Neighborhood Built Environment Make a Difference in Children’s Development? Building the Research Agenda to Create Evidence for Place-Based Children’s Policy. Acad. Pediatr. 2016, 16, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Boraita, R.J.; Alsina, D.A.; Ibort, E.G.; Torres, J.M.D. Quality of life related to health and habits: Differences between adolescents in rural and urban environments. An. Pediatría Engl. Ed. 2022, 96, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Petrovič, F.; Maturkanič, P. Urban-Rural Dichotomy of Quality of Life. Sustainability 2022, 14, 8658. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- The BELLA Study Group; Bullinger, M.; Brütt, A.L.; Erhart, M.; Ravens-Sieberer, U. Psychometric properties of the KINDL-R questionnaire: Results of the BELLA study. Eur. Child Adolesc. Psychiatry 2008, 17, 125–132. [Google Scholar] [CrossRef]
- Norton, K.I. Standards for Anthropometry Assessment. In Kinanthropometry and Exercise Physiology, 4th ed.; Norton, K., Eston, R., Eds.; Routledge: New York, NY, USA, 2018; pp. 68–137. ISBN 978-1-315-38566-2. [Google Scholar]
- Wilson, P.W.; Abbott, R.D.; Garrison, R.J.; Castelli, W.P. Estimation of very-low-density lipoprotein cholesterol from data on triglyceride concentration in plasma. Clin. Chem. 1981, 27, 2008–2010. [Google Scholar] [CrossRef]
- Gidding, S.S.; Dennison, B.A.; Birch, L.L.; Daniels, S.R.; Gilman, M.W.; Lichtenstein, A.H.; Rattay, K.T.; Steinberger, J.; Stettler, N.; Van Horn, L. Dietary Recommendations for Children and Adolescents: A Guide for Practitioners: Consensus Statement From the American Heart Association. Circulation 2005, 112, 2061–2075. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Manchola-González, J.; Bagur-Calafat, C.; Girabent-Farrés, M. Fiabilidad de la versión española del Cuestionario de actividad física PAQ-C/Reliability of the Spanish Version of Questionnaire of Physical Activity PAQ-C. Rev. Int. Med. Cienc. Act. Física Deporte 2017, 17, 139–152. [Google Scholar] [CrossRef]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef]
- The Jamovi Project Jamovi 2025. Jamovi Project. Jamovi (Version 2.6) [Computer Software]. 2025. Available online: https://www.jamovi.org (accessed on 13 March 2025).
- Gallucci, M. GAMLj: General Analyses for the Linear Model in Jamovi, Version 2.6.44; GAMLj: Milan, Italy, 2019.
- Ravens-Sieberer, U.; Erhart, M.; Gosch, A.; Wille, N. The European KIDSCREEN Group Mental health of children and adolescents in 12 European countries—Results from the European KIDSCREEN study. Clin. Psychol. Psychother. 2008, 15, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Gao, K.; Wu, Z.; Guo, P. The influence of academic pressure on adolescents’ problem behavior: Chain mediating effects of self-control, parent–child conflict, and subjective well-being. Front. Psychol. 2022, 13, 954330. [Google Scholar] [CrossRef]
- Dam, V.A.T.; Dao, N.G.; Nguyen, D.C.; Vu, T.M.T.; Boyer, L.; Auquier, P.; Fond, G.; Ho, R.C.M.; Ho, C.S.H.; Zhang, M.W.B. Quality of life and mental health of adolescents: Relationships with social media addiction, Fear of Missing out, and stress associated with neglect and negative reactions by online peers. PLoS ONE 2023, 18, e0286766. [Google Scholar] [CrossRef]
- Steare, T.; Gutiérrez Muñoz, C.; Sullivan, A.; Lewis, G. The association between academic pressure and adolescent mental health problems: A systematic review. J. Affect. Disord. 2023, 339, 302–317. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, T.; Ribeiro, J.P.; De Matos, M.G.; Leal, I.; Ferreira, A. Health-Related Quality of Life in Children and Adolescents: Subjective Well Being. Span. J. Psychol. 2012, 15, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Spinneker, A.; Egert, S.; González-Gross, M.; Breidenassel, C.; Albers, U.; Stoffel-Wagner, B.; Huybrechts, I.; Manios, Y.; Venneria, E.; Molnar, D.; et al. Lipid, lipoprotein and apolipoprotein profiles in European adolescents and its associations with gender, biological maturity and body fat—The HELENA Study. Eur. J. Clin. Nutr. 2012, 66, 727–735. [Google Scholar] [CrossRef][Green Version]
- Galan-Lopez, P.; Sánchez-Oliver, A.J.; Ries, F.; González-Jurado, J.A. Mediterranean Diet, Physical Fitness and Body Composition in Sevillian Adolescents: A Healthy Lifestyle. Nutrients 2019, 11, 2009. [Google Scholar] [CrossRef]
- Wang, W.; Zhu, Y.; Yu, H.; Wu, C.; Li, T.; Ji, C.; Jiang, Y.; Ding, D. The impact of sleep quality on emotion regulation difficulties in adolescents: A chained mediation model involving daytime dysfunction, social exclusion, and self-control. BMC Public Health 2024, 24, 1862. [Google Scholar] [CrossRef]
- Hedin, G.; Norell-Clarke, A.; Hagell, P.; Tønnesen, H.; Westergren, A.; Garmy, P. Insomnia in Relation to Academic Performance, Self-Reported Health, Physical Activity, and Substance Use Among Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 6433. [Google Scholar] [CrossRef]
- Bauducco, S.V.; Özdemir, M.; Gradisar, M.; Boersma, K.; Bayram-Özdemir, S. Trajectories of insomnia symptoms and insufficient sleep duration in early adolescents: Associations with school stress. Sleep Adv. 2022, 3, zpac018. [Google Scholar] [CrossRef] [PubMed]
- Gradisar, M.; Gardner, G.; Dohnt, H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2011, 12, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Neil-Sztramko, S.E.; Caldwell, H.; Dobbins, M. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2021, 9, CD007651. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; Siahpush, M. Widening Rural–Urban Disparities in Life Expectancy, U.S., 1969–2009. Am. J. Prev. Med. 2014, 46, e19–e29. [Google Scholar] [CrossRef]
- Bole, A.; Bernstein, A.; White, M.J.; Council On Environmental Health And Climate Change; Bole, A.; Balk, S.J.; Byron, L.G.; Huerta-Montañez, G.M.; Landrigan, P.J.; Marcus, S.M.; et al. The Built Environment and Pediatric Health. Pediatrics 2024, 153, e2023064773. [Google Scholar] [CrossRef] [PubMed]
- Pfledderer, C.D.; Burns, R.D.; Byun, W.; Carson, R.L.; Welk, G.J.; Brusseau, T.A. School-based physical activity interventions in rural and urban/suburban communities: A systematic review and meta-analysis. Obes. Rev. 2021, 22, e13265. [Google Scholar] [CrossRef]
- UNICEF. Basis for a European Child Guarantee Action Plan in Spain; UNICEF: New York, NY, USA, 2021. [Google Scholar]
- Ow, N.; Mayo, N.E. Health-related quality of life scores of typically developing children and adolescents around the world: A meta-analysis with meta-regression. Qual. Life Res. 2020, 29, 2311–2332. [Google Scholar] [CrossRef]
| Variable | All (n = 571) | Girls (n = 254) | Boys (n = 358) | p-Values |
|---|---|---|---|---|
| Age (years) a | 11.64 ± 1.64 | 11.63 ± 1.65 | 11.65 ± 1.64 | 0.870 |
| Height (m) a | 1.53 ± 0.12 | 1.52 ± 0.11 | 1.54 ± 0.13 | 0.043 |
| Weight (kg) a | 46.87 ± 12.09 | 46.61 ± 11.37 | 47.05 ± 12.60 | 0.658 |
| WtH (cm·m−1) a | 0.43 ± 0.05 | 0.42 ± 0.06 | 0.43 ± 0.05 | <0.001 |
| Waist (cm) b | 65.80 ± 10.00 | 64.00 ± 9.13 | 66.50 ± 11.00 | <0.001 |
| Fat mass (%) a | 23.25 ± 6.21 | 25.61 ± 5.01 | 21.40 ± 6.44 | <0.001 |
| Muscle mass (kg) a | 33.96 ± 8.01 | 32.52 ± 6.87 | 35.08 ± 8.65 | 0.001 |
| Tanner stage, I–V c | 101/192/163/116/20 | 34/73/74/56/9 | 67/119/89/60/11 | 0.145 |
| IPAQ (MET-min·week−1) a | 2.99 ± 0.60 | 2.84 ± 0.56 | 3.09 ± 0.60 | <0.001 |
| KIDMED (AU) a | 6.19 ± 2.44 | 6.34 ± 2.51 | 6.09 ± 2.38 | 0.229 |
| PSQI, 0–21 (AU) b | 3.00 ± 2.00 | 3.00 ± 2.00 | 3.00 ± 2.00 | 0.871 |
| HDL (mmMol·dL−1) a | 48.13 ± 15.10 | 52.04 ± 14.29 | 45.35 ± 15.06 | <0.001 |
| LDL (mmMol·dL−1) a | 71.85 ± 25.32 | 76.51 ± 23.80 | 68.54 ± 25.87 | <0.001 |
| Effect | Estimate | SE | Lower 95% CI | Upper 95% CI | β | t | p |
|---|---|---|---|---|---|---|---|
| (Intercept) | 77.42 | 0.50 | 76.45 | 78.35 | −0.11 | 153.34 | <0.001 |
| Sex (B-G) | 0.19 | 0.97 | −1.67 | 2.10 | 0.03 | 0.19 | 0.847 |
| Age (years) | −1.07 | 0.28 | −1.61 | −0.53 | −0.15 | −3.78 | <0.001 |
| WtH (cm·m−1) | −0.12 | 0.28 | −0.64 | 0.43 | −0.02 | −0.44 | 0.661 |
| HDL (mmMol·dL−1) | −0.31 | 0.38 | −1.01 | 0.43 | −0.04 | −0.84 | 0.404 |
| LDL (mmMol·dL−1) | 0.25 | 0.36 | −0.39 | 0.92 | 0.04 | 0.69 | 0.493 |
| KIDMED (AU) | 0.72 | 0.32 | 0.09 | 1.37 | 0.10 | 2.29 | 0.023 |
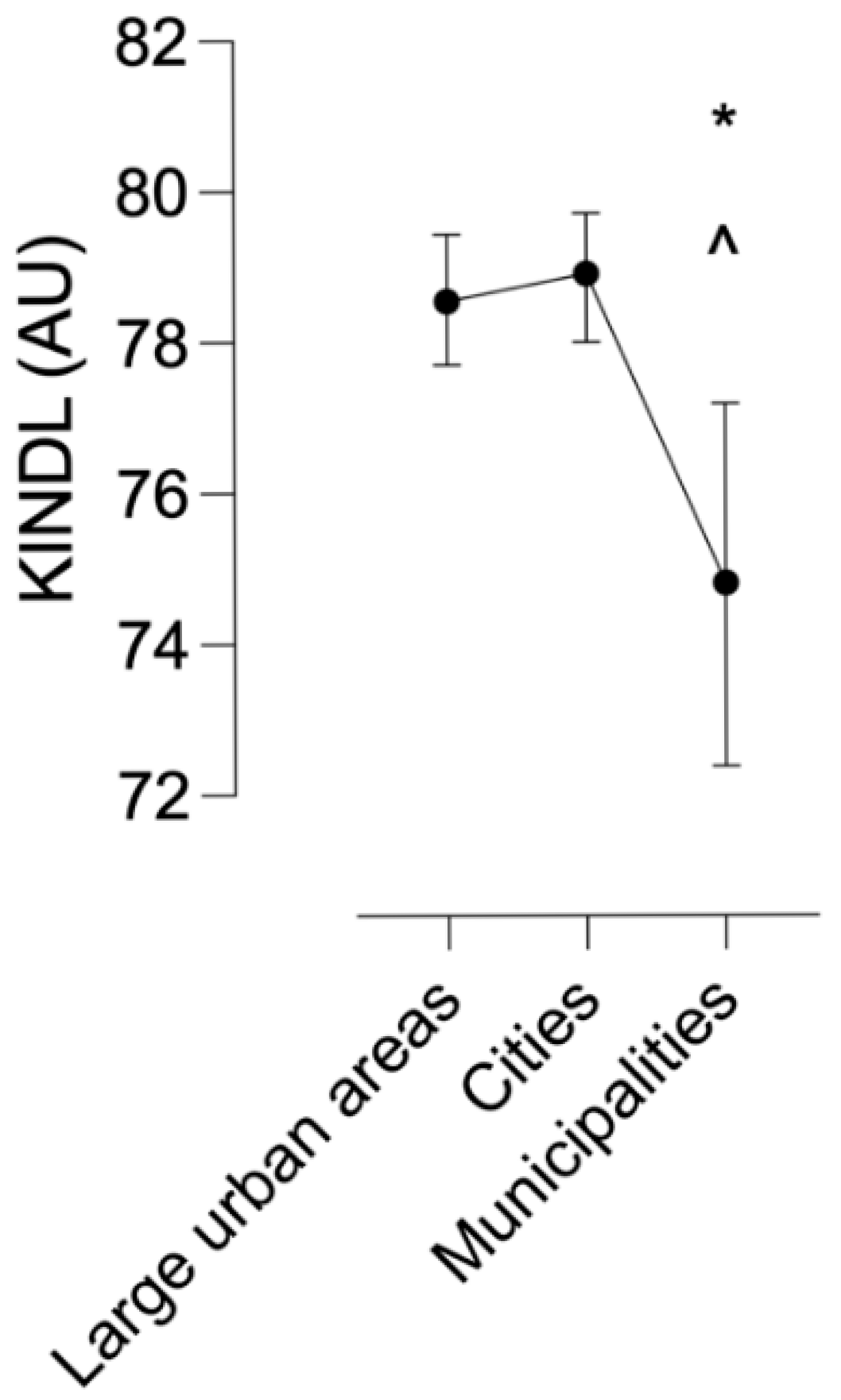
| Large urban areas–Cities a | −0.37 | 0.61 | −1.50 | 0.73 | −0.05 | −0.60 | 0.546 |
| Municipalities–Cities a | −4.10 | 1.35 | −6.78 | −1.66 | −0.58 | −3.03 | 0.003 |
| IPAQ (MET-min·week−1) | 0.54 | 0.32 | −0.04 | 1.19 | 0.08 | 1.69 | 0.093 |
| PSQI, 0–21 (AU) | −2.48 | 0.29 | −3.03 | −1.93 | −0.35 | −8.67 | <0.001 |
| (B-G) × (Large urban areas–Cities a) | −0.17 | 1.23 | −2.51 | 2.22 | −0.02 | −0.14 | 0.893 |
| (B-G) × (Municipalities–Cities a) | 3.87 | 2.72 | −0.90 | 8.93 | 0.55 | 1.42 | 0.155 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pano-Rodriguez, A.; Aixa-Requena, S.; Beltran-Garrido, J.V.; Batalla-Gavaldà, A.; Hernández-González, V.; Conesa-Milian, E.; López-Laval, I.; Reverter-Masia, J. What Shapes Quality of Life in Youth? A Multidimensional Approach from Lifestyle to Residential Context—Cor-School Study. Healthcare 2025, 13, 1256. https://doi.org/10.3390/healthcare13111256
Pano-Rodriguez A, Aixa-Requena S, Beltran-Garrido JV, Batalla-Gavaldà A, Hernández-González V, Conesa-Milian E, López-Laval I, Reverter-Masia J. What Shapes Quality of Life in Youth? A Multidimensional Approach from Lifestyle to Residential Context—Cor-School Study. Healthcare. 2025; 13(11):1256. https://doi.org/10.3390/healthcare13111256
Chicago/Turabian StylePano-Rodriguez, Alvaro, Saül Aixa-Requena, Jose Vicente Beltran-Garrido, Abraham Batalla-Gavaldà, Vicenç Hernández-González, Enric Conesa-Milian, Isaac López-Laval, and Joaquin Reverter-Masia. 2025. "What Shapes Quality of Life in Youth? A Multidimensional Approach from Lifestyle to Residential Context—Cor-School Study" Healthcare 13, no. 11: 1256. https://doi.org/10.3390/healthcare13111256
APA StylePano-Rodriguez, A., Aixa-Requena, S., Beltran-Garrido, J. V., Batalla-Gavaldà, A., Hernández-González, V., Conesa-Milian, E., López-Laval, I., & Reverter-Masia, J. (2025). What Shapes Quality of Life in Youth? A Multidimensional Approach from Lifestyle to Residential Context—Cor-School Study. Healthcare, 13(11), 1256. https://doi.org/10.3390/healthcare13111256














