Healthcare Utilization Among United States Service Members with Combat-Related Lower Extremity Limb Salvage
Abstract
1. Introduction
2. Methods
2.1. Data Sources and Study Sample
2.2. Statistical Analysis
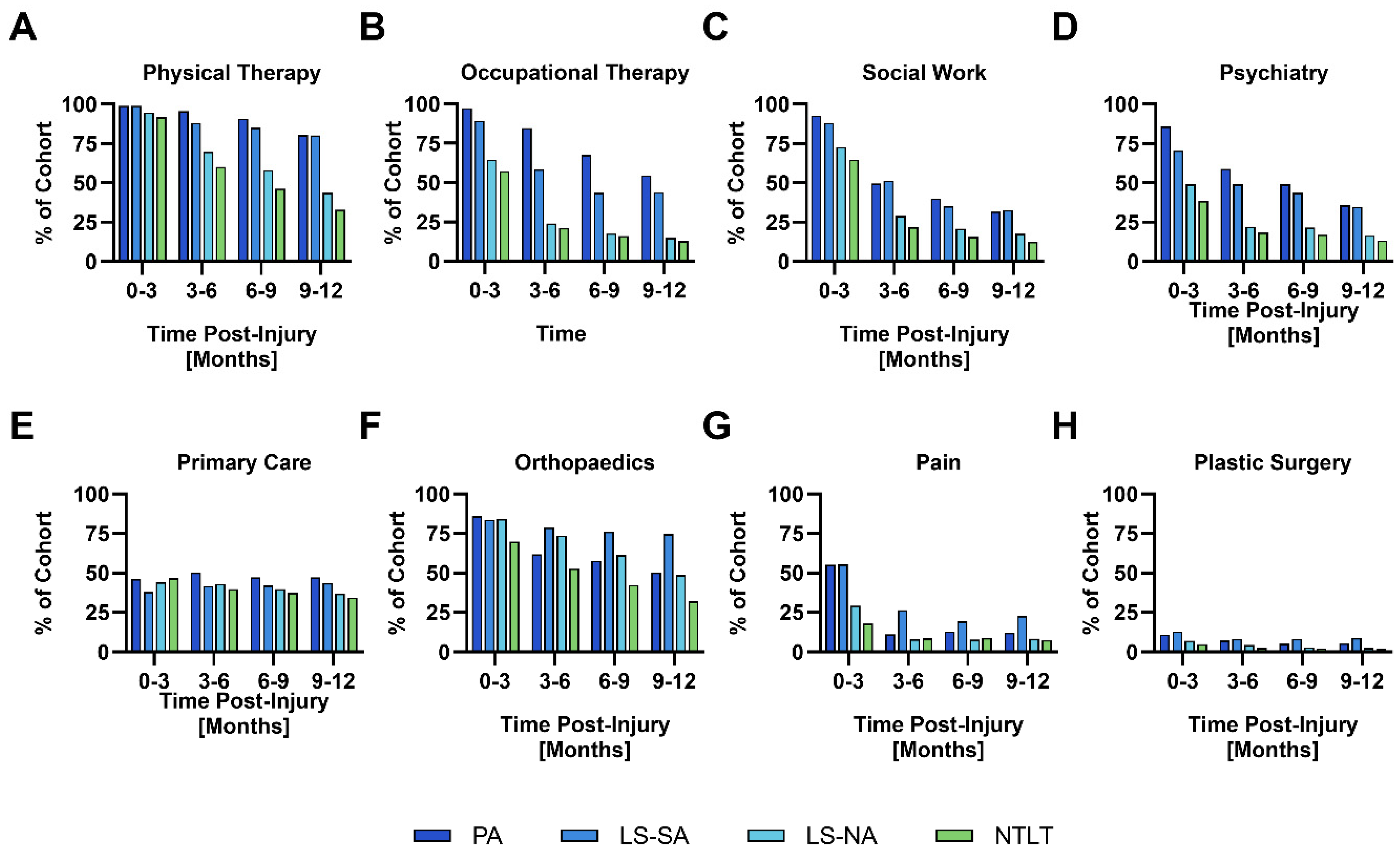
3. Results
4. Discussion
4.1. Physical and Occupational Therapy Service Utilization
4.2. Mental Health Service Utilization
4.3. Peer Support Networks
4.4. Distribution of Care for Complex Extremity Trauma Patients
4.5. Follow-Up and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Owens, B.D.; Kragh, J.F., Jr.; Macaitis, J.; Svoboda, S.J.; Wenke, J.C. Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J. Orthop. Trauma 2007, 21, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Owens, B.D.; Kragh, J.F., Jr.; Wenke, J.C.; Macaitis, J.; Wade, C.E.; Holcomb, J.B. Combat wounds in operation Iraqi Freedom and operation Enduring Freedom. J. Trauma 2008, 64, 295–299. [Google Scholar] [CrossRef]
- Eskridge, S.L.; Macera, C.A.; Galarneau, M.R.; Holbrook, T.L.; Woodruff, S.I.; MacGregor, A.J.; Morton, D.J.; Shaffer, R.A. Injuries from combat explosions in Iraq: Injury type, location, and severity. Injury 2012, 43, 1678–1682. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, C.K.; Green, B.; Moore, J.; Wyatt, M.; Boulanger, L.; Belnap, B.; Harsch, P.; Donaldson, D.S. Integrated musculoskeletal rehabilitation care at a comprehensive combat and complex casualty care program. J. Manip. Physiol. Ther. 2009, 32, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, K.F.; Pasquina, P.F. Overview of the rehabilitation of the combat casualty. Mil. Med. 2010, 175 (Suppl. S7), 13–17. [Google Scholar] [CrossRef] [PubMed]
- Gordon, W.T.; Stannard, J.P.; Pasquina, P.F.; Archer, K.R. Evolution of orthopaedic rehabilitation care. J. Am. Acad. Orthop. Surg. 2012, 20 (Suppl. S1), S80–S83. [Google Scholar] [CrossRef]
- Rivera, J.C.; Pasquina, P.F. Comprehensive Rehabilitation Following Combat Extremity Trauma: Evolution and Its Impact on Outcomes. J. Orthop. Trauma 2016, 30 (Suppl. S3), S31–S33. [Google Scholar] [CrossRef]
- Castillo, R.C.; Carlini, A.R.; Doukas, W.C.; Hayda, R.A.; Frisch, H.M.; Andersen, R.C.; D’Alleyrand, J.-C.; Mazurek, M.T.; Ficke, J.R.; Keeling, J.J. Pain, depression, and posttraumatic stress disorder following major extremity trauma among United States military serving in Iraq and Afghanistan: Results from the military extremity trauma and amputation/limb salvage study. J. Orthop. Trauma 2021, 35, e96–e102. [Google Scholar] [CrossRef]
- Melcer, T.; Walker, J.; Sechriest, V.F.; Bhatnagar, V.; Richard, E.; Perez, K.; Galarneau, M. A retrospective comparison of five-year health outcomes following upper limb amputation and serious upper limb injury in the Iraq and Afghanistan conflicts. PM&R 2019, 11, 577–589. [Google Scholar]
- Low, E.E.; Inkellis, E.; Morshed, S. Complications and revision amputation following trauma-related lower limb loss. Injury 2017, 48, 364–370. [Google Scholar] [CrossRef]
- Masini, B.D.; Waterman, S.M.; Wenke, J.C.; Owens, B.D.; Hsu, J.R.; Ficke, J.R. Resource utilization and disability outcome assessment of combat casualties from Operation Iraqi Freedom and Operation Enduring Freedom. J. Orthop. Trauma 2009, 23, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Schulz, R.N.; Jannace, K.C.; Cooper, D.B.; Sparling, T.L.; Luken, M.L.; Pasquina, P.F. Health Care Utilization After Major Limb Loss in Adults (18–64) Receiving Care in the Military Health System From 2001 to 2017. Arch. Phys. Med. Rehabil. 2024, 105, 335–342. [Google Scholar] [CrossRef]
- Melcer, T.; Walker, J.; Bhatnagar, V.; Richard, E. Clinic Use at the Departments of Defense and Veterans Affairs Following Combat Related Amputations. Mil. Med. 2020, 185, e244–e253. [Google Scholar] [CrossRef] [PubMed]
- Galarneau, M.R.; Hancock, W.C.; Konoske, P.; Melcer, T.; Vickers, R.R.; Walker, G.J.; Zouris, J.M. The Navy-Marine Corps Combat Trauma Registry. Mil. Med. 2006, 171, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.M.; Althausen, P.L.; Kellam, J.; Bosse, M.J.; Castillo, R. Complications following limb-threatening lower extremity trauma. J. Orthop. Trauma 2009, 23, 1–6. [Google Scholar] [CrossRef]
- Busse, J.W.; Jacobs, C.L.; Swiontkowski, M.F.; Bosse, M.J.; Bhandari, M. Complex limb salvage or early amputation for severe lower-limb injury: A meta-analysis of observational studies. J. Orthop. Trauma 2007, 21, 70–76. [Google Scholar] [CrossRef]
- Goldman, S.M.; Eskridge, S.L.; Franco, S.R.; Souza, J.M.; Tintle, S.M.; Dowd, T.C.; Alderete, J.; Potter, B.K.; Dearth, C.L. A Data-Driven Method to Discriminate Limb Salvage from Other Combat-Related Extremity Trauma. J. Clin. Med. 2023, 12, 6357. [Google Scholar] [CrossRef]
- Goldman, S.M.; Eskridge, S.L.; Franco, S.R.; Dearth, C.L. Demographics and Comorbidities of United States Service Members with Combat-Related Lower Extremity Limb Salvage. J. Clin. Med. 2023, 12, 6879. [Google Scholar] [CrossRef]
- Melcer, T.; Sechriest, V.F.; Walker, J.; Galarneau, M. A comparison of health outcomes for combat amputee and limb salvage patients injured in Iraq and Afghanistan wars. J. Trauma Acute Care Surg. 2013, 75 (Suppl. 2), S247–S254. [Google Scholar] [CrossRef]
- MacKenzie, E.J.; Jones, A.S.; Bosse, M.J.; Castillo, R.C.; Pollak, A.N.; Webb, L.X.; Swiontkowski, M.F.; Kellam, J.F.; Smith, D.G.; Sanders, R.W.; et al. Health-care costs associated with amputation or reconstruction of a limb-threatening injury. J. Bone Jt. Surg. 2007, 89, 1685–1692. [Google Scholar] [CrossRef]
- Wolf, S.J.; Bebarta, V.S.; Bonnett, C.J.; Pons, P.T.; Cantrill, S.V. Blast injuries. Lancet 2009, 374, 405–415. [Google Scholar] [CrossRef] [PubMed]
- DePalma, R.G.; Burris, D.G.; Champion, H.R.; Hodgson, M.J. Blast injuries. N. Engl. J. Med. 2005, 352, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Mullenix, P.S.; Steele, S.R.; Andersen, C.A.; Starnes, B.W.; Salim, A.; Martin, M.J. Limb salvage and outcomes among patients with traumatic popliteal vascular injury: An analysis of the National Trauma Data Bank. J. Vasc. Surg. 2006, 44, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Castillo, R.C.; MacKenzie, E.J.; Webb, L.X.; Bosse, M.J.; Avery, J. Use and perceived need of physical therapy following severe lower-extremity trauma. Arch. Phys. Med. Rehabil. 2005, 86, 1722–1728. [Google Scholar] [CrossRef]
- Franco, S.R.; Eskridge, S.L.; Goldman, S.M.; Dearth, C.L. Characterization of Secondary Health Conditions among United States Service Members with Combat-Related Lower Extremity Limb Salvage. J. Clin. Med. 2025, 14, 3472. [Google Scholar] [CrossRef]
- Richardson, L.K.; Frueh, B.C.; Acierno, R. Prevalence estimates of combat-related post-traumatic stress disorder: Critical review. Aust. N. Z. J. Psychiatry 2010, 44, 4–19. [Google Scholar] [CrossRef]
- Doukas, W.C.; Hayda, R.A.; Frisch, H.M.; Andersen, R.C.; Mazurek, M.T.; Ficke, J.R.; Keeling, J.J.; Pasquina, P.F.; Wain, H.J.; Carlini, A.R.; et al. The Military Extremity Trauma Amputation/Limb Salvage (METALS) study: Outcomes of amputation versus limb salvage following major lower-extremity trauma. J. Bone Jt. Surg. 2013, 95, 138–145. [Google Scholar] [CrossRef]
- Holbrook, T.L.; Anderson, J.P.; Sieber, W.J.; Browner, D.; Hoyt, D.B. Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. J. Trauma 1999, 46, 765–771, discussion 771–763. [Google Scholar] [CrossRef]
- Michaels, A.J.; Michaels, C.E.; Moon, C.H.; Smith, J.S.; Zimmerman, M.A.; Taheri, P.A.; Peterson, C. Posttraumatic stress disorder after injury: Impact on general health outcome and early risk assessment. J. Trauma 1999, 47, 460–466, discussion 466–467. [Google Scholar] [CrossRef]
- Richardson, J.D.; Contractor, A.A.; Armour, C.; St Cyr, K.; Elhai, J.D.; Sareen, J. Predictors of long-term treatment outcome in combat and peacekeeping veterans with military-related PTSD. J. Clin. Psychiatry 2014, 75, e1299–e1305. [Google Scholar] [CrossRef]
- McCarthy, M.L.; MacKenzie, E.J.; Edwin, D.; Bosse, M.J.; Castillo, R.C.; Starr, A. Psychological distress associated with severe lower-limb injury. J. Bone Jt. Surg. 2003, 85, 1689–1697. [Google Scholar] [CrossRef] [PubMed]
- Reichmann, J.P.; Bartman, K.R. An integrative review of peer support for patients undergoing major limb amputation. J. Vasc. Nurs. 2018, 36, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Keeves, J.; Hutchison, A.; D’Cruz, K.; Anderson, S. Social and community participation following traumatic lower limb amputation: An exploratory qualitative study. Disabil. Rehabil. 2023, 45, 4404–4412. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.D.; Forshaw, M.J. The experience of amputation and prosthesis use for adults: A metasynthesis. Disabil. Rehabil. 2013, 35, 1133–1142. [Google Scholar] [CrossRef]
- Cain, J.J.; Ignaszewski, D.; Blymire, C. Living Well After Amputation: Lessons in Innovation, Peer Support, and Health Policy. Tech. Orthop. 2021, 36, 360–366. [Google Scholar] [CrossRef]
- Bosse, M.J.; MacKenzie, E.J.; Kellam, J.F.; Burgess, A.R.; Webb, L.X.; Swiontkowski, M.F.; Sanders, R.W.; Jones, A.L.; McAndrew, M.P.; Patterson, B.M.; et al. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N. Engl. J. Med. 2002, 347, 1924–1931. [Google Scholar] [CrossRef]
| Military Medical Treatment Facilities |
|---|
| Blanchfield Army Community Hospital |
| Brooke Army Medical Center # |
| Eisenhower Army Medical Center |
| Landstuhl Regional Medical Center |
| Madigan Army Medical Center |
| Naval Hospital Camp Lejeune |
| Naval Medical Center San Diego # |
| Walter Reed Army/National Military Medical Center # |
| Womack Army Medical Center-Ft Bragg |
| Outpatient Clinics |
| Mental Health |
| Neurology |
| Occupational Therapy |
| Orthopedics |
| Orthotic Laboratory * |
| Pain Management |
| Physical Medicine |
| Physical Therapy |
| Plastic Surgery |
| Primary Care |
| Psychiatry |
| Psychology |
| Social Work |
| Inpatient Utilization | PA n = 882 | LS-SA n = 269 | LS-NA n = 1716 | NTLT n = 1343 | p Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Inpatient bed days 1–6 | 56.2 | 37.1 | 65.6 | 56.7 | 28.2 | 26.2 | 20.3 | 26.6 | <0.001 |
| ICU bed days 2–5 | 6.3 | 12.4 | 5.3 | 14.3 | 2.0 | 5.6 | 1.7 | 5.8 | <0.001 |
| Hospitalizations | f | % | f | % | f | % | f | % | <0.001 |
| 1 | 3 | 0.3 | 2 | 0.7 | 151 | 8.8 | 276 | 20.6 | |
| 2 | 318 | 36.0 | 60 | 22.3 | 893 | 52.0 | 708 | 52.7 | |
| 3 | 290 | 32.9 | 98 | 36.4 | 426 | 24.8 | 230 | 16.4 | |
| ≥4 | 271 | 30.7 | 109 | 40.5 | 246 | 14.3 | 139 | 10.3 | |
| Outpatient Clinics | Total Sample (n = 4275) | PA (n = 885) | LS-SA (n = 269) | LS-NA (n = 1749) | NTLT (n = 1372) | p Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| f | % | f | % | f | % | f | % | f | % | ||
| Physical Therapy | 4158.0 | 97.3 | 880.0 | 99.4 | 267.0 | 99.3 | 1706.0 | 97.5 | 1305.0 | 95.1 | <0.001 |
| Orthopedics | 3831.0 | 89.6 | 837.0 | 94.6 | 261.0 | 97.0 | 1614.0 | 92.3 | 1119.0 | 81.6 | <0.001 |
| Social Work | 3388.0 | 79.2 | 853.0 | 96.4 | 245.0 | 91.1 | 1339.0 | 76.6 | 951.0 | 69.3 | <0.001 |
| Occupational Therapy | 3163.0 | 74.0 | 873.0 | 98.6 | 255.0 | 94.8 | 1202.0 | 68.7 | 833.0 | 60.7 | <0.001 |
| Primary Care | 2854.0 | 66.8 | 572.0 | 64.6 | 167.0 | 62.1 | 1166.0 | 66.7 | 949.0 | 69.2 | 0.04 |
| Psychiatry | 2579.0 | 60.3 | 796.0 | 89.9 | 213.0 | 79.2 | 955.0 | 54.6 | 615.0 | 44.8 | <0.001 |
| Neurology | 2447.0 | 57.2 | 569.0 | 64.3 | 166.0 | 61.7 | 940.0 | 53.7 | 772.0 | 56.3 | <0.001 |
| Physical Medicine | 2186.0 | 51.1 | 869.0 | 98.2 | 222.0 | 82.5 | 653.0 | 37.3 | 442.0 | 32.2 | <0.001 |
| Orthotic Laboratory * | 2005.0 | 46.9 | 716.0 | 80.9 | 187.0 | 69.5 | 730.0 | 41.7 | 372.0 | 27.1 | <0.001 |
| Pain Management | 1708.0 | 39.9 | 544.0 | 61.5 | 183.0 | 68.0 | 626.0 | 35.8 | 355.0 | 25.9 | <0.001 |
| Mental Health | 1521.0 | 35.6 | 280.0 | 31.6 | 99.0 | 36.8 | 622.0 | 35.6 | 520.0 | 37.9 | 0.02 |
| Psychology | 1217.0 | 28.5 | 274.0 | 31.0 | 81.0 | 30.1 | 492.0 | 28.1 | 370.0 | 27.0 | 0.2 |
| Plastic Surgery | 508.0 | 11.9 | 165.0 | 18.6 | 61.0 | 22.7 | 181.0 | 10.3 | 101.0 | 7.4 | <0.001 |
| Outpatient Clinics | Total Sample | PA | LS-SA | LS-NA | NTLT | p Value ^ | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Physical Therapy 1–6 | 58.9 | 52.6 | 120.4 | 43.7 | 90.2 | 50.0 | 41.7 | 38.5 | 32.8 | 35.7 | <0.001 |
| Occupational Therapy 1–5 | 28.9 | 37.9 | 57.3 | 49.4 | 29.5 | 29.8 | 17.0 | 23.9 | 16.1 | 24.2 | <0.001 |
| Psychiatric 2–5 | 14.9 | 16.4 | 20.4 | 16.9 | 21.1 | 20.3 | 11.5 | 14.1 | 10.9 | 14.8 | <0.001 |
| Orthopedics 2–6 | 14.8 | 17.9 | 25.7 | 26.8 | 22.4 | 20.6 | 12.3 | 12.0 | 8.6 | 9.9 | <0.001 |
| Orthotic Laboratory *,1–5 | 13.6 | 18.0 | 30.0 | 19.8 | 14.2 | 13.3 | 2.8 | 2.8 | 2.7 | 3.3 | <0.001 |
| Primary Care 2–6 | 13.0 | 15.6 | 18.6 | 18.6 | 17.5 | 18.6 | 11.9 | 14.5 | 10.1 | 13.2 | <0.001 |
| Social Work 2–6 | 12.6 | 13.3 | 19.2 | 15.6 | 18.5 | 16.8 | 10.1 | 10.6 | 8.6 | 10.5 | <0.001 |
| Physical Medicine 1–5 | 12.1 | 12.8 | 20.1 | 13.3 | 12.5 | 12.1 | 5.9 | 8.2 | 5.3 | 7.3 | <0.001 |
| Pain Management 2–5 | 8.0 | 9.3 | 8.9 | 9.6 | 10.9 | 11.2 | 7.0 | 8.9 | 6.6 | 8.1 | <0.001 |
| Mental Health 1,4,5 | 7.1 | 11.4 | 6.5 | 6.7 | 11.5 | 20.6 | 6.3 | 8.0 | 7.6 | 14.0 | <0.001 |
| Plastic Surgery | 5.5 | 7.5 | 4.5 | 7.0 | 6.8 | 9.1 | 6.3 | 8.5 | 4.8 | 4.9 | 0.19 |
| Psychology | 5.2 | 6.9 | 6.0 | 8.5 | 5.8 | 6.9 | 5.0 | 6.3 | 4.7 | 6.1 | 0.05 |
| Neurology | 3.4 | 5.3 | 4.0 | 5.2 | 3.8 | 6.0 | 3.2 | 5.7 | 3.3 | 4.8 | 0.28 |
| Inpatient Admission Facility | PA n = 2824 (Total) n = 882 (First/Last Only) | LS-SA n = 971 (Total) n = 269 (First/Last Only) | LS-NA n = 4364 (Total) n = 1716 (First/Last Only) | NTLT n = 2983 (Total) n = 1343 (First/Last Only) | ||||
|---|---|---|---|---|---|---|---|---|
| f | % | f | % | f | % | f | % | |
| Walter Reed Army/National Military Medical Center | ||||||||
| Total | 1297 | 45.9 | 395 | 40.7 | 1120 | 25.7 | 650 | 21.8 |
| First admission | 2 | <1 | 2 | <1 | 16 | <1 | 16 | 1.2 |
| Last admission | 533 | 60.4 | 134 | 49.8 | 607 | 35.4 | 399 | 29.1 |
| Landstuhl Regional Medical Center | ||||||||
| Total | 881 | 31.2 | 267 | 27.5 | 1692 | 38.8 | 1305 | 43.7 |
| First admission | 880 | 99.8 | 265 | 98.5 | 1672 | 97.4 | 1284 | 95.6 |
| Last admission | 1 | <1 | 2 | <1 | 133 | 7.7 | 245 | 18.2 |
| Brooke Army Medical Center | ||||||||
| Total | 463 | 16.4 | 135 | 13.9 | 526 | 12 | 296 | 9.9 |
| First admission | 0 | 0 | 0 | 0 | 1 | <1 | 5 | <1 |
| Last admission | 246 | 27.9 | 62 | 23 | 289 | 16.8 | 174 | 13.0 |
| Naval Medical Center San Diego | ||||||||
| Total | 149 | 5.3 | 82 | 8.4 | 162 | 3.7 | 128 | 4.3 |
| First admission | 0 | 0 | 0 | 0 | 1 | <1 | 4 | <1 |
| Last admission | 84 | 9.5 | 35 | 13.0 | 98 | 5.7 | 77 | 5.7 |
| Madigan Army Medical Center | ||||||||
| Total | 2 | <1 | 22 | 1.0 | 129 | 3.0 | 87 | 2.9 |
| First admission | 0 | 0 | 0 | 0 | 2 | <1 | 5 | <1 |
| Last admission | 1 | <1 | 10 | 3.7 | 100 | 5.8 | 67 | 5.7 |
| Womack Army Medical Center | ||||||||
| Total | 2 | <1 | 5 | <1 | 138 | 3.2 | 82 | 2.7 |
| First admission | 0 | 0 | 0 | 0 | 4 | <1 | 1 | <1 |
| Last admission | 1 | <1 | 1 | <1 | 87 | 5.1 | 67 | 5.0 |
| Eisenhower Army Medical Center | ||||||||
| Total | 3 | <1 | 6 | <1 | 83 | 1.9 | 56 | 1.9 |
| First admission | 0 | 0 | 0 | 0 | 1 | <1 | 2 | <1 |
| Last admission | 3 | <1 | 3 | 1.1 | 58 | 3.4 | 42 | 3.1 |
| Other inpatient facilities (<1% individually) | ||||||||
| Total | 27 | 1.0 | 59 | 6.1 | 515 | 11.8 | 379 | 12.7 |
| First admission | 0 | 0 | 2 | <1 | 19 | 1.1 | 26 | 1.9 |
| Last admission | 13 | 1.5 | 22 | 8.2 | 344 | 20.0 | 272 | 20.2 |
| Outpatient Location of Care | PA | LS-SA | LS-NA | NTLT | ||||
|---|---|---|---|---|---|---|---|---|
| n = 268,807 | n = 58,996 | n = 167,900 | n = 103,747 | |||||
| f | % | f | % | f | % | f | % | |
| Walter Reed Army/National Military Medical Center | 177,418 | 66.0 | 33,928 | 57.5 | 63,911 | 38.1 | 36,197 | 34.9 |
| Brooke Army Medical Center | 65,007 | 24.2 | 13,188 | 22.3 | 34,788 | 20.7 | 15,743 | 15.2 |
| Naval Medical Center San Diego | 21,036 | 7.8 | 6344 | 10.7 | 8013 | 4.8 | 4293 | 4.1 |
| Landstuhl Regional Medical Center | 2087 | <1 | 601 | 1.0 | 3907 | 2.3 | 3433 | 3.3 |
| Madigan Army Medical Center | 156 | <1 | 1006 | 1.7 | 5557 | 3.3 | 3239 | 3.1 |
| Womack Army Medical Center-Ft Bragg | 106 | <1 | 274 | <1 | 4996 | 3.0 | 3534 | 3.4 |
| Naval Hospital Camp Lejeune | 143 | <1 | 89 | <1 | 4228 | 2.5 | 3782 | 3.6 |
| Blanchfield Army Community Hospital | 96 | <1 | 137 | <1 | 4647 | 2.8 | 2719 | 2.6 |
| Other outpatient facilities (<1% individually) | 2758 | 1.0 | 3429 | 5.8 | 37,853 | 22.5 | 30,807 | 29.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eskridge, S.L.; McQuade, A.; Huang, B.; Goldman, S.M.; Dearth, C.L. Healthcare Utilization Among United States Service Members with Combat-Related Lower Extremity Limb Salvage. Healthcare 2025, 13, 1164. https://doi.org/10.3390/healthcare13101164
Eskridge SL, McQuade A, Huang B, Goldman SM, Dearth CL. Healthcare Utilization Among United States Service Members with Combat-Related Lower Extremity Limb Salvage. Healthcare. 2025; 13(10):1164. https://doi.org/10.3390/healthcare13101164
Chicago/Turabian StyleEskridge, Susan L., Aidan McQuade, Benjamin Huang, Stephen M. Goldman, and Christopher L. Dearth. 2025. "Healthcare Utilization Among United States Service Members with Combat-Related Lower Extremity Limb Salvage" Healthcare 13, no. 10: 1164. https://doi.org/10.3390/healthcare13101164
APA StyleEskridge, S. L., McQuade, A., Huang, B., Goldman, S. M., & Dearth, C. L. (2025). Healthcare Utilization Among United States Service Members with Combat-Related Lower Extremity Limb Salvage. Healthcare, 13(10), 1164. https://doi.org/10.3390/healthcare13101164






