User Experiences and Attitudes Toward Sharing Wearable Activity Tracker Data with Healthcare Providers: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting and Participants
2.3. Variables
2.3.1. Participant and Wearable Activity Tracker Characteristics
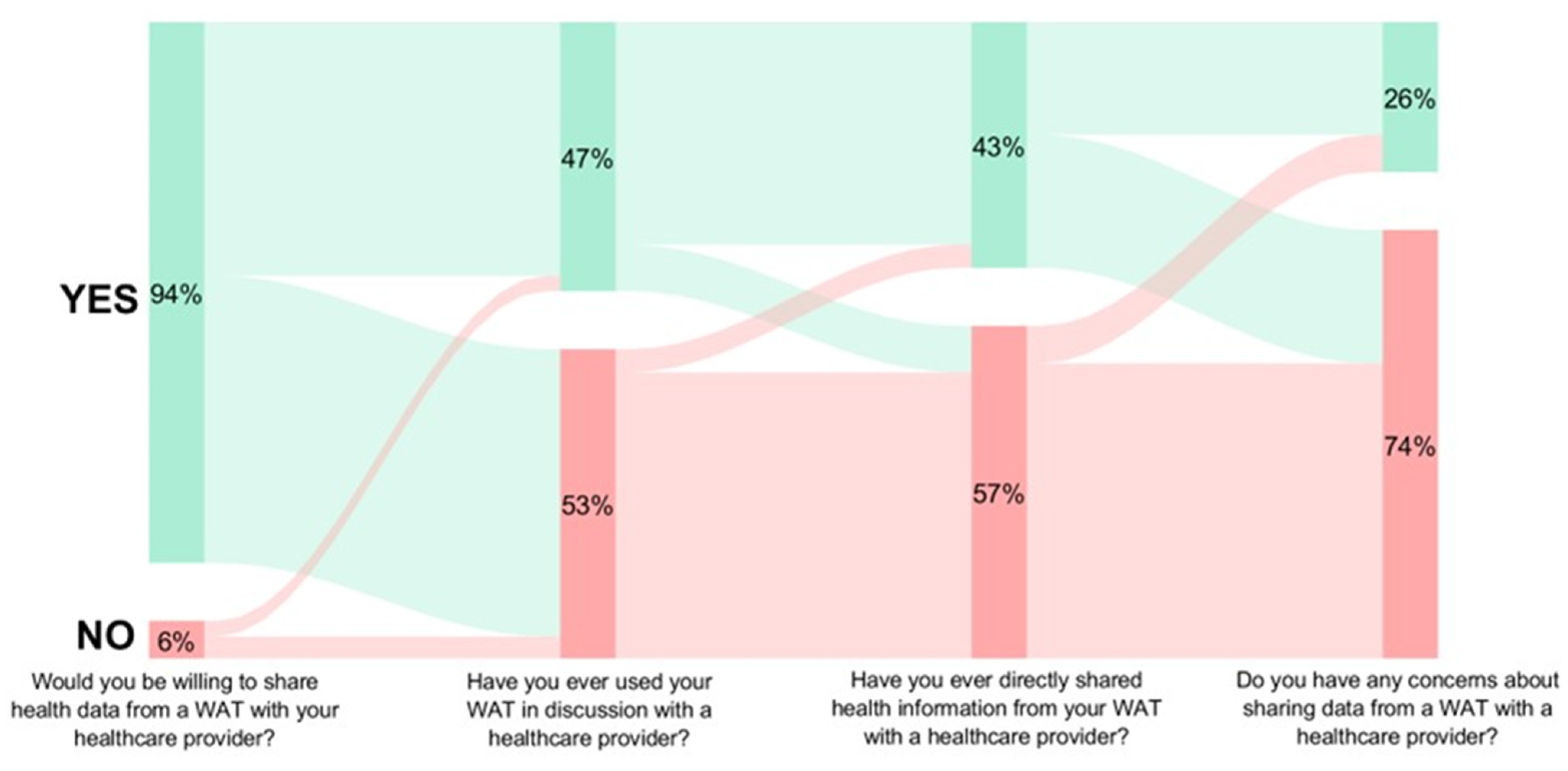
2.3.2. Data Sharing with Healthcare Providers
- (1)
- “Have you ever used your WAT in discussions with a healthcare provider?”
- (2)
- “Have you ever directly shared health information from your WAT with a healthcare provider?”
- (3)
- “Would you be willing to share health data from a WAT with your healthcare provider?”
- (4)
- “Do you have any concerns about sharing health data from a WAT with a healthcare provider?”
2.4. Statistical Analysis
3. Results
3.1. Participants
3.2. Wearable Activity Tracker Characteristics
3.3. Health Data Sharing
3.4. Subgroup Analyses
4. Discussion
4.1. Strengths and Limitations
4.2. Implications and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WAT | Wearable Activity Tracker |
| INT | International Dollars |
| AUD | Australian Dollars |
| USD | United States Dollars |
| US | United States |
References
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2019.
- Li, J.; Cao, D.; Huang, Y.; Chen, Z.; Wang, R.; Dong, Q.; Wei, Q.; Liu, L. Sleep duration and health outcomes: An umbrella review. Sleep Breath. 2022, 26, 1479–1501. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Friedenreich, C.; Shiroma, E.J.; Lee, I.M. Physical inactivity and non-communicable disease burden in low-income, middle-income and high-income countries. Br. J. Sports Med. 2021, 56, 101–106. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2015, 115, 780–800.e5. [Google Scholar] [CrossRef] [PubMed]
- Medic, G.; Wille, M.; Hemels, M.E.H. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef]
- Chattu, V.K.; Manzar, M.D.; Kumary, S.; Burman, D.; Spence, D.W.; Pandi-Perumal, S.R. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare 2019, 7, 1. [Google Scholar] [CrossRef]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; Van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef] [PubMed]
- Jardim, T.V.; Mozaffarian, D.; Abrahams-Gessel, S.; Sy, S.; Lee, Y.; Liu, J.; Huang, Y.; Rehm, C.; Wilde, P.; Micha, R.; et al. Cardiometabolic disease costs associated with suboptimal diet in the United States: A cost analysis based on a microsimulation model. PLoS Med. 2019, 16, e1002981. [Google Scholar] [CrossRef] [PubMed]
- Hillman, D.; Mitchell, S.; Streatfeild, J.; Burns, C.; Bruck, D.; Pezzullo, L. The economic cost of inadequate sleep. Sleep 2018, 41, zsy083. [Google Scholar] [CrossRef]
- Research, S. Wearable Fitness Trackers Market Size, Share & Trends; Analysis Report by Product Type (Smartwatches, Fitness Bands, Smart Clothing, Others), by Applications (Heart Rate Tracking, Stress Management, Glucose Monitoring, Running Tracking, Cycling Tracking, Others), by Distribution Channel (Online, Offline) and by Region(North America, Europe, APAC, Middle East and Africa, LATAM) Forecasts, 2025–2033; Report No.: SRHI1798DR; Straits Research: Maharashtra, India, 2024. [Google Scholar]
- Pureprofile. PRESS RELEASE: Wearables Work—Australians More Active with Fitness Trackers. 2015. Available online: https://business.pureprofile.com/press-release-wearables-work-australians-more-active-with-fitness-trackers/ (accessed on 13 May 2025).
- M+C Saatchi Performance. Tracking Wearable Tech Trends in the USA. M&C Saatchi Performance. 2021. Available online: https://www.mcsaatchiperformance.com/news/tracking-wearable-tech-trends-in-the-usa/ (accessed on 13 May 2025).
- Beckett, D.; Curtis, R.; Szeto, K.; Maher, C. Changing User Experience of Wearable Activity Monitors Over 7 Years: Repeat Cross-Sectional Survey Study. J. Med. Internet Res. 2025, 27, e56251. [Google Scholar] [CrossRef]
- del Rosario, M.B.; Redmond, S.J.; Lovell, N.H. Tracking the Evolution of Smartphone Sensing for Monitoring Human Movement. Sensors 2015, 15, 18901–18933. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, T.; Olds, T.; Curtis, R.; Blake, H.; Crozier, A.J.; Dankiw, K.; Dumuid, D.; Kasai, D.; O’Connor, E.; Virgara, R.; et al. Effectiveness of wearable activity trackers to increase physical activity and improve health: A systematic review of systematic reviews and meta-analyses. Lancet Digit. Health 2022, 4, e615-26. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.Y.C.; Mong, M.S.A.; Cheng, L.J.; Lau, Y. The effect of wearable-delivered sleep interventions on sleep outcomes among adults: A systematic review and meta-analysis of randomized controlled trials. Nurs. Health Sci. 2023, 25, 44–62. [Google Scholar] [CrossRef] [PubMed]
- Lobelo, F.; Rohm Young, D.; Sallis, R.; Garber, M.D.; Billinger, S.A.; Duperly, J.; Hutber, A.; Pate, R.R.; Thomas, R.J.; Widlansky, M.E.; et al. Routine Assessment and Promotion of Physical Activity in Healthcare Settings: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e495–e522. [Google Scholar] [CrossRef]
- Nyberd, S.T.; Singh-Manoux, A.; Pentti, J.; Madsen, I.E.; Sabia, S.; Alfedsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Goldberg, M.; et al. Association of healthy lifestyle with years lived without major chronic diseases. JAMA Intern. Med. 2020, 180, 760–768. [Google Scholar] [CrossRef]
- Ma, J.K.; McCracken, L.A.; Voss, C.; Chan, F.H.; West, C.R.; Martin Ginis, K.A. Physical activity measurement in people with spinal cord injury: Comparison of accelerometry and self-report (the Physical Activity Recall Assessment for People with Spinal Cord Injury). Disabil. Rehabil. 2020, 42, 240–246. [Google Scholar] [CrossRef]
- Lawrence, G.; Muza, R. Assessing the sleeping habits of patients in a sleep disorder centre: A review of sleep diary accuracy. J. Thorac. Dis. 2018, 10 (Suppl. 1), S177–S183. [Google Scholar] [CrossRef]
- Olds, T.S.; Gommersall, S.R.; Olds, S.T.; Ridley, K. A source of systematic bias in self-reported physical activity: The cutpoint bias hypothesis. J. Sci. Med. Sport 2019, 22, 924–928. [Google Scholar] [CrossRef]
- Natalucci, V.; Marmondi, F.; Biraghi, M.; Bonato, M. The Effectiveness of Wearable Devices in Non-Communicable Diseases to Manage Physical Activity and Nutrition: Where We Are? Nutrients 2023, 15, 913. [Google Scholar] [CrossRef]
- Greiwe, J.; Nyenhuis, S.M. Wearable Technology and How This Can Be Implemented into Clinical Practice. Curr. Allergy Asthma Rep. 2020, 20, 36. [Google Scholar] [CrossRef]
- Franssen, W.M.; Franssen, G.H.; Spaas, J.; Solmi, F.; Eijnde, B.O. Can consumer wearable activity tracker-based interventions improve physical activity and cardiometabolic health in patients with chronic diseases? A systematic review and meta-analysis of randomised controlled trials. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 57. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.K.; Sankar, P.; Wilson, M.D.; Haynes, S.C. Factors affecting willingness to share electronic health data among California consumers. BMC Med. Ethics 2017, 18, 25. [Google Scholar] [CrossRef] [PubMed]
- Kalkman, S.; van Delden, J.; Banerjee, A.; Tyl, B.; Mostert, M.; van Thiel, G. Patients’ and public views and attitudes towards the sharing of health data for research: A narrative review of the empirical evidence. J. Med. Ethics 2022, 48, 3. [Google Scholar] [CrossRef] [PubMed]
- Varhol, R.J.; Norman, R.; Randall, S.; Man Ying Lee, C.; Trevenen, L.; Boyd, J.H.; Robinson, S. Public preference on sharing health data to inform research, health policy and clinical practice in Australia: A stated preference experiment. PLoS ONE 2023, 18, e0290528. [Google Scholar] [CrossRef]
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.A.; Puleo, V.; De Maio, L.; Ricciardi, W. Health data sharing attitudes towards primary and secondary use of data: A systematic review. eClinicalMedicine 2024, 71, 102551. [Google Scholar] [CrossRef]
- Serrano, K.J.; Yu, M.; Riley, W.T.; Patel, V.; Hughes, P.; Marchesini, K.; Atienza, A.A. Willingness to Exchange Health Information via Mobile Devices: Findings From a Population-Based Survey. Ann. Fam. Med. 2016, 14, 34–40. [Google Scholar] [CrossRef]
- Rising, C.J.; Gaysynsky, A.; Blake, K.D.; Jensen, R.E.; Oh, A. Willingness to Share Data From Wearable Health and Activity Trackers: Analysis of the 2019 Health Information National Trends Survey Data. JMIR Mhealth Uhealth 2021, 9, e29190. [Google Scholar] [CrossRef]
- Shin, G.D.; Feng, Y.; Gafinowitz, N.; Jarrahi, M.H. Improving patient engagement by fostering the sharing of activity tracker data with providers: A qualitative study. Health Inf. Libr. J. 2020, 37, 204–215. [Google Scholar] [CrossRef]
- Maher, C.; Ryan, J.; Ambrosi, C.; Edney, S. Users’ experiences of wearable activity trackers: A cross-sectional study. BMC Public Health 2017, 17, 880. [Google Scholar] [CrossRef]
- Keogh, A.; Taraldsen, K.; Caulfield, B.; Vereijken, B. It’s not about the capture, it’s about what we can learn”: A qualitative study of experts’ opinions and experiences regarding the use of wearable sensors to measure gait and physical activity. J. Neuroeng. Rehabil. 2021, 18, 78. [Google Scholar] [CrossRef]
- Smuck, M.; Odonkor, C.A.; Wilt, J.K.; Schmidt, N.; Swiemik, M.A. The emerging role of wearables: Factors for successful implementation inhealthcare. MPJ Digit. Med. 2021, 4, 45. [Google Scholar]
- Shin, G.; Jarrahi, M.H.; Fei, Y.; Karami, A.; Gafinowitz, N.; Byun, A.; Lu, X. Wearable activity trackers, accuracy, adoption, acceptance and health impact: A systematic literature review. J. Biomed. Inform. 2019, 93, 103153. [Google Scholar] [CrossRef] [PubMed]
- Van Oostrom, S.H.; Picavet, H.S.; De Bruin, S.R.; Stirbu, I.; Korevaar, J.C.; Schellevis, F.G.; Baan, C.A. Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam. Pract. 2014, 15, 61. [Google Scholar] [CrossRef] [PubMed]
- Glynn, L.G.; Valderas, J.M.; Healy, P.; Burke, E.; Newell, J.; Gillespie, P.; Murphy, A.W. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam. Pract. 2011, 28, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, C.; Johnson, L.; Purdy, S.; Valderas, J.M.; Montgomery, A.A. Epidemiology and impact of multimorbidity in primary care: A retrospective cohort study. Br. J. Gen. Pract. 2011, 61, e12. [Google Scholar] [CrossRef]
- Folkes, V.S. The availability heuristic and perceived risk. J. Consum. Res. 1988, 15, 13–23. [Google Scholar] [CrossRef]
- Treacy, D.; Hassett, L.; Schurr, K.; Chagpar, S.; Paul, S.S.; Sherrington, C. Validity of different activity monitors to count steps in an inpatient rehabilitation setting. Phys. Ther. 2017, 97, 581–588. [Google Scholar] [CrossRef]

| n | (%) | ||
|---|---|---|---|
| Gender | Female | 268 | (60.0) |
| Male | 178 | (39.8) | |
| Non-binary/third gender | 1 | (0.2) | |
| Age (in years) | 18–24 | 66 | (14.8) |
| 25–34 | 204 | (45.6) | |
| 35–44 | 105 | (23.5) | |
| 45–54 | 54 | (12.1) | |
| ≥55 | 18 | (4) | |
| Country | United States of America | 268 | (60.0) |
| Australia | 122 | (27.3) | |
| Other | 57 | (12.7) | |
| Education | Secondary school or below | 117 | (26.1) |
| Vocational qualification (i.e., certificate or diploma) | 46 | (10.3) | |
| University bachelor’s degree | 213 | (47.7) | |
| Post graduate degree (e.g., Master’s degree, PhD) | 71 | (15.9) | |
| Self-rated health | Excellent | 80 | (17.9) |
| Very good | 190 | (42.5) | |
| Good | 143 | (32.0) | |
| Fair | 30 | (6.7) | |
| Poor | 4 | (0.9) | |
| Chronic conditions | None | 149 | (33.3%) |
| 1 | 171 | (38.3%) | |
| 2 or more | 127 | (28.4%) |
| n | (%) | ||
|---|---|---|---|
| User status | Current | 359 | (80.3) |
| Former | 88 | (19.7) | |
| Wearable brand | Apple | 199 | (44.5) |
| Fitbit | 87 | (19.5) | |
| Garmin | 89 | (19.9) | |
| Samsung | 46 | (10.3) | |
| Other | 26 | (5.8) | |
| Duration of use | ≤6 months | 92 | (20.6) |
| >6–12 months | 106 | (23.7) | |
| >1–2 years | 103 | (23.0) | |
| 3–5 years | 85 | (19.0) | |
| ≥6 years | 39 | (6.5) | |
| Not reported | 22 | (7.2) | |
| Frequency of use (% of current users, n = 359) | Every day including overnight | 90 | (25) |
| Every day during waking hours | 148 | (41.2) | |
| Once a week | 69 | (19.2) | |
| When I remember | 27 | (8) | |
| Other | 5 | (1.4) | |
| Not reported | 20 | (3.6) | |
| Perceived change in physical activity since using wearable | Increased and maintained | 130 | (29.1) |
| Constantly increased activity | 165 | (36.9) | |
| No change | 81 | (18.1) | |
| Increased but unable to maintain | 43 | (9.6) | |
| Other | 6 | (1.3) | |
| Not reported | 22 | (4.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szeto, K.; Maher, C.; Curtis, R.G.; Singh, B.; Cain, T.; Beckett, D.; Ferguson, T. User Experiences and Attitudes Toward Sharing Wearable Activity Tracker Data with Healthcare Providers: A Cross-Sectional Study. Healthcare 2025, 13, 1215. https://doi.org/10.3390/healthcare13111215
Szeto K, Maher C, Curtis RG, Singh B, Cain T, Beckett D, Ferguson T. User Experiences and Attitudes Toward Sharing Wearable Activity Tracker Data with Healthcare Providers: A Cross-Sectional Study. Healthcare. 2025; 13(11):1215. https://doi.org/10.3390/healthcare13111215
Chicago/Turabian StyleSzeto, Kimberley, Carol Maher, Rachel G. Curtis, Ben Singh, Tara Cain, Darcy Beckett, and Ty Ferguson. 2025. "User Experiences and Attitudes Toward Sharing Wearable Activity Tracker Data with Healthcare Providers: A Cross-Sectional Study" Healthcare 13, no. 11: 1215. https://doi.org/10.3390/healthcare13111215
APA StyleSzeto, K., Maher, C., Curtis, R. G., Singh, B., Cain, T., Beckett, D., & Ferguson, T. (2025). User Experiences and Attitudes Toward Sharing Wearable Activity Tracker Data with Healthcare Providers: A Cross-Sectional Study. Healthcare, 13(11), 1215. https://doi.org/10.3390/healthcare13111215








