Assessment of Risk Factors for Coronary Artery Restenosis and Patient Survival During the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Characteristics of the Study Groups
2.1.1. Study Design
2.1.2. Outcomes
2.1.3. Age Distribution
2.1.4. Collection of Clinical and Laboratory Parameters
2.2. Statistical Analysis
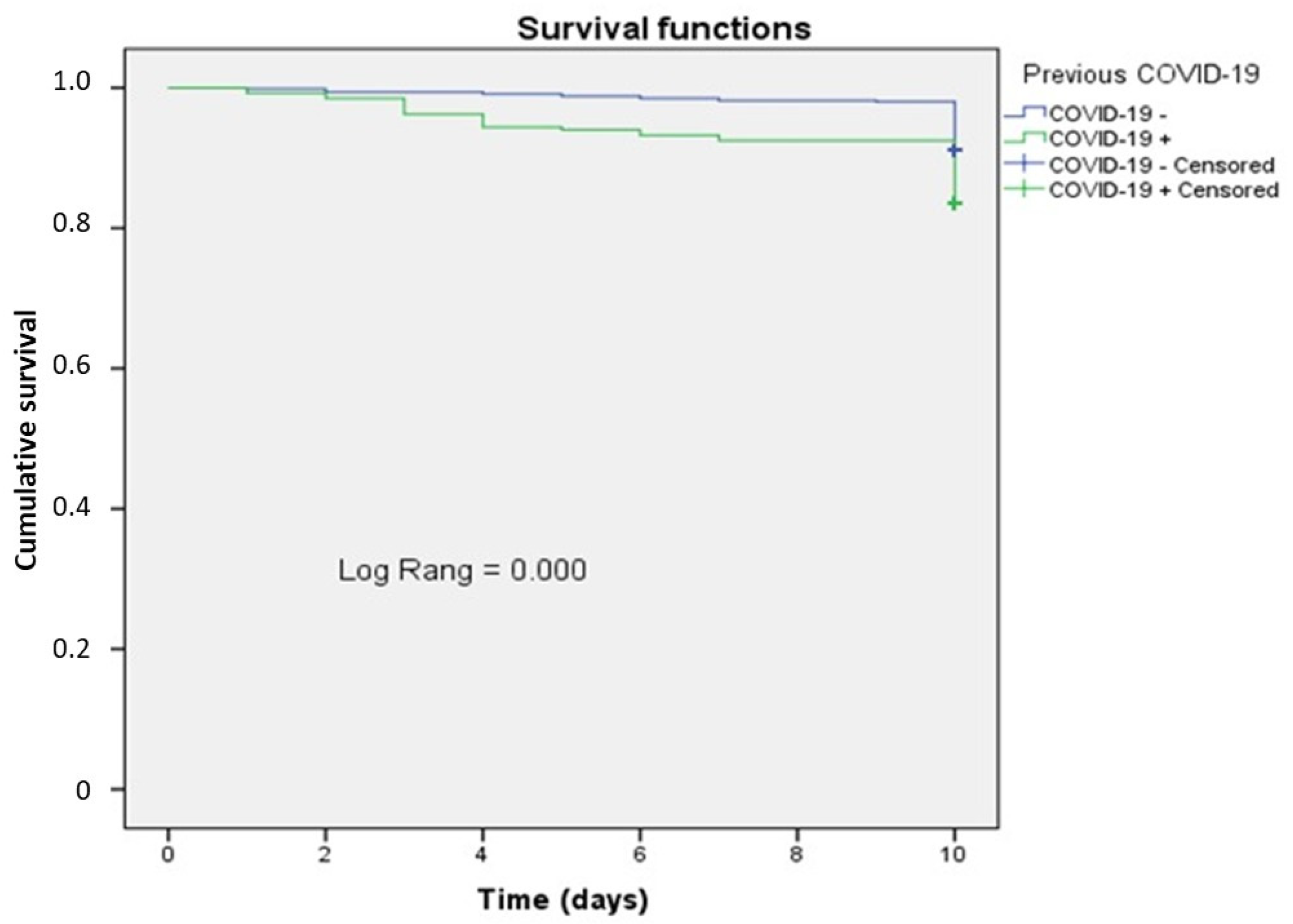
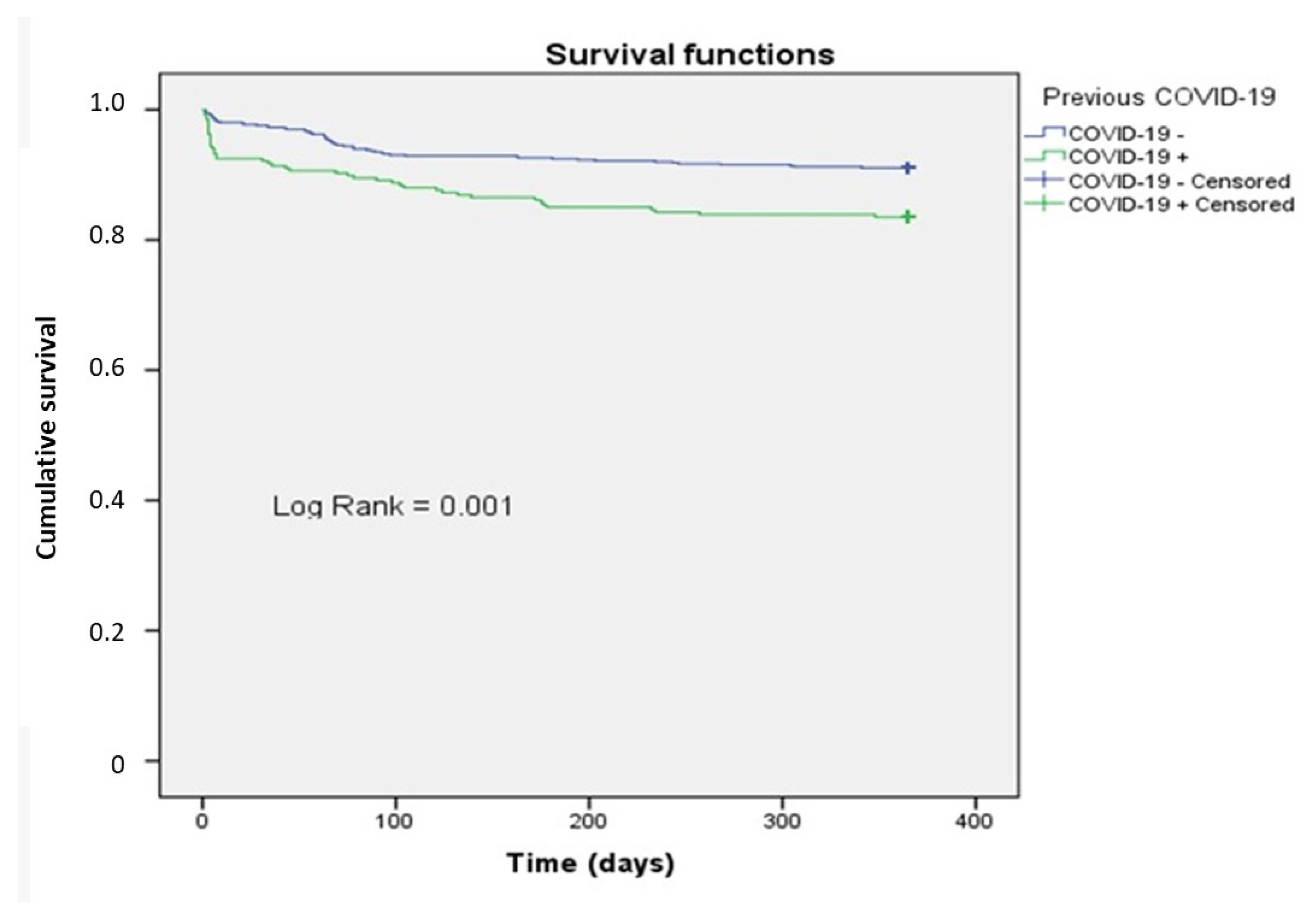
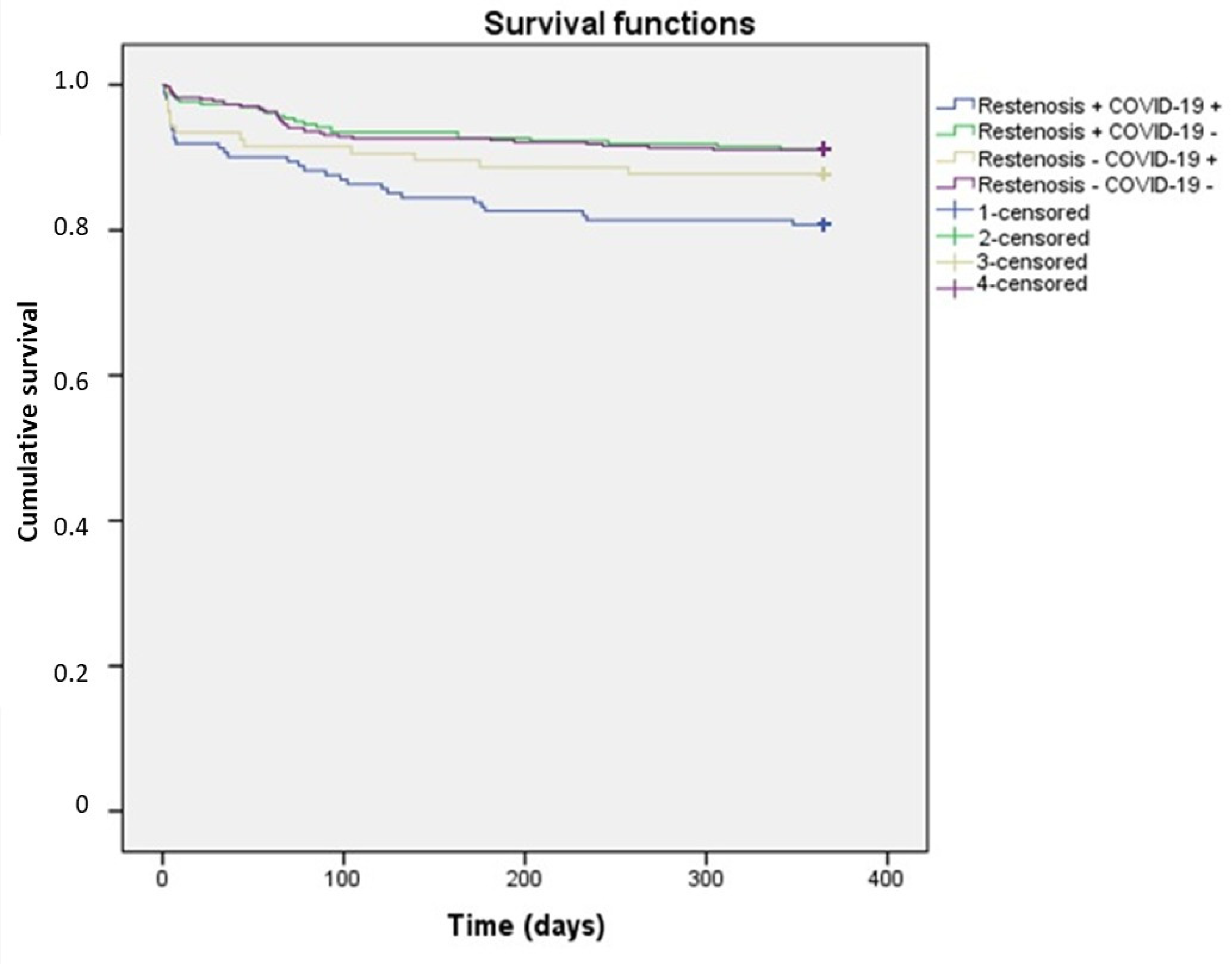
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Megaly, M.; Alani, F.; Cheng, C.I.; Ragina, N. Risk Factors for the Development of Carotid Artery In-Stent Restenosis: Multivariable Analysis. Cardiovasc. Revasc. Med. 2021, 24, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Xue, Z.; Qi, J.; Yin, L.; Duan, B.; Wu, L.; Yang, K.; Gao, B.; Cao, Q.; Mi, J. Risk factors for instent restenosis of sirolimus-coated stents in coronary intervention for patients with unstable angina. Sci. Rep. 2024, 14, 2537. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.; Wang, C.; Zhang, J.; Liu, Z.; Bai, Y.; Chen, Z.; Huang, H.; He, Y. Triglyceride-glucose index and coronary artery disease: A systematic review and meta-analysis of risk, severity, and prognosis. Cardiovasc. Diabetol. 2023, 22, 170. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Hou, J.; Gu, X.; Weng, R.; Zhong, Z.; Liu, S. Incidence and risk factors of in-stent restenosis after percutaneous coronary intervention in patients from southern China. Eur. J. Med. Res. 2022, 27, 12. [Google Scholar] [CrossRef] [PubMed]
- Cortese, B.; Testa, G.; Rivero, F.; Erriquez, A.; Alfonso, F. Long-Term Outcome of Drug-Coated Balloon vs Drug-Eluting Stent for Small Coronary Vessels: PICCOLETO-II 3-Year Follow-Up. JACC Cardiovasc. Interv. 2023, 16, 1054–1061. [Google Scholar] [CrossRef] [PubMed]
- Sheng, X.; Yang, G.; Zhang, Q.; Zhou, Y.; Pu, J. Impact of risk factors on intervened and non-intervened coronary lesions. Am. J. Cardiovasc. Dis. 2024, 14, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Asakura, H.; Ogawa, H. COVID-19-associated coagulopathy and disseminated intravascular coagulation. Int. J. Hematol. 2021, 113, 45–57. [Google Scholar] [CrossRef] [PubMed]
- Valencia, I.; Lumpuy-Castillo, J.; Magalhaes, G.; Sánchez-Ferrer, C.F.; Lorenzo, Ó.; Peiró, C. Mechanisms of endothelial activation, hypercoagulation and thrombosis in COVID-19: A link with diabetes mellitus. Cardiovasc. Diabetol. 2024, 23, 75. [Google Scholar] [CrossRef] [PubMed]
- Azova, M.; Timizheva, K.; Ait Aissa, A.; Blagonravov, M.; Gigani, O.; Aghajanyan, A.; Tskhovrebova, L. Gene Polymorphisms of the Renin-Angiotensin-Aldosterone System as Risk Factors for the Development of In-Stent Restenosis in Patients with Stable Coronary Artery Disease. Biomolecules 2021, 11, 763. [Google Scholar] [CrossRef] [PubMed]
- Pivina, L.; Batenova, G.; Omarov, N.; Ygiyeva, D.; Messova, A.; Alibayeva, G.; Jamedinova, U.; Kurumbayev, R.; Pivin, M. Peculiarities of in-Stent Thrombosis and Restenosis in Coronary Arteries Post-COVID-19: A Systematic Review of Clinical Cases and Case Series. Open Access Emerg. Med. 2025, 17, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Nanavaty, D.; Sinha, R.; Kaul, D.; Sanghvi, A.; Kumar, V.; Vachhani, B.; Singh, S.; Devarakonda, P.; Reddy, S.; Verghese, D. Impact of COVID-19 on Acute Myocardial Infarction: A National Inpatient Sample Analysis. Curr. Probl. Cardiol. 2024, 49, 102030. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Malik, A.H.; Bandyopadhyay, D.; Isath, A.; Gupta, R.; Hajra, A.; Shrivastav, R.; Virani, S.S.; Fonarow, G.C.; Lavie, C.J.; et al. Impact of COVID-19 on Outcomes of Patients Hospitalized With STEMI: A Nationwide Propensity-matched Analysis. Curr. Probl. Cardiol. 2023, 48, 101547. [Google Scholar] [CrossRef] [PubMed]
- Mohsenizadeh, S.A.; Alidoosti, M.; Jalali, A.; Tofighi, S.; Salarifar, M.; Poorhosseini, H.; Jenab, Y.; Ahmadian, T. Comparison of Angiographic and Clinical Outcomes After Primary Percutaneous Coronary Intervention for ST-elevation Myocardial Infarction Between Patients with and Without Concomitant COVID-19 Infection. Crit. Pathw. Cardiol. 2022, 21, 141–146. [Google Scholar] [CrossRef]
- Pivina, L.; Batenova, G.; Ygiyeva, D.; Orekhov, A.; Pivin, M.; Dyussupov, A. Assessment of the Predictive Ability of the Neutrophil-to-Lymphocyte Ratio in Patients with In-Stent Restenosis after COVID-19. Diagnostics 2024, 14, 2262. [Google Scholar] [CrossRef] [PubMed]
- Gu, N.; Chen, P.; Wang, X.; Shen, C.; Deng, Y.; Chen, J.; Ma, Y.; Ma, S.; Hu, X.; Zhao, R.; et al. Association Between the Neutrophil-to-Lymphocyte Ratio and in-Stent Neoatherosclerosis and Plaque Vulnerability: An Optical Coherence Tomography Study. J. Cardiovasc. Pharmacol. 2024, 84, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Adolf, R.; Krinke, I.; Datz, J.; Cassese, S.; Kastrati, A.; Joner, M.; Schunkert, H.; Wall, W.; Hadamitzky, M.; Engel, L.C. Specific calcium deposition on pre-procedural CCTA at the time of percutaneous coronary intervention predicts in-stent restenosis in symptomatic patients. J. Cardiovasc. Comput. Tomogr. 2025, 19, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Lee, O.-H.; Hong, S.-J.; Ahn, C.-M.; Kim, J.-S.; Kim, B.-K.; Ko, Y.-G.; Choi, D.; Jang, Y.; Hong, M.-K. The incidence of noncardiac surgery in patients treated with drug-eluting stents according to age. J. Invasive Cardiol. 2019, 31, E9–E14. [Google Scholar] [CrossRef] [PubMed]
| Risk Factors | Group with In-Stent Restenosis (N = 420) | Group Without In-Stent Restenosis (N = 511) | p | Reference | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Diabetes mellitus | 91 | 201.7 | 100 | 19.6 | 0.430 a | |
| Arterial hypertension | 414 | 98.6 | 497 | 97.3 | 0.170 a | |
| History of COVID-19 | 161 | 38.4 | 106 | 20.8 | 0.001 a | |
| Male gender | 315 | 75 | 385 | 75.3 | 0.904 a | |
| Middle age | 64.2 (56.0–72.4) | 64.3 (56.2–72.4) | 0.813 b | |||
| LVEF | 52.0 (45.75–57.0) | 52.0 (43.0–56.0) | 0.455 b | |||
| D-dimer (ng/mL) | 452.0 (295–619) | 437.0 (293–613) | 0.58 b | 0.0–550.0 | ||
| Troponin I (mcg/L) | 0.1 (0.1–0.26) | 0.1 (0.1–0.28) | 0.831 b | 0.017–0.05 | ||
| ALT (U/L) | 25.0 (17.47–35.95) | 25.6 (18.0–37.9) | 0.43 b | 0.0–32.0 | ||
| AST (U/L) | 23.1 (17.38–33.51) | 23.52 (17.36–36.3) | 0.681 b | 5.0–34.0 | ||
| Creatinine (µmol/L) | 85.25 (72.0–102.0) | 87.0 (72.0–102.1) | 0.794 b | 71.0–115.0 | ||
| C-reactive protein (mg/L) | 10.7 (5.97–17.55) | 9.06 (4.5–17.78) | 0.003 b | 0.10–7.0 | ||
| Triglycerides (mmol/L) | 1.67 (1.17–2.38) | 1.6 (1.12–2.36) | 0.677 b | 0.34–1.70 | ||
| LDL (mmol/L) | 2.78 (2.19–3.45) | 2.78 (2.17–3.49) | 0.882 b | 0.10–3.0 | ||
| Risk Factors | B | OR | 95% Confidence Interval | p | |
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| Diabetes mellitus | 0.128 | 1.137 | 0.826 | 1.564 | 0.431 |
| Arterial hypertension | −0.665 | 0.514 | 0.196 | 1.351 | 0.177 |
| History of COVID-19 | 0.866 | 2.378 | 2.778 | 3.191 | <0.001 |
| Age | −0.001 | 0.999 | 0.986 | 1.012 | 0.858 |
| Male gender | 0.018 | 1.019 | 0.755 | 1.373 | 0.904 |
| LVEF | 0.004 | 1.004 | 0.990 | 1.018 | 0.570 |
| D-dimer | 0.000 | 1.0 | 1.000 | 1.000 | 0.799 |
| Troponin | 0.000 | 1.02 | 0.998 | 1.012 | 0.983 |
| ALT | 0.002 | 1.002 | 0.998 | 1.006 | 0.304 |
| AST | 0.001 | 0.999 | 0.998 | 1.000 | 0.686 |
| Creatinine | 0.001 | 1.001 | 0.999 | 1.002 | 0.953 |
| C-reactive protein | 0.009 | 1.009 | 1.0003 | 1.015 | 0.002 |
| Triglycerides | −0.002 | 0.998 | 0.926 | 1.076 | 0.969 |
| LDL | 0.025 | 1.025 | 0.897 | 1.172 | 0.716 |
| Risk Factors | B | OR | 95% Confidence Interval for OR | p | |
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| COVID-19 | 0.948 | 2.29 | 1.711 | 3.078 | <0.001 |
| C-reactive protein | 0.077 | 1.08 | 1.002 | 1.013 | 0.012 |
| Factors | COVID-19 History +, N = 269 | COVID-19 History −. N = 662 | p |
|---|---|---|---|
| Restenosis, n (%) | 161 (60.3) | 258 (39.0) | <0.001 a |
| Age | 64.0 (59.0–70.0) | 64.0 (57.0–72.0) | 0.824 a |
| Sex: male, n(%) | 193 (72.3) | 506 (76.4) | 0.486 b |
| Arterial hypertension | 179 (96.8) | 300 (98.7) | 0.189 c |
| Diabetes mellitus | 41 (22.2) | 59 (19.4) | 0.464 b |
| Systolic BP | 130.0 (120–141.5) | 130.0 (120.0–141.5) | 0.683 a |
| Diastolic BP | 80.0 (70.0–90.0) | 80.0 (80.0–90,0) | 0.179 a |
| Heart rate | 77.0 (70.0–82.0) | 78.0 (70.0–81.50) | 0.451 a |
| LV EF, % | 51.0 (46.0–56.0) | 52.0 (46.0–56.0) | 0.837 a |
| Leukocytes | 8.2 (6.48–10.6) | 8.04 (6.7–10.30) | 0.755 a |
| Lymphocytes | 24.9 (18.85–33.15) | 25.0 (20.05–31.60) | 0.830 a |
| Neutrophils | 65.0 (57.7–74.3) | 65.35 (58.0–71.67) | 0.764 a |
| NLR | 2.72 (1.75–4.03) | 2.58 (1.89–3.48) | 0.604 a |
| PLR | 122.83 (89.78–168.59) | 115.06 (86.57–149.34) | 0.033 a |
| Platelets | 234.0 (200.0–272.0) | 231.0 (193.0–272.25) | 0.157 a |
| Hemoglobin | 140.0 (128.0–152.0) | 143.0 (132.0–153.25) | 0.093 a |
| APTT | 31.3 (26.7–34.55) | 28.50 (25.14–33.38) | <0.001 a |
| INR | 1.0 (0.9–1.1) | 1.0 (0.93–1.1) | 0.714 a |
| Fibrinogen | 3.30 (2.73–4.16) | 3.14 (2.56–3.80) | 0.014 a |
| D-dimer | 490.0 (346.3–714.0) | 472.0 (282.25–594.00) | <0.001 a |
| Troponin | 0.1 (0.1–2.76) | 0.1 (0.1–0.15) | <0.001 a |
| ALT | 27.0 (17.85–36.8) | 24.2 (17.77–37.00) | 0.295 a |
| AST | 25.0 (18.4–39.0) | 23.0 (17.05–34.0) | 0.002 a |
| CPK | 198.0 (148.5–370.0) | 183.2 (102.6–274.5) | 0.001 a |
| MB CPK | 23.1 (17.1–47.9) | 18.0 (14.3–27.73) | <0.001 a |
| Glucose | 6.2 (5.43–8.66) | 6.0 (5.4–7.38) | 0.012 a |
| Urea | 5.75 (4.74–7.20) | 5.8 (4.80–7.30) | 0.775 a |
| Creatinine | 82.0 (71.0–101.35) | 87.0 (72.63–102.0) | 0.092 a |
| CRP | 11.8 (4.85–21.2) | 8.27 (4.1–15.6) | 0.005 a |
| LDL | 2.88 (2.19–3.48) | 2.71 (2.17–3.47) | 0.542 a |
| HDL | 0.99 (0.88–1.23) | 1.02 (0.9–1.24) | 0.456 a |
| Triglycerides | 1.60 (1.11–2.30) | 1.65 (1.15–2.40) | 0.666 a |
| Risk Factors | Unadjusted Risk | Adjusted Risk | ||
|---|---|---|---|---|
| HR; 95% CI | p | HR; 95% CI | p | |
| COVID-19 | 1.948; 1.319–2.879 | <0.001 | 2.017; 1.364–2.981 | <0.001 |
| LV EF | 0.972; 0.954–0.991 | 0.004 | 0.972; 0.953–0.991 | 0.004 |
| Age | 1.028; 1.008–1.049 | 0.005 | 1.028; 1.008–1.048 | 0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pivina, L.; Orekhov, A.; Batenova, G.; Ygiyeva, D.; Belikhina, T.; Pivin, M.; Dyussupov, A. Assessment of Risk Factors for Coronary Artery Restenosis and Patient Survival During the COVID-19 Pandemic. Healthcare 2025, 13, 1175. https://doi.org/10.3390/healthcare13101175
Pivina L, Orekhov A, Batenova G, Ygiyeva D, Belikhina T, Pivin M, Dyussupov A. Assessment of Risk Factors for Coronary Artery Restenosis and Patient Survival During the COVID-19 Pandemic. Healthcare. 2025; 13(10):1175. https://doi.org/10.3390/healthcare13101175
Chicago/Turabian StylePivina, Lyudmila, Andrey Orekhov, Gulnara Batenova, Diana Ygiyeva, Tatyana Belikhina, Maksim Pivin, and Altay Dyussupov. 2025. "Assessment of Risk Factors for Coronary Artery Restenosis and Patient Survival During the COVID-19 Pandemic" Healthcare 13, no. 10: 1175. https://doi.org/10.3390/healthcare13101175
APA StylePivina, L., Orekhov, A., Batenova, G., Ygiyeva, D., Belikhina, T., Pivin, M., & Dyussupov, A. (2025). Assessment of Risk Factors for Coronary Artery Restenosis and Patient Survival During the COVID-19 Pandemic. Healthcare, 13(10), 1175. https://doi.org/10.3390/healthcare13101175






