Technology Readiness Drives Digital Adoption in Dentistry: Insights from a Cross-Sectional Study
Abstract
1. Introduction
- The first dimension is Optimism. This dimension describes the belief in technology’s ability to enhance efficiency and control.
- The second dimension is Innovativeness. It is a proactive approach to adopting new technologies.
- The third dimension is Discomfort. It describes challenges or hesitations in using digital tools.
2. Materials and Methods
2.1. Survey Instrument and Data Collection
- Demographics—Age, gender, years of experience, clinic type (solo practice, group practice, or MVZ), and geographical location.
- Technology Readiness—Measured using the Technology Readiness Index (TRI 2.0), assessing the four dimensions: Optimism, Innovativeness, Discomfort, and Insecurity [17]. The TRI 2.0 captures participants’ general attitude toward the adoption of new technologies, independent of specific clinical contexts [17]. The full TRI 2.0 questionnaire has been added as Appendix A at the end of the manuscript.
- To link these general attitudes to practical behavior in dental practice, additional survey Section 3 assessed the actual use of specific digital devices within operational workflows, patient management, diagnostics, and treatment planning.
- 3.
- Digital Equipment Usage—The digital technologies included in the survey were selected based on a comprehensive literature review, an analysis of current offerings from leading dental aid providers, and input from an expert panel of 15 experienced dentists. The selection focused on technologies that are currently relevant and applicable in daily clinical practice and oriented toward the patient journey (see Figure 1 in the Results section) [4,5,6,7]. Particular attention was paid to covering all critical phases of the patient journey, ensuring that the most relevant technologies were captured for each area.
- Inclusion criteria for technologies were practical applicability and clinical relevance; highly experimental or purely forensic technologies were excluded.
Independent and Dependent Variables
- Demographic factors such as age, gender, and years of experience.
- Practice characteristics like clinic size, clinic type, number of employees
- Professional development: Level of experience.
- The dependent variables include the following:
- The analysis of the Technology Readiness Score (including the TRI 2.0 total-Score and sub-dimension Scores).
- The number of digital technologies implemented in daily practice was also analyzed.
2.2. Statistical Analysis
- Pearson and Spearman correlations were tested to assess bivariate relationships.
- A multiple linear regression analysis was conducted to examine effects of key demographic and organizational factors on technology readiness.
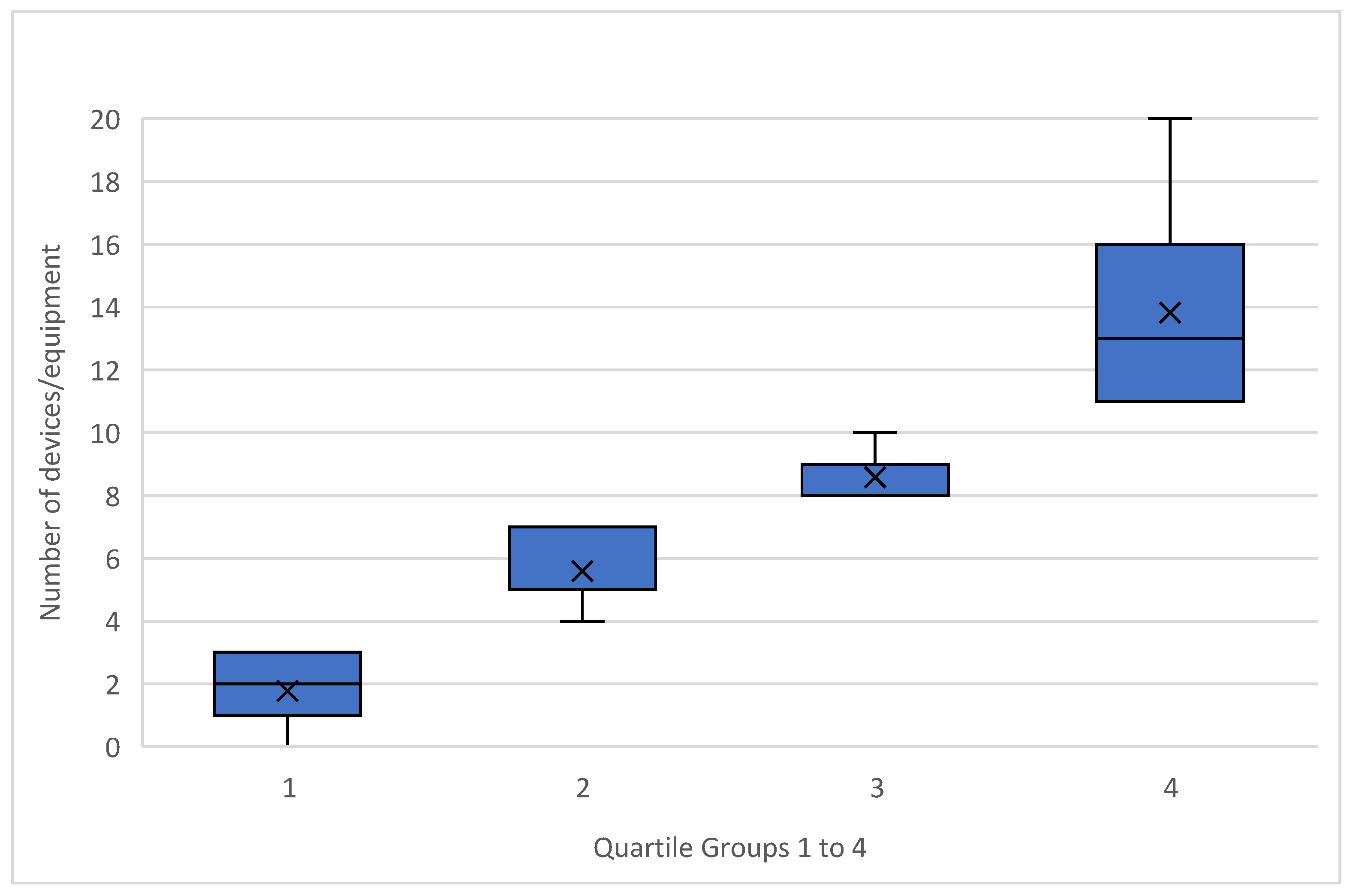
- Quartile-based group comparisons were built to split participants into four groups according to the number of digital devices used, allowing for subgroup comparisons of technology readiness and adoption behaviors.
2.3. Participant Eligibility and Data Anonymization
2.4. Ethical Considerations
3. Results
3.1. Participant Demographics
Gender Distribution
3.2. Current Digital Equipment in Clinics
- I.
- Registration Process:
- II.
- Patient Management:
- III.
- Patient Treatment:
- IV.
- Radiographic Diagnostics and Implantation:
- V.
- AI-Support and Cloud storage:
- VI.
- 3D Applications:
- VII.
- Back-office Processes:
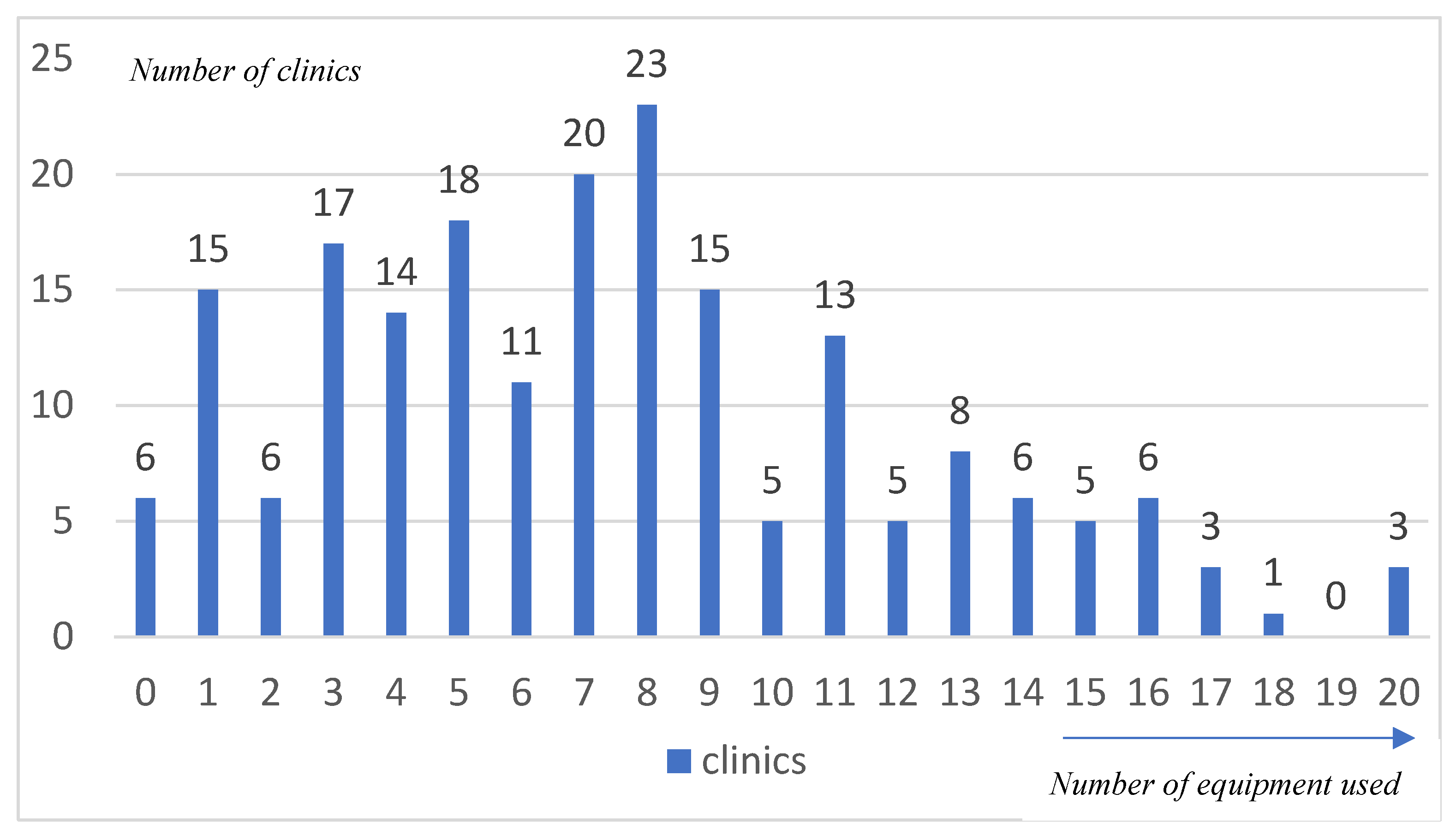
- The mean number of equipment per clinic is 7.5.
- The median number of equipment per clinic is 7.
- The standard deviation is (±) 4.6.
3.3. Technology Readiness
- I.
- TRI-Score: An overall measure of technology readiness.
- II.
- Optimism: The positive attitude towards technology and the belief that it offers more flexibility, efficiency, and control.
- III.
- Innovativeness: The tendency to be open to new technology and to implement it at an early stage.
- IV.
- Discomfort: An uncomfortable feeling caused by technology. This is caused by the impression of not having enough control over the technology or being overwhelmed by the complexity.
- V.
- Insecurity: Uncertainty, which is caused by skepticism regarding the reliability and functionality of technology. [17]
- I.
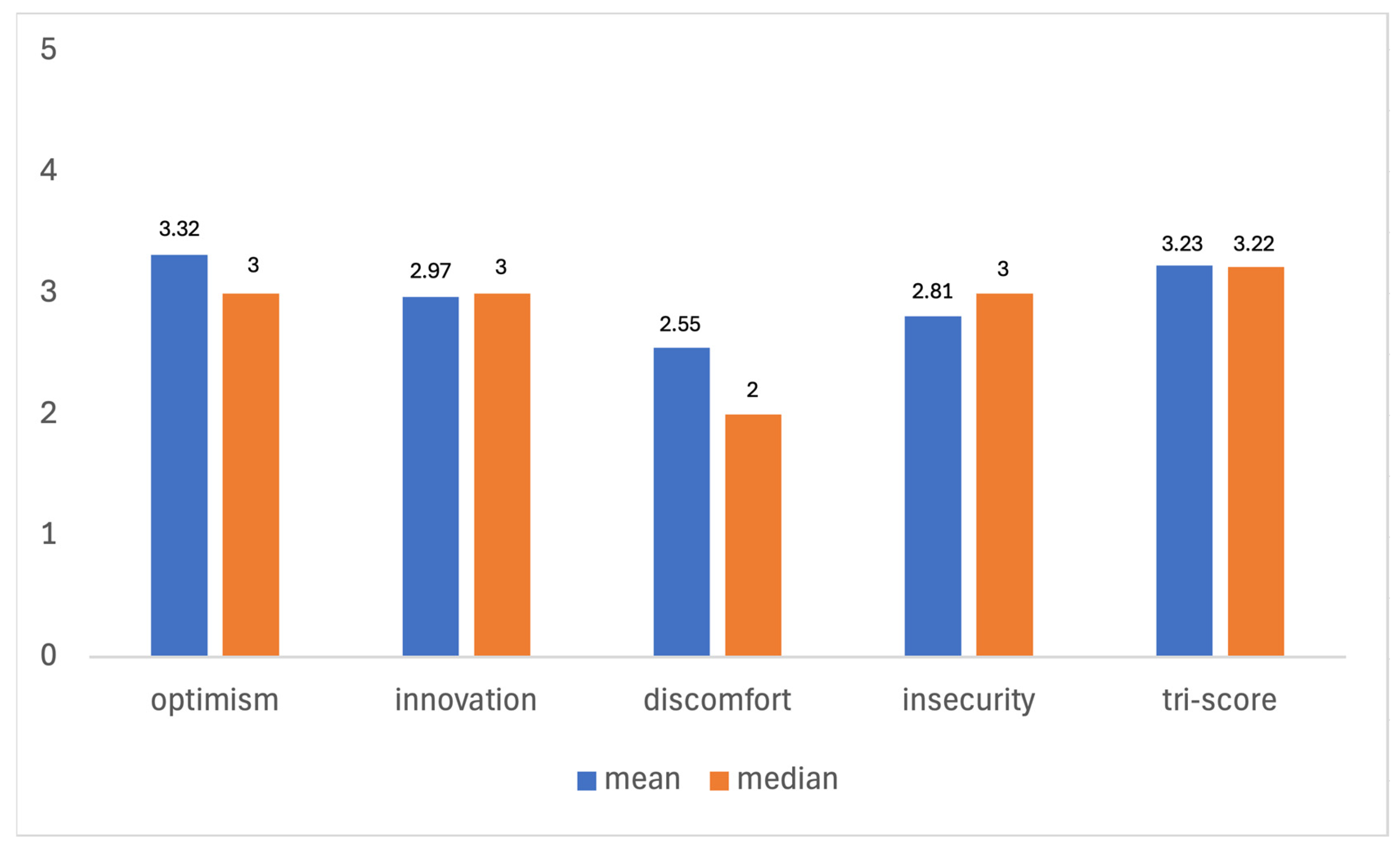
- The mean TRI-Score of 3.23 suggests a moderate level of overall technology readiness among the participants, indicating that, on average, dentists are neither highly resistant nor highly inclined towards adopting new technologies. The median TRI-Score of 3.22 corroborates this finding.
- II.
- Optimism: With a mean score of 3.22 (±) 0.94 and a median of 3, participants generally have a positive attitude towards technology and believe it improves their efficiency and control.
- III.
- Innovativeness: The mean score of 2.97 (±) 1.09 and median of 3 indicate a moderate tendency among dentists to be technology pioneers.
- IV.
- Discomfort: A mean score of 2.55 (±) 0.95 and a median of 2 reflect a moderate level of discomfort with technology, suggesting some participants feel overwhelmed by it.
- V.
- Insecurity: The mean score of 2.81 (±) 1.07 and median of 3 show a moderate level of insecurity, indicating some skepticism about the reliability of technology.
3.4. Correlation Between TRI-Score and Other Parameters
- TRI-Score vs. Age:
- A very significant negative correlation (p < 0.001) was found between the TRI score and the age of the dentists. Younger dentists exhibited higher technology readiness, suggesting that younger professionals are more inclined towards embracing digital technologies.
- TRI-Score vs. Clinic Type:
- The correlation between the TRI score and the type of clinic was non-significant (p = 0.198), indicating that the clinic structure does not significantly influence technology readiness.
- TRI-Score vs. Number of Employees:
- There was a very significant positive correlation (p < 0.001) between the TRI score and the number of employees in the clinic. Dentists in clinics with larger teams exhibited higher technology readiness, indicating that bigger teams may have a greater capacity to support and integrate new technologies.
- TRI-Score vs. Clinic Location:
- The correlation between the TRI score and the location of the clinic (urban, suburban, rural) was not significant (p = 0.331), suggesting that location does not substantially affect technology readiness.
- TRI-Score vs. Gender:
- The correlation between the TRI score and the gender of the dentist was non-significant (p = 0.306), indicating no gender-based differences in technology readiness.
- TRI-Score vs. Professional Development:
- The correlation between the TRI score and the professional development of the dentists was found to be non-significant (p = 0.127), suggesting that continuing education alone may not significantly influence overall technology readiness.
- TRI-Score vs. Number of Equipment:
- A very significant correlation (p < 0.001) was observed between the number of equipment and the TRI score. Dentists in clinics with more equipment had higher technology readiness scores, underscoring the link between digital investment and overall technology readiness.
3.5. Multivariate Analysis TRI-Score
3.6. Correlation Between Number of Equipment and Other Parameters
- Number of Equipment vs. Age:
- The correlation between the number of equipment and the age of the dentists was found to be non-significant (p = 0.338), indicating that age does not significantly influence the extent of digital equipment utilization in clinics.
- Number of Equipment vs. Clinic Type:
- A highly significant correlation (p < 0.001) was observed between the number of equipment and the type of clinic. Multi-dentist clinics (MVZ) and group clinics had significantly more equipment compared to solo clinics, suggesting that larger clinic structures tend to invest more in digital technologies. Table 4 shows the distribution of digital equipment by clinic type, with the average difference between solo practices and multi-dentist clinics (MVZ) being approximately six devices/services.
- Number of Equipment vs. Number of Employees:
- There was a very significant positive correlation (p < 0.001) between the number of equipment and the number of employees in the clinic. This finding indicates that clinics with more staff are likely to have a greater number of digital equipment, possibly to support the higher operational demands.
- Number of Equipment vs. Clinic Location:
- The correlation between the number of equipment and the location of the clinic (urban, suburban, rural) was not significant (p = 0.152), suggesting that geographical location does not make a major contribution to the adoption of digital technologies.
- Number of Equipment vs. Gender:
- The correlation between the number of equipment and the gender of the dentist was found to be non-significant (p = 0.278), indicating no gender-based differences in the adoption of digital technologies.
- Number of Equipment vs. Professional Development:
- A significant (p = 0.022) but weak correlation was found between the number of equipment and the professional development of the dentists. Dentists who participated in more continuing education tended to have slightly more equipment, suggesting that ongoing education may play a role in supporting digital adoption.
3.7. Digitalization Types
- 1
- Low Adopters (1st Quartile) (n = 44):
- 2
- Moderate Adopters (2nd Quartile) (n = 63):
- 3
- Advanced Adopters (3rd Quartile) (n = 43):
- 4
- Power Users (4th Quartile) (n = 50):
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Not True at All | True Little | Partly True | Pretty Much Right | Completely True | |
|---|---|---|---|---|---|
| New technologies contribute to a better quality of life | 1 | 2 | 3 | 4 | 5 |
| Technology gives me more freedom of mobility | 1 | 2 | 3 | 4 | 5 |
| Technology gives people more control over their daily lives | 1 | 2 | 3 | 4 | 5 |
| Technology makes me more productive in my personal live | 1 | 2 | 3 | 4 | 5 |
| Other people come to me for advice on new technologies | 1 | 2 | 3 | 4 | 5 |
| In general, I am among the first in my circle of friends to acquire new technology when it appears | 1 | 2 | 3 | 4 | 5 |
| I can usually figure out new high-tech products and services without help from others | 1 | 2 | 3 | 4 | 5 |
| I keep up with the latest technological developments in my areas of interest | 1 | 2 | 3 | 4 | 5 |
| When I get technical support from a provider of a high-tech product or service, I sometimes feel as if I am being taken advantage of by someone who knows more than I do | 1 | 2 | 3 | 4 | 5 |
| Technical support lines are not helpful because they don’t explain things in terms I understand | 1 | 2 | 3 | 4 | 5 |
| Sometimes, I think that technology systems are not designed for use by ordinary people | 1 | 2 | 3 | 4 | 5 |
| There is no such thing as a manual for a high-tech product or service that’s written in plain language | 1 | 2 | 3 | 4 | 5 |
| People are too dependent on technology to do things for them | 1 | 2 | 3 | 4 | 5 |
| Too much technology distracts people to a point that is harmful | 1 | 2 | 3 | 4 | 5 |
| Technology lowers the quality of relationships by reducing personal interaction | 1 | 2 | 3 | 4 | 5 |
| I do not feel confident doing business with a place that can only be reached online | 1 | 2 | 3 | 4 | 5 |
References
- Kostkova, P. Grand Challenges in Digital Health. Front. Public Health 2015, 3, 134. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.; Trenfield, S.J.; Pollard, T.D.; Ong, J.J.; Elbadawi, M.; McCoubrey, L.E.; Goyanes, A.; Gaisford, S.; Basit, A.W. Connected healthcare: Improving patient care using digital health technologies. Adv. Drug Deliv. Rev. 2021, 178, 113958. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Williams, N.L.; Ip, A.; Dicker, A.P. Clinical Integration of Digital Solutions in Health Care: An Overview of the Current Landscape of Digital Technologies in Cancer Care. JCO Clin. Cancer Inform. 2018, 2, 1–9. [Google Scholar] [CrossRef]
- Khurshid, Z. Digital Dentistry: Transformation of Oral Health and Dental Education with Technology. Eur. J. Dent. 2023, 17, 943–944. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Bornstein, M.M.; Jung, R.E.; Ferrari, M.; Waltimo, T.; Zitzmann, N.U. Recent Trends and Future Direction of Dental Research in the Digital Era. Int. J. Environ. Res. Public Health 2020, 17, 1987. [Google Scholar] [CrossRef]
- Gavali, N.; Chandak, A.; Waghmare, P.; Jamkhande, A.; Nisa, S.U.; Shah, P. Implementation of Digitization in Dentistry from the Year 2011 to 2021: A Bibliometric Analysis. J. Int. Clin. Dent. Res. Organ. 2023, 15, 67–74. [Google Scholar] [CrossRef]
- Yeslam, H.E.; Freifrau Von Maltzahn, N.; Nassar, H.M. Revolutionizing CAD/CAM-based restorative dental processes and materials with artificial intelligence: A concise narrative review. PeerJ 2024, 12, e17793. [Google Scholar] [CrossRef]
- Radwan, H.A.; Alsharif, A.T.; Alsharif, M.T.; Aloufi, M.R.; Alshammari, B.S. Digital technologies in dentistry in Saudi Arabia: Perceptions, practices and challenges. Digit. Health 2023, 9, 1–11. [Google Scholar] [CrossRef]
- Van Der Zande, M.M.; Gorter, R.C.; Aartman, I.H.A.; Wismeijer, D. Adoption and Use of Digital Technologies among General Dental Practitioners in the Netherlands. PLoS ONE 2015, 10, e0120725. [Google Scholar] [CrossRef]
- Hammerton, M.; Benson, T.; Sibley, A. Readiness for five digital technologies in general practice: Perceptions of staff in one part of southern England. BMJ Open Qual. 2022, 11, e001865. [Google Scholar] [CrossRef]
- Blut, M.; Wang, C. Technology readiness: A meta-analysis of conceptualizations of the construct and its impact on technology usage. J. Acad. Mark. Sci. 2020, 48, 649–669. [Google Scholar] [CrossRef]
- Schott, T.C.; Arsalan, R.; Weimer, K. Students’ perspectives on the use of digital versus conventional dental impression techniques in orthodontics. BMC Med. Educ. 2019, 19, 81. [Google Scholar] [CrossRef] [PubMed]
- Schlenz, M.A.; Schulz-Weidner, N.; Olbrich, M.; Buchmann, D.; Wöstmann, B. Insights on the digitalisation of dental practices: A cross-sectional pilot study in Hesse. Int. J. Comput. Dent. 2023, 28, 9–19. [Google Scholar] [CrossRef]
- Nassani, L.M.; Javed, K.; Amer, R.S.; Pun, M.H.J.; Abdelkarim, A.Z.; Fernandes, G.V.O. Technology Readiness Level of Robotic Technology and Artificial Intelligence in Dentistry: A Comprehensive Review. Surgeries 2024, 5, 273–287. [Google Scholar] [CrossRef]
- Schnitzler, C.; Bohnet-Joschko, S. Digital Transformation in Dentistry: A Survey on Trends and Business Implications. 2024. Available online: https://www.ssrn.com/abstract=4920815 (accessed on 8 December 2024).
- Parasuraman, A. Technology Readiness Index (Tri): A Multiple-Item Scale to Measure Readiness to Embrace New Technologies. J. Serv. Res. 2000, 2, 307–320. [Google Scholar] [CrossRef]
- Parasuraman, A.; Colby, C.L. An Updated and Streamlined Technology Readiness Index: TRI 2.0. J. Serv. Res. 2015, 18, 59–74. [Google Scholar] [CrossRef]
- Mulcahy, R.; Letheren, K.; McAndrew, R.; Glavas, C.; Russell-Bennett, R. Are households ready to engage with smart home technology? J. Mark. Manag. 2019, 35, 1370–1400. [Google Scholar] [CrossRef]
- Humbani, M.; Wiese, M. An integrated framework for the adoption and continuance intention to use mobile payment apps. Int. J. Bank Mark. 2019, 37, 646–664. [Google Scholar] [CrossRef]
- Hameed, M.A.; Counsell, S.; Swift, S. A meta-analysis of relationships between organizational characteristics and IT innovation adoption in organizations. Inf. Manag. 2012, 49, 218–232. [Google Scholar] [CrossRef]
- Morris, M.G.; Venkatesh, V. Age Differences in Technology Adoption Decisions: Implications for a Changing Work Force. Pers. Psychol. 2000, 53, 375–403. [Google Scholar] [CrossRef]
- Erbe, S. Die Lage im deutschen Gesundheitswesen. Wirtschaftsdienst 2024, 104, 580–582. [Google Scholar] [CrossRef]
- Faxvaag, A.; Reponen, J.; Hardardottir, G.A.; Vehko, T.; Viitanen, J.; Eriksen, J.; Koch, S.; Nøhr, C. Towards Accountable E-Health Policies in the Nordic Countries. In Studies in Health Technology and Informatics; Mantas, J., Hasman, A., Demiris, G., Saranto, K., Marschollek, M., Arvanitis, T.N., Ognjanović, I., Benis, A., Gallos, P., Zoulias, E., et al., Eds.; IOS Press: Amsterdam, The Netherlands, 2024; Available online: https://ebooks.iospress.nl/doi/10.3233/SHTI240413 (accessed on 22 February 2025).
- Maass, L. Digital public health in Germany. Eur. J. Public Health 2023, 33, ckad160.374. [Google Scholar] [CrossRef]
- Lelyana, N. Strategic Analysis in the Application of Digital Technology in Dental Practice. J. Soc. Interactions Humanit. 2023, 2, 253–274. [Google Scholar] [CrossRef]
- Mitchell, M.; Kan, L. Digital Technology and the Future of Health Systems. Health Syst. Reform 2019, 5, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Natasha Azzopardi Muscat on the path to an equitable and sustainable digital future for European health systems. Eur. J. Public Health 2023, 33 (Suppl. S2), ckad160.004. [CrossRef]
- Dhingra, D.; Dabas, A. Global Strategy on Digital Health. Indian Pediatr. 2020, 57, 356–358. [Google Scholar] [CrossRef]
- World Dental Federation Artificial intelligence in dentistry. Int. Dent. J. 2025, 75, 3–4. [CrossRef]
- Pfannstiel, M.A. Positioning and self-presentation of innovative organizational forms on the European healthcare market. J. Manag. Mark. Healthc. 2011, 4, 77–84. [Google Scholar] [CrossRef]
- Pourhoseingholi, M.A.; Vahedi, M.; Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench 2013, 6, 14–17. [Google Scholar]
- Bernstein, B.A. An Introduction to Sample Size and Power. J. Dev. Behav. Pediatr. 2008, 29, 516–522. [Google Scholar] [CrossRef]
- Angell, K. Open source assessment of academic library patron satisfaction. Ref. Serv. Rev. 2013, 41, 593–604. [Google Scholar] [CrossRef]
- Cole, N.S. Bias in Selection. J. Educ. Meas. 1973, 10, 237–255. [Google Scholar] [CrossRef]
- Broadbent, D.E. Word-frequency effect and response bias. Psychol. Rev. 1967, 74, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Tempelaar, D.; Rienties, B.; Nguyen, Q. Subjective data, objective data and the role of bias in predictive modelling: Lessons from a dispositional learning analytics application. PLoS ONE 2020, 15, e0233977. [Google Scholar] [CrossRef]
- Franke, T.M.; Ho, T.; Christie, C.A. The Chi-Square Test: Often Used and More Often Misinterpreted. Am. J. Eval. 2012, 33, 448–458. [Google Scholar] [CrossRef]
- Jankovic, S. Tests for Comparison of Two Groups: Student’s T-test, Mann-Whitney U-test and Chi-square Test. Int. J. Biomed. Healthc. 2022, 10, 134. [Google Scholar] [CrossRef]
- Koh, E.T.; Owen, W.L. Relationships Among Variables. In Introduction to Nutrition and Health Research; Springer: Boston, MA, USA, 2000; pp. 103–126. ISBN 978-1-4613-5535-9. [Google Scholar]
- Betensky, R.A. The p-Value Requires Context, Not a Threshold. Am. Stat. 2019, 73, 115–117. [Google Scholar] [CrossRef]
- Bentzen, H.B.; Høstmælingen, N. Balancing Protection and Free Movement of Personal Data: The New European Union General Data Protection Regulation. Ann. Intern. Med. 2019, 170, 335. [Google Scholar] [CrossRef]
- Joda, T.; Yeung, A.W.K.; Hung, K.; Zitzmann, N.U.; Bornstein, M.M. Disruptive Innovation in Dentistry: What It Is and What Could Be Next. J. Dent. Res. 2021, 100, 448–453. [Google Scholar] [CrossRef]
- Alauddin, M.S.; Baharuddin, A.S.; Mohd Ghazali, M.I. The Modern and Digital Transformation of Oral Health Care: A Mini Review. Healthcare 2021, 9, 118. [Google Scholar] [CrossRef]
- Eldh, A.C.; Sverker, A.; Bendtsen, P.; Nilsson, E. Health Care Professionals’ Experience of a Digital Tool for Patient Exchange, Anamnesis, and Triage in Primary Care: Qualitative Study. JMIR Hum. Factors 2020, 7, e21698. [Google Scholar] [CrossRef] [PubMed]
- Dioguardi, M.; Spirito, F.; Quarta, C.; Sovereto, D.; Basile, E.; Ballini, A.; Caloro, G.A.; Troiano, G.; Lo Muzio, L.; Mastrangelo, F. Guided Dental Implant Surgery: Systematic Review. J. Clin. Med. 2023, 12, 1490. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.; Zhang, K.; Zhang, J.; Shi, J.; Qiu, H.; Hou, N.; Han, F.; Kan, C.; Sun, X. Revolutionizing public health through digital health technology. Psychol. Health Med. 2025, 1–16. [Google Scholar] [CrossRef]
- Matlin, S.A.; Hanefeld, J.; Corte-Real, A.; Da Cunha, P.R.; De Gruchy, T.; Manji, K.N.; Netto, G.; Nunes, T.; Şanlıer, İ.; Takian, A.; et al. Digital solutions for migrant and refugee health: A framework for analysis and action. Lancet Reg. Health Eur. 2025, 50, 101190. [Google Scholar] [CrossRef]
- LeRouge, C.; Van Slyke, C.; Seale, D.; Wright, K. Baby Boomers’ Adoption of Consumer Health Technologies: Survey on Readiness and Barriers. J. Med. Internet Res. 2014, 16, e200. [Google Scholar] [CrossRef]
- Meyer, J. Older Workers and the Adoption of New Technologies. SSRN Journal. 2007. Available online: http://www.ssrn.com/abstract=1010288 (accessed on 20 September 2024).
- Nassani, L.M.; Bencharit, S.; Schumacher, F.; Lu, W.-E.; Resende, R.; Fernandes, G.V.O. The Impact of Technology Teaching in the Dental Predoctoral Curriculum on Students’ Perception of Digital Dentistry. Dent. J. 2024, 12, 75. [Google Scholar] [CrossRef]
- Omrani, N.; Rejeb, N.; Maalaoui, A.; Dabić, M.; Kraus, S. Drivers of Digital Transformation in SMEs. IEEE Trans. Eng. Manag. 2024, 71, 5030–5043. [Google Scholar] [CrossRef]
- Jafari-Sadeghi, V.; Garcia-Perez, A.; Candelo, E.; Couturier, J. Exploring the impact of digital transformation on technology entrepreneurship and technological market expansion: The role of technology readiness, exploration and exploitation. J. Bus. Res. 2021, 124, 100–111. [Google Scholar] [CrossRef]
- Damanpour, F. Organizational Size and Innovation. Organ. Stud. 1992, 13, 375–402. [Google Scholar] [CrossRef]
- Giancotti, M.; Guglielmo, A.; Mauro, M. Efficiency and optimal size of hospitals: Results of a systematic search. PLoS ONE 2017, 12, e0174533. [Google Scholar] [CrossRef]
- Vanberkel, P.T.; Boucherie, R.J.; Hans, E.W.; Hurink, J.L.; Litvak, N. Efficiency evaluation for pooling resources in health care. OR Spectr. 2012, 34, 371–390. [Google Scholar] [CrossRef]
- Pettigrew, L.M.; Kumpunen, S.; Rosen, R.; Posaner, R.; Mays, N. Lessons for ‘large-scale’ general practice provider organisations in England from other inter-organisational healthcare collaborations. Health Policy 2019, 123, 51–61. [Google Scholar] [CrossRef]
- Orser, B.; Riding, A.; Li, Y. Technology adoption and gender-inclusive entrepreneurship education and training. Int. J. Gend. Entrep. 2019, 11, 273–298. [Google Scholar] [CrossRef]
- Orser, B.J.; Riding, A. The influence of gender on the adoption of technology among SMEs. Int. J. Entrep. Small Bus. 2018, 33, 514. [Google Scholar] [CrossRef]
- Chi, Y. Multivariate methods. WIREs Comput. Stats 2012, 4, 35–47. [Google Scholar] [CrossRef]
- Cirillo, V.; Fanti, L.; Mina, A.; Ricci, A. The adoption of digital technologies: Investment, skills, work organisation. Struct. Change Econ. Dyn. 2023, 66, 89–105. [Google Scholar] [CrossRef]
- Pedota, M.; Grilli, L.; Piscitello, L. Technology adoption and upskilling in the wake of Industry 4.0. Technol. Forecast. Soc. Change 2023, 187, 122085. [Google Scholar] [CrossRef]
- Kohli, R.; Melville, N.P. Digital innovation: Review and synthesis. Inf. Syst. J. 2019, 29, 200–223. [Google Scholar] [CrossRef]
- Tretyak, V.; Lyakina, M.; Volkova, E. The ways of business digitalization in global corporations. SHS Web Conf. 2021, 92, 05027. [Google Scholar] [CrossRef]
- Spector, P.E. Do Not Cross Me: Optimizing the Use of Cross-Sectional Designs. J. Bus Psychol. 2019, 34, 125–137. [Google Scholar] [CrossRef]


| Gender | Age (Mean) | Age (Median) | SD |
|---|---|---|---|
| female | 37.7 | 35 | (±) 10.18 |
| male | 45.4 | 46 | (±) 12.97 |
| Correlation–Analysis | Age | Clinic Type | Number of Employees | Clinic Location | Gender | Professional Development | Number of Equipment |
|---|---|---|---|---|---|---|---|
| TRI-Score | −0.338i (p < 0.001) | 123.406 (111) ii (p = 0.198) | 0.316i (p < 0.001) | 116.935 (111) ii (p = 0.331) | 40.832 (37) ii (p = 0.306) | 167.785 (127) ii (p = 0.127) | 0.384i (p < 0.001) |
| Correlation–Analysis | Age | Clinic Type | Number of Employees | Clinic Location | Gender | Professional Development |
|---|---|---|---|---|---|---|
| Number of Equipment | −0.068 i (p = 0.338) | 121.391 (57)ii (p < 0.001) | 0.388i (p < 0.001) | 67.938 (57) ii (p = 0.152) | 22.130 (57) ii (p = 0.278) | 102.780 (76)ii (p = 0.022) |
| Clinic Type | Average Number of Equipment/Medians |
|---|---|
| Solo clinic | 4.96/3 |
| Group clinic | 7.27/7 |
| Multi-dentist (MVZ) | 11.2/11 |
| University clinic | 8.03/8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schnitzler, C.; Bohnet-Joschko, S. Technology Readiness Drives Digital Adoption in Dentistry: Insights from a Cross-Sectional Study. Healthcare 2025, 13, 1155. https://doi.org/10.3390/healthcare13101155
Schnitzler C, Bohnet-Joschko S. Technology Readiness Drives Digital Adoption in Dentistry: Insights from a Cross-Sectional Study. Healthcare. 2025; 13(10):1155. https://doi.org/10.3390/healthcare13101155
Chicago/Turabian StyleSchnitzler, Christian, and Sabine Bohnet-Joschko. 2025. "Technology Readiness Drives Digital Adoption in Dentistry: Insights from a Cross-Sectional Study" Healthcare 13, no. 10: 1155. https://doi.org/10.3390/healthcare13101155
APA StyleSchnitzler, C., & Bohnet-Joschko, S. (2025). Technology Readiness Drives Digital Adoption in Dentistry: Insights from a Cross-Sectional Study. Healthcare, 13(10), 1155. https://doi.org/10.3390/healthcare13101155





