Pretransplant Physical Activity and Cardiovascular Risk Factors in Kidney Transplant Candidates: A Cross-Sectional Study
Abstract
1. Introduction
Background
2. Materials and Methods
2.1. Study Design and Participants
2.2. Variables and Data Collection
2.3. Data Analysis
2.4. Ethical Issues
3. Results
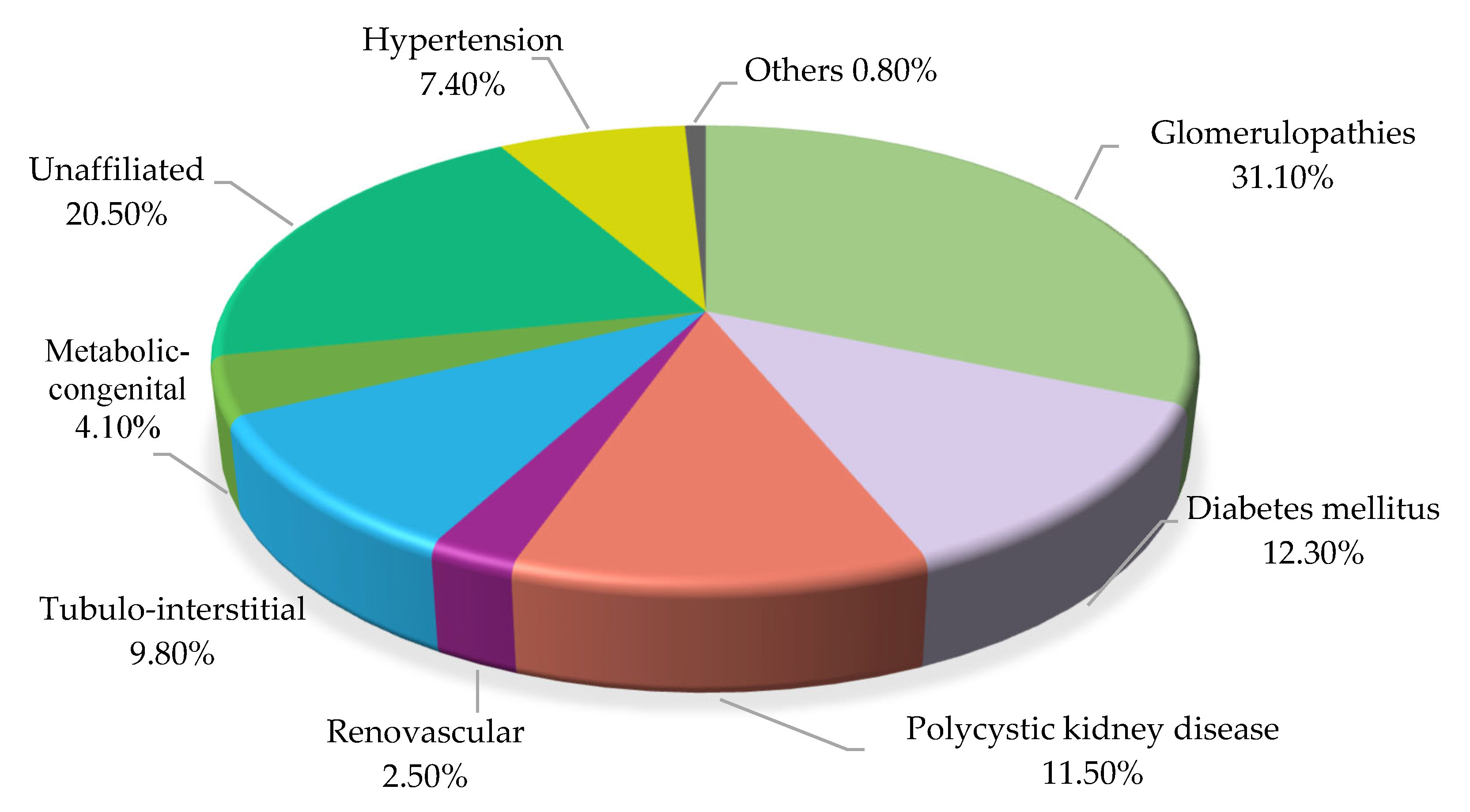
3.1. Descriptive Analysis
3.2. Inferential Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| CI | Confidence Interval |
| CKD | Chronic Kidney Disease |
| CPG | Clinical Practice Guideline |
| CVD | Cardiovascular Disease |
| HD | Hemodialysis |
| IPAQ | International PA Questionnaire |
| IQR | Interquartile Range |
| KDIGO | Kidney Disease Improving Global Outcomes |
| MET | Metabolic Equivalent Unit |
| PA | Physical Activity |
| PD | Peritoneal Dialysis |
| RRT | Renal Replacement Therapy |
| WHO | World Health Organization |
References
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024, 105, S117–S314. [Google Scholar] [CrossRef]
- García-Maset, R.; Bover, J.; Segura de la Morena, J.; Goicoechea Diezhandino, M.; Cebollada del Hoyo, J.; Escalada San Martín, J.; Fácila Rubio, L.; Gamarra Ortiz, J.; García-Donaire, J.A.; García-Matarín, L.; et al. Documento de Información y Consenso Para La Detección y Manejo de La Enfermedad Renal Crónica. Nefrología 2022, 42, 233–264. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.M.; Edwards, D.; Ahdoot, R.S.; Burton, J.O.; Conway, P.T.; Fishbane, S.; Gallego, D.; Gallieni, M.; Gedney, N.; Hayashida, G.; et al. Living Well With Kidney Disease and Effective Symptom Management: Consensus Conference Proceedings. Kidney Int. Rep. 2022, 7, 1951–1963. [Google Scholar] [CrossRef] [PubMed]
- Pommer, W. Preventive Nephrology: The Role of Obesity in Different Stages of Chronic Kidney Disease. Kidney Dis. 2018, 4, 199–204. [Google Scholar] [CrossRef]
- Zelle, D.M.; Klaassen, G.; van Adrichem, E.; Bakker, S.J.L.; Corpeleijn, E.; Navis, G. Physical Inactivity: A Risk Factor and Target for Intervention in Renal Care. Nat. Rev. Nephrol. 2017, 13, 152–168. [Google Scholar] [CrossRef]
- Ibrahim, A.A.; Althomali, O.W.; Atyia, M.R.; Hussein, H.M.; Abdelbasset, W.K.; Eldesoky, M.T.M.; Gamal, M. A Systematic Review of Trials Investigating the Efficacy of Exercise Training for Functional Capacity and Quality of Life in Chronic Kidney Disease Patients. Int. Urol. Nephrol. 2022, 54, 289–298. [Google Scholar] [CrossRef]
- Muras-Szwedziak, K.; Masajtis-Zagajewska, A.; Pawłowicz, E.; Nowicki, M. Effects of a Structured Physical Activity Program on Serum Adipokines and Markers of Inflammation and Volume Overload in Kidney Transplant Recipients. Ann. Transplant. 2019, 24, 569–575. [Google Scholar] [CrossRef]
- Kanbay, M.; Copur, S.; Yildiz, A.B.; Tanriover, C.; Mallamaci, F.; Zoccali, C. Physical Exercise in Kidney Disease: A Commonly Undervalued Treatment Modality. Eur. J. Clin. Investig. 2024, 54, e14105. [Google Scholar] [CrossRef]
- Ponticelli, C.; Favi, E. Physical Inactivity: A Modifiable Risk Factor for Morbidity and Mortality in Kidney Transplantation. J. Pers. Med. 2021, 11, 927. [Google Scholar] [CrossRef]
- Chen, G.; Gao, L.; Li, X. Effects of Exercise Training on Cardiovascular Risk Factors in Kidney Transplant Recipients: A Systematic Review and Meta-Analysis. Ren. Fail. 2019, 41, 408–418. [Google Scholar] [CrossRef]
- Rangaswami, J.; Mathew, R.O.; Parasuraman, R.; Tantisattamo, E.; Lubetzky, M.; Rao, S.; Yaqub, M.S.; Birdwell, K.A.; Bennett, W.; Dalal, P.; et al. Cardiovascular Disease in the Kidney Transplant Recipient: Epidemiology, Diagnosis and Management Strategies. Nephrol. Dial. Transplant. 2019, 34, 760–773. [Google Scholar] [CrossRef] [PubMed]
- Schardong, J.; Marcolino, M.A.Z.; Plentz, R.D.M. Muscle Atrophy in Chronic Kidney Disease. Adv. Exp. Med. Biol. 2018, 1088, 393–412. [Google Scholar] [CrossRef]
- Neuberger, J.; Armstrong, M.J.; Fisher, J.; Mark, P.; Schmidtke, K.; Sharif, A.; Vlaev, I. Sport and Exercise in Improving Outcomes After Solid Organ Transplantation: Overview From a UK Meeting. Transplantation 2019, 103, S1–S11. [Google Scholar] [CrossRef]
- Calella, P.; Hernández-Sánchez, S.; Garofalo, C.; Ruiz, J.R.; Carrero, J.J.; Bellizzi, V. Exercise Training in Kidney Transplant Recipients: A Systematic Review. J. Nephrol. 2019, 32, 567–579. [Google Scholar] [CrossRef]
- Lima, P.S.; Campos, A.S.D.; Corrêa, C.S.; Dias, C.J.M.; Mostarda, C.T.; Amorim, C.E.N.; Garcia, A.M.C. Effects of Chronic Physical Activity on Glomerular Filtration Rate, Creatinine, and the Markers of Anemia of Kidney Transplantation Patients. Transplant. Proc. 2018, 50, 746–749. [Google Scholar] [CrossRef]
- Deligiannis, A.; D’Alessandro, C.; Cupisti, A. Exercise Training in Dialysis Patients: Impact on Cardiovascular and Skeletal Muscle Health. Clin. Kidney J. 2021, 14, ii25–ii33. [Google Scholar] [CrossRef]
- Broers, N.J.H.; Martens, R.J.H.; Cornelis, T.; Van Der Sande, F.M.; Diederen, N.M.P.; Hermans, M.M.H.; Wirtz, J.J.J.M.; Stifft, F.; Konings, C.J.A.M.; Dejagere, T.; et al. Physical Activity in End-Stage Renal Disease Patients: The Effects of Starting Dialysis in the First 6 Months after the Transition Period. Nephron 2017, 137, 47–56. [Google Scholar] [CrossRef]
- Cheng, X.S.; Myers, J.N.; Chertow, G.M.; Rabkin, R.; Chan, K.N.; Chen, Y.; Tan, J.C. Prehabilitation for Kidney Transplant Candidates: Is It Time? Clin. Transplant. 2017, 31, e13020. [Google Scholar] [CrossRef]
- Ma, X.; Zhang, Z.; Peng, M.; Yao, B.; Jiang, H.; Ji, X.; You, Y. Face-to-Face Mentoring, Remotely Supervised Home Exercise Prehabilitation to Improve Physical Function in Patients Awaiting Kidney Transplantation: A Randomized Clinical Trial. Front. Psychol. 2022, 13, 831445. [Google Scholar] [CrossRef]
- O’Brien, T.; Meyer, T. A Feasibility Study for Teaching Older Kidney Transplant Recipients How to Wear and Use an Activity Tracker to Promote Daily Physical Activity. Nephrol. Nurs. J. 2020, 47, 47. [Google Scholar] [CrossRef]
- Masiero, L.; Puoti, F.; Bellis, L.; Lombardini, L.; Totti, V.; Angelini, M.L.; Spazzoli, A.; Nanni Costa, A.; Cardillo, M.; Sella, G.; et al. Physical Activity and Renal Function in the Italian Kidney Transplant Population. Ren. Fail. 2020, 42, 1192–1204. [Google Scholar] [CrossRef] [PubMed]
- Tlatoa Ramírez, H.M.; López López, J.C.; Luna Blas, H.G.; Aguilar Becerril, J.A.; Ocaña Servín, H.L. Proteinuria inducida por ejercicio físico. Med. Investig. 2014, 2, 141–145. [Google Scholar] [CrossRef]
- Ricardo, A.C.; Anderson, C.A.; Yang, W.; Zhang, X.; Fischer, M.J.; Dember, L.M.; Fink, J.C.; Frydrych, A.; Jensvold, N.G.; Lustigova, E.; et al. Healthy Lifestyle and Risk of Kidney Disease Progression, Atherosclerotic Events, and Death in CKD: Findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am. J. Kidney Dis. 2015, 65, 412–424. [Google Scholar] [CrossRef]
- Kang, A.W.; Garber, C.E.; Eaton, C.B.; Risica, P.M.; Bostom, A.G. Physical Activity and Cardiovascular Risk among Kidney Transplant Patients. Med. Sci. Sports Exerc. 2019, 51, 1154–1161. [Google Scholar] [CrossRef]
- Yanishi, M.; Tsukaguchi, H.; Kimura, Y.; Koito, Y.; Yoshida, K.; Seo, M.; Jino, E.; Sugi, M.; Kinoshita, H.; Matsuda, T. Evaluation of Physical Activity in Sarcopenic Conditions of Kidney Transplantation Recipients. Int. Urol. Nephrol. 2017, 49, 1779–1784. [Google Scholar] [CrossRef]
- Yang, Q.; Yang, W.; Liu, F. The Associations of Weekend Warrior and Other Physical Activity Patterns with the Risk of All-Cause and Cardiovascular Disease Mortality in People with Diabetes Mellitus and Chronic Kidney Disease: From NHANES 2007–2020. Int. Urol. Nephrol. 2023, 56, 1703–1712. [Google Scholar] [CrossRef]
- Carmines, E.; Zeller, R. Reliability and Validity Assessment; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 1979; ISBN 978-0-8039-1371-4. [Google Scholar]
- Painter, P.; Kuskowski, M. A Closer Look at Frailty in ESRD: Getting the Measure Right. Hemodial. Int. 2013, 17, 41–49. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health; WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization: Geneva, Switzerland, 2010; ISBN 978-92-4-159997-9. [Google Scholar]
- Baker, L.A.; March, D.S.; Wilkinson, T.J.; Billany, R.E.; Bishop, N.C.; Castle, E.M.; Chilcot, J.; Davies, M.D.; Graham-Brown, M.P.M.; Greenwood, S.A.; et al. Clinical Practice Guideline Exercise and Lifestyle in Chronic Kidney Disease. BMC Nephrol. 2022, 23, 75. [Google Scholar] [CrossRef]
- González, A.; Diz, J.C.; García, Ó.; Carbajales, D.; Diz-Ferreira, E.; Ayán Pérez, C. Eficacia del ejercicio intradialítico semisupervisado en la capacidad funcional de los pacientes: Un estudio exploratorio. Nefrología 2023, 43, 796–798. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour, 1st ed.; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-001512-8. [Google Scholar]
- Vejby, S.; Eriksson, A.; Nordin, K.; Johansson, B. Is It Possible to Increase the Amount of Physical Activity in Patients Isolated Due to Hematopoietic Stem Cell Transplantation Using a Nursing Intervention? A Feasibility Study. Nord. J. Nurs. Res. 2021, 42, 18–27. [Google Scholar] [CrossRef]
- Tan, S.; Thang, Y.W.; Mulley, W.R.; Polkinghorne, K.R.; Ramkumar, S.; Cheng, K.; Chan, J.; Galligan, J.; Nolan, M.; Brown, A.J.; et al. Prognostic Value of Exercise Capacity in Kidney Transplant Candidates. J. Am. Heart Assoc. 2022, 11, e025862. [Google Scholar] [CrossRef]
- Sim, J.A.P.; Perinpanayagam, M.A.; Bahry, V.; Wytsma-Fisher, K.; Burak, K.W.; Isaac, D.L.; Mustata, S.; Culos-Reed, S.N. An Exercise and Wellness Behavior Change Program for Solid Organ Transplant: A Clinical Research Protocol for the Transplant Wellness Program. Can. J. Kidney Health Dis. 2024, 11, 20543581241289196. [Google Scholar] [CrossRef] [PubMed]
- Janaudis-Ferreira, T.; Tansey, C.M.; Mathur, S.; Blydt-Hansen, T.; Lamoureaux, J.; Räkel, A.; De Sousa Maia, N.P.; Bussières, A.; Ahmed, S.; Boruff, J. The Effects of Exercise Training in Adult Solid Organ Transplant Recipients: A Systematic Review and Meta-analysis. Transpl. Int. 2021, 34, 801–824. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Román Viñas, B.; Ribas Barba, L.; Ngo, J.; Serra Majem, L. Validación En Población Catalana Del Cuestionario Internacional de Actividad Física. Gac. Sanit. 2013, 27, 254–257. [Google Scholar] [CrossRef]
- Rubio Castañeda, F.J.; Tomás Aznar, C.; Muro Baquero, C.M. Medición De La Actividad Física En Personas Mayores De 65 Años Mediante El Ipaq-E: Validez De Contenido, Fiabilidad Y Factores Asociados. Rev. Española Salud Pública 2017, 91, 1–12. [Google Scholar]
- Ravussin, E.; Bogardus, C. Relationship of Genetics, Age, and Physical Fitness to Daily Energy Expenditure and Fuel Utilization. Am. J. Clin. Nutr. 1989, 49, 968–975. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Wilk, P.; Clark, A.F.; Maltby, A.; Smith, C.; Tucker, P.; Gilliland, J.A. Examining Individual, Interpersonal, and Environmental Influences on Children’s Physical Activity Levels. SSM—Popul. Health 2018, 4, 76–85. [Google Scholar] [CrossRef]
- Lue, H. An Inverse-regression Method of Dependent Variable Transformation for Dimension Reduction with Non-linear Confounding. Scand. J. Stat. 2015, 42, 760–774. [Google Scholar] [CrossRef]
- Pedreira-Robles, G.; Garcimartín, P.; Pérez-Sáez, M.J.; Bach-Pascual, A.; Crespo, M.; Morín-Fraile, V. Complex Management and Descriptive Cost Analysis of Kidney Transplant Candidates: A Descriptive Cross-Sectional Study. BMC Health Serv. Res. 2024, 24, 763. [Google Scholar] [CrossRef]
- Melk, A.; Babitsch, B.; Borchert-Mörlins, B.; Claas, F.; Dipchand, A.I.; Eifert, S.; Eiz-Vesper, B.; Epping, J.; Falk, C.S.; Foster, B.; et al. Equally Interchangeable? How Sex and Gender Affect Transplantation. Transplantation 2019, 103, 1094–1110. [Google Scholar] [CrossRef]
- Gorostidi, M.; Sánchez-Martínez, M.; Ruilope, L.M.; Graciani, A.; de la Cruz, J.J.; Santamaría, R.; del Pino, M.D.; Guallar-Castillón, P.; de Álvaro, F.; Rodríguez-Artalejo, F.; et al. Prevalencia de enfermedad renal crónica en España: Impacto de la acumulación de factores de riesgo cardiovascular. Nefrología 2018, 38, 606–615. [Google Scholar] [CrossRef]
- Ricardo, A.C.; Yang, W.; Sha, D.; Appel, L.J.; Chen, J.; Krousel-Wood, M.; Manoharan, A.; Steigerwalt, S.; Wright, J.; Rahman, M.; et al. Sex-Related Disparities in CKD Progression. J. Am. Soc. Nephrol. 2019, 30, 137–146. [Google Scholar] [CrossRef]
- Carrero, J.J.; Hecking, M.; Chesnaye, N.C.; Jager, K.J. Sex and Gender Disparities in the Epidemiology and Outcomes of Chronic Kidney Disease. Nat. Rev. Nephrol. 2018, 14, 151–164. [Google Scholar] [CrossRef]
- Kurnikowski, A.; Krenn, S.; Lewandowski, M.J.; Schwaiger, E.; Tong, A.; Jager, K.J.; Carrero, J.J.; Hecking, M.; Hödlmoser, S. Country-Specific Sex Disparities in Living Kidney Donation. Nephrol. Dial. Transplant. 2022, 37, 595–598. [Google Scholar] [CrossRef]
- Hecking, M.; Tu, C.; Zee, J.; Bieber, B.; Hödlmoser, S.; Reichel, H.; Sesso, R.; Port, F.K.; Robinson, B.M.; Carrero, J.J.; et al. Sex-Specific Differences in Mortality and Incident Dialysis in the Chronic Kidney Disease Outcomes and Practice Patterns Study. Kidney Int. Rep. 2021, 7, 410–423. [Google Scholar] [CrossRef]
- Brar, A.; Markell, M. Impact of Gender and Gender Disparities in Patients with Kidney Disease. Curr. Opin. Nephrol. Hypertens. 2019, 28, 178–182. [Google Scholar] [CrossRef]
- Katz-Greenberg, G.; Shah, S. Sex and Gender Differences in Kidney Transplantation. Semin. Nephrol. 2022, 42, 219–229. [Google Scholar] [CrossRef]
- Estupiñán-Bohórquez, A.; Acosta-Reyes, J.; Viasus-Pérez, D.; García-López, A.; Patino-Jaramillo, N.; Girón-Luque, F. Trasplante Renal de Donantes Con Criterios Expandidos En La Región Caribe Colombiana. Rev. Nefrol. Latinoam. 2021, 18, 119–127. [Google Scholar] [CrossRef]
- Arcos, E.; Pérez-Sáez, M.J.; Comas, J.; Lloveras, J.; Tort, J.; Pascual, J. Assessing the Limits in Kidney Transplantation: Use of Extremely Elderly Donors and Outcomes in Elderly Recipients. Transplantation 2020, 104, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Arias-Cabrales, C.; Pérez-Sáez, M.J.; Redondo-Pachón, D.; Buxeda, A.; Burballa, C.; Bermejo, S.; Sierra, A.; Mir, M.; Burón, A.; Zapatero, A.; et al. Usefulness of the KDPI in Spain: A Comparison with Donor Age and Definition of Standard/Expanded Criteria Donor. Nefrología 2018, 38, 503–513. [Google Scholar] [CrossRef]
- Peters-Sengers, H.; Heemskerk, M.B.A.; Geskus, R.B.; Kers, J.; Homan van der Heide, J.J.; Berger, S.P.; Bemelman, F.J. Validation of the Prognostic Kidney Donor Risk Index Scoring System of Deceased Donors for Renal Transplantation in the Netherlands. Transplantation 2018, 102, 162–170. [Google Scholar] [CrossRef]
- Lehner, L.J.; Kleinsteuber, A.; Halleck, F.; Khadzhynov, D.; Schrezenmeier, E.; Duerr, M.; Eckardt, K.-U.; Budde, K.; Staeck, O. Assessment of the Kidney Donor Profile Index in a European Cohort. Nephrol. Dial. Transplant. 2018, 33, 1465–1472. [Google Scholar] [CrossRef]
- Del Moral Martín, R.M.G.; Retamero Díaz, J.A.; Cava Molina, M.; Cobacho Tornel, B.M.; Bravo Soto, J.; Osuna Ortega, A.; O’Valle Ravassa, F. Validación del KDRI/KPDI para la selección de donantes renales con criterios expandidos. Nefrología 2018, 38, 297–303. [Google Scholar] [CrossRef]
- Rosas, S.E.; Reese, P.P.; Huan, Y.; Doria, C.; Cochetti, P.T.; Doyle, A. Pretransplant Physical Activity Predicts All-Cause Mortality in Kidney Transplant Recipients. Am. J. Nephrol. 2012, 35, 17–23. [Google Scholar] [CrossRef]
- Wilkinson, T.J.; Clarke, A.L.; Nixon, D.G.D.; Hull, K.L.; Song, Y.; Burton, J.O.; Yates, T.; Smith, A.C. Prevalence and Correlates of Physical Activity across Kidney Disease Stages: An Observational Multicentre Study. Nephrol. Dial. Transplant. 2021, 36, 641–649. [Google Scholar] [CrossRef]
- Taryana, A.A.; Krishnasamy, R.; Bohm, C.; Palmer, S.C.; Wiebe, N.; Boudville, N.; MacRae, J.; Coombes, J.S.; Hawley, C.; Isbel, N.; et al. Physical Activity for People with Chronic Kidney Disease: An International Survey of Nephrologist Practice Patterns and Research Priorities. BMJ Open 2019, 9, e032322. [Google Scholar] [CrossRef]
- Kutner, N.G.; Zhang, R.; Bowles, T.; Painter, P. Pretransplant Physical Functioning and Kidney Patients’ Risk for Posttransplantation Hospitalization/Death: Evidence from a National Cohort. Clin. J. Am. Soc. Nephrol. 2006, 1, 837–843. [Google Scholar] [CrossRef]
- Pedreira-Robles, G.; Garcimartín, P.; Sevilla-Guerra, S.; Bach-Pascual, A.; García-Martínez, M.; Morín-Fraile, V. Nurse-led Clinical Activity in Kidney Transplantation Care in Spain: A Cross-sectional Observational Study. J. Ren. Care 2024, 50, 168–175. [Google Scholar] [CrossRef]
- Bolívar, J.; Daponte, A.; Rodríguez, M.; Sánchez, J.J. The Influence of Individual, Social and Physical Environment Factors on Physical Activity in the Adult Population in Andalusia, Spain. Int. J. Environ. Res. Public Health 2010, 7, 60–77. [Google Scholar] [CrossRef]
- Kwakkel, G.; van Peppen, R.; Wagenaar, R.C.; Wood Dauphinee, S.; Richards, C.; Ashburn, A.; Miller, K.; Lincoln, N.; Partridge, C.; Wellwood, I.; et al. Effects of Augmented Exercise Therapy Time after Stroke: A Meta-Analysis. Stroke 2004, 35, 2529–2539. [Google Scholar] [CrossRef]
- Kaysen, G.A.; Larive, B.; Painter, P.; Craig, A.; Lindsay, R.M.; Rocco, M.V.; Daugirdas, J.T.; Schulman, G.; Chertow, G.M. FHN Trial Group Baseline Physical Performance, Health, and Functioning of Participants in the Frequent Hemodialysis Network (FHN) Trial. Am. J. Kidney Dis. 2011, 57, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Klobučar, K.; Vrbanac, Z.; Gotić, J.; Bojanić, K.; Bureš, T.; Brkljača Bottegaro, N. Changes in Biochemical Parameters in Horses during 40 Km and 80 Km Endurance Races. Acta Vet. 2019, 69, 73–87. [Google Scholar] [CrossRef]
- Raj, D.S.C.; Zager, P.; Shah, V.O.; Dominic, E.A.; Adeniyi, O.; Blandon, P.; Wolfe, R.; Ferrando, A. Protein Turnover and Amino Acid Transport Kinetics in End-Stage Renal Disease. Am. J. Physiol.-Endocrinol. Metab. 2004, 286, E136–E143. [Google Scholar] [CrossRef]
- Al-rawi, K.F.; Ali, H.H.; Guma, M.A.; Mohammed Aldahham, B.J.; Tuleab Alaaraji, S.F.; Al-Ani, O.; Ali, A.T. Relationship Between IL-2, IL-17 Concentrations, and Serum Creatinine Levels in Men with Chronic Kidney Diseases. Rep. Biochem. Mol. Biol. 2022, 10, 664–674. [Google Scholar] [CrossRef]
- Ferrando, A.A.; Wolfe, R.R.; Hirsch, K.R.; Church, D.D.; Kviatkovsky, S.A.; Roberts, M.D.; Stout, J.R.; Gonzalez, D.E.; Sowinski, R.J.; Kreider, R.B.; et al. International Society of Sports Nutrition Position Stand: Effects of Essential Amino Acid Supplementation on Exercise and Performance. J. Int. Soc. Sports Nutr. 2023, 20, 2263409. [Google Scholar] [CrossRef]
- Metges, C.C.; Lang, I.S.; Hennig, U.; Brüssow, K.-P.; Kanitz, E.; Tuchscherer, M.; Schneider, F.; Weitzel, J.M.; Steinhoff-Ooster, A.; Sauerwein, H.; et al. Intrauterine Growth Retarded Progeny of Pregnant Sows Fed High Protein:Low Carbohydrate Diet Is Related to Metabolic Energy Deficit. PLoS ONE 2012, 7, e31390. [Google Scholar] [CrossRef]
- Cheng, X.S.; Myers, J.; Han, J.; Stedman, M.R.; Watford, D.J.; Lee, J.; Discipulo, K.V.; Chan, K.N.; Chertow, G.M.; Tan, J.C. Physical Performance Testing in Kidney Transplant Candidates at the Top of the Waitlist. Am. J. Kidney Dis. 2020, 76, 815–825. [Google Scholar] [CrossRef]
- Yuguero-Ortiz, A.; Gomez, M.; Arias-Guillén, M.; Ojeda, R.; Fontseré, N.; Rodas, L.; Broseta, J.J.; Vera, M.; Hernandez-Sanchez, S.; Maduell, F. Eficacia y seguridad de un programa de ejercicio físico intradiálisis. Nefrología 2021, 41, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Villanego, F.; Naranjo, J.; Vigara, L.A.; Cazorla, J.M.; Montero, M.E.; García, T.; Torrado, J.; Mazuecos, A. Impacto del ejercicio físico en pacientes con enfermedad renal crónica: Revisión sistemática y metaanálisis. Nefrología 2020, 40, 237–252. [Google Scholar] [CrossRef]
- Aoike, D.T.; Baria, F.; Kamimura, M.A.; Ammirati, A.; Cuppari, L. Home-Based versus Center-Based Aerobic Exercise on Cardiopulmonary Performance, Physical Function, Quality of Life and Quality of Sleep of Overweight Patients with Chronic Kidney Disease. Clin. Exp. Nephrol. 2018, 22, 87–98. [Google Scholar] [CrossRef]
- Takahashi, A.; Hu, S.L.; Bostom, A. Physical Activity in Kidney Transplant Recipients: A Review. Am. J. Kidney Dis. 2018, 72, 433–443. [Google Scholar] [CrossRef]
- Tang, Q.; Yang, B.; Fan, F.; Li, P.; Yang, L.; Guo, Y. Effects of Individualized Exercise Program on Physical Function, Psychological Dimensions, and Health-Related Quality of Life in Patients with Chronic Kidney Disease: A Randomized Controlled Trial in China. Int. J. Nurs. Pract. 2017, 23, e12519. [Google Scholar] [CrossRef]
- Pinillos-Patiño, Y.; Herazo-Beltrán, Y.; Gil Cataño, J.; Ramos De Ávila, J. Actividad Física y Calidad de Vida En Personas Con Enfermedad Renal Crónica. Rev. Med. Chile 2019, 147, 153–160. [Google Scholar] [CrossRef]
- Reese, P.P.; Bloom, R.D.; Shults, J.; Thomasson, A.; Mussell, A.; Rosas, S.E.; Johansen, K.L.; Abt, P.; Levine, M.; Caplan, A.; et al. Functional Status and Survival after Kidney Transplantation. Transplantation 2014, 97, 189–195. [Google Scholar] [CrossRef]
- Molsted, S.; Bennett, P.N.; Wilund, K.; Bruun, K.; Pakpour, A.H.; Liljehult, J.M.; Brandi, L. Nurses’ and Medical Doctors’ Attitudes towards Exercise for People with Chronic Kidney Disease in Denmark. J. Ren. Care 2023, 49, 206–216. [Google Scholar] [CrossRef]
- Bates, A.; Letton, M.E.; Arnold, R.; Lambert, K. Barriers and Enablers to Exercise in Kidney Transplant Recipients: Systematic Review of Qualitative Studies. J. Ren. Care 2024, 50, 384–404. [Google Scholar] [CrossRef]
- Antoun, J.; Brown, D.J.; Clarkson, B.G.; Shepherd, A.I.; Sangala, N.C.; Lewis, R.J.; McNarry, M.A.; Mackintosh, K.A.; Corbett, J.; Saynor, Z.L. Experiences of Adults Living with a Kidney Transplant—Effects on Physical Activity, Physical Function, and Quality of Life: A Descriptive Phenomenological Study. J. Ren. Care 2023, 49, 198–205. [Google Scholar] [CrossRef]
| Category | Characteristics |
|---|---|
| Low Category 1 (<600 METs) | No PA. Insufficient PA to reach categories 2 (Moderate) or 3 (High). |
| Moderate Category 2 (600–1499 METs) | Moderate PA and/or walking on five or more days for at least 30 min each day OR Combination of walking and/or moderate to vigorous PA, achieving an energy expenditure of at least 600 METs per minute and per week on five or more days OR Vigorous PA on three or more days for at least 25 min each day. |
| High Category 3 (>1500 METs) | Combination of walking and/or moderate to vigorous PA on seven or more days per week, achieving an energy expenditure of at least 3000 METs per minute and per week ORVigorous PA on at least three days per week, achieving an energy expenditure of 1500 METs per minute and per week. |
| Variable | Category | n (%) | Men | Women | p |
|---|---|---|---|---|---|
| 122 (100%) | 86 (70.5%) | 36 (29.5%) | |||
| Age (categorized) | 18–64 | 83 (68.0%) | 59 (48.4%) | 24 (19.7%) | 0.682 |
| ≥65 | 39 (32.0%) | 27 (22.1%) | 12 (9.8%) | 0.221 | |
| Renal replacement therapy | Nondialysis | 9 (7.4%) | 6 (4.9%) | 3 (2.5%) | 0.622 |
| Peritoneal dialysis | 31 (25.4%) | 24 (19.7%) | 7 (5.7%) | ||
| Hemodialysis | 82 (67.2%) | 56 (45.9%) | 26 (21.3%) | ||
| Vascular access | No vascular access | 40 (32.8%) | 30 (24.6%) | 10 (8.2%) | 0.205 + |
| Arteriovenous fistula | 55 (45.1%) | 40 (32.8%) | 15 (12.3%) | ||
| Catheter | 27 (22.1%) | 16 (13.1%) | 11 (9.0%) | ||
| Previous transplant | Non-previous transplant | 104 (85.2%) | 74 (60.7%) | 30 (24.6%) | 0.781 + |
| Previous transplant | 18 (14.8%) | 12 (9.8%) | 6 (4.9%) | ||
| BMI | Underweight | 6 (4.9%) | 2 (1.6%) | 4 (3.3%) | 0.013 + |
| Normal weight | 54 (44.3%) | 34 (27.9%) | 20 (16.4%) | ||
| Overweight | 42 (34.4%) | 36 (29.5%) | 6 (4.9%) | ||
| Obesity | 20 (16.4%) | 14 (11.5%) | 6 (4.9%) | ||
| Patients with hypertension | 112 (91.8%) | 86 (64.8%) | 36 (27.0%) | 0.972 | |
| Patients with previous diabetes | 24 (19.7%) | 17 (13.9%) | 7 (5.7%) | 0.967 | |
| Patients with dyslipidemia | 62 (50.8%) | 44 (71.0%) | 18 (29%) | 0.907 | |
| Patients with ischemic heart disease | 33 (27.0%) | 23 (18.9%) | 36 (8.2%) | 0.907 | |
| Patients with respiratory disease | 18 (14.8%) | 16 (13.1%) | 2 (1.6%) | 0.064 | |
| Patients with cerebrovascular accident | 6 (4.9%) | 4 (3.3%) | 2 (1.6%) | 0.574 + | |
| Patients with toxic habits | 22 (18.2%) | 16 (13.2%) | 6 (5.0%) | 0.850 | |
| Median (IRQ) | Men | Women | |||
| Waiting list time in days | 423 (405) | 381 (471) | 253 (499) | 0.227 | |
| Mean (SD) | Men | Women | p | |
|---|---|---|---|---|
| Ferritin (15–200 ng/mL) | 384.85 (458.62) | 384.85 (471.42) | 384.85 (417.12) | 0.650 |
| Creatinine (0.51–0.95 mg/dL) | 6.08 (3.03) | 6.27 (3.90) | 5.33 (2.95) | 0.010 |
| Urea (17–43 mg/dL) | 106.50 (80.0) | 110 (81.50) | 102 (75.75) | 0.148 |
| Protein (6.6–8.3 g/dL) | 6.65 (0.83) | 6.7 (0.90) | 6.6 (0.80) | 0.331 |
| Albumin (3.5–5.2 g/dL) | 4 (0.52) | 4 (0.60) | 3.90 (0.58) | 0.168 |
| Hemoglobin (g/dL) | 12.17 (1.38) | 12.10 (1.82) | 11.70 (2.10) | 0.415 |
| Hematocrit (%) | 35.80 (4.92) | 36 (4.80) | 35.60 (18.20) | 0.678 |
| Glycated hemoglobin (HbA1c) | 5.30 (0.70) | 5.30 (0.70) | 5.30 (0.78) | 0.280 |
| Total | High PA | Moderate PA | Low PA | |
|---|---|---|---|---|
| n (%) | 122 (100%) | 65 (53.3%) | 38 (31.1%) | 19 (15.6%) |
| MET-min/week | 1742 (1719) | 2772 (2240) | 1386 (346.13) | 393 (306) |
| Variable | Category | n (%) | Median (IQR) | p |
|---|---|---|---|---|
| Sex | Men | 86 (70.5%) | 2076 (2037) | 0.062 U |
| Women | 36 (29.5%) | 1386 (1238) | ||
| Age | 18–64 | 83 (68%) | 1746 (1557) | 0.925 U |
| ≥65 | 39 (32%) | 1533 (2340) | ||
| Renal replacement therapy | No dialysis | 9 (7.4%) | 2619 (1386) | 0.574 + |
| Peritoneal dialysis | 31 (25.4%) | 1626 (1601) | ||
| Hemodialysis | 82 (67.2%) | 1739 (1922) | ||
| Vascular access | No vascular access | 40 (32.8%) | 1741 (1575) | 0.912 + |
| Arteriovenous fistula | 55 (45.1%) | 1848 (1879) | ||
| Catheter | 27 (22.1%) | 1466 (2538) | ||
| BMI | Underweight | 6 (4.9%) | 1213 (1869) | 0.232 + |
| Normal weight | 54 (44.3%) | 1562 (1732) | ||
| Overweight | 42 (34.4%) | 2016 (2666) | ||
| Obesity (BMI ≥ 30) | 20 (16.4%) | 1426 (1439) | ||
| Previous transplant | Yes | 104 (85.2%) | 1913 (2027) | 0.483 U |
| No | 18 (14.8%) | 1735 (1646) | ||
| Hypertension | No | 10 (8.2%) | 2086 (3878) | 0.940 U |
| Yes | 112 (91.8%) | 1742 (1559) | ||
| Previous diabetes | No | 98 (80.3%) | 1762 (1719) | 0.799 U |
| Yes | 24 (19.7%) | 1506 (1520) | ||
| Dyslipidemia | No | 60 (49.2%) | 1764 (1784) | 0.501 U |
| Yes | 62 (50.8%) | 1682 (1704) | ||
| Ischemic heart disease | No | 89 (73%) | 1782 (1550) | 0.611 U |
| Yes | 33 (27%) | 1386 (2754) | ||
| Respiratory disease | No | 104 (85.2%) | 1746 (1796) | 0.831 U |
| Yes | 18 (14.8%) | 1426 (1213) | ||
| Cerebrovascular accident | No | 116 (95.1%) | 1633 (1646) | 0.035 U |
| Yes | 6 (4.9%) | 3462 (3533) | ||
| Toxic habits | No | 100 (81.8%) | 1737 (1606) | 0.903 U |
| Yes | 22 (18.2%) | 2079 (2274) |
| Variable | Correlation Value | p |
|---|---|---|
| Age | 0.008 | 0.927 |
| BMI | 0.122 | 0.182 |
| Waiting list time | −0.018 | 0.846 |
| Ferritin | −0.020 | 0.824 |
| Creatinine | 0.081 | 0.376 |
| Urea | 0.204 | 0.024 |
| Protein | 0.106 | 0.246 |
| Albumin | 0.009 | 0.921 |
| Hemoglobin | 0.081 | 0.377 |
| Hematocrit | 0.101 | 0.267 |
| Glycated hemoglobin | 0.099 | 0.280 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrer-López, E.; Cantín-Lahoz, V.; Rubio-Castañeda, F.J.; Aguilón-Leiva, J.J.; García-Magán, M.; Navas-Ferrer, C.; Benito-Ruiz, E.; Serrano-Vicente, M.I.; Blázquez-Ornat, I.; Antón-Solanas, I.; et al. Pretransplant Physical Activity and Cardiovascular Risk Factors in Kidney Transplant Candidates: A Cross-Sectional Study. Healthcare 2025, 13, 1200. https://doi.org/10.3390/healthcare13101200
Ferrer-López E, Cantín-Lahoz V, Rubio-Castañeda FJ, Aguilón-Leiva JJ, García-Magán M, Navas-Ferrer C, Benito-Ruiz E, Serrano-Vicente MI, Blázquez-Ornat I, Antón-Solanas I, et al. Pretransplant Physical Activity and Cardiovascular Risk Factors in Kidney Transplant Candidates: A Cross-Sectional Study. Healthcare. 2025; 13(10):1200. https://doi.org/10.3390/healthcare13101200
Chicago/Turabian StyleFerrer-López, Emilia, Víctor Cantín-Lahoz, Francisco Javier Rubio-Castañeda, Juan José Aguilón-Leiva, María García-Magán, Carlos Navas-Ferrer, Eva Benito-Ruiz, María Isabel Serrano-Vicente, Isabel Blázquez-Ornat, Isabel Antón-Solanas, and et al. 2025. "Pretransplant Physical Activity and Cardiovascular Risk Factors in Kidney Transplant Candidates: A Cross-Sectional Study" Healthcare 13, no. 10: 1200. https://doi.org/10.3390/healthcare13101200
APA StyleFerrer-López, E., Cantín-Lahoz, V., Rubio-Castañeda, F. J., Aguilón-Leiva, J. J., García-Magán, M., Navas-Ferrer, C., Benito-Ruiz, E., Serrano-Vicente, M. I., Blázquez-Ornat, I., Antón-Solanas, I., & Urcola-Pardo, F. (2025). Pretransplant Physical Activity and Cardiovascular Risk Factors in Kidney Transplant Candidates: A Cross-Sectional Study. Healthcare, 13(10), 1200. https://doi.org/10.3390/healthcare13101200







