Digital Health Literacy and Physical Activity Programme for Improvement of Quality of Life in Caregivers of People with Dementia (CAREFIT): Study Protocol
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Description of the Programme and Its Contents
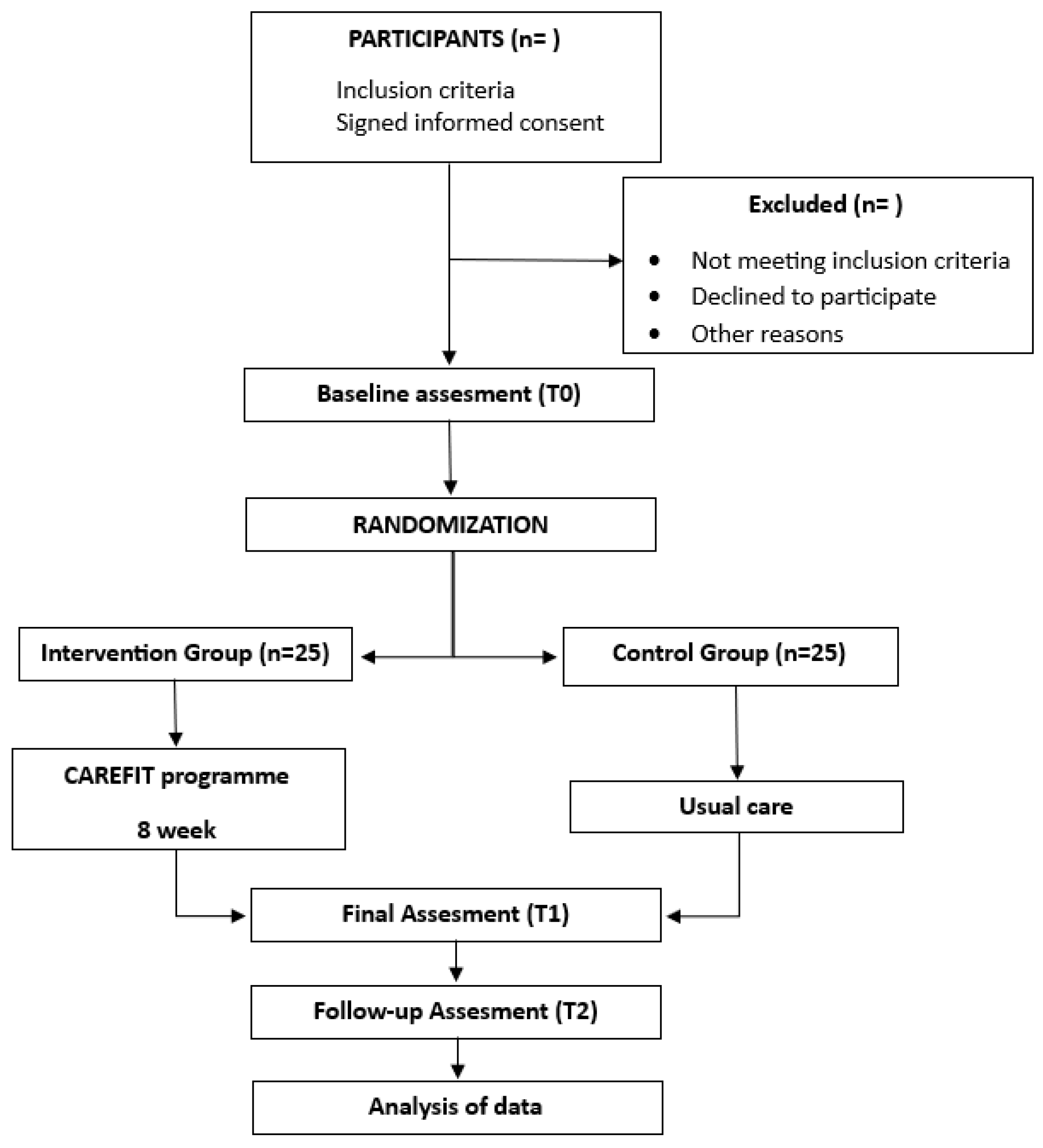
2.2. Randomised Controlled Trial
2.2.1. Desing
2.2.2. Ethics
2.2.3. Sample Calculation
2.2.4. Participants
2.2.5. Intervention
2.2.6. Measurements and Instrument
- (1)
- Quality of life
- EQ-5D-5L. This questionnaire measures the health status of participants and is divided into the following three assessments: (1) the assessment of several dimensions of health (mobility, self-care, activities of daily living, pain/discomfort, and anxiety/depression) using a descriptive Likert-type system from 1 to 5 points (no problems to problems/external impossibility); (2) the assessment of health status using a visual analogue scale; and (3) the assessment of social value using an index generated from the health states obtained in the first level [42]. It is a valid and reliable questionnaire both in the Spanish population [43] and in other populations [44] and in caregivers of people with other pathologies, with a validity of 0.987 [45].
- (2)
- Stress
- Perceived Stress Scale (PSS) [46]. This scale will measure perceived stress and consists of 14 questions that measure the degree to which situations in a person’s life are rated as stressful. The questions are formulated in terms of feelings and thoughts over the last month, and participants are asked to rate the frequency with which they have experienced them on a 5-point Likert scale. The score will be used to assess the participants’ level of stress. This scale showed a good reliability in the Spanish population, with a Cronbach’s alpha 0.82 [47].
- (3)
- Anxiety and depression
- General Health Questionnaire (GHQ-12) [48]. This scale will be used for the assessment of depression and anxiety. It is composed of 12 items (Yes/No). The cut-off point for the anxiety subscale is 4 or more points and 2 or more points for the depression subscale. Higher point values indicate a more severe problem, with 6 being the highest possible value for each subscale. The internal consistency analysis in Spanish population yielded an alpha coefficient of 0.78 [49].
- Geriatric Depression Scale (GDS). This questionnaire will measure depression and consists of 15 questions about how the participant has been feeling in the last 14 days, with the answers limited to ‘yes’ or ‘no’. The internal consistency analysis yielded an alpha coefficient of 0.87 [50].
- (4)
- Caregiver burden
- Zarit Burden Inventory (ZBI) (Spanish version). This 22-item questionnaire quantifies caregiver strain. This scale consists of 22 items in a Likert scale format, using a scale from one (never) to five (almost always). The recommended cut-off points are as follows: <46 indicating no caregiver burden; 46 to 56 items indicating mild caregiver burden, and >56 items indicating severe caregiver burden. Its internal consistency is high, with a Cronbach’s alpha coefficient of 0.91 [51].
- (5)
- Occupational balance
- Occupational Balance Questionnaire (OBQ-E). This questionnaire assesses participants’ satisfaction with their occupations by the means of 13 items, answered on a Likert scale from zero ‘strongly disagree’ to five ‘strongly agree’. The internal consistency obtained a value of Cronbach’s alpha of 0.948 [52].
- (6)
- Perceived social support
- Functional Social Support Questionnaire DukeUNC-11 [53]. This instrument consists of 11 items that are answered on a Likert scale from 1 to 5, where 1 represents ‘much less than I want’ and 5 ‘as much as I want’, where the questionnaire score ranges from 11 to 55 points. A score of 32 or above indicates standard social support, while a score below 32 suggests low perceived social support. In the Spanish population, the internal consistency of the questionnaire was found to be high, with a consistency coefficient of 0.90 [53].
2.2.7. Statistical Analysis
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abbott, A. DEMENTIA A problem for our age. Nature 2011, 475, S2–S4. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.; Wimo, A.; Guerchet, M.; Ali, G.C.; Wu, Y.T.; Prina, M. World Alzheimer Report. The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends; Alzheimer’s Disease International: London, UK, 2015. [Google Scholar]
- Ponjoan, A.; Garre-Olmo, J.; Blanch, J.; Fages, E.; Alves-Cabratosa, L.; Martí-Lluch, R.; Comas-Cufí, M.; Parramon, D.; Garcia-Gil, M.; Ramos, R. Epidemiology of dementia: Prevalence and incidence estimates using validated electronic health records from primary care. Clin. Epidemiol. 2019, 11, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Garre-Olmo, J. Epidemiology of Alzheimer’s disease and other dementias. Rev. Neurol. 2018, 66, 377–386. [Google Scholar] [CrossRef]
- Maria Vargas-Escobar, L. Nursing’s Contribution to the Quality of Life of Family Caregivers of Alzheimer Patients. Aquichan 2012, 12, 62–76. [Google Scholar] [CrossRef]
- Alzheimer’s Association. 2020 Alzheimer’s disease facts and figures. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2020, 16, 391–460. [Google Scholar] [CrossRef]
- Vitaliano, P.P. An Ironic Tragedy: Are Spouses of Persons with Dementia at Higher Risk for Dementia than Spouses of Persons without Dementia? J. Am. Geriatr. Soc. 2010, 58, 976–978. [Google Scholar] [CrossRef]
- Richardson, T.J.; Lee, S.J.; Berg-Weger, M.; Grossberg, G.T. Caregiver Health: Health of Caregivers of Alzheimer’s and Other Dementia Patients. Curr. Psychiatry Rep. 2013, 15, 367. [Google Scholar] [CrossRef]
- Xiong, C.; Biscardi, M.; Astell, A.; Nalder, E.; Cameron, J.I.; Mihailidis, A.; Colantonio, A. Sex and gender differences in caregiving burden experienced by family caregivers of persons with dementia: A systematic review. PLoS ONE 2020, 15, e0231848. [Google Scholar] [CrossRef]
- Alzheimer’s Association. 2023 Alzheimer’s disease facts and figures. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2023, 19, 1598–1695. [Google Scholar] [CrossRef]
- Pöysti, M.M.; Laakkonen, M.-L.; Strandberg, T.; Savikko, N.; Tilvis, R.S.; Eloniemi-Sulkava, U.; Pitkälä, K.H. Gender differences in dementia spousal caregiving. Int. J. Alzheimer’s Dis. 2012, 2012, 162960. [Google Scholar] [CrossRef]
- AOTA. Occupational Therapy Practice Framework: Domain and Process; American Occupational Therapy Association: Bethesda, MD, USA, 2014; Volume 56, pp. 609–639. [Google Scholar]
- Jiménez Buñuales, M.T.; González Diego, P.; Martín Moreno, J.M. International classification of functioning, disability and health (ICF) 2001. Rev. Esp. Salud Publica 2002, 76, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Durocher, E.; Gibson, B.E.; Rappolt, S. Justicia ocupacional: Una revisión de conceptos. J. Occup. Sci. 2019, 28, 561–573. [Google Scholar] [CrossRef]
- Liu, C.; Wang, D.; Liu, C.; Jiang, J.; Wang, X.; Chen, H.; Ju, X.; Zhang, X. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam. Med. Community Health 2020, 8, e000351. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Bliss, D.; Rolnick, C.; Jackson, J.; Arntson, C.; Mullins, J.; Hepburn, K. Health literacy needs related to incontinence and skin damage among family and friend caregivers of individuals with dementia. J. Wound Ostomy Cont. Nurs. Off. Publ. Wound Ostomy Cont. Nurses Soc./WOCN 2013, 40, 515–523. [Google Scholar] [CrossRef]
- Häikiö, K.; Cloutier, D.; Rugkåsa, J. Is health literacy of family carers associated with carer burden, quality of life, and time spent on informal care for older persons living with dementia? PLoS ONE 2020, 15, e0241982. [Google Scholar] [CrossRef]
- Kindig, D.A.; Panzer, A.M.; Nielsen-Bohlman, L. Health Literacy: A Prescription to End Confusion; National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Dassel, K.B.; Carr, D.C. Does dementia caregiving accelerate frailty? Findings from the Health and Retirement Study. Gerontologist 2016, 56, 444–450. [Google Scholar] [CrossRef]
- Fredman, L.; Bertrand, R.M.; Martire, L.M.; Hochberg, M.; Harris, E.L. Leisure-time exercise and overall physical activity in older women caregivers and non-caregivers from the Caregiver-SOF Study. Prev. Med. 2006, 43, 226–229. [Google Scholar] [CrossRef]
- da Silva-Sauer, L.; Garcia, R.B.; Fonsêca, É.K.G.; Fernández-Calvo, B. Physical activity and its relationship to burden and health concerns in family caregivers of people with dementia. Psychogeriatrics 2023, 24, 165–173. [Google Scholar] [CrossRef]
- Farina, N.; Williams, A.; Clarke, K.; Hughes, L.J.; Thomas, S.; Lowry, R.G.; Banerjee, S. Barriers, motivators and facilitators of physical activity in people with dementia and their family carers in England: Dyadic interviews. Aging Ment. Health 2021, 25, 1115–1124. [Google Scholar] [CrossRef]
- Leng, M.; Zhao, Y.; Xiao, H.; Li, C.; Wang, Z. Internet-Based Supportive Interventions for Family Caregivers of People With Dementia: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e19468. [Google Scholar] [CrossRef]
- Kales, H.C.; Gitlin, L.N.; Stanislawski, B.; Myra Kim, H.; Marx, K.; Turnwald, M.; Chiang, C.; Lyketsos, C.G. Effect of the WeCareAdvisor™ on family caregiver outcomes in dementia: A pilot randomized controlled trial. BMC Geriatr. 2018, 18, 113. [Google Scholar] [CrossRef]
- Deeken, F.; Rezo, A.; Hinz, M.; Discher, R.; Rapp, M.A. Evaluation of technology-based interventions for informal caregivers of patients with dementia—A meta-analysis of randomized controlled trials. Am. J. Geriatr. Psychiatry 2019, 27, 426–445. [Google Scholar] [CrossRef] [PubMed]
- Maciá, E.S.; López, B.B. Desarrollo de un programa psicoeducativo en inteligencia emocional para cuidadores principales de enfermos de Alzheimer. Eur. J. Investig. Health Psychol. Educ. 2015, 4, 257–266. [Google Scholar]
- Cristancho-Lacroix, V.; Wrobel, J.; Cantegreil-Kallen, I.; Dub, T.; Rouquette, A.; Rigaud, A.S. A web-based psychoeducational program for informal caregivers of patients with Alzheimer’s disease: A pilot randomized controlled trial. J. Med. Internet Res. 2015, 17, e117. [Google Scholar] [CrossRef] [PubMed]
- Velasquez, V.; Lopez, L.; Lopez, H.; Catano, N.; Munoz, E. The effect of an elderly people caregivers’ educational program: A cultural perspective. Rev. Salud Publica 2011, 13, 458–469. [Google Scholar]
- Sánchez-Pascual, P.; Mouronte-Liz, P.; Olazarán-Rodríguez, J. Beneficios de un programa de formación del cuidador en la demencia: Experiencia piloto desde la enfermería especializada. Rev. Neurol. 2001, 33, 432–434. [Google Scholar] [CrossRef]
- Vicente, M.M.; Delgado, M.G.; Fuertes, N.G.; Prieto, J.P. Effects of an Individual Home-Based Physical Exercise Program in Caregivers of Alzheimer Patients: A Pilot Study. Rev. Psicol. Deporte 2009, 18, 255–270. [Google Scholar]
- Lamotte, G.; Shah, R.C.; Lazarov, O.; Corcos, D.M. Exercise Training for Persons with Alzheimer’s Disease and Caregivers: A Review of Dyadic Exercise Interventions. J. Mot. Behav. 2017, 49, 365–377. [Google Scholar] [CrossRef]
- Xie, Y.; Shen, S.; Liu, C.; Hong, H.; Guan, H.; Zhang, J.; Yu, W. Internet-Based Supportive Interventions for Family Caregivers of People With Dementia: Randomized Controlled Trial. JMIR Aging 2024, 7, e50847. [Google Scholar] [CrossRef]
- Solorzano, C.S.; Orini, S.; Zanetti, O.; Chattat, R.; Pievani, M.; Festari, C. Effect of an eHealth intervention to support care management in caregivers of people with dementia: A pre-post pilot study. Alzheimer's Dement. 2023, 19, e082082. [Google Scholar] [CrossRef]
- Festari, C.; Bonomini, C.; Rosini, S.; Gattuso, M.; Singh Solorzano, C.; Zanetti, O.; Corbo, D.; Agnelli, G.; Quattrini, G.; Ferrari, C.; et al. Virtual Reality Combined With Psychoeducation to Improve Emotional Well-Being in Informal Caregivers of Alzheimer’s Disease Patients: Rationale and Study Design of a Randomized Controlled Trial. Int. J. Geriatr. Psychiatry 2024, 39, e6145. [Google Scholar] [CrossRef]
- Possin, K.L.; Merrilees, J.J.; Dulaney, S.; Bonasera, S.J.; Chiong, W.; Lee, K.; Hooper, S.M.; Allen, I.E.; Braley, T.; Bernstein, A. Effect of collaborative dementia care via telephone and internet on quality of life, caregiver well-being, and health care use: The care ecosystem randomized clinical trial. JAMA Intern. Med. 2019, 179, 1658–1667. [Google Scholar] [CrossRef]
- Usage of Content Management Systems for Websites. Available online: https://w3techs.com/technologies/overview/content_management/all/ (accessed on 28 February 2025).
- Moher, D.; Schulz, K.F.; Altman, D. La Declaración CONSORT: Recomendaciones revisadas para mejorar la calidad de los informes de ensayos aleatorizados de grupos paralelos. Rev. Sanid. Mil. 2017, 56, 23–28. [Google Scholar] [CrossRef]
- Walters, S.J.; Brazier, J.E. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual. Life Res. 2005, 14, 1523–1532. [Google Scholar] [CrossRef]
- Igarashi, A.; Fukuda, A.; Teng, L.; Ma, F.-F.; Dorey, J.; Onishi, Y. Family caregiving in dementia and its impact on quality of life and economic burden in Japan-web based survey. J. Mark. Access Health Policy 2020, 8, 1720068. [Google Scholar] [CrossRef]
- Cardinal, B.J.; Esters, J.; Cardinal, M.K. Evaluation of the revised physical activity readiness questionnaire in older adults. Med. Sci. Sports Exerc. 1996, 28, 468–472. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Hernandez, G.; Garin, O.; Pardo, Y.; Vilagut, G.; Pont, À.; Suárez, M.; Neira, M.; Rajmil, L.; Gorostiza, I.; Ramallo-Fariña, Y.; et al. Validity of the EQ-5D-5L and reference norms for the Spanish population. Qual. Life Res. 2018, 27, 2337–2348. [Google Scholar] [CrossRef]
- Buchholz, I.; Janssen, M.F.; Kohlmann, T.; Feng, Y.S. A Systematic Review of Studies Comparing the Measurement Properties of the Three-Level and Five-Level Versions of the EQ-5D. Pharmacoeconomics 2018, 36, 645–661. [Google Scholar] [CrossRef]
- Li, L.; Liu, C.; Cai, X.; Yu, H.; Zeng, X.; Sui, M.; Zheng, E.; Li, Y.; Xu, J.; Zhou, J.; et al. Validity and reliability of the EQ-5D-5 L in family caregivers of leukemia patients. BMC Cancer 2019, 19, 522. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Remor, E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span. J. Psychol. 2006, 9, 86–93. [Google Scholar] [CrossRef]
- Montón, C.; Pérez-Echevarría, M.; Campos, R.; García-Campayo, J.; Lobo, A.; Zaragoza Working Group for the Study of Psychiatric and Psychosomatic Morbidity. Escalas de ansiedad y depresión de Goldberg: Una guía de entrevista eficaz para la detección del malestar psíquico. Atención Primaria 1993, 12, 345–349. [Google Scholar]
- Sánchez-López Mdel, P.; Dresch, V. The 12-Item General Health Questionnaire (GHQ-12): Reliability, external validity and factor structure in the Spanish population. Psicothema 2008, 20, 839–843. [Google Scholar]
- Sanz, J.; Perdigón, A.L.; Vázquez, C. Adaptación española del Inventario para la Depresión de Beck-II (BDI-II): 2. Propiedades psicométricas en población general. Clín. Salud 2003, 14, 249–280. [Google Scholar]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontology 1980, 20, 649–655. [Google Scholar] [CrossRef]
- Gómez, P.P. Equilibrio Ocupacional en Estudiantes de Terapia Ocupacional. Ph.D. Thesis, Universidad Miguel Hernández, Elche, Spain, 2017. [Google Scholar]
- Saameño, J.A.B.; Luna del Castillo, J. Validity and reliability of the Duke-UNC-11 questionnaire of functional social support. Aten. Primaria 1996, 18, 153–156, 158–163. [Google Scholar]
- Pinquart, M.; Sörensen, S. Correlates of physical health of informal caregivers: A meta-analysis. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2007, 62, P126–P137. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and mental health effects of family caregiving. Am. J. Nurs. 2008, 108, 23–27, quiz 27. [Google Scholar] [CrossRef]
- Mc Donnell, E.; Ryan, A. Male caregiving in dementia: A review and commentary. Dementia 2013, 12, 238–250. [Google Scholar] [CrossRef] [PubMed]
- Czaja, S.J.; Schulz, R.; Lee, C.C.; Belle, S.H. A methodology for describing and decomposing complex psychosocial and behavioral interventions. Psychol. Aging 2003, 18, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Boots, L.M.; de Vugt, M.E.; van Knippenberg, R.J.; Kempen, G.I.; Verhey, F.R. A systematic review of Internet-based supportive interventions for caregivers of patients with dementia. Int. J. Geriatr. Psychiatry 2014, 29, 331–344. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Cámara, S.; Palomino-Moral, P.Á.; Moral-Fernández, L.; Frías-Osuna, A.; Parra-Anguita, L.; del-Pino-Casado, R. Perceived needs of the family caregivers of people with dementia in a mediterranean setting: A qualitative study. Int. J. Environ. Res. Public Health 2019, 16, 993. [Google Scholar] [CrossRef] [PubMed]
- Grossman, M.R.; Zak, D.K.; Zelinski, E.M. Mobile apps for caregivers of older adults: Quantitative content analysis. JMIR Mhealth Uhealth 2018, 6, e9345. [Google Scholar] [CrossRef]
- Brown, E.L.; Ruggiano, N.; Li, J.; Clarke, P.J.; Kay, E.S.; Hristidis, V. Smartphone-based health technologies for dementia care: Opportunities, challenges, and current practices. J. Appl. Gerontol. 2019, 38, 73–91. [Google Scholar] [CrossRef]
- Wagner, C.A.; Mohebbi, N. Urinary pH and stone formation. J. Nephrol. 2010, 23, S165–S169. [Google Scholar]
| Section | Modality | Module |
|---|---|---|
| Physical activities section | Virtual | Ranging from stretching |
| Strength, balance, or endurance | ||
| Educational section | Virtual | Healthy lifestyle habits |
| Self-care resources | ||
| Family care resources | ||
| Psychoemotional support section | Overload | |
| Virtual | Stress | |
| Anxiety | ||
| Depression | ||
| Social support section | Virtual | Information on support networks Care services for dependent persons |
| Assessment | Baseline | Final | Follow-Up |
|---|---|---|---|
| Socio-demographic data | X | ||
| Quality of Life | X | X | X |
| Stress | X | X | X |
| Anxiety | X | X | X |
| Depression | X | X | X |
| Caregiver burden | X | X | X |
| Occupational balance | X | X | X |
| Perceived social support | X | X | X |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrero-Sereno, P.; Palomo-López, P.; Mendoza-Muñoz, M.; Luna-Castaño, P.; Caballero-De la Calle, R.; Muñoz-Bermejo, L. Digital Health Literacy and Physical Activity Programme for Improvement of Quality of Life in Caregivers of People with Dementia (CAREFIT): Study Protocol. Healthcare 2025, 13, 1219. https://doi.org/10.3390/healthcare13111219
Ferrero-Sereno P, Palomo-López P, Mendoza-Muñoz M, Luna-Castaño P, Caballero-De la Calle R, Muñoz-Bermejo L. Digital Health Literacy and Physical Activity Programme for Improvement of Quality of Life in Caregivers of People with Dementia (CAREFIT): Study Protocol. Healthcare. 2025; 13(11):1219. https://doi.org/10.3390/healthcare13111219
Chicago/Turabian StyleFerrero-Sereno, Patricia, Patricia Palomo-López, María Mendoza-Muñoz, Patricia Luna-Castaño, Raquel Caballero-De la Calle, and Laura Muñoz-Bermejo. 2025. "Digital Health Literacy and Physical Activity Programme for Improvement of Quality of Life in Caregivers of People with Dementia (CAREFIT): Study Protocol" Healthcare 13, no. 11: 1219. https://doi.org/10.3390/healthcare13111219
APA StyleFerrero-Sereno, P., Palomo-López, P., Mendoza-Muñoz, M., Luna-Castaño, P., Caballero-De la Calle, R., & Muñoz-Bermejo, L. (2025). Digital Health Literacy and Physical Activity Programme for Improvement of Quality of Life in Caregivers of People with Dementia (CAREFIT): Study Protocol. Healthcare, 13(11), 1219. https://doi.org/10.3390/healthcare13111219









