The Impact of the COVID-19 Pandemic on Young Adults with Autism Spectrum Disorder: A Systematic Review
Abstract
1. Introduction
1.1. Background of the COVID-19 Pandemic
1.2. Autism Spectrum Disorder: Historical Context, Diagnosis, and Core Features
1.3. Impact of COVID-19 on Individuals with Autism Spectrum Disorder (ASD)
1.4. Research Gap and Study Aims
- (1)
- What specific effects did the COVID-19 pandemic have on young adults with ASD?
- (2)
- How did these effects evolve throughout the pandemic in this population, considering immediate impacts as well as short-, medium-, and long-term changes?
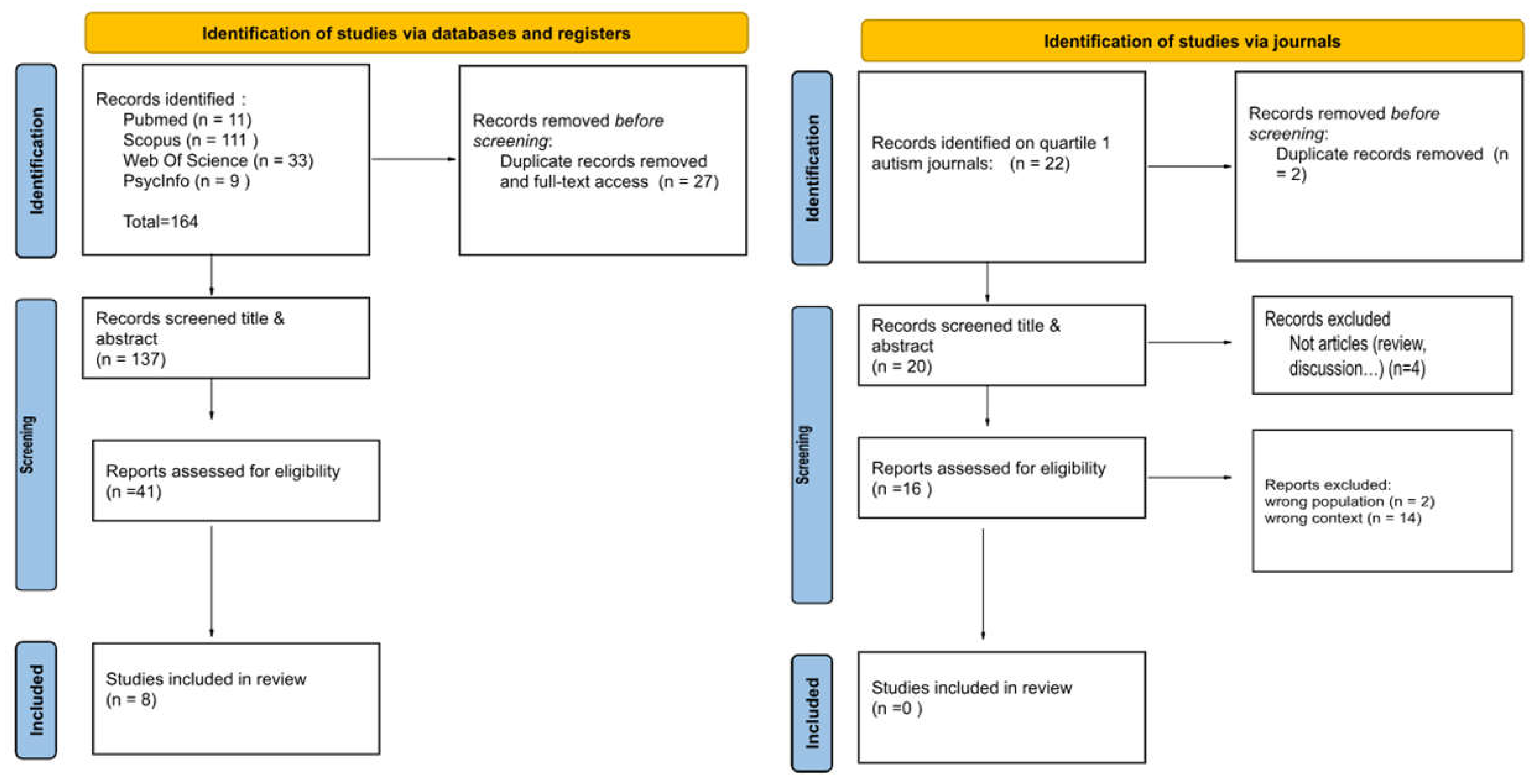
2. Materials and Methods
2.1. Search Strategy
2.2. Screening and Eligibility
2.3. Methodological Quality Assessment
2.4. Variables Studied
3. Results
3.1. Characteristics of Studies
3.2. Daily Life and Accessibility
3.3. Social and Emotional Impact
3.4. Behavioral and Cognitive Outcomes
3.5. Impact of COVID-19 on Young Adults: Before, During and After the Pandemic
3.6. Methodological Quality of the Studies and Risk of Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Adhanom Ghebreyesus, T. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry 2020, 19, 129–130. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Disability Considerations During the COVID-19 Outbreak; World Health Organization: Geneva, Switzerland, 2020; Available online: https://applications.emro.who.int/docs/9789292740603-eng.pdf (accessed on 18 March 2025).
- Centers for Disease Control and Prevention (CDC). Timeline of COVID-19 Developments in the U.S.; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020. Available online: https://www.cdc.gov/museum/timeline/covid19.html (accessed on 18 March 2025).
- Wilder-Smith, A.; Freedman, D.O. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020, 27, taaa020. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Public Health Measures for COVID-19 Prevention and Control. 2020. Available online: https://www.who.int/ (accessed on 19 March 2025).
- Kanner, L. Autistic disturbances of affective contact. Nerv. Child 1943, 2, 217–250. [Google Scholar]
- Asperger, H. Die Autistischen Psychopathen im Kindesalter. Arch. F. Psychiatr. 1944, 117, 76–136. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Hodges, H.; Fealko, C.; Soares, N. Autism spectrum disorder: Definition, epidemiology, causes, and clinical evaluation. Transl. Pediatr. 2020, 9 (Suppl. S1), S55–S65. [Google Scholar] [CrossRef]
- Masi, A.; DeMayo, M.M.; Glozier, N.; Guastella, A.J. An Overview of Autism Spectrum Disorder, Heterogeneity and Treatment Options. Neurosci. Bull. 2017, 33, 183–193. [Google Scholar] [CrossRef]
- Al-Dewik, N.; Al-Jurf, R.; Styles, M.; Tahtamouni, S.; Alsharshani, D.; Alsharshani, M.; Ahmad, A.I.; Khattab, A.; Al Rifai, H.; Walid Qoronfleh, M. Overview and Introduction to Autism Spectrum Disorder (ASD). Adv. Neurobiol. 2020, 24, 3–42. [Google Scholar] [CrossRef] [PubMed]
- Waizbard-Bartov, E.; Miller, M. Does the severity of autism symptoms change over time? A review of the evidence, impacts, and gaps in current knowledge. Clin. Psychol. Rev. 2023, 99, 102230. [Google Scholar] [CrossRef]
- Macchia, A.; Albantakis, L.; Zebhauser, P.T.; Brandi, M.L.; Schilbach, L.; Brem, A.K. Autistic Adults Avoid Unpredictability in Decision-Making. J. Autism Dev. Disord. 2024. [Google Scholar] [CrossRef]
- Najeeb, P.; Quadt, L. Autistic well-being: A scoping review of scientific studies from a neurodiversity-affirmative perspective. Neurodiversity 2024, 2, 27546330241233088. [Google Scholar] [CrossRef]
- Delemere, E.; Dounavi, K. Parent-Implemented Bedtime Fading and Positive Routines for Children with Autism Spectrum Disorders. J. Autism Dev. Disord. 2018, 48, 1002–1019. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.C.; Kassee, C.; Besney, R.; Bonato, S.; Hull, L.; Mandy, W.; Szatmari, P.; Ameis, S.H. Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. Lancet Psychiatry 2019, 6, 819–829. [Google Scholar] [CrossRef]
- Muskens, J.B.; Velders, F.P.; Staal, W.G. Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: A systematic review. Eur. Child Adolesc. Psychiatry 2017, 26, 1093–1103. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Kwong, A.S.F.; Pearson, R.M.; Adams, M.J.; Northstone, K.; Tilling, K.; Smith, D.; Fawns-Ritchie, C.; Bould, H.; Warne, N.; Zammit, S.; et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br. J. Psychiatry 2021, 218, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Niedzwiedz, C.L.; Green, M.J.; Benzeval, M.; Campbell, D.; Craig, P.; Demou, E.; Leyland, A.; Pearce, A.; Thomson, R.; Whitley, E.; et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: Longitudinal analyses of the UK Household Longitudinal Study. J. Epidemiol. Community Health 2021, 75, 224–231. [Google Scholar] [CrossRef]
- Patel, U.K.; Mehta, N.; Patel, A.; Patel, N.; Ortiz, J.F.; Khurana, M.; Urhoghide, E.; Parulekar, A.; Bhriguvanshi, A.; Patel, N.; et al. Long-Term Neurological Sequelae Among Severe COVID-19 Patients: A Systematic Review and Meta-Analysis. Cureus 2022, 14, e29694. [Google Scholar] [CrossRef]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Li, G.; Hilgenfeld, R.; Whitley, R.; De Clercq, E. Therapeutic strategies for COVID-19: Progress and lessons learned. Nat. Rev. Drug Discov. 2023, 22, 449–475. [Google Scholar] [CrossRef]
- Liu, B.; Stepien, S.; Dobbins, T.; Gidding, H.; Henry, D.; Korda, R.; Mills, L.; Pearson, S.A.; Pratt, N.; Vajdic, C.M.; et al. Effectiveness of COVID-19 vaccination against COVID-19 specific and all-cause mortality in older Australians: A population-based study. Lancet Reg. Health West. Pac. 2023, 40, 100928. [Google Scholar] [CrossRef]
- Narzisi, A. Handle the Autism Spectrum Condition During Coronavirus (COVID-19) Stay at Home Period: Ten Tips for Helping Parents and Caregivers of Young Children. Brain Sci. 2020, 10, 207. [Google Scholar] [CrossRef]
- Bentenuto, A.; Mazzoni, N.; Giannotti, M.; Venuti, P.; de Falco, S. Psychological impact of COVID-19 pandemic in Italian families of children with neurodevelopmental disorders. Res. Dev. Disabil. 2021, 109, 103840. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.J.; Liu, J.; Liu, K.; Koh, M.; Sherman, H.; Liu, S.; Tian, R.; Sukijthamapan, P.; Wang, J.; Fong, M.; et al. Probiotic and Oxytocin Combination Therapy in Patients with Autism Spectrum Disorder: A Randomized, Double-Blinded, Placebo-Controlled Pilot Trial. Nutrients 2021, 13, 1552. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Vaillancourt, T.; Szatmari, P.; Georgiades, K.; Krygsman, A. The impact of COVID-19 on the mental health of Canadian children youth. Facets 2021, 6, 1628–1648. [Google Scholar] [CrossRef]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef]
- Huang, Y.; Yang, C. A Metacognitive Approach to Reconsidering Risk Perceptions and Uncertainty: Understand Information Seeking During COVID-19. Sci. Commun. 2020, 42, 616–642. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental Health and the COVID-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Qiao, Y.; Shin, J.I.; Chen, T.K.; Inker, L.A.; Coresh, J.; Alexander, G.C.; Jackson, J.W.; Chang, A.R.; Grams, M.E. Association Between Renin-Angiotensin System Blockade Discontinuation and All-Cause Mortality Among Persons with Low Estimated Glomerular Filtration Rate. JAMA Intern. Med. 2020, 180, 718–726. [Google Scholar] [CrossRef]
- Rubin, G.J.; Wessely, S. The psychological effects of quarantining a city. BMJ 2020, 368, m313. [Google Scholar] [CrossRef]
- Marquenie, K.; Rodger, S.; Mangohig, K.; Cronin, A. Dinnertime and bedtime routines and rituals in families with a young child with an autism spectrum disorder. Aust. Occup. Ther. J. 2011, 58, 145–154. [Google Scholar] [CrossRef]
- Stoppelbein, L.; Biasini, F.; Pennick, M.; Greenin, L. Predicting Internalizing and Externalizing Symptoms among Children Diagnosed with an Autism Spectrum Disorder: The Role of Routines. J. Child Fam. Stud. 2016, 25, 251–261. [Google Scholar] [CrossRef]
- Oomen, D.; Nijhof, A.D.; Wiersema, J.R. The psychological impact of the COVID-19 pandemic on adults with autism: A survey study across three countries. Mol. Autism 2021, 12, 21. [Google Scholar] [CrossRef]
- Bishop-Fitzpatrick, L.; Kind, A.J.H. A Scoping Review of Health Disparities in Autism Spectrum Disorder. J. Autism Dev. Disord. 2017, 47, 3380–3391. [Google Scholar] [CrossRef] [PubMed]
- Hirvikoski, T.; Blomqvist, M. High self-perceived stress and poor coping in intellectually able adults with autism spectrum disorder. Autism: Int. J. Res. Pract. 2015, 19, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.L.; Corbett, B.A. A review of rhythm and responsiveness of cortisol in individuals with autism spectrum disorders. Psychoneuroendocrinology 2014, 49, 207–228. [Google Scholar] [CrossRef] [PubMed]
- Courtenay, K.; Perera, B. COVID-19 and people with intellectual disability: Impacts of a pandemic. Ir. J. Psychol. Med. 2020, 37, 231–236. [Google Scholar] [CrossRef]
- Frankova, H. The impact of COVID-19 on people with autism, learning disabilities and mental health conditions. Nurs. Resid. Care 2020, 22, 1–3. [Google Scholar] [CrossRef]
- Bal, V.H.; Mournet, A.M.; Glascock, T.; Shinall, J.; Gunin, G.; Jadav, N.; Zhang, H.; Brennan, E.; Istvan, E.; Kleiman, E.M. The emotional support plan: Feasibility trials of a brief, telehealth-based mobile intervention to support coping for autistic adults. Autism Int. J. Res. Pract. 2024, 28, 932–944. [Google Scholar] [CrossRef]
- Dekker, L.; Hooijman, L.; Louwerse, A.; Visser, K.; Bastiaansen, D.; Ten Hoopen, L.; De Nijs, P.; Dieleman, G.; Ester, W.; Van Rijen, S.; et al. Impact of the COVID-19 pandemic on children and adolescents with autism spectrum disorder and their families: A mixed-methods study protocol. BMJ Open 2022, 12, e049336. [Google Scholar] [CrossRef]
- Kreysa, H.; Schneider, D.; Kowallik, A.E.; Dastgheib, S.S.; Doğdu, C.; Kühn, G.; Ruttloff, J.M.; Schweinberger, S.R. Psychosocial and Behavioral Effects of the COVID-19 Pandemic on Children and Adolescents with Autism and Their Families: Overview of the Literature and Initial Data from a Multinational Online Survey. Healthcare 2022, 10, 714. [Google Scholar] [CrossRef] [PubMed]
- Lugo-Marín, J.; Gisbert-Gustemps, L.; Setien-Ramos, I.; Español-Martín, G.; Ibañez-Jimenez, P.; Forner-Puntonet, M.; Arteaga-Henríquez, G.; Soriano-Día, A.; Duque-Yemail, J.D.; Ramos-Quiroga, J.A. COVID-19 pandemic effects in people with Autism Spectrum Disorder and their caregivers: Evaluation of social distancing and lockdown impact on mental health and general status. Res. Autism Spectr. Disord. 2021, 83, 101757. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.A.; Sosnowy, C.; Kuo, A.A.; Shattuck, P.T. Transition of Individuals with Autism to Adulthood: A Review of Qualitative Studies. Pediatrics 2018, 141 (Suppl. S4), S318–S327. [Google Scholar] [CrossRef]
- Thompson, C.; Bölte, S.; Falkmer, T.; Girdler, S. To be understood: Transitioning to adult life for people with Autism Spectrum Disorder. PLoS ONE 2018, 13, e0194758. [Google Scholar] [CrossRef]
- Ng, C.S.M.; Ng, S.S.L. Impact of the COVID-19 pandemic on children’s mental health: A systematic review. Front. Psychiatry 2022, 13, 975936. [Google Scholar] [CrossRef]
- Bussières, E.L.; Malboeuf-Hurtubise, C.; Meilleur, A.; Mastine, T.; Hérault, E.; Chadi, N.; Montreuil, M.; Généreux, M.; Camden, C.; PRISME-COVID Team. Consequences of the COVID-19 Pandemic on Children’s Mental Health: A Meta-Analysis. Front. Psychiatry 2021, 12, 691659. [Google Scholar] [CrossRef]
- Meade, J. Mental Health Effects of the COVID-19 Pandemic on Children and Adolescents: A Review of the Current Research. Pediatr. Clin. North Am. 2021, 68, 945–959. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, I.W.M.; Lima, D.G.S.; Pires, J.P.; Vieira, N.B.; Brasil, A.A.G.M.; Pereira, Y.T.G.; de Oliveira, E.G.; de Menezes, H.L.; Lima, N.N.R.; Reis, A.O.A.; et al. Impacts of COVID-19 on children and adolescents: A systematic review analyzing its psychiatric effects. World J. Psychiatry 2022, 12, 1313–1322. [Google Scholar] [CrossRef]
- Theberath, M.; Bauer, D.; Chen, W.; Salinas, M.; Mohabbat, A.B.; Yang, J.; Chon, T.Y.; Bauer, B.A.; Wahner-Roedler, D.L. Effects of COVID-19 pandemic on mental health of children and adolescents: A systematic review of survey studies. SAGE Open Med. 2022, 10, 20503121221086712. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Critical Appraisal Skills Programme. 2018 CASP Checklist: Systematic Review. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 20 March 2025).
- Byers, J.F.; Beaudin, C.L. Critical appraisal tools facilitate the work of the quality professional. J. Healthc. Qual. 2001, 23, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Dixon-Woods, M.; Sutton, A.; Shaw, R.; Miller, T.; Smith, J.; Young, B.; Bonas, S.; Booth, A.; Jones, D. Appraising qualitative research for inclusion in systematic reviews: A quantitative and qualitative comparison of three methods. J. Health Serv. Res. Policy 2007, 12, 42–47. [Google Scholar] [CrossRef]
- Katrak, P.; Bialocerkowski, A.E.; Massy-Westropp, N.; Kumar, S.; Grimmer, K.A. A systematic review of the content of critical appraisal tools. BMC Med. Res. Methodol. 2004, 4, 22. [Google Scholar] [CrossRef]
- Brondino, N.; Damiani, S.; Politi, P. Effective strategies for managing COVID-19 emergency restrictions for adults with severe ASD in a daycare center in Italy. Brain Sci. 2020, 10, 436. [Google Scholar] [CrossRef] [PubMed]
- Davidson, A.; Pfeiffer, B. Community participation challenges for young adults with autism spectrum disorders during COVID-19 A photovoice study. Community Ment. Health J. 2024, 60, 60–71. [Google Scholar] [CrossRef]
- Mosquera, M.L.; Mandy, W.; Pavlopoulou, G.; Dimitriou, D. Autistic adults’ personal experiences of navigating a social world prior to and during Covid-19 lockdown in Spain. Res. Dev. Disabil. 2021, 117, 104057. [Google Scholar] [CrossRef]
- Pfeiffer, B.; Brusilovskiy, E.; Hallock, T.; Salzer, M.; Davidson, A.P.; Slugg, L.; Feeley, C. Impact of COVID-19 on community participation and mobility in young adults with autism spectrum disorders. J. Autism Dev. Disord. 2022, 52, 1553–1567. [Google Scholar] [CrossRef]
- Schnitzler, T.; Korn, C.; CHerpertz, S.; Fuchs, T. Emotion recognition in autism spectrum condition during the COVID-19 pandemic. Autism 2024, 28, 1690–1702. [Google Scholar] [CrossRef]
- Taylor, J.L.; Adams, R.E.; Pezzimenti, F.; Zheng, S.; Bishop, S.L. Job loss predicts worsening depressive symptoms for young adults with autism: A COVID-19 natural experiment. Autism Res. 2022, 15, 93–102. [Google Scholar] [CrossRef]
- Tovin, M.M.; Núñez-Gaunaurd, A. Implementation of Peer-Assisted Physical Activity Via Telehealth for Adults on the Autism Spectrum: A Mixed Methods Feasibility Study. Phys. Ther. 2024, 104, pzae005. [Google Scholar] [CrossRef]
- Valenti, M.; Pino, M.C.; Le Donne, I.; Vagnetti, R.; Tiberti, S.; Attanasio, M.; Mazza, M. Adaptive response of Italian young adults with autism to the COVID-19 pandemic: A longitudinal study. Res. Dev. Disabil. 2022, 131, 104333. [Google Scholar] [CrossRef]
- Pazhoohi, F.; Forby, L.; Kingstone, A. Facial masks affect emotion recognition in the general population and individuals with autistic traits. PLoS ONE 2021, 16, e0257740. [Google Scholar] [CrossRef] [PubMed]
- Fujioka, K.; O’Neil, P.M.; Davies, M.; Greenway, F.; Lau, C.W.D.; Claudius, B.; Skjøth, T.V.; Bjørn Jensen, C.; Wilding, P.H.J. Early Weight Loss with Liraglutide 3.0 mg Predicts 1-Year Weight Loss and Is Associated with Improvements in Clinical Markers. Obesity 2016, 24, 2278–2288. [Google Scholar] [CrossRef] [PubMed]
- Klin, A.; Jones, W.; Schultz, R.; Volkmar, F.; Cohen, D. Visual fixation patterns during viewing of naturalistic social situations as predictors of social competence in individuals with autism. Arch. Gen. Psychiatry 2002, 59, 809–816. [Google Scholar] [CrossRef]
- Cassidy, S.A.; Gould, K.; Townsend, E.; Pelton, M.; Robertson, A.E.; Rodgers, J. Is Camouflaging Autistic Traits Associated with Suicidal Thoughts and Behaviours? Expanding the Interpersonal Psychological Theory of Suicide in an Undergraduate Student Sample. J. Autism Dev. Disord. 2020, 50, 3638–3648. [Google Scholar] [CrossRef]
- Wigham, S.; Rodgers, J.; South, M.; McConachie, H.; Freeston, M. The interplay between sensory processing abnormalities, intolerance of uncertainty, anxiety and restricted and repetitive behaviours in autism spectrum disorder. J. Autism Dev. Disord. 2015, 45, 943–952. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Zhu, Z.; Zhang, X.; Tang, H.; Xing, J.; Hu, X.; Lu, J.; Qu, X. Identifying Autism with Head Movement Features by Implementing Machine Learning Algorithms. J. Autism Dev. Disord. 2022, 52, 3038–3049. [Google Scholar] [CrossRef]
- Colizzi, M.; Lasalvia, A.; Ruggeri, M. Prevention and early intervention in youth mental health: Is it time for a multidisciplinary and trans-diagnostic model for care? Int. J. Ment. Health Syst. 2020, 14, 23. [Google Scholar] [CrossRef]
- Kalb, L.G.; Badillo-Goicoechea, E.; Holingue, C.; Riehm, K.E.; Thrul, J.; Stuart, E.A.; Smail, E.J.; Law, K.; White-Lehman, C.; Fallin, D. Psychological distress among caregivers raising a child with autism spectrum disorder during the COVID-19 pandemic. Autism Res. 2021, 14, 2183–2188. [Google Scholar] [CrossRef]
- Aarabi, M.A.; Abdi, K.; Khanjani, M.S. Challenges of accessing and using rehabilitation services in people with autism spectrum disorder: A systematic review. J. Rehabil. 2021, 22, 260–277. [Google Scholar] [CrossRef]
- Jodra, M.; García-Domingo, M. Mediating effect of autistic traits between the emotional impact of pandemic and depressive symptoms. Acción Psicológica 2023, 19, 43–54. [Google Scholar] [CrossRef]
- Carter, A.S.; Martínez-Pedraza Fde, L.; Gray, S.A. Stability and individual change in depressive symptoms among mothers raising young children with ASD: Maternal and child correlates. J. Clin. Psychol. 2009, 65, 1270–1280. [Google Scholar] [CrossRef]
- Lloyd, T.; Hastings, R.P. Psychological variables as correlates of adjustment in mothers of children with intellectual disabilities: Cross-sectional and longitudinal relationships. J. Intellect. Disabil. Res. 2008, 52, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Giallo, R.; Wood, C.E.; Jellett, R.; Porter, R. Fatigue, wellbeing and parental self-efficacy in mothers of children with an autism spectrum disorder. Autism. 2013, 17, 465–480. [Google Scholar] [CrossRef]
- Warreman, E.B.; Lloyd, S.E.; Nooteboom, L.A.; Leenen, P.J.M.; Terry, M.B.; Hoek, H.W.; van Rossum, E.F.C.; Vermeiren, R.R.J.M.; Ester, W.A. Psychological, behavioural, and physical aspects of caregiver strain in autism-caregivers: A cohort study. EClinicalMedicine 2023, 64, 102211. [Google Scholar] [CrossRef]
- Vigna, E.; Meek, A.; Beyer, S. Supported employment, quality of jobs and employment typicalness: The experience of the Engage to Change project. J. Appl. Res. Intellect. Disabil. 2024, 37, e13226. [Google Scholar] [CrossRef]
- Ozsivadjian, A.; Milner, V.; Pickard, H.; Hollocks, M.J.; Gaigg, S.B.; Colvert, E.; Happé, F.; Magiati, I. Autistic and non-autistic young people’s and caregivers’ perspectives on COVID-19-related schooling changes and their impact on emotional well-being: An opportunity for change? Autism 2022, 27, 1477–1491. [Google Scholar] [CrossRef] [PubMed]
- Magklara, K.; Kyriakopoulos, M. The impact of the COVID-19 pandemic on children and young people. Psychiatriki 2023, 34, 265–268. [Google Scholar] [CrossRef]
- Featherstone, K.; Northcott, A.; Boddington, P.; Edwards, D.; Vougioukalou, S.; Bale, S.; Harrison Dening, K.; Logan, K.; Tope, R.; Kelly, D.; et al. Understanding Approaches to Continence Care for People Living with Dementia in Acute Hospital Settings: An Ethnographic Study; National Institute for Health and Care Research: London, UK, 2022. [Google Scholar]
- Friedman, S.; James, M.; Brocklebank, J.; Cox, S.; Morrison, S. Facilitating Nature-Based Learning with Autistic Students. Child. Educ. 2023, 99, 14–23. [Google Scholar] [CrossRef]
- Almeida, M.L.; Garon-Carrier, G.; Cinar, E.; Frizzo, G.B.; Fitzpatrick, C. Prospective associations between child screen time and parenting stress and later inattention symptoms in preschoolers during the COVID-19 pandemic. Front. Psychol. 2023, 14, 1053146. [Google Scholar] [CrossRef]
- Brosnan, M.; Gavin, J. The impact of higher levels of autistic traits on risk of hikikomori (pathological social withdrawal) in young adults. PLoS ONE 2023, 18, e0281833. [Google Scholar] [CrossRef] [PubMed]
- Shakeshaft, A.; Heron, J.; Blakey, R.; Riglin, L.; Davey Smith, G.; Stergiakouli, E.; Tilling, K.; Thapar, A. Co-development of attention deficit hyperactivity disorder and autistic trait trajectories from childhood to early adulthood. J. Child Psychol. Psychiatry Allied Discip. 2023, 64, 1596–1607. [Google Scholar] [CrossRef] [PubMed]
- Mottron, L.; Bzdok, D. Autism spectrum heterogeneity: Fact or artifact? Psiquiatr. Mol. 2020, 25, 3178–3185. [Google Scholar] [CrossRef]
- Barreto, C.; Curtin, A.; Topoglu, Y.; Day-Watkins, J.; Garvin, B.; Foster, G.; Ormanoglu, Z.; Sheridan, E.; Connell, J.; Bennett, D.; et al. Prefrontal Cortex Responses to Social Video Stimuli in Young Children with and Without Autism Spectrum Disorder. Brain Sci. 2024, 14, 503. [Google Scholar] [CrossRef]
- Arnett, J.J. Emerging adulthood: A theory of development from the late teens through the twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Anthony, N.; Bobzien, J. Using Two Formats of a Social Story to Increase the Verbal Initiations and On-Topic Responses of Two Adolescents with Autism Spectrum Disorders. J. Autism Dev. Disord. 2022, 52, 4138–4149. [Google Scholar] [CrossRef]
- Clarke, E.; Hull, L.; Loomes, R.; McCormick, C.E.B.; Sheinkopf, S.J.; Mandy, W. Assessing gender differences in autism spectrum disorder using the Gendered Autism Behavioral Scale (GABS): An exploratory study. Res. Autism Spectr. Disord. 2021, 88, 101844. [Google Scholar] [CrossRef]
- Hume, K.; Sreckovic, M.; Snyder, K.; Carnahan, C.R. Smooth Transitions: Helping Students with Autism Spectrum Disorder Navigate the School Day. Teach. Except. Child. 2014, 47, 35–45. [Google Scholar] [CrossRef]
- Levy, S.E.; Giarelli, E.; Lee, L.C.; Schieve, L.A.; Kirby, R.S.; Cunniff, C.; Nicholas, J.; Reaven, J.; Rice, C.E. Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. J. Dev. Behav. Pediatr. 2010, 31, 267–275. [Google Scholar] [CrossRef]
| Authors | Aim of the Study | Country of Sample | Study Design | Age (M/SD) | Gender Distribution (Female/Male/Others) | Groups Comparison | COVID-19 Phase |
|---|---|---|---|---|---|---|---|
| Brondino et al. [59] | This study aimed to evaluate the impact of COVID-19 restrictions on challenging behaviors in individuals with severe ASD. | Italy | Longitudinal | 22.72 ± 4.75 | 27.8%/72.2% | Autistics before vs. Autistic during the COVID-19 restrictions | First stage (between 19 February 2020 and 4 March 2020). |
| Davidson and Pfeiffer [60] | This study explores community participation barriers and facilitators for autistic individuals during COVID-19, using Photovoice methodology. | USA | Cross-sectional | 20.5 ± 1.44 | 18%/76%/6% others | Autistic individuals with vs. without co-occurring mental health conditions during COVID-19. | Early COVID-19 (summer of 2020) |
| Mosquera et al. [61] | This study explored the lived experiences of autistic adults regarding social expectations before and during the first COVID-19 lockdown in Spain. | Spain | Longitudinal | 30.2 ± 5.06 | 20%/60%/20% non binary | Autistic before vs. Autistic during the first COVID-19 lockdown in Spain. | First COVID-19 lockdown |
| Pfeiffer et al. [62] | This study examined the impact of COVID-19 on community mobility and participation for young adults with ASD. | USA | Longitudinal | 23.5 ± 2.4. | 33.33%/66.67% | Autistic Before vs. Autistic after the COVID-19 pandemic. | Beginning of the COVID-19 lockdown (between March 20th and April 2nd/between April 20th and May 3rd). |
| Schnitzler et al. [63] | This study investigated how partial face covering, such as masks, affects emotion recognition in individuals with ASD. | Germany | Cross-sectional | 28.08 ± 9.09 | 19.44%/80.56% | ASD vs. control. | From August to December 2021, during the mandated outdoor mask-wearing period. |
| Taylor et al. [64] | This study examined whether employment changes due to COVID-19 predicted increased depressive symptoms in young adults with ASD. | USA | Longitudinal | 26.5 ± 4.91 | 46.9/47.6%/5.6% others | ADS with employment changes during COVID-19 vs. ADS no employment changes. | Initial reopening phase (May 2020). |
| Tovin & Núñez-Gaunaurd [65] | This study examined the feasibility and acceptability of the Physical Activity Connections program via Telehealth, implemented during the COVID-19 pandemic lockdown as an alternative to in-person programming for autistic adults. | USA | Longitudinal | 25.83 ± 3.91 | 38.8/61.1% | ASD physical activity intervention vs. ASD without physical activity intervention | COVID-19 quarantine lockdown |
| Valenti et al. [66] | This study aimed to evaluate the adaptive behavior of young adults with ASD. | Italy | Longitudinal | 21.95 ± 5.78 | 31.82%/68.18% | ASD with no access to in-person care (only telehealth) vs. ASD with access to in-person care | During the first COVID-19 lockdown (T0), after 6 months (T1), and after 1 years (T2). |
| Authors | Domains Covered | Main Findings |
|---|---|---|
| Brondino et al. [59] | Behavioral and Cognitive | No significant changes in behaviors after COVID-19 restrictions. |
| Davidson and Pfeiffer [60] | Daily Life and Accessibility | Transportation was identified as a barrier 32% of the time and a facilitator 0%. |
| Social and Emotional Impact | COVID-19 was identified as a barrier 47% of the time and facilitator 21% of the time. | |
| Mosquera et al. [61] | Daily Life and Accessibility | Participants noted several impacts on their daily lives. Anxiety and insecurity grew due to public insults, but some felt less pressure to mask autistic traits. The extra time for personal interests and family was valued, and applause for healthcare workers was seen as a symbol of unity. Remote work provided new inclusion opportunities, while shortages in specialized services limited access to care and support. |
| Pfeiffer et al. [62] | Daily Life and Accessibility | Significant reduction in daily activities, travel, and transportation; mobility remained lower than pre-pandemic levels (GPS data). |
| Schnitzler et al. [63] | Social and Emotional Impact | ASD group had more difficulties recognizing emotions (fear, pride, embarrassment and anger) than the non-ASD group, especially with masks/sunglasses. |
| Behavioral and Cognitive Outcomes | There were no significant differences between the ASD and non-ASD groups in emotion recognition or spatial distance, as both groups maintained similar interpersonal distances. | |
| Taylor et al. [64] | Daily Life and Accessibility | A majority of autistic individuals reported employment disruptions during the pandemic, while 30% experienced positive changes. Negative perceptions of these changes were associated with increased depressive symptoms. |
| Tovin & Núñez-Gaunaurd [65] | Social and Emotional Impact | Employment and Mental Health: Job loss linked to increased depressive symptoms (+3.76 points) in adults with ASD. |
| Social and Emotional Impact | Physical Activity via Telehealth: 80% attendance; <20% dropout; high satisfaction and goal achievement; technology boosted engagement. | |
| Valenti et al. [66] | Daily Life and Accessibility | Autonomy declined, especially in hygiene, dressing, and eating, with younger individuals being more affected. Disruptions in routines also led to a decrease in domestic skills and greater reliance on parents. |
| Social and Emotional Impact | Interpersonal Relationships: Significant reduction between T0-T2 and T1-T2; isolation and social routine disruption likely increased stress and anxiety. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miranda Gálvez, A.L.; Pacheco-Unguetti, A.P. The Impact of the COVID-19 Pandemic on Young Adults with Autism Spectrum Disorder: A Systematic Review. Healthcare 2025, 13, 1216. https://doi.org/10.3390/healthcare13111216
Miranda Gálvez AL, Pacheco-Unguetti AP. The Impact of the COVID-19 Pandemic on Young Adults with Autism Spectrum Disorder: A Systematic Review. Healthcare. 2025; 13(11):1216. https://doi.org/10.3390/healthcare13111216
Chicago/Turabian StyleMiranda Gálvez, Azahara Leonor, and Antonia Pilar Pacheco-Unguetti. 2025. "The Impact of the COVID-19 Pandemic on Young Adults with Autism Spectrum Disorder: A Systematic Review" Healthcare 13, no. 11: 1216. https://doi.org/10.3390/healthcare13111216
APA StyleMiranda Gálvez, A. L., & Pacheco-Unguetti, A. P. (2025). The Impact of the COVID-19 Pandemic on Young Adults with Autism Spectrum Disorder: A Systematic Review. Healthcare, 13(11), 1216. https://doi.org/10.3390/healthcare13111216


_MD__MPH_PhD.png)





