Lifestyle, Age, and Heart Disease Evidence from European Datasets
Abstract
1. Introduction
2. Theory
2.1. Exercise and BMI by Age
2.2. Exercise and Age
2.3. Overweight and Cardiovascular Disease at Different Ages
- Children and Adolescents: While cardiovascular diseases are rare in this age group, a high BMI can set the stage for future cardiovascular risk. Early intervention and weight management are essential to prevent the development of cardiovascular conditions later in life.
- Young Adults: In young adults, lifestyle factors such as diet and physical activity play a significant role in BMI and cardiovascular risk. A high BMI in this age group is associated with an increased risk of developing cardiovascular diseases, emphasizing the need for healthy lifestyle choices.
- Middle-Aged Adults: The risk of cardiovascular diseases increases significantly in middle-aged adults with a high BMI. This age group often experiences the cumulative effects of a long-term high BMI, making weight management and regular health check-ups critical.
- Older Adults: Older adults with a high BMI are at the highest risk of cardiovascular diseases. Age-related changes in the cardiovascular system, combined with a high BMI, contribute to the increased prevalence of angina, heart attacks, and strokes in this population. Comprehensive management strategies, including medication, lifestyle changes, and regular monitoring, are essential for this age group.
2.4. Regression with Interaction
2.5. Stratified Logistic Regression and Odds Ratios
2.6. The LISS Panel
- Background Variables: Monthly updated socio-economic and demographic information.
- LISS Core Study: An annual longitudinal survey consisting of multiple questionnaires covering a broad range of topics, including health, religion, social integration, family, work, personality, politics, and economic situation.
- Assembled Studies: Surveys and experiments conducted as paid or externally funded assignments.
3. Materials and Methods
3.1. Italian Dataset
3.1.1. Survey Methodology
3.1.2. Data Collection Process
- Pre visit: Online survey on eating habits, food preferences, sleep, and physical activity.
- Visit: Bioelectrical impedance analysis (BIA) and anthropometric measurements.
- Follow-up: Seven-day food diary based on prescribed diet plans.
3.1.3. Sampling and Study Size
3.1.4. Ethical Considerations
3.1.5. Dietary and Physical Activity Assessment
3.2. LISS
3.3. Statistics
4. Results
4.1. Description of Italian Dataset
4.2. BMI and Exercise by Age Group
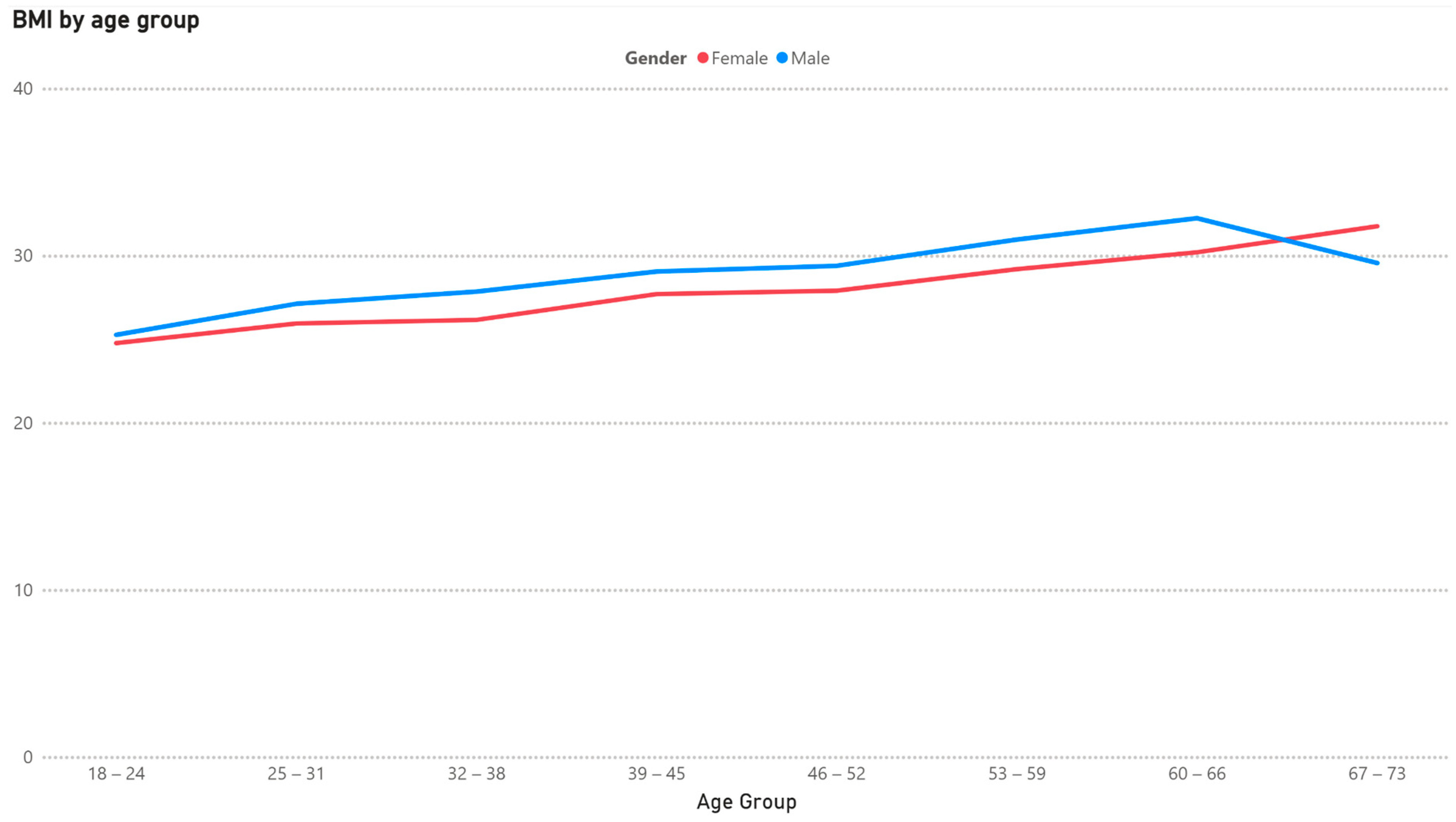
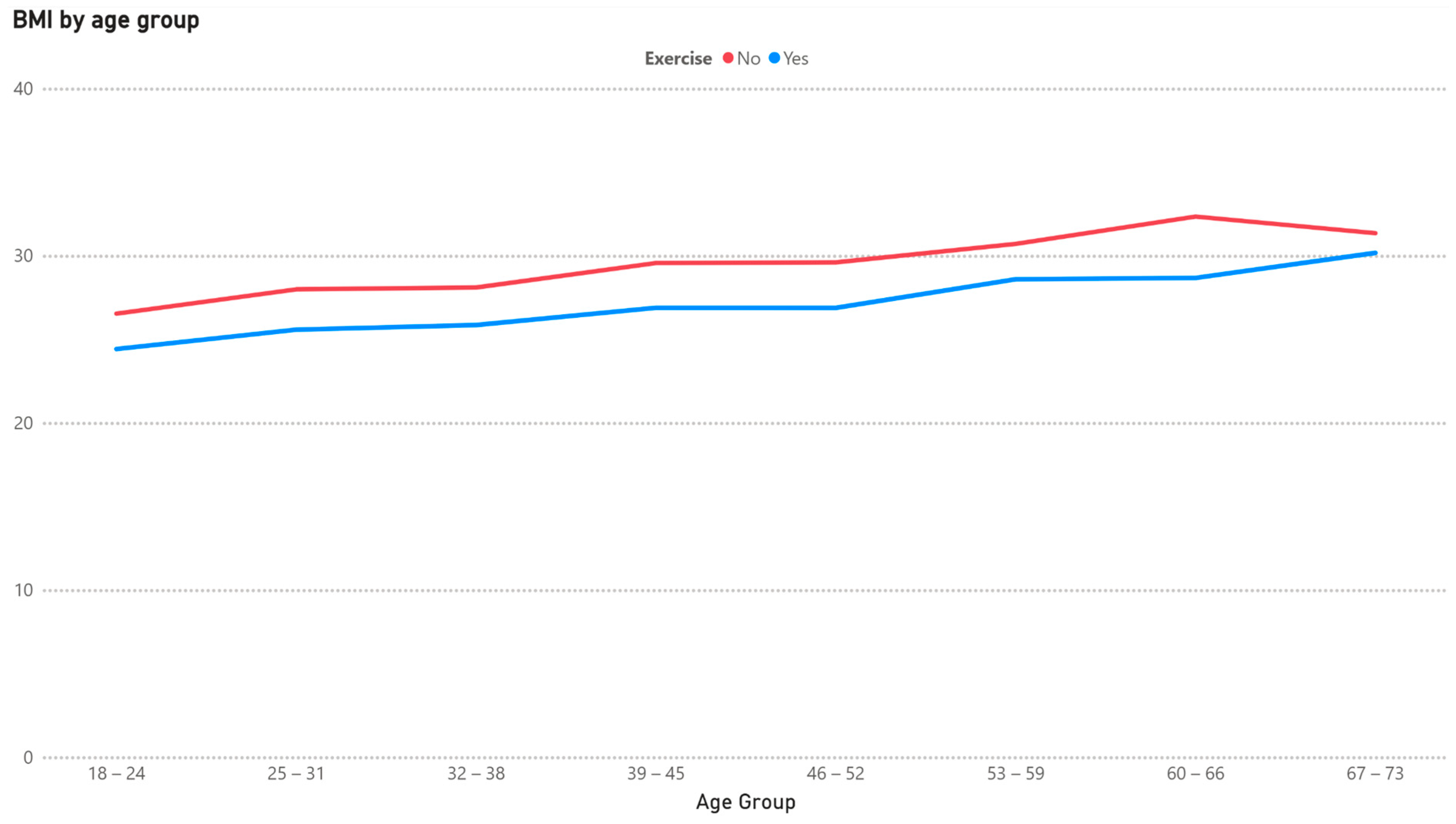
4.3. Interaction Between Exercise, BMI, and Age
4.4. Descriptives LISS Set
4.5. Heart Disease by Age Group
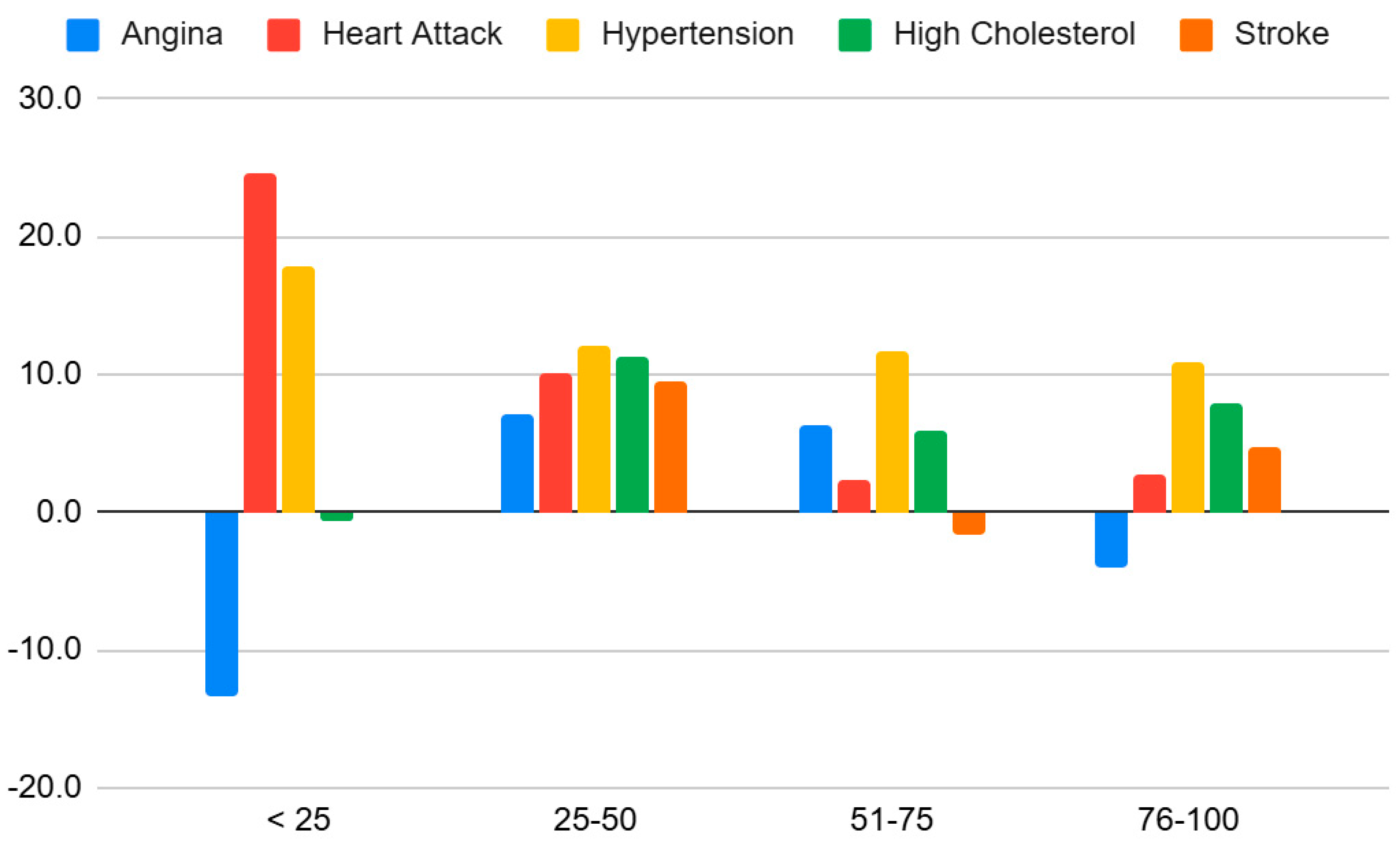
4.6. Connection Between Heart Disease and BMI by Age Group
5. Discussion
5.1. Age and Gender Differences
5.2. Exercise vs. Non-Exercise
5.3. Connection to Heart Disease
5.4. Study Limitations
5.5. Future Research Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rethemiotaki, I. Global prevalence of cardiovascular diseases by gender and age during 2010–2019. Arch. Med. Sci. Atheroscler. Dis. 2024, 8, 196–205. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Benefits of Physical Activity. 2022. Available online: https://www.cdc.gov/physical-activity-basics/about/index.html?CDC_AAref_Val=https://www.cdc.gov/physicalactivity/basics/benefits/index.htm (accessed on 8 April 2025).
- WHO Guidelines on Physical Activity and Sedentary Behaviour 25 November 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 8 April 2025).
- Church, T.S.; Blair, S.N.; Cocreham, S.; Johannsen, N.; Johnson, W.; Kramer, K.; Mikus, C.R.; Myers, V.; Nauta, M.; Rodarte, R.Q.; et al. Effects of Aerobic and Resistance Training on Hemoglobin A1cLevels in Patients With Type 2 Diabetes: A Randomized Controlled Trial. JAMA 2010, 304, 2253. [Google Scholar] [CrossRef]
- Swift, D.L.; McGee, J.E.; Earnest, C.P.; Carlisle, E.; Nygard, M.; Johannsen, N.M. The Effects of Exercise and Physical Activity on Weight Loss and Maintenance. Prog. Cardiovasc. Dis. 2018, 61, 206–213. [Google Scholar] [CrossRef]
- Huang, Z.; Sun, G.; Li, J.; Zhang, B.; Lai, G.; Jing, H.; Zhou, Y. Optimal exercise dose on Body Mass Index (BMI) in children and adolescents with overweight and obesity: A systematic review and bayesian model-based network meta-analysis. BMC Public Health 2025, 25, 215. [Google Scholar] [CrossRef]
- Patel, R.; Mirabello, S. Exercise and BMI: How Much Activity Is Enough? Now Patient. 2024. Available online: https://nowpatient.com/blog/exercise-and-bmi-how-much-activity-is-enough (accessed on 8 April 2025).
- Grasdalsmoen, M.; Eriksen, H.R.; Lønning, K.J.; Sivertsen, B. Physical exercise and body-mass index in young adults: A national survey of Norwegian university students. BMC Public Health 2019, 19, 1354. [Google Scholar] [CrossRef]
- Borgeraas, H.; Hertel, J.K.; Svingen, G.F.; Seifert, R.; Pedersen, E.K.; Schartum-Hansen, H.; Hjelmesæth, J.; Nygård, O. Association of body mass index with risk of acute myocardial infarction and mortality in Norwegian male and female patients with suspected stable angina pectoris: A prospective cohort study. BMC Cardiovasc. Disord. 2014, 14, 68. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adams, B.; Jacocks, L.; Guo, H. Higher BMI is linked to an increased risk of heart attacks in European adults: A Mendelian randomisation study. BMC Cardiovasc. Disord. 2020, 20, 258. [Google Scholar] [CrossRef]
- Wang, X.; Huang, Y.; Chen, Y.; Yang, T.; Su, W.; Chen, X.; Yan, F.; Han, L.; Ma, Y. The relationship between body mass index and stroke: A systemic review and meta-analysis. J. Neurol. 2022, 269, 6279–6289. [Google Scholar] [CrossRef]
- Aiken, L.S.; West, S.G. Multiple Regression: Testing and Interpreting Interactions; Sage Publications: Thousand Oaks, CA, USA, 1991; ISBN 978-0803936053. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2018; ISBN 978-1462534654. [Google Scholar]
- Jaccard, J.; Turrisi, R. Interaction Effects in Multiple Regression, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 2003; ISBN 978-0761927516. [Google Scholar]
- Olowe, K.J.; Edoh, N.L.; Zouo, S.J.C.; Olamijuwon, J. Comprehensive review of logistic regression techniques in predicting health outcomes and trends. World J. Adv. Pharm. Life Sci. 2024, 7, 016–026. [Google Scholar] [CrossRef]
- Boateng, E.Y.; Abaye, D.A. A Review of the Logistic Regression Model with Emphasis on Medical Research. J. Data Anal. Inf. Process. 2019, 07, 190–207. [Google Scholar] [CrossRef]
- Jing-Nan, Y.; Yu-Zhu, T.; Yue, W.; Chun-Ho, W. Multiple-response logistic regression modeling with application to an analysis of cirrhosis liver disease data. Comput. Stat. 2024, 39, 345–367. [Google Scholar] [CrossRef]
- Palmer, A.K.; Jensen, M.D. Metabolic changes in aging humans: Current evidence and therapeutic strategies. J. Clin. Investig. 2022, 132, e158451. [Google Scholar] [CrossRef] [PubMed]
- Moran, L.; Norman, R.J. Understanding and managing disturbances in insulin metabolism and body weight in women with polycystic ovary syndrome. Best Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 719–736. [Google Scholar] [CrossRef]
- Li, D.C.W.; Rudloff, S.; Langer, H.T.; Norman, K.; Herpich, C. Age-Associated Differences in Recovery from Exercise-Induced Muscle Damage. Cells 2024, 13, 255. [Google Scholar] [CrossRef]
- Steltenpohl, C.N.; Shuster, M.; Peist, E.; Pham, A.; Mikels, J.A. Me Time, or We Time? Age Differences in Motivation for Exercise. Gerontol. 2018, 59, 709–717. [Google Scholar] [CrossRef]
- Box, A.G.; Feito, Y.; Matson, A.; Heinrich, K.M.; Petruzzello, S.J. Is age just a number? Differences in exercise participatory motives across adult cohorts and the relationships with exercise behaviour. Int. J. Sport Exerc. Psychol. 2019, 19, 61–73. [Google Scholar] [CrossRef]
- European Commission. Sport and Physical Activity—September 2022—Eurobarometer Survey—European Union. 2022. Available online: https://europa.eu/eurobarometer/surveys/detail/2668. (accessed on 18 March 2025).
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, A.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 2019, 112, 2735–2752. [Google Scholar] [CrossRef]
- Westerterp, K.R. Exercise, energy balance and body composition. Eur. J. Clin. Nutr. 2018, 72, 1246–1250. [Google Scholar] [CrossRef]
- Hunter, G.R.; Fisher, G.; Neumeier, W.H.; Carter, S.J.; Plaisance, E.P. Exercise Training and Energy Expenditure following Weight Loss. Med. Sci. Sports Exerc. 2015, 47, 1950–1957. [Google Scholar] [CrossRef]
- Sjödin, A.M.; Forslund, A.H.; Westerterp, K.R.; Andersson, A.B.; Forslund, J.M.; Hambreus, L.M. The influence of physical activity on BMR. Med. Sci. Sports Exerc. 1996, 28, 85–91. [Google Scholar] [CrossRef]
- Jayedi, A.; Soltani, S.; Emadi, A.; Zargar, M.S.; Najafi, A. Aerobic Exercise and Weight Loss in Adults: A Systematic Review and Dose-Response Meta-Analysis. JAMA Netw. Open 2024, 7, e2452185. [Google Scholar] [CrossRef] [PubMed]
- Aasdahl, L.; Iversen, V.M.; Skovlund, E.; Aune, D.; Fimland, M.S. What should be the preferred exercise modality for overweight and obese individuals? Protocol for a systematic review and network meta-analysis. Syst. Rev. 2019, 8, 1–5. [Google Scholar] [CrossRef]
- Cheng, R.K.; Kittleson, M.M.; Beavers, C.J.; Birnie, D.H.; Blankstein, R.; Bravo, P.E.; Gilotra, N.A.; Judson, M.A.; Patton, K.K.; Rose-Bovino, L. American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology, and Council on Cardiovascular and Stroke Nursing. Diagnosis and Management of Cardiac Sarcoidosis: A Scientific Statement From the American Heart Association. Circulation 2024, 149, e1197–e1216. [Google Scholar] [CrossRef]
- Landi, F.; Calvani, R.; Picca, A.; Tosato, M.; Martone, A.M.; Ortolani, E.; Sisto, A.; D′Angelo, E.; Serafini, E.; Desideri, G.; et al. Body Mass Index is Strongly Associated with Hypertension: Results from the Longevity Check-Up 7+ Study. Nutrients 2018, 10, 1976. [Google Scholar] [CrossRef]
- Dulloo, A.G.; Jacquet, J.; Montani, J.P. Pathways from weight fluctuations to metabolic diseases: Focus on maladaptive thermogenesis during catch-up fat. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 2002, 26 (Suppl. S2), S46–S57. [Google Scholar] [CrossRef]
- Schwarz, N. Self-reports: How the questions shape the answers. Am. Psychol. 1999, 54, 93–105. [Google Scholar] [CrossRef]
- Abramowitz, M.K.; Hall, C.B.; Amodu, A.; Sharma, D.; Androga, L.; Hawkins, M. Muscle mass, BMI, and mortality among adults in the United States: A population-based cohort study. PLoS ONE 2018, 13, e0194697. [Google Scholar] [CrossRef]
- Fuchs, F.D.; Whelton, P.K. High Blood Pressure and Cardiovascular Disease. Hypertension 2020, 75, 285–292. [Google Scholar] [CrossRef] [PubMed]

| Question | Follow-Up | Unit |
|---|---|---|
| How tall are you? | cm | |
| How much do you weigh, without clothes or shoes? | kg | |
| Has a physician told you this last year that you suffer from… | Yes/No | |
| angina, pain in the chest? | ||
| a heart attack including infarction or coronary thrombosis or another heart problem including heart failure? | ||
| a stroke or brain infarction or a disease affecting the blood vessels in the brain? |
| Feature | Mean/Distribution |
|---|---|
| Age | 39.72 years |
| BMI | 27.63 kg/m |
| Exercise | 53.12% |
| Age Group | BMI Mean Males/Females | Percentage of Population Engaging in Exercise Males/Females | ||
|---|---|---|---|---|
| 18–24 | 25.26 | 24.76 | 76.80 | 68.61 |
| 25–31 | 27.12 | 25.94 | 67.88 | 61.36 |
| 32–38 | 27.85 | 26.15 | 68.29 | 43.07 |
| 39–45 | 29.05 | 27.70 | 52.94 | 46.90 |
| 46–52 | 29.39 | 27.90 | 50.00 | 42.44 |
| 53–59 | 30.96 | 29.19 | 35.90 | 38.39 |
| 60–66 | 32.24 | 30.20 | 44.12 | 41.67 |
| 67–73 | 29.56 | 31.76 | 35.00 | 30.56 |
| Term | Estimate | Pr (>|t|) |
|---|---|---|
| exercise | −2.13 | 0.0023 ** |
| age_group [25, 32) | 1.76 | 0.016 * |
| age_group [32, 39) | 1.47 | 0.032 * |
| age_group [39, 46) | 2.94 | 2.5 × 10−5 *** |
| age_group [46, 53) | 3.22 | 3.6 × 10−6 *** |
| age_group [53, 60) | 4.33 | 8.7 × 10−9 *** |
| age_group [60, 67) | 6.26 | 1.2 × 10−13 *** |
| age_group [67, 74) | 4.80 | 1.5 × 10−6 *** |
| exercise × age_group [25, 32) | −0.44 | 0.61 |
| exercise × age_group [32, 39) | −0.03 | 0.97 |
| exercise × age_group [39, 46) | −0.55 | 0.53 |
| exercise × age_group [46, 53) | −0.76 | 0.39 |
| exercise × age_group [53, 60) | −0.42 | 0.68 |
| exercise × age_group [60, 67) | −2.05 | 0.07 |
| exercise × age_group [67, 74) | 0.97 | 0.54 |
| Feature | Mean/Distribution |
|---|---|
| Age | 44 years |
| BMI | 25.0 kg/m2 |
| Angina | 1.9% |
| Heart Attack | 1.4% |
| Hypertension | 11.9% |
| High Cholesterol | 7.5% |
| Stroke | 0.7% |
| Age Group | Angina% Male/Female | Heart Attack% Male/Female | Stroke% Male/Female | |||
|---|---|---|---|---|---|---|
| 16–25 | 0.5 | 1.5 | 0.2 | 0.2 | 0.0 | 0.0 |
| 26–35 | 1.4 | 1.2 | 0.5 | 0.2 | 0.3 | 0.4 |
| 36–45 | 0.8 | 1.4 | 0.6 | 0.2 | 0.1 | 0.1 |
| 46–55 | 2.6 | 1.4 | 1.6 | 0.3 | 0.4 | 0.4 |
| 56–65 | 2.9 | 1.6 | 3.7 | 1.7 | 2.0 | 1.0 |
| 66–75 | 3.7 | 3.4 | 4.8 | 3.1 | 2.0 | 1.9 |
| 76–85 | 6.4 | 3.3 | 7.8 | 6.2 | 3.0 | 3.1 |
| 86–95 | 5.8 | 2.0 | 10.0 | 5.3 | 5.0 | N/A a |
| <25 | 25–50 | 51–75 | 76–100 | |
|---|---|---|---|---|
| Angina | −13.4 | 7.2 ** | 6.4 ** | −3.9 |
| Heart Attack | 24.6 *** | 10.0 * | 2.3 | 2.7 |
| Hypertension | 17.8 *** | 12.1 *** | 11.6 *** | 10.8 *** |
| High Cholesterol | −0.7 | 11.3 *** | 5.8 *** | 8.0 * |
| Stroke | 0.0 | 9.6 | −1.7 | 4.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Engst, S.; Fangrat, K.; Lane, H.; Lombardo, M. Lifestyle, Age, and Heart Disease Evidence from European Datasets. Healthcare 2025, 13, 1123. https://doi.org/10.3390/healthcare13101123
Engst S, Fangrat K, Lane H, Lombardo M. Lifestyle, Age, and Heart Disease Evidence from European Datasets. Healthcare. 2025; 13(10):1123. https://doi.org/10.3390/healthcare13101123
Chicago/Turabian StyleEngst, Samuel, Kristoffer Fangrat, Håkan Lane, and Mauro Lombardo. 2025. "Lifestyle, Age, and Heart Disease Evidence from European Datasets" Healthcare 13, no. 10: 1123. https://doi.org/10.3390/healthcare13101123
APA StyleEngst, S., Fangrat, K., Lane, H., & Lombardo, M. (2025). Lifestyle, Age, and Heart Disease Evidence from European Datasets. Healthcare, 13(10), 1123. https://doi.org/10.3390/healthcare13101123