Abstract
Background: Acupotomy is a modern acupuncture technique using a knife-shaped needle for pain treatment, combining traditional and anatomical knowledge. This study evaluates the diversity and safety of acupotomy procedures for lumbar spine disorders to aid in developing safety and reporting guidelines for clinical studies. Methods: A literature search was conducted on 30 October 2023 in PubMed, five Korean databases, and relevant journals with keywords like ‘low back pain’ and ‘acupotomy’. The search included clinical trial articles in English or Korean on lumbar spinal disorders treated by acupotomy. We reviewed 22 clinical studies involving 731 Korean patients published from 2008 to 2023. Data extracted included disease types, diagnosis methods, treatment specifics, needling factors, anesthesia, clinical outcomes, and safety reports. Results: Most studies focused on lumbar herniated discs and stenosis, with acupotomy performed on damaged tissue sites. Treatment frequency varied, and outcomes included pain scales and imaging assessments. Reporting gaps were found in needle size, insertion depth, and anesthesia status. Safety measures were poorly documented, with only six studies addressing safety and two reporting adverse events. Conclusions: There is a critical need for standardized clinical and reporting guidelines for acupotomy, akin to acupuncture’s existing guidelines, to enhance research consistency and quality. Future studies should develop guidelines covering target tissues, needle details, techniques, anesthesia, and adverse effects to improve acupotomy safety and effectiveness.
1. Introduction
Acupotomy is an innovative acupuncture technique that integrates traditional acupuncture practices with modern anatomical knowledge, thus not necessarily adhering to traditional medical principles such as the concept of acupoints and meridians. This therapy involves a needle with a knife-shaped tip that is wider and thicker than a fine acupuncture needle to dissect, cut, or detach adhesions in soft tissues (Figure 1), and primarily treats chronic pain disorders resulting from tissue damage [1]. This technique stems from a long, thick needle resembling a spear, one of the ‘nine classical needles’ described in the ‘Huangdi Neijing’. Specifically, it is designed for lancing abscesses, treating carbuncles and furuncles, and performing bloodletting. In 1976, Hanzhang Zhu modernized this procedure using an acupotomy needle consisting of a handle, needle body, and blade and transformed it into the technique used today [2]. The procedure is relatively simpler than typical surgical procedures, causes minimal tissue damage, and carries a lower risk of infection compared to open surgery. The technique is straightforward, quick, and less painful than traditional surgery, providing strong stimulation to muscles, tendons, and ligaments, and easily separating adhered soft tissues. Acupotomy has recently been employed in China and the Republic of Korea to address musculoskeletal disorders, especially those resulting from cumulative damage like disc herniation [3], neck pain [4], and knee osteoarthritis [5]. Minimally invasive techniques that share clinical indications with acupotomy include Intra-Muscular Stimulation (IMS), which relieves chronic pain by stimulating deep muscle layers [6], and prolotherapy, which promotes soft tissue regeneration by injecting proliferative solutions into damaged ligaments and tendons [7]. Notably, this technique has been predominantly applied to the lumbar and cervical regions.
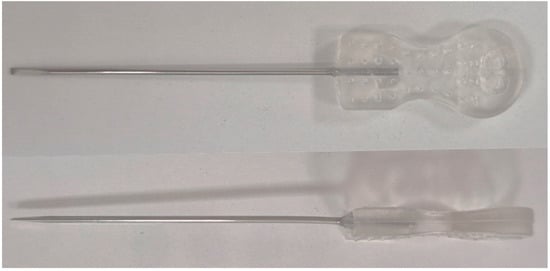
Figure 1.
Front and side view of acupotomy needle (Dongbang medical, Seongnam, Republic of Korea; needle size 1.0 × 50). The acupotomy needle features a sharp, knife-like tip at the end, which gives it a unique shape compared to a standard acupuncture needle.
Acupotomy delivers a more intense level of stimulation than conventional acupuncture and demonstrates its efficacy in the dissection of soft tissue adhesions [8]. Compared to a surgical scalpel, it is less invasive and presents a lower risk of complications, making it a clinically valuable therapeutic modality. One of its key advantages is its ability to achieve significant therapeutic effects through minimally invasive access to pain-generating structures. While acupotomy is traditionally based on the framework of meridians and acupoints, in clinical practice, it is commonly applied to areas identified through the practitioner’s palpatory diagnosis. These areas often correspond to Ashi points or extra-meridian points, targeting muscles, ligaments, and other soft tissue structures associated with pain. Acupotomy is usually applied to these anatomical targets either to release adhesions or to stimulate dysfunctional tissues. The procedure is generally administered repeatedly over several sessions, rather than as a single treatment, depending on the patient’s condition and disease characteristics. Prior to treatment, strict sterilization and adherence to clean needling technique are essential. Post-treatment care includes compression and antiseptic management of the puncture site to prevent bleeding, hematoma, and infection. Local adverse effects such as bruising, pain, and paresthesia may occur, and in rare cases, systemic symptoms like dizziness or fatigue may also be observed.
However, like other invasive medical procedures, the acupotomy treatment process should adhere to strict guidelines to prevent adverse effects, minimize unnecessary tissue damage, reduce painful sensations in patients, and lower the risk of infection. Moreover, the specifications of the needle used (e.g., length, diameter, and width and thickness of the blade part) along with the stimulation parameters (e.g., the depth of needle insertion, the number of stimulation sites, and the number of needle manipulations including insertions and removals) significantly affect the intensity of the stimulation. The dose–response relationship is one of the most important yet challenging issues that remains unresolved in acupuncture research [9], and it is also a concern in the context of acupotomy. For example, for acupuncture treatment, various safety guidelines have been distributed and Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guidelines were designed to improve the completeness of reporting in clinical trials involving acupuncture [10]. As the acupotomy procedure can be more invasive than fine needle acupuncture, it requires its own safety and reporting guidelines. The lack of specific guidelines for reporting the diversity and quality of acupotomy procedures, as well as adverse events, creates a gap in research. Further research is needed to understand the diversity of acupotomy procedure reporting and to effectively report and investigate the safety of these procedures and their potential adverse effects.
This study aims to (1) assess the diversity of and safety reporting in acupotomy therapy procedures for lumbar spine disorders in South Korea, and to (2) compile essential information that will support the development of safety and reporting guidelines for clinical studies involving acupotomy treatments in the near future.
2. Methods
To analyze clinical trials including acupotomy treatment for lumbar spine disorders in South Korea, this study reviewed articles and organized and discussed the publication year, study participants, acupotomy treatment details, and clinical outcome assessment tools. We conducted a systematic search strategy following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to identify relevant studies. The literature search, conducted on 30 October 2023, utilized academic research information services and PubMed with the search string: ‘(low back pain [Title/Abstract] OR lower back pain [Title/Abstract] OR lumbar pain [Title/Abstract] OR lumbago [Title/Abstract]) AND (acupotomy [Title/Abstract] OR acupotomology [Title/Abstract] OR “needle knife” [Title/Abstract] OR knife [Title/Abstract] OR scalpel [Title/Abstract] OR miniscalpel [Title/Abstract] OR “stiletto needle” [Title/Abstract] OR “sword-like needle” [Title/Abstract])’. Additionally, articles were searched using related keywords in the Journal of Korean Medical Society of Acupotomology and Korean Journal of Traditional Knowledge as well as in five Korean databases [KoreaMed, Research Information Service System (RISS), Korean Studies Information Service System (KISS), Database Periodical Information Academic (DBpia), and Oriental Medicine Advanced Searching Integrated System (OASIS)]. We also conducted a hand search of the citations in the selected papers. From those identified through electronic and manual searches, articles were excluded if they were duplicates, unrelated to lumbar spinal disorders, were not original clinical studies (e.g., reviews, meta-analyses, or protocols), or were not written in English or Korean. Two reviewers (YB and ES) independently screened articles based on titles, abstracts, and full texts for eligibility according to the inclusion criteria. Data were independently extracted from selected articles by the two reviewers and cross-checked for accuracy. Disagreements were resolved through discussions between the two reviewers and, if necessary, with a third reviewer (ISL), a doctor of Korean Medicine specializing in meridians and acupoints.
3. Results
3.1. Results of the Search
A flowchart based on the PRISMA guidelines is shown in Figure 2. The search retrieved 289 records, and 224 records were identified after removing duplicates. When reviewing the titles and abstracts, all but 22 articles were excluded from further full-text assessment due to various reasons: not written in English or Korean (n = 8); not original clinical studies (n = 41); unrelated to lumbar spine disorders (n = 153). Ultimately, we included 22 studies in the review.
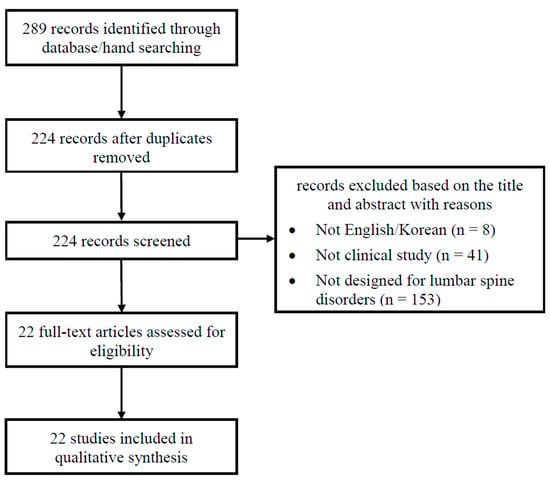
Figure 2.
Flow diagram of literature search.
3.2. Participants in Included Clinical Trials
The included studies, published between 2008 and 2023, comprised 22 clinical studies: 2 randomized controlled trials, 2 controlled clinical trials, 1 clinical trial, 7 case series, and 10 case reports, involving a total of 731 patients with lumbar spine disorders. The majority of the studies, seventeen in total, involved fewer than 10 patients each. Fifteen studies included patients with lumbar herniated intervertebral discs (HIVD) [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25]. Two studies included patients with lumbar stenosis [26,27], and one study each included patients with fractures and sprains [28], ankylosing spondylitis [29], acute myelitis [30], and abnormal spinal curvature [31]. Additionally, one case series encompassed various conditions [32] (Table 1).

Table 1.
Characteristics of clinical studies using acupotomy for lumbar spine disorders in South Korea.
Four papers included control groups: Yun et al. [14] compared the effects of combining acupotomy with acupuncture to those in an acupuncture-only group, Park et al. [13] assessed the effects of combining acupotomy with spin decompression against those in an acupotomy-only group, and Wang et al. [16] examined the effects of combining acupotomy with herbal medicine in contrast to an herbal medicine-only group. Sung et al. [22] evaluated the effects of acupotomy compared to an acupuncture group.
3.3. Reporting of Treatment Procedures
3.3.1. Diagnosis
Out of 22 studies, 21 used imaging techniques such as magnetic resonance imaging (MRI), computed tomography (CT), and X-ray to diagnose lumbar spine diseases. MRI was also employed to evaluate treatment responses [11,19,20,25], for example, by measuring the volume of extruded discs.
3.3.2. Acupotomy Treatment Procedures
In the majority of studies (21 out of 22), detailed descriptions of the acupotomy treatment procedures and infection prevention measures were provided. In most cases, the patient’s position, disinfection of treatment sites, methods of penetration, depth of needle insertion, and methods of stimulation were described (Supplementary Table S1). Acupotomy was primarily performed on damaged tissue sites, with the frequency and number of treatments varying from 1 to 127 times. In 10 studies [13,14,15,16,17,18,24,27,30,31], acupotomy needles penetrated acupoints, and in eight studies [12,15,18,23,24,25,28,31], they targeted Ashi or tender points.
In 17 out of 22 studies (77.27%), the number of acupotomy needles inserted at each treatment session was not reported [11,15,16,17,19,20,22,23,24,25,26,27,28,30,31,32]. Regarding the size of the acupotomy needle, only five studies (22.73%) [13,14,21,24,26] provided complete details on all three critical dimensions: length, diameter, and width of the needle’s knife portion. The depth of needle insertion was reported in six studies (27.27%), ranging from 0.5 to 3 cm [14,18,20,27,28,29]. Only six studies (27.27%) provided details on anesthesia. One study did not administer anesthesia to the patients [12], three studies used lidocaine [18,26,29], and two studies applied a cream containing lidocaine and prilocaine [22,27].
3.4. Reporting Clinical Outcomes, Safety, and Adverse Events
The most commonly reported clinical outcomes included the pain numerical rating scale (NRS) in 14 papers, Oswestry Disability Index (ODI) in 13 papers, range of movement (ROM) in 10 papers, visual analogue scale (VAS) in 6 papers, and MRI in 4 papers. Notably, more recent studies have increasingly utilized diagnostic imaging tools such as MRI to monitor treatment effects (e.g., extruded disc volume). In most studies, it was confirmed that the intensity of pain or ROM improved after acupuncture treatment. In studies that used MRI to confirm improvement in diseases or symptoms due to acupuncture, it was often simply stated as ‘improvement was also confirmed radiologically on L-spine MRI examination’ [11] or ‘the improvement in radiology’ [19] without detailing which specific areas showed improvement or how they improved radiologically. Alternatively, it was stated as ‘the volume of extruded disc in MRI images was reduced’ [20] or ‘substantial resorption of the respective herniated disc’ [25].
Safety measures were reported in only six of the 22 papers [13,16,18,22,23,27], and these frequently lacked specific and clear indicators to confirm safety. Safety-related measures reported included methods for preventing infection, monitoring pain and other sensations, observing erythema and bleeding, and conducting blood tests. One study used a surgical safety checklist and conducted blood tests when adverse events occurred [18], suggesting that a specified safety checklist for acupotomy treatment should be developed in the near future. Out of the 22 papers reviewed, only two papers reported adverse events [12,20]. For example, Jang et al. [12] reported that the patient experienced a moderate level of discomfort and a slight increase in pain, which were relieved in a day. Park et al. [20] reported that the patient suffered from pain at the treatment sites, but without any restrictions in daily life. Four papers noted no adverse events [18,22,23,27] (Supplementary Table S2).
4. Discussion
We reviewed 22 clinical studies involving 731 Korean patients with various lumbar spine disorders. We found that MRI has increasingly been used in recent years to assess treatment efficacy by measuring changes in affected regions comparing pre- and post-treatment MRI scans. Acupotomy primarily targeted damaged tissue in the lumbar area but also focused on acupoints. While a significant portion of studies reported the number of needles (77.27%), over 70% did not report details on needle size (22.73%), needle insertion depth, or anesthesia status (27.27%). Furthermore, despite the critical importance of needle manipulation intensity (such as the number of lifting–thrusting techniques and the depth of needle insertion) for the dose–response relationship, it was rarely reported in clinical studies. Clinical outcomes focused on pain and function of the lumbar spine, yet the reporting of safety measures and adverse events was inconsistent. For example, acupotomy treatment may cause discomfort, pain, bleeding and bruising, infection, tissue damage, scar formation, and nerve damage (e.g., spinal cord injury); however, only discomfort and pain symptoms were reported in detail. In addition, where adverse effects were reported, only the presence and type of adverse effects were documented, with limited reporting on severity, course and prognosis, and other detailed information regarding the adverse effects. This underscores the need for standardized reporting and safety protocols for acupotomy treatment, as well as clinical practice guidelines, in the near future.
After reviewing current clinical studies on acupotomy treatments for lumbar spine disorders, it is clear that specific guidelines for reporting and safety are essential for both clinicians and researchers. While several studies had detailed acupotomy procedures even including MRI images and illustrations, a comprehensive set of reporting guidelines, similar to those used for acupuncture such as STRICTA, would greatly improve our understanding of the intervention’s rationale, the practitioner’s qualifications, co-interventions, the treatment environment, and control interventions. It might be beneficial to tailor the STRICTA guidelines to better reflect the distinct aspects of acupotomy. For instance, since acupotomy needle features a knife-shaped tip, it is crucial to report not only the length and diameter of the needle but also the width and thickness of the knife part. Additionally, details on anesthesia methods and thorough documentation of any adverse events are critical components that should be included in the checklist for acupotomy procedures. For instance, while mild bleeding and discomfort at treatment sites might not be classified as serious adverse events, the presence of erythema and swelling along with these symptoms could indicate potential infection or inflammation. Therefore, documenting adverse events, post-treatment measures, and follow-up actions is essential, regardless of whether the adverse events are mild or severe. In addition to developing acupotomy-specific safety and reporting standards, referring to established frameworks from other minimally invasive therapies may offer practical insights. For example, prolotherapy—used to promote soft tissue regeneration by injecting irritant solutions into damaged ligaments or tendons—has accumulated safety protocols and standardized reporting procedures through clinical trials and systematic reviews [33].
In clinical settings, one of the major challenges is the absence of objective criteria for determining appropriate dosage intensity during acupotomy procedures. Clinicians currently rely on subjective measures—such as patient-reported tenderness and procedural pain—to guide decisions regarding the depth of needle insertion, intensity of stimulation, and the number of targeted sites. However, these parameters remain largely unstandardized and difficult to quantify. To address this gap, future studies should incorporate digital technologies such as pressure sensors, real-time ultrasound, and patient feedback systems to quantify stimulation intensity and monitor procedural consistency in real time. Moreover, given acupotomy’s relatively stronger stimulation and more invasive nature compared to conventional acupuncture, it is essential to identify patient subgroups who are most likely to benefit from this modality. Factors such as the chronicity of pain, structural abnormalities confirmed through imaging, or the clarity of tissue pathology may help determine clinical appropriateness. Utilizing diagnostic tools such as X-ray or MRI to stratify indications and develop data-driven, personalized application criteria will be critical for optimizing both therapeutic efficacy and safety in acupotomy treatment. In parallel, future research should also focus on developing multi-dimensional post-treatment evaluation indices that go beyond subjective symptom improvement to include quantifiable changes in pressure/pain thresholds and structural improvements confirmed by imaging.
We found that acupotomy treatments predominantly target adhesions within the low back, along with the adjacent muscles and ligaments. Notably, 16 of the 22 studies also targeted acupoints, tender points, and Ashi points. This indicates that while acupotomy treatments rely heavily on anatomical knowledge and are generally aimed at damaged tissues, clinicians are also applying techniques to stimulate specific acupoints. Specifically, treatments often involved acupoints along the Bladder and Governor Vessel meridians in the lumbar region, such as BL21-26 and GV3. As the technique of selecting local acupoints (acupoints located near the affected areas) is widely used to manage pain, it may enhance the pain-relieving effects of acupotomy on damaged tissues. In future studies, the exploration of optimal treatment sites, such as comparing the effects of acupotomy stimulating both affected regions and nearby acupoints with the effects of acupotomy targeting adhered tissues alone (while controlling for the number of needles and dose of stimulation), holds promise for enhancing treatment outcomes and minimizing adverse events in patients with lumbar spine disorders.
Most studies involved co-interventions in conjunction with acupotomy, which could have made it challenging to evaluate the effectiveness, safety, and adverse events of acupotomy alone. In addition, acupotomy treatment procedures varied among studies, and long-term follow-up investigations were rare, which indicates that additional research and consideration are needed in this area. More recent papers have increasingly used imaging tools such as MRI to evaluate the effects of treatment, suggesting that future acupotomy procedures might also be assessed using such diagnostic tools, suggesting that more precise and agreed-upon formats could evolve. For example, Wang et al. applied ultrasound to guide needle insertion while performing acupotomy procedures [16], and Yoon et al. measured the safe depth for acupotomy treatment in the lumbar spine using MRI [34]. From our perspective, MRI-guided safe treatment protocols and ultrasound-guided acupotomy procedures will become more common in clinics in the near future.
In terms of safety indicators, only 6 out of 22 papers (27.27%) addressed relevant content. Acupotomy, being a tool with significant invasiveness capable of detaching adhered tissues in the body, highlights the necessity for researchers to establish a consensus on safety indicators or checklists to confirm the safety of the procedure. The findings from this and a previous study [4] indicate that the data on adverse events related to acupotomy treatment are generally insufficient. We recommend the development of tools for assessing the safety of acupotomy, including establishing clear criteria for evaluating its safety and reporting adverse effects. These should focus on understanding the physiological changes acupotomy induces in the human body. Providing guidelines for future safety research papers on acupotomy presents challenges; therefore, discussions should involve experts in the field to identify necessary elements for such guidelines.
This study has several limitations. It only included clinical studies applying acupotomy treatments to lumbar spine disorders, which limits the generalizability of our findings. Reviewing the current state of clinical research on acupotomy applied to other diseases, such as knee arthritis, could provide broader insights. Based on our findings, we plan to conduct comprehensive research to fill the gaps identified in reporting needle size, needle insertion depth, and anesthesia status in acupotomy therapy. Additionally, we will develop and propose standardized safety and reporting guidelines to improve the consistency and quality of future clinical studies involving acupotomy treatments.
5. Conclusions
Our review of 22 clinical studies with 731 Korean patients with lumbar spine disorders highlights the increased use of MRI for treatment assessment and a preference for acupotomy targeting both acupoints and damaged tissue. However, inconsistencies in reporting crucial details and safety highlight the need for standardized clinical and reporting guidelines for acupotomy. Future research should focus on creating practical guidelines for safe, effective acupotomy procedures, detailing target tissues, needle specifications, and protocols for adverse effect reporting. Establishing objective criteria for stimulation dosage and incorporating digital technologies, such as pressure sensors and ultrasound guidance, could enhance procedure accuracy and reproducibility. Stratifying patients by imaging-confirmed abnormalities and symptom chronicity could further optimize treatment, while developing outcome indices that combine symptom relief and objective measures will be essential for comprehensively evaluating acupotomy efficacy.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare13101141/s1, Table S1: Acupotomy procedures and measures to prevent infection reported in the included studies. Table S2: Safety measures and adverse events reported in the included studies. Refs. [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32] are cited in the supplementary materials.
Author Contributions
Conceptualization: I.-S.L. and S.L. (Sooyoon Lee); Methodology: Y.B., E.S. and S.L. (Sooyoon Lee); Investigation: Y.B. and E.S.; Formal analysis: Y.B. and E.S.; Resources: Y.C., S.-H.Y. and J.L.; Writing—original draft: Y.B. and E.S.; Writing—review and editing: I.-S.L. and S.L. (Seunghoon Lee); Supervision: I.-S.L. and S.L. (Seunghoon Lee); Funding acquisition: I.-S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (Grant Number: HI23C1283). This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (RS-2023-00279315).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors have declared that no competing interests exist.
References
- Zhu, H. Summarization of acupotomology system. J. Eng. Sci. 2006, 8, 1–15. [Google Scholar]
- Zhu, H.; Quan, W.; Zhang, X.; Qiao, J.; Liu, Z.; Fu, P.; You, S. Clinical evaluation of needle knife in the treatment of cervical spondylosis. Chin. Acupunct. Moxibustion 2006, 5, 316–318. [Google Scholar]
- Jiang, C.; Li, Y.; Guo, M.; Li, X.; Guo, J.; Yu, S.; Lin, Z. Acupotomy therapy for lumbar disc herniation: Protocol for a systematic review and meta-analysis. Medicine 2018, 97, e12624. [Google Scholar] [CrossRef]
- Liu, F.; Zhou, F.; Zhao, M.; Fang, T.; Chen, M.; Yan, X. Acupotomy therapy for chronic nonspecific neck pain: A systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2017, 2017, 6197308. [Google Scholar] [CrossRef]
- Sun, J.; Zhao, Y.; Zhu, R.; Chen, Q.; Song, M.; Xue, Z.; Wang, R.; Chen, W. Acupotomy therapy for knee osteoarthritis pain: Systematic review and meta-analysis. Evid. Based Complement. Altern. Med. 2020, 2020, 2168283. [Google Scholar] [CrossRef]
- Kim, T.H.; Lee, C.R.; Choi, T.Y.; Lee, M.S. Intramuscular stimulation therapy for healthcare: A systematic review of randomised controlled trials. Acupunct. Med. 2012, 30, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Rabago, D.; Slattengren, A.; Zgierska, A. Prolotherapy in primary care practice. Prim. Care 2010, 37, 65. [Google Scholar] [CrossRef]
- Jeong, J.K.; Kim, E.; Yoon, K.S.; Jeon, J.H.; Kim, Y.I.; Lee, H.; Kwon, O.; Jung, S.-Y.; Lee, J.-H.; Yang, C.; et al. Acupotomy versus manual acupuncture for the treatment of back and/or leg pain in patients with lumbar disc herniation: A multicenter, randomized, controlled, assessor-blinded clinical trial. J. Pain Res. 2020, 13, 677–687. [Google Scholar] [CrossRef]
- Yoon, D.E.; Lee, I.S.; Chae, Y. Determining the adequate dose of acupuncture for personalised medicine. Acupunct. Med. 2021, 39, 565–566. [Google Scholar] [CrossRef]
- MacPherson, H.; Altman, D.G.; Hammerschlag, R.; Youping, L.; Taixiang, W.; White, A.; Moher, D. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): Extending the CONSORT statement. J. Altern. Complement. Med. 2010, 16, ST-1–ST-14. [Google Scholar] [CrossRef]
- Choi, J.I.; Jeon, J.H.; Kim, Y.I. A Case Report of a lumbar herniated intervertebral disc Patient Treated with Korean Medical Treatments, Mainly Managed by Acupotomy. J. Haehwa Med. 2022, 31, 1–10. [Google Scholar]
- Jang, E.H.; Kim, S.C.; Lim, N.R.; Na, W.M.; Lim, S.I.; Shin, J.B.; Lee, G.-M. Case study of Oriental Medicine treatment with acupotomy of the herniated lumbar intervertebral disc patient. J. Korean Acupunct. Moxibustion Soc. 2008, 25, 171–181. [Google Scholar]
- Park, S.W.; Kim, S.S.; Kim, J.Y.; Kim, S.H.; Lee, G.M. The Comparative Study of Effects between Acupotomy and its Cotreatment with Spine Decompression Therapy on HIVD Patients. J. Korean Acupunct. Moxibustion Soc. 2012, 29, 29–39. [Google Scholar]
- Yun, J.Y.; Kim, H.W.; Kim, S.S.; Park, S.W.; Kim, E.K.; Lee, G.H.; Lee, G.M. The Clinical Effects of acupuncture and Acupotomy Therapy for HIVD. J. Korean Acupunct. Moxibustion Soc. 2010, 27, 85–97. [Google Scholar]
- Woo, J.; Cho, S. A Case Report of Acupotomy Treatment on the Failed Back Surgery Syndrome. J. Korean Med. Soc. Acupotomology 2023, 7, 195–201. [Google Scholar] [CrossRef]
- Wang, Y.H.; Zhou, Y.; Xie, Y.Z.; Fan, X.H.; Liang, W.Q.; Wei, X.; Zhao, M.-D.; Huo, Y.-X.B.; Zhang, T.B.; Yin, Y. The effect of ultrasound-guided acupotomy and Juanbi decoction on lumbar disc herniation: A randomized controlled trial. Medicine 2023, 102, e32622. [Google Scholar] [CrossRef]
- Sun, T.C.; Choi, J.; Kim, H. A Case Report of Acupotomy Treatment at Internal Intervertebral Foramen on the Chronic HIVD Patient. J. Korean Med. Soc. Acupotomology 2023, 7, 15–22. [Google Scholar] [CrossRef]
- Kim, H.J.; Jeon, J.H.; Kim, Y.I. Clinical effect of acupotomy combined with Korean medicine: A case series of a herniated intervertebral disc. J. Acupunct. Meridian Stud. 2016, 9, 31–41. [Google Scholar] [CrossRef]
- Choi, H.K.; Lee, Y.R.; Cha, H.J.; Sung, K.J.; Kim, B.S.; Kim, M.J.; Lee, Y.J.; Jeon, J.H.; Kim, Y.I. Intractable Pain Management by Combined Korean Medicine Treatment Including Acupotomy in Lumbar Disc Herniation: A Case Report. Korean J. Acupunct. 2021, 38, 175–181. [Google Scholar] [CrossRef]
- Park, S.K.; Kim, Y.S.; Jo, H.K.; Yoo, H.R.; Seol, I.C. Case Report: Changes in Magnetic Resonance Imaging in Lumbar Disc Herniation Treated with Korean Medicine. J. Intern. Korean Med. 2018, 39, 863–869. [Google Scholar] [CrossRef]
- Lee, G.M.; Kim, D.H.; Kim, H.W.; Yeom, S.C.; Kim, H.S.; Kim, D.E.; Song, D.-S. The study on the effect of acupotomy in lumbar HIVD. J. Acupunct. Res. 2008, 25, 183–190. [Google Scholar]
- Sung, I.S.; Yuk, D.I.; Song, D.H.; Kim, M.J.; Hong, K.E. Case Study of with Dochim (刀鍼) & Gwanchim (管鍼) Therapy Combined with Korean Medicine Treatment of Herniated Lumbar Intervertebral Disc Patients. J. Korean Acupunct. Moxibustion Soc. 2013, 28, 153–159. [Google Scholar]
- Kim, H.S.; Kim, S.Y.; Kim, H.J.; Kim, E.S.; Kim, Y.I. The effect of acupotomy on lumbar herniated intervertebral disc: Report of a case series. Acupuncture 2015, 32, 185–195. [Google Scholar] [CrossRef]
- Kwak, B.M.; Hong, K.E. Four case of HIVD-lumbar spine patient treated with acupotomy. J. Acupunct. Res. 2008, 25, 149–156. [Google Scholar]
- Lee, Y.J.; Kim, J.I.; Kim, H.B.; Jeon, J.H.; Kim, E.; Kim, Y.I. Cervical and lumbar herniated nucleus pulposus resorption after acupotomy with integrative Korean medicine treatment: A case series of two patients. J. Acupunct. Res. 2019, 36, 107–112. [Google Scholar] [CrossRef]
- Jung, K.Y.; Sur, Y.C.; Jang, W.S.; Lee, J.E.; Kim, K.H.; Shin, G.S.; Han, Y.-S. Study and three Cases Report for Lumbar Spinal Stenosis Treatment Using a Combination of Acupotomy and Existing Treatments. Korean J. Orient. Physiol. Pathol. 2012, 26, 120–127. [Google Scholar]
- Yuk, D.I.; Sung, I.s.; Song, D.H.; Kim, M.J.; Hong, K.E. Clinical study of lumbar spine stenosis treated by using acupotomy combined with oriental medical treatments. J. Pharmacopunct. 2013, 16, 46. [Google Scholar] [CrossRef]
- Choi, C.W.; Choi, B.S.; Oh, M.S. The Effect of Acupotomy on Traumatic Acute Low back pain: Case Report. J. Haehwa Med. 2017, 26, 81–87. [Google Scholar]
- Kim, B.S.; Kim, J.I.; Kim, H.B.; Lee, Y.J.; Sung, K.J.; Jeon, J.H.; Kim, E.; Kim, Y.I. A patient with ankylosing spondylitis treated with acupotomy and traditional Korean medicine. J. Acupunct. Res. 2019, 36, 172–181. [Google Scholar] [CrossRef]
- Sun, T.C.; Kim, H.; Jung, S. A Case Report of Acupotomy Treatment on the Acute Myelitis Patient. J. Korean Med. Soc. Acupotomology 2023, 7, 187–194. [Google Scholar] [CrossRef]
- Choi, J. Case Report of Abnormal Spinal Curvature Improved by Acupotomy and Combined Korean Medicine Treatment. J. Korean Med. Soc. Soft Tissue 2022, 6, 128–134. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, H.J.; Ji, Y.S.; Lee, S.M.; Kim, Y.I. The effect of acupotomy on lumbar and cervical spine combined with oriental medical treatment: Report of five cases. J. Acupunct. Res. 2014, 31, 183–193. [Google Scholar] [CrossRef]
- Mafhoumi, A.; Nabian, M.H.; Mehrpour, S.R. Prolotherapy in musculoskeletal disorders, guideline for orthopedic application. Open J. Regen. Med. 2023, 12, 64–84. [Google Scholar] [CrossRef]
- Yoon, S.H.; Kim, S.A.; Lee, G.Y.; Kim, H.; Lee, J.H.; Leem, J. Using magnetic resonance imaging to measure the depth of acupotomy points in the lumbar spine: A retrospective study. Integr. Med. Res. 2021, 10, 100679. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).