Injury Risk and Overall Well-Being During the Menstrual Cycle in Elite Adolescent Team Sports Athletes
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Procedures
2.4. Data Collection
2.4.1. Menstrual Cycle Phase Identification
2.4.2. Injury Incidence and Severity
2.4.3. Wellness Questionnaire
2.5. Data Analysis
3. Results
3.1. Participants Description
3.2. Wellness Data
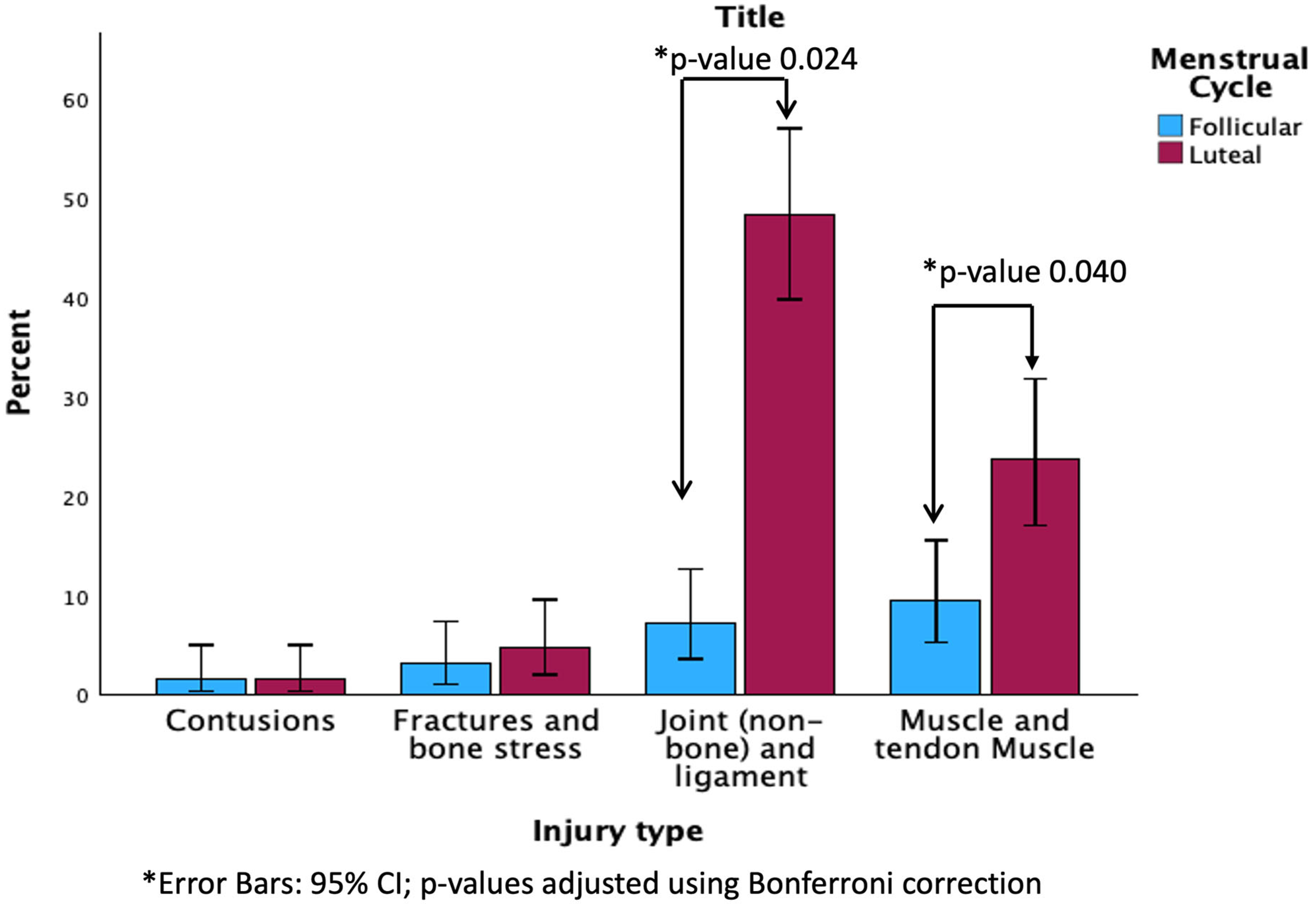
3.3. Injury Data
4. Discussion
4.1. Menstrual Cycle Characteristics in Adolescents
4.2. Wellness and MC
4.3. Injuries and MC
4.4. Limitations, Strengths, and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Forsyth, J.R.C. The Exercising Female Science and Its Application; Routledge: London, UK, 2018. [Google Scholar]
- Costello, J.T.; Bieuzen, F.; Bleakley, C.M. Where Are All the Female Participants in Sports and Exercise Medicine Research? Eur. J. Sport. Sci. 2014, 14, 847–851. [Google Scholar] [CrossRef] [PubMed]
- Oosthuyse, T.; Bosch, A.N. The Effect of the Menstrual Cycle on Exercise Metabolism. Sports Med. 2010, 40, 207–227. [Google Scholar] [CrossRef] [PubMed]
- de Jonge, X.J.; Thompson, B.; Ahreum, H.A.N. Methodological Recommendations for Menstrual Cycle Research in Sports and Exercise. Med. Sci. Sports Exerc. 2019, 51, 2610–2617. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K. Which Type of Exercise Keeps You Young? Curr. Opin. Clin. Nutr. Metab. Care 2019, 22, 167–173. [Google Scholar] [CrossRef]
- Jayanthi, N.; Pinkham, C.; Dugas, L.; Patrick, B.; Labella, C. Sports Specialization in Young Athletes: Evidence-Based Recommendations. Sports Health 2013, 5, 251–257. [Google Scholar] [CrossRef]
- Blagrove, R.C.; Bruinvels, G.; Read, P. Early Sport Specialization and Intensive Training in Adolescent Female Athletes: Risks and Recommendations. Strength. Cond. J. 2017, 39, 14–23. [Google Scholar] [CrossRef]
- Carmichael, M.A.; Thomson, R.L.; Moran, L.J.; Wycherley, T.P. The Impact of Menstrual Cycle Phase on Athletes’ Performance: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 1667. [Google Scholar] [CrossRef]
- Bloemers, F.; Collard, D.; Paw, M.C.A.; Van Mechelen, W.; Twisk, J.; Verhagen, E. Physical Inactivity Is a Risk Factor for Physical Activity-Related Injuries in Children. Br. J. Sports Med. 2012, 46, 669–674. [Google Scholar] [CrossRef]
- Kerkhoffs, G.M.M.J.; Servien, E.; Dunn, W.; Dahm, D.; Bramer, J.A.M.; Haverkamp, D. The Influence of Obesity on the Complication Rate and Outcome of Total Knee Arthroplasty. J. Bone Jt. Surg. 2012, 94, 1839–1844. [Google Scholar] [CrossRef]
- Armour, M.; Parry, K.A.; Steel, K.; Smith, C.A. Australian Female Athlete Perceptions of the Challenges Associated with Training and Competing When Menstrual Symptoms Are Present. Int. J. Sports Sci. Coach. 2020, 15, 316–323. [Google Scholar] [CrossRef]
- Findlay, R.J.; MacRae, E.H.R.; Whyte, I.Y.; Easton, C.; Forrest, L.J. How the Menstrual Cycle and Menstruation Affect Sporting Performance: Experiences and Perceptions of Elite Female Rugby Players. Br. J. Sports Med. 2020, 54, 1108–1113. [Google Scholar] [CrossRef] [PubMed]
- Herzberg, S.D.; Motu’apuaka, M.L.; Lambert, W.; Fu, R.; Brady, J.; Guise, J.-M. The Effect of Menstrual Cycle and Contraceptives on ACL Injuries and Laxity: A Systematic Review and Meta-Analysis. Orthop. J. Sports Med. 2017, 5. [Google Scholar] [CrossRef] [PubMed]
- Chidi-Ogbolu, N.; Baar, K. Effect of Estrogen on Musculoskeletal Performance and Injury Risk. Front Physiol. 2019, 10, 1834. [Google Scholar] [CrossRef]
- Harrison, C.B.; Gill, N.D.; Kinugasa, T.; Kilding, A.E. Development of Aerobic Fitness in Young Team Sport Athletes. Sports Med. 2015, 45, 969–983. [Google Scholar] [CrossRef]
- Romero-Parra, N.; Cupeiro, R.; Alfaro-Magallanes, V.M.; Rael, B.; Rubio-Arias, J.Á.; Peinado, A.B.; Benito, P.J.; on behalf of the IronFEMME Study Group. Exercise-Induced Muscle Damage During the Menstrual Cycle: A Systematic Review and Meta-Analysis. J. Strength Cond. Res. 2020, 35, 549–561. [Google Scholar] [CrossRef]
- Hewett, T.E.; Zazulak, B.T.; Myer, G.D. Effects of the Menstrual Cycle on Anterior Cruciate Ligament Injury Risk. Am. J. Sports Med. 2007, 35, 659–668. [Google Scholar] [CrossRef]
- Balachandar, V. Effects of the Menstrual Cycle on Lower-Limb Biomechanics, Neuromuscular Control, and Anterior Cruciate Ligament Injury Risk: A Systematic Review. Muscle Ligaments Tendons J. 2017, 7, 136. [Google Scholar] [CrossRef]
- Slauterbeck, J.R.; Fuzie, S.F.; Smith, M.P.; Clark, R.J.; Tom Xu, K.; Starch, D.W.; Hardy, D.M. By the National Athletic Trainers; Association, Inc.: Des Moines, IA, USA, 2002; Volume 37. [Google Scholar]
- Myklebust, G.; Mæhlum, S.; Holm, I.; Bahr, R. A Prospective Cohort Study of Anterior Cruciate Ligament Injuries in Elite Norwegian Team Handball. Scand. J. Med. Sci. Sports 1998, 8, 149–153. [Google Scholar] [CrossRef]
- Lago-Fuentes, C.; Padrón-Cabo, A.; Fernández-Villarino, M.; Mecías-Calvo, M.; Muñoz-Pérez, I.; García-Pinillos, F.; Rey, E. Follicular Phase of Menstrual Cycle Is Related to Higher Tendency to Suffer from Severe Injuries among Elite Female Futsal Players. Phys. Ther. Sport. 2021, 52, 90–96. [Google Scholar] [CrossRef]
- Bull, J.R.; Rowland, S.P.; Scherwitzl, E.B.; Scherwitzl, R.; Danielsson, K.G.; Harper, J. Real-World Menstrual Cycle Characteristics of More than 600,000 Menstrual Cycles. NPJ Digit. Med. 2019, 2, 83. [Google Scholar] [CrossRef]
- Mumford, S.L.; Steiner, A.Z.; Pollack, A.Z.; Perkins, N.J.; Filiberto, A.C.; Albert, P.S.; Mattison, D.R.; Wactawski-Wende, J.; Schisterman, E.F. The Utility of Menstrual Cycle Length as an Indicator of Cumulative Hormonal Exposure. J. Clin. Endocrinol. Metab. 2012, 97, E1871–E1879. [Google Scholar] [CrossRef] [PubMed]
- Hillard, P.J.A. Menstruation in Adolescents: What Do We Know and What Do We Do with the Information. J. Pediatr. Adolesc. Gynecol. 2014, 27, 309–319. [Google Scholar] [CrossRef] [PubMed]
- de Paula Oliveira, T.; Bruinvels, G.; Pedlar, C.R.; Moore, B.; Newell, J. Modelling Menstrual Cycle Length in Athletes Using State-Space Models. Sci. Rep. 2021, 11, 16972. [Google Scholar] [CrossRef] [PubMed]
- Rae, K.; Orchard, J. The Orchard Sports Injury Classification System (OSICS) Version 10. Clin. J. Sport. Med. 2007, 17, 201–204. [Google Scholar] [CrossRef]
- Fuller, C.W.; Ekstrand, J.; Junge, A.; Andersen, T.E.; Bahr, R.; Dvorak, J.; Hägglund, M.; McCrory, P.; Meeuwisse, W.H. Consensus Statement on Injury Definitions and Data Collection Procedures in Studies of Football (Soccer) Injuries. Scand. J. Med. Sci. Sports 2006, 16, 83–92. [Google Scholar] [CrossRef]
- Hooper, S.L.; Mackinnon, L.T.; Howard, A.; Gordon, R.D.; Bachmann, A.W. Markers for Monitoring Overtraining and Recovery. Med. Sci. Sports Exerc. 1995, 27, 106–112. [Google Scholar] [CrossRef]
- Carmichael, M.A.; Thomson, R.L.; Moran, L.J.; Dunstan, J.R.; Nelson, M.J.; Mathai, M.L.; Wycherley, T.P. A Pilot Study on the Impact of Menstrual Cycle Phase on Elite Australian Football Athletes. Int. J. Environ. Res. Public Health 2021, 18, 9591. [Google Scholar] [CrossRef]
- Hrozanova, M.; Klöckner, C.A.; Sandbakk, Ø.; Pallesen, S.; Moen, F. Sex Differences in Sleep and Influence of the Menstrual Cycle on Women’s Sleep in Junior Endurance Athletes. PLoS ONE 2021, 16, e0253376. [Google Scholar] [CrossRef]
- Romans, S.E.; Kreindler, D.; Einstein, G.; Laredo, S.; Petrovic, M.J.; Stanley, J. Sleep Quality and the Menstrual Cycle. Sleep. Med. 2015, 16, 489–495. [Google Scholar] [CrossRef]
- Baker, F.C.; Lee, K.A. Menstrual Cycle Effects on Sleep. Sleep. Med. Clin. 2022, 17, 283–294. [Google Scholar] [CrossRef]
- Driver, H.S.; Werth, E.; Dijk, D.-J.; Borbély, A.A. The Menstrual Cycle Effects on Sleep. Sleep Med. Clin. 2008, 3, 1–11. [Google Scholar] [CrossRef]
- Bruinvels, G.; Burden, R.J.; McGregor, A.J.; Ackerman, K.E.; Dooley, M.; Richards, T.; Pedlar, C. Sport, Exercise and the Menstrual Cycle: Where Is the Research? Br. J. Sports Med. 2017, 51, 487–488. [Google Scholar] [CrossRef] [PubMed]
- Bruinvels, G.; Goldsmith, E.; Blagrove, R.; Simpkin, A.; Lewis, N.; Morton, K.; Suppiah, A.; Rogers, J.P.; Ackerman, K.E.; Newell, J.; et al. Prevalence and frequency of menstrual cycle symptoms are associated with availability to train and compete: A study of 6812 exercising women recruited using the Strava exercise app. Br. J. Sports Med. 2021, 55, 438–443. [Google Scholar] [CrossRef]
- Barlow, A.; Blodgett, J.M.; Williams, S.; Pedlar, C.R.; Bruinvels, G. Injury Incidence, Severity and Type across the Menstrual Cycle in Elite Female Professional Footballers: A Prospective Three Season Cohort Study. Med. Sci. Sports Exerc. 2024, 56, 1151–1158. [Google Scholar] [CrossRef]
- Martin, D.; Timmins, K.; Cowie, C.; Alty, J.; Mehta, R.; Tang, A.; Varley, I. Injury Incidence Across the Menstrual Cycle in International Footballers. Front. Sports Act. Living 2021, 3, 616999. [Google Scholar] [CrossRef]
| N | Mean (SD) | |
|---|---|---|
| Age (years) | 59 | 15.91 (1.23) |
| Years post PHV | 59 | 3.76 (0.99) |
| Body mass (kg) | 59 | 68.12 (9.23) |
| Height (m) | 59 | 1.76 (0.08) |
| BMI (kg·m−2) | 59 | 21.72 (2.06) |
| Training experience (years) | 59 | 7.17 (2.12) |
| Menstruation days | 59 | 4.56 (0.93) |
| Cycle length | 59 | 28.12 (3.21) |
| Contraceptives (Yes) | 2 | 3.30% |
| Basketball | 23 | 38.90% |
| Handball | 21 | 35.60% |
| Volleyball | 15 | 25.50% |
| N | Mean (SD) | CI 95% | p-Value * | Post Hoc Comparisons ** | Effect Size (Eta-Squared) | ||
|---|---|---|---|---|---|---|---|
| Sleep | Phase 1. Menstruation | 59 | 2.24 (0.763) | (2.02–2.45) | 0.001 | 1 vs. 3.4; 2 vs. 3.4; | |
| Phase 2. Late follicular | 59 | 2.27 (0.784) | (2.04–2.49) | ||||
| Phase 3. Early luteal | 59 | 3.07 (0.543) | (2.89–3.24) | 0.351 (0.237; 0.437) | |||
| Phase 4. Pre-menstrual | 59 | 3.32 (0.518) | (3.18–3.47) | ||||
| Total | 59 | 2.7 (0.825) | (2.58–2.82) | ||||
| Stress | Phase 1. Menstruation | 59 | 2.53 (1.069) | (2.22–2.83) | 0.755 | Non-Significant | |
| Phase 2. Late follicular | 59 | 2.54 (1.057) | (2.24–2.84) | ||||
| Phase 3. Early luteal | 59 | 2.42 (1.022) | (2.02–2.81) | 0.002 (0.00; 0.006) | |||
| Phase 4. Pre-menstrual | 59 | 2.5 (1.049) | (2.21–2.8) | ||||
| Total | 59 | 2.5 (1.086) | (2.35–2.66) | ||||
| Fatigue | Phase 1. Menstruation | 59 | 2.79 (1.043) | (2.5–3.09) | 0.001 | 1 vs. 3.4; 2 vs. 3.4; | |
| Phase 2. Late follicular | 59 | 2.8 (1.033) | (2.51–3.1) | ||||
| Phase 3. Early luteal | 59 | 3.33 (0.718) | (3.1–3.57) | 0.80 (0.14; 0.251) | |||
| Phase 4. Pre-menstrual | 59 | 3.31 (0.682) | (3.11–3.5) | ||||
| Total | 59 | 3.04 (0.925) | (2.91–3.18) | ||||
| Pain | Phase 1. Menstruation | 59 | 2.16 (0.925) | (1.9–2.43) | 0.825 | Non-Significant | |
| Phase 2. Late follicular | 59 | 2.19 (0.974) | (1.92–2.47) | ||||
| Phase 3. Early luteal | 59 | 2.2 (1.037) | (1.87–2.54) | 0.001 (0.00; 0.005) | |||
| Phase 4. Pre-menstrual | 59 | 2.17 (0.915) | (1.91–2.43) | ||||
| Total | 59 | 2.18 (0.952) | (2.04–2.32) |
| N | % | ||
|---|---|---|---|
| Severity | Slight (0–1 days) | 33 | 26.40% |
| Mild (4–7 days) | 23 | 18.40% | |
| Minimal (2–3 days) | 21 | 16.80% | |
| Moderate (8–28 days) | 28 | 22.40% | |
| Severe (>28 days) | 20 | 16.00% | |
| Injury localization | Head and neck | 6 | 4.69% |
| Lower limbs | 84 | 65.63% | |
| Trunk | 10 | 7.81% | |
| Upper limbs | 28 | 21.88% | |
| Side | Both | 15 | 12.30% |
| Right | 61 | 50.00% | |
| Left | 46 | 37.70% | |
| Injury type | Contusions | 4 | 3.13% |
| Fractures and bone stress | 10 | 7.81% | |
| Joint (non-bone) and ligament | 72 | 55.47% | |
| Muscle and tendon Muscle | 42 | 32.81% | |
| Previous injury | No | 98 | 79.03% |
| Si | 26 | 20.97% | |
| Recurrence level | Delayed recurrence (>12 months) | 1 | 4.76% |
| Early (<2 months) | 13 | 61.90% | |
| Late recurrence (2–12 months) | 7 | 33.33% | |
| Cause | Overuse | 51 | 43.22% |
| Trauma | 67 | 56.78% | |
| Injury circumstances | Others | 3 | 2.50% |
| Practice | 84 | 70.00% | |
| Match | 33 | 27.50% | |
| Injury mechanism | Ball contact | 3 | 2.38% |
| Object contact | 5 | 3.97% | |
| Direct contact | 18 | 14.29% | |
| Indirect contact | 19 | 15.08% | |
| Non-contact | 81 | 64.29% |
| Contusions | Fractures and Bone Stress | Joint (Non-Bone) and Ligament | Muscle and Tendon Muscle | p-Value * | |
|---|---|---|---|---|---|
| Phase 1. Menstruation | 0 (0.0%) | 3 (30.0%) | 4 (5.7%) | 5 (11.9%) | 0.064 |
| Phase 2. Late follicular | 2 (50.0%) | 1 (10.0%) | 5 (7.1%) | 7 (16.7%) | |
| Phase 3. Early luteal | 2 (50.0%) | 4 (40.0%) | 31 (44.3%) | 17 (40.5%) | |
| Phase 4. Pre-menstrual | 0 (0.0%) | 2 (20.0%) | 30 (42.9%) | 13 (31.0%) | |
| Total | 4 (100%) | 10 (100%) | 70 (100%) | 42 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fort-Vanmeerhaeghe, A.; Pujol-Marzo, M.; Milà, R.; Campos, B.; Nevot-Casas, O.; Casadevall-Sayeras, P.; Peña, J. Injury Risk and Overall Well-Being During the Menstrual Cycle in Elite Adolescent Team Sports Athletes. Healthcare 2025, 13, 1154. https://doi.org/10.3390/healthcare13101154
Fort-Vanmeerhaeghe A, Pujol-Marzo M, Milà R, Campos B, Nevot-Casas O, Casadevall-Sayeras P, Peña J. Injury Risk and Overall Well-Being During the Menstrual Cycle in Elite Adolescent Team Sports Athletes. Healthcare. 2025; 13(10):1154. https://doi.org/10.3390/healthcare13101154
Chicago/Turabian StyleFort-Vanmeerhaeghe, Azahara, Montse Pujol-Marzo, Rai Milà, Berta Campos, Oriol Nevot-Casas, Pep Casadevall-Sayeras, and Javier Peña. 2025. "Injury Risk and Overall Well-Being During the Menstrual Cycle in Elite Adolescent Team Sports Athletes" Healthcare 13, no. 10: 1154. https://doi.org/10.3390/healthcare13101154
APA StyleFort-Vanmeerhaeghe, A., Pujol-Marzo, M., Milà, R., Campos, B., Nevot-Casas, O., Casadevall-Sayeras, P., & Peña, J. (2025). Injury Risk and Overall Well-Being During the Menstrual Cycle in Elite Adolescent Team Sports Athletes. Healthcare, 13(10), 1154. https://doi.org/10.3390/healthcare13101154







