Assessing the Knowledge of HPV-Associated Oropharyngeal Squamous Cell Carcinoma, HPV Vaccination, and Practice Scope among Saudi Dental Students in the Western Region
Abstract
1. Introduction
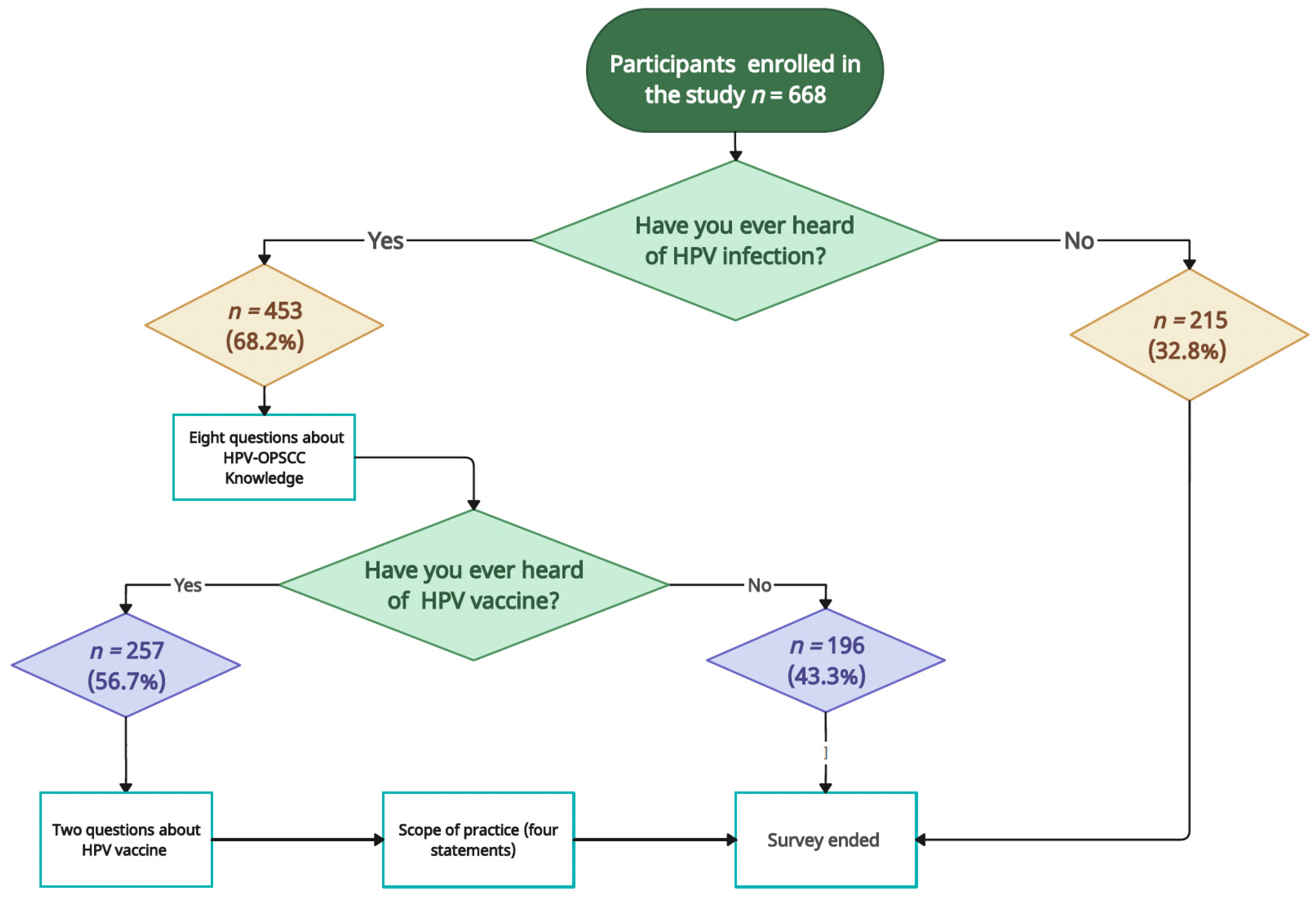
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sample Size and Participants Recruitments
2.3. Data Collection
2.4. Ethical Consideration and Informed Consent
2.5. Statistical Analysis
3. Results
3.1. HPV-OPSCC Knowledge
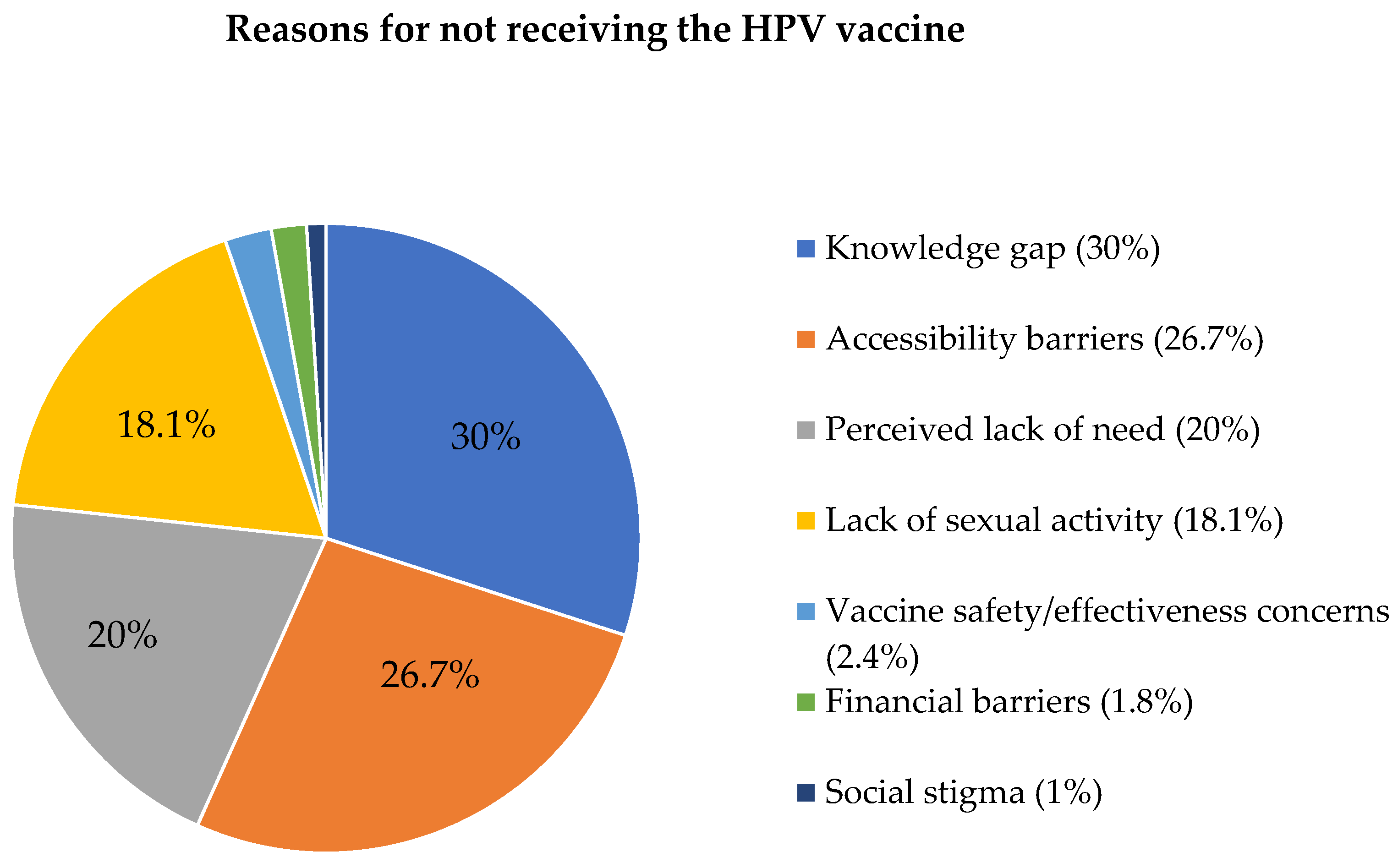
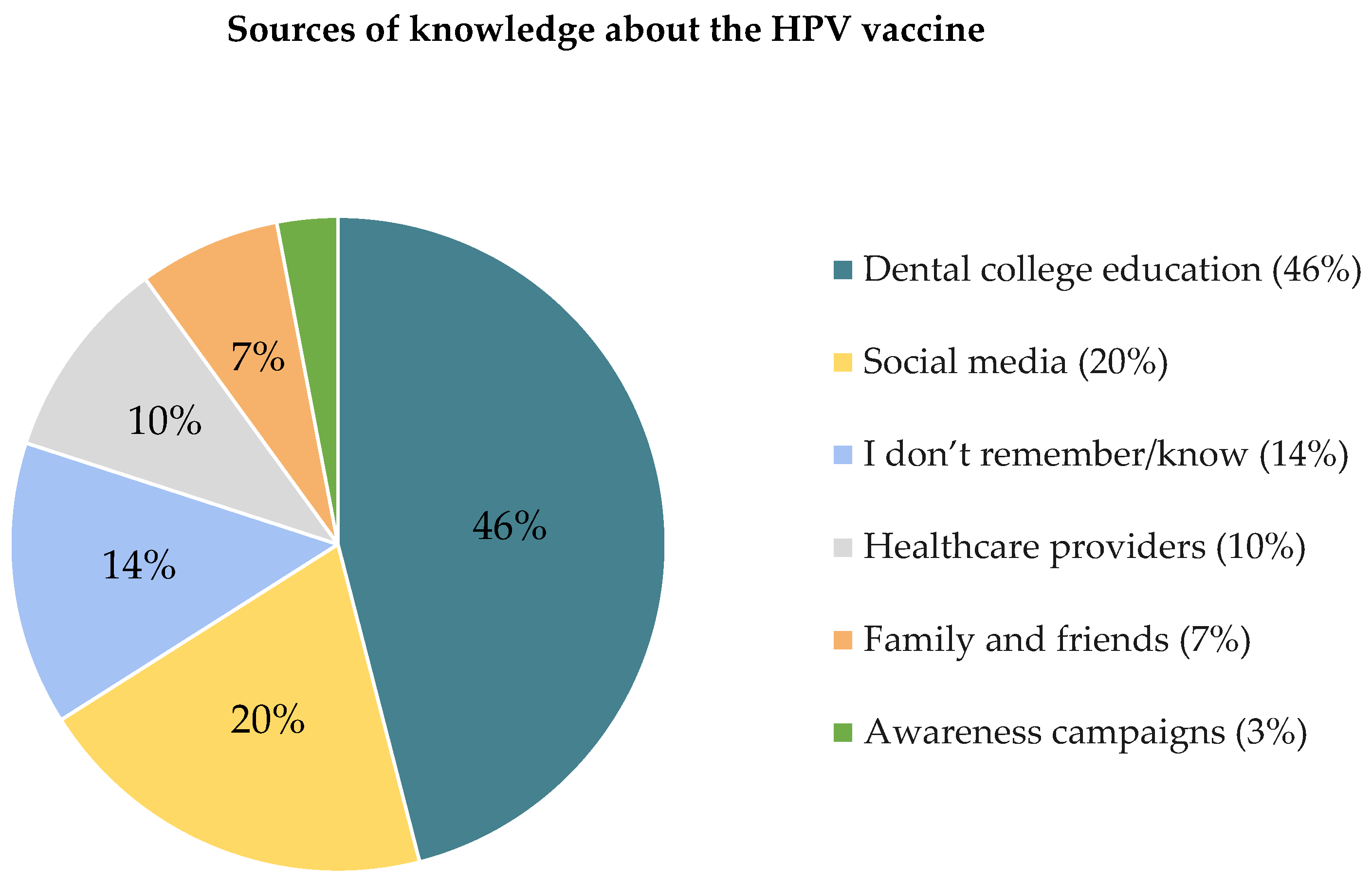
3.2. HPV Vaccine Knowledge
3.3. HPV in the Dental Practice Scope
3.4. Regression Model Analysis
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Cleveland, J.L.; Junger, M.L.; Saraiya, M.; Markowitz, L.E.; Dunne, E.F.; Epstein, J.B. The connection between human papillomavirus and oropharyngeal squamous cell carcinomas in the United States: Implications for dentistry. J. Am. Dental Assoc. 2011, 142, 915–924. [Google Scholar] [CrossRef]
- Badoual, C. Update from the 5th edition of the World Health Organization classification of head and neck tumors: Oropharynx and nasopharynx. Head Neck Pathol. 2022, 16, 19–30. [Google Scholar] [CrossRef]
- Hashibe, M.; Brennan, P.; Chuang, S.-C.; Boccia, S.; Castellsague, X.; Chen, C.; Curado, M.P.; Dal Maso, L.; Daudt, A.W.; Fabianova, E. Interaction between tobacco and alcohol use and the risk of head and neck cancer: Pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol. Biomark. Prev. 2009, 18, 541–550. [Google Scholar] [CrossRef]
- Alsahafi, E.; Begg, K.; Amelio, I.; Raulf, N.; Lucarelli, P.; Sauter, T.; Tavassoli, M. Clinical update on head and neck cancer: Molecular biology and ongoing challenges. Cell Death Dis. 2019, 10, 540. [Google Scholar] [CrossRef]
- Wang, H.; Wang, B.; Wei, J.; Meng, L.; Zhang, Q.; Qu, C.; Xin, Y.; Jiang, X. Molecular mechanisms underlying increased radiosensitivity in human papillomavirus-associated oropharyngeal squamous cell carcinoma. Int. J. Biol. Sci. 2020, 16, 1035. [Google Scholar] [CrossRef]
- Lu, Y.; Xie, Z.; Luo, G.; Yan, H.; Qian, H.-Z.; Fu, L.; Wang, B.; Huang, R.; Cao, F.; Lin, H. Global burden of oropharyngeal cancer attributable to human papillomavirus by anatomical subsite and geographic region. Cancer Epidemiol. 2022, 78, 102140. [Google Scholar] [CrossRef]
- Mehanna, H.; Franklin, N.; Compton, N.; Robinson, M.; Powell, N.; Biswas Baldwin, N.; Paleri, V.; Hartley, A.; Fresco, L.; Al-Booz, H. Geographic variation in human papillomavirus–related oropharyngeal cancer: Data from 4 multinational randomized trials. Head Neck 2016, 38, E1863–E1869. [Google Scholar] [CrossRef]
- Conarty, J.P.; Wieland, A. The tumor-specific immune landscape in HPV+ head and neck cancer. Viruses 2023, 15, 1296. [Google Scholar] [CrossRef]
- Al-Shahrani, Z.; Al-Rawaji, A.; Al-Madouj, A.; Hayder, M. Saudi cancer registry: Cancer incidence report Saudi Arabia 2014. Saudi Health Counc. Riyadh Saudi Arab. 2017, 1–82. Available online: https://shc.gov.sa/Arabic/NCC/Activities/AnnualReports/2014.pdf (accessed on 8 March 2024).
- Alsbeih, G.; Al-Harbi, N.; Bin Judia, S.; Al-Qahtani, W.; Khoja, H.; El-Sebaie, M.; Tulbah, A. Prevalence of human papillomavirus (HPV) infection and the association with survival in Saudi patients with head and neck squamous cell carcinoma. Cancers 2019, 11, 820. [Google Scholar] [CrossRef]
- Gupta, B.; Johnson, N.W.; Kumar, N. Global epidemiology of head and neck cancers: A continuing challenge. Oncology 2016, 91, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Khalid, M.B.; Ting, P.; Pai, A.; Russo, J.L.; Bakst, R.; Chai, R.L.; Teng, M.S.; Genden, E.M.; Miles, B.A. Initial presentation of human papillomavirus-related head and neck cancer: A retrospective review. Laryngoscope 2019, 129, 877–882. [Google Scholar] [CrossRef]
- Ferrando-Díez, A.; Pavón, M.A.; Cirauqui, B.; Alemany, L.; Mesía, R. How to prevent human papillomavirus-related oropharyngeal cancer? Curr. Opin. Oncol. 2023, 35, 145–150. [Google Scholar] [CrossRef]
- Al-Shaikh, G.K.; Almussaed, E.M.; Fayed, A.A.; Khan, F.H.; Syed, S.B.; Al-Tamimi, T.N.; Elmorshedy, H.N. Knowledge of Saudi female university students regarding cervical cancer and acceptance of the human papilloma virus vaccine. Saudi Med. J. 2014, 35, 1223. [Google Scholar] [PubMed]
- Macilwraith, P.; Malsem, E.; Dushyanthen, S. The effectiveness of HPV vaccination on the incidence of oropharyngeal cancers in men: A review. Infect. Agents Cancer 2023, 18, 24. [Google Scholar] [CrossRef] [PubMed]
- Kline, N.; Vamos, C.; Thompson, E.; Catalanotto, F.; Petrila, J.; DeBate, R.; Griner, S.; Vázquez-Otero, C.; Merrell, L.; Daley, E. Are dental providers the next line of HPV-related prevention? Providers’ perceived role and needs. Papillomavirus Res. 2018, 5, 104–108. [Google Scholar] [CrossRef]
- Walker, K.K.; Jackson, R.D.; Sommariva, S.; Neelamegam, M.; Desch, J. USA dental health providers’ role in HPV vaccine communication and HPV-OPC protection: A systematic review. Hum. Vaccines Immunother. 2019, 15, 1863–1869. [Google Scholar] [CrossRef] [PubMed]
- Ciarrocca, K.; Jackson, L.L.; Rossi, S.S.D. Human papillomavirus: The fundamentals of HPV for oral health care providers. J. Calif. Dent. Assoc. 2013, 41, 349–355. [Google Scholar] [CrossRef]
- Wright, M.; Pazdernik, V.; Luebbering, C.; Davis, J.M. Dental students’ knowledge and attitudes about human papillomavirus prevention. Vaccines 2021, 9, 888. [Google Scholar] [CrossRef]
- Altamimi, T. Human papillomavirus and its vaccination: Knowledge and attitudes among female university students in Saudi Arabia. J. Fam. Med. Prim. Care 2020, 9, 1849–1855. [Google Scholar] [CrossRef]
- Aldawood, E.; Alzamil, L.; Faqih, L.; Dabbagh, D.; Alharbi, S.; Hafiz, T.A.; Alshurafa, H.H.; Altukhais, W.F.; Dabbagh, R. Awareness of human papillomavirus among male and female University students in Saudi Arabia. Healthcare 2023, 11, 649. [Google Scholar] [CrossRef]
- Farsi, N.J.; Al Sharif, S.; Al Qathmi, M.; Merdad, M.; Marzouki, H.; Merdad, L. Knowledge of human papillomavirus (HPV) and oropharyngeal cancer and acceptability of the HPV vaccine among dental students. Asian Pac. J. Cancer Prev. 2020, 21, 3595. [Google Scholar] [CrossRef]
- Waller, J.; Ostini, R.; Marlow, L.A.; McCaffery, K.; Zimet, G. Validation of a measure of knowledge about human papillomavirus (HPV) using item response theory and classical test theory. Prev. Med. 2013, 56, 35–40. [Google Scholar] [CrossRef]
- Gillison, M.L.; Chaturvedi, A.K.; Lowy, D.R. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer 2008, 113, 3036–3046. [Google Scholar] [CrossRef]
- Farsi, N.J.; Baharoon, A.H.; Jiffri, A.E.; Marzouki, H.Z.; Merdad, M.A.; Merdad, L.A. Human papillomavirus knowledge and vaccine acceptability among male medical students in Saudi Arabia. Hum. Vaccin. Immunother. 2021, 17, 1968–1974. [Google Scholar] [CrossRef]
- Alqarawi, S.A.; Aljarbooa, E.F.; Almuqaytib, A.Y.; Alomar, I.A.; Altwaijri, M.H.; Aldakhil, A.Y.; Altowaijri, A.H. Assessment of Saudi Females’ Knowledge Regarding Human Papillomavirus Infection, Screening, and Available Methods for Prevention: A Cross-Sectional Study in Qassim Region. Cureus 2023, 15, e33311. [Google Scholar] [CrossRef]
- Algudaibi, L.Y.; AlMeaigel, S.; AlQahtani, N.; Shaheen, N.A.; Aboalela, A. Oral and oropharyngeal cancer: Knowledge, attitude and practices among medical and dental practitioners. Cancer Rep. 2021, 4, e1349. [Google Scholar] [CrossRef]
- Lingam, A.S.; Koppolu, P.; Alhussein, S.A.; Abdelrahim, R.K.; Abusalim, G.S.; ElHaddad, S.; Asrar, S.; Nassani, M.Z.; Gaafar, S.S.; Bukhary, F.M.T. Dental students’ perception, awareness and knowledge about hpv infection, vaccine, and its association with oral cancer: A multinational study. Infect. Drug Resist. 2022, 3711–3724. [Google Scholar] [CrossRef]
- Rutkoski, H.; Tay, D.L.; Dixon, B.L.; Pinzon, L.M.; Mooney, R.; Winkler, J.R.; Kepka, D. A multi-state evaluation of oral health students’ knowledge of human papillomavirus-related oropharyngeal cancer and HPV vaccination. J. Cancer Educ. 2020, 35, 1017–1025. [Google Scholar] [CrossRef]
- Rumianek, M.B.; Siedlecka, E.; Sawleshwarkar, S.; Ajwani, S. Australian dentists’ knowledge and attitude towards HPV infection. Int. Dent. J. 2023, 73, S17. [Google Scholar] [CrossRef]
- Rakhra, D.; Walker, T.; Hall, S.; Fleming, C.; Thomas, S.; Kerai, A.; Horwood, J.; Waylen, A. Human papillomavirus (HPV) and its vaccine: Awareness and opinions of clinical dental students in a UK dental school. Br. Dent. J. 2018, 225, 976–981. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Fraihat, E.; Dababseh, D.; Yaseen, A.; Taim, D.; Zabadi, S.; Hamdan, A.A.; Hassona, Y.; Mahafzah, A.; Şahin, G.Ö. Dental students’ awareness and attitudes toward HPV-related oral cancer: A cross sectional study at the University of Jordan. BMC Oral Health 2019, 19, 171. [Google Scholar] [CrossRef]
- Rashwan, H.H.; Saat, N.Z.N.M.; Manan, D.N.A. Knowledge, attitude and practice of malaysian medical and pharmacy students towards human papillomavirus vaccination. Asian Pac. J. Cancer Prev. 2012, 13, 2279–2283. [Google Scholar] [CrossRef]
- Almutairi, S.N.; Aljalfan, A.A.; Alqahtani, Z.A.; Shadid, A.M.; Aljalfan, A.A.; Shadid, A. Knowledge of human papillomavirus, risk of anogenital cancers, and benefits of vaccination: A medical student survey in Saudi Arabia. Cureus 2019, 11, e5051. [Google Scholar] [CrossRef]
- Ahken, S.; Fleming, N.; Dumont, T.; Black, A. Hpv awareness in higher-risk young women: The need for a targeted hpv catch-up vaccination program. J. Obstet. Gynaecol. Can. 2015, 37, 122–128. [Google Scholar] [CrossRef]
- Chiang, V.C.L.; Wong, H.T.; Yeung, P.C.A.; Choi, Y.K.; Fok, M.S.Y.; Mak, O.I.; Wong, H.Y.; Wong, K.H.; Wong, S.Y.; Wong, Y.S. Attitude, acceptability and knowledge of HPV vaccination among local university students in Hong Kong. Int. J. Environ. Res. Public Health 2016, 13, 486. [Google Scholar] [CrossRef]
- Collange, F.; Fressard, L.; Pulcini, C.; Sebbah, R.; Peretti-Watel, P.; Verger, P. General practitioners’ attitudes and behaviors toward HPV vaccination: A French national survey. Vaccine 2016, 34, 762–768. [Google Scholar] [CrossRef]
- Alsubaie, A.S.R. Exploring sexual behaviour and associated factors among adolescents in Saudi Arabia: A call to end ignorance. J. Epidemiol. Glob. Health 2019, 9, 76–80. [Google Scholar] [CrossRef]
- Swarnapriya, K.; Kavitha, D.; Reddy, G. Knowledge, attitude and practices regarding HPV vaccination among medical and para medical in students, India a cross sectional study. Asian Pac. J. Cancer Prev. 2015, 16, 8473–8477. [Google Scholar] [CrossRef]
- Rajeh, M.T.; Sembawa, S.N.; Nassar, A.A.; Al Hebshi, S.A.; Aboalshamat, K.T.; Badri, M.K. Social media as a learning tool: Dental students’ perspectives. J. Dent. Educ. 2021, 85, 513–520. [Google Scholar] [CrossRef]
- Vázquez-Otero, C.; Vamos, C.A.; Thompson, E.L.; Merrell, L.K.; Griner, S.B.; Kline, N.S.; Catalanotto, F.A.; Giuliano, A.R.; Daley, E.M. Assessing dentists’ human papillomavirus–related health literacy for oropharyngeal cancer prevention. J. Am. Dent. Assoc. 2018, 149, 9–17. [Google Scholar] [CrossRef]
| Demographics | Total n (%) | HPV Knowledge Score | p-Value | HPV Vaccine Awareness | p-Value | Total n (%) | HPV Scope of Practice | p-Value | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes n (%) | No n (%) | |||||||||
| Total | 453 (100%) | 53.44 ± 29.3 | - | 257 (56.7%) | 196 (43.3%) | - | 257 (100%) | 12.16 ± 3.0 | - | |
| Age (years) | <20 | 25 (5.5%) | 42.80 ± 32.2 AC* | 0.012 a,c | 12 (48.0%) | 13 (52.0%) | 0.23 | 12 (4.7%) | 10.08 ± 2.7 | 0.101 |
| 20–25 | 364 (80.3%) | 54.84 ± 28.9 B* | 203 (55.8%) | 161 (44.2%) | 203 (79%) | 12.25 ± 3.0 | ||||
| 25–30 | 61 (13.5%) | 51.64 ± 29.1 AB* | 41 (67.2%) | 2 (32.8%) | 41 (16%) | 12.32 ± 2.8 | ||||
| >30 | 3 (0.7%) | 10.00 ± 10.0 C* | 1 (33.3%) | 2 (66.7%) | 1 (0.3%) | 12.00 ± 0.0 | ||||
| Gender | Male | 198 (43.7%) | 54.75 ± 30.2 | 0.405 | 100 (50.5%) | 98 (49.5%) | 0.018 d | 100 (38.9%) | 12.20 ± 3.0 | 0.848 |
| Female | 255 (56.3%) | 52.43 ± 28.6 | 157 (61.6%) | 98 (38.4%) | 157 (61.1%) | 12.13 ± 2.9 | ||||
| Dental college | Private | 160 (35.4%) | 55.82 ± 27.1 | <0.008 b | 101 (63.1%) | 59 (36.9%) | 0.043 d | 101 (39.3%) | 12.25 ± 3.0 | <0.098 |
| Governmental | 293 (64.6%) | 48.97 ± 26.1 | 156 (53.2%) | 137 (46.8%) | 156 (60.7%) | 11.7 ± 2.3 | ||||
| Clinical | Clinical | 353 (77.9%) | 56.29 ± 29.1 | <0.001 b | 201 (56.9%) | 152 (43.1%) | 0.867 | 201 (78.9%) | 12.26 ± 3.0 | 0.268 |
| Non-Clinical | 100 (22.1%) | 43.40 ± 27.9 | 56 (56.0%) | 44 (44.0%) | 56 (21.1%) | 11.77 ± 2.8 | ||||
| Grade point average | ≤2.99 | 8 (1.8%) | 47.50 ± 27.1 AB* | 0.047 a,c | 6 (75.0%) | 2 (25.0%) | 0.83 | 6 (2.3%) | 10.00 ± 2.5 | 0.068 |
| 3–3.49 | 46 (10.1%) | 49.35 ± 30.7 AB* | 25 (54.3%) | 21 (45.7%) | 25 (9.7%) | 12.12 ± 2.2 | ||||
| 3.50–3.99 | 81 (17.9%) | 45.80 ± 32.6 B* | 48 (59.3%) | 33 (40.7%) | 48 (18.7%) | 12.58 ± 3.2 | ||||
| 4–4.49 | 155 (34.2%) | 55.35 ± 28.7 A* | 87 (56.1%) | 68 (43.9%) | 87 (33.9%) | 12.60 ± 2.8 | ||||
| ≥4.50 | 163 (36%) | 56.87 ± 27.3 A* | 91 (55.8%) | 7 (44.2%) | 91 (35.4%) | 11.66 ± 3.1 | ||||
| Marital status | Single | 425 (93.8%) | 53.34 ± 29.1 | 0.772 | 243 (57.2%) | 182 (42.8%) | 0.458 | 243 (94.6%) | 12.21 ± 2.9 | 0.221 |
| Married | 28 (6.2%) | 55.00 ± 32.4 | 14 (50.0%) | 14 (50.0%) | 14 (5.4%) | 11.21 ± 3.7 | ||||
| History of sexually transmitted disease | Yes | 17 (3.8%) | 65.29 ± 33.2 | 0.089 | 15 (88.2%) | 2 (11.8%) | 0.008 d | 15 (5.8%) | 12.33 ± 2.1 | 0.811 |
| No | 436 (96.2%) | 52.98 ± 29.1 | 242 (55.5%) | 194 (44.5%) | 242 (94.2%) | 12.14 ± 3.0 | ||||
| Smoking status | Yes (current/former) | 127 (28%) | 56.61 ± 30.3 | 0.151 | 65 (51.2%) | 62 (48.8%) | 0.137 | 65 (25.3%) | 12.43 ± 2.7 | 0.386 |
| No | 326 (72%) | 52.21 ± 28.8 | 192 (58.9%) | 134 (41.1%) | 192 (74.7%) | 12.06 ± 3.0 | ||||
| HPV, HPV-OPSCC and Vaccine Knowledge Questions | Assessment of HPV Infection and HPV-OPSCC Knowledge n (%) | |
|---|---|---|
| Correct | Incorrect | |
| Understanding of HPV types (low-risk and high-risk) | 280 (61.8%) | 173 (38.2%) |
| HPV’s link to cervical cancer and OPSCC | 282 (62.3%) | 171 (37.7%) |
| High-risk HPV link (HPV type 16) to OPSCC | 226 (49.9%) | 227 (50.1%) |
| Global Increase in HPV-Associated OPSCC Prevalence | 203 (44.8%) | 250 (55.2%) |
| HPV-OPSCC has clear clinical signs and symptoms | 215 (47.5%) | 238 (52.5%) |
| Improved prognosis for HPV-OPSCC | 177 (39.1%) | 276 (60.9%) |
| Spread of HPV infection | 329 (72.6%) | 124 (27.4%) |
| Common sites for the onset of HPV-OPSCC | 213 (47.0%) | 240 (53.0%) |
| HPV vaccine awareness | 257 (56.7%) | 196 (43.3%) |
| Suitable age for the HPV vaccine * | 164 (63.8%) | 93 (36.2%) |
| HPV Vaccine Knowledge | Total n (%) | HPV-OPSCC Knowledge | p-Value | |
|---|---|---|---|---|
| Awareness of the HPV vaccine (n = 453) | Yes | 257 (56.7%) | 56.03 ± 28.6 | 0.031 a |
| No | 196 (43.3%) | 50.05 ± 30.0 | ||
| Received HPV vaccination previously (n = 257) | Yes | 60 (23.3%) | 59.33 ± 28.5 | 0.307 |
| No | 197 (76.7%) | 55.03 ± 28.6 | ||
| Suitable age for the HPV vaccine (n = 257) | Yes | 93 (36.2%) | 67.53 ± 27.6 | 0.001 a |
| No | 164 (63.8%) | 49.51 ± 27.1 | ||
| Dependent Variable: HPV Knowledge | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | B | S.E. | 95% C.I. | p-Value | |||
| Lower Bound | Upper Bound | ||||||
| Intercept | 4.838 | 15.197 | −25.031 | 34.706 | 0.750 | ||
| Age | <20 | 44.899 | 16.875 | 11.733 | 78.065 | 0.008 a | |
| 20–25 | 44.944 | 15.670 | 14.145 | 75.742 | 0.004 a | ||
| 25–30 | 37.966 | 15.931 | 6.654 | 69.277 | 0.018 a | ||
| Grade point average | <2.99 | −9.802 | 10.069 | −29.591 | 9.987 | 0.331 | |
| 3–3.49 | −7.943 | 4.781 | −17.340 | 1.454 | 0.097 | ||
| 3.50–3.99 | −10.082 | 3.699 | −17.351 | −2.812 | 0.007 a | ||
| 4.4–4.9 | −8.590 | 3.107 | −14.697 | −2.482 | 0.006 a | ||
| Dependent Variable: HPV Vaccine Knowledge | |||||||
| Variables in Equation | B | S.E. | Exp (B) | 95% C.I. for Exp (B) | p-Value | ||
| Lower | Upper | ||||||
| Step 1 b | Gender (Male) | 0.479 | 0.194 | 1.614 | 1.104 | 2.360 | 0.013 c |
| History of sexually transmitted disease (Yes) | −1.859 | 0.762 | 0.156 | 0.035 | 0.694 | 0.015 c | |
| Constant | −0.431 | 0.130 | 0.650 | 0.001 c | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsharif, M.T.; Alsahafi, E. Assessing the Knowledge of HPV-Associated Oropharyngeal Squamous Cell Carcinoma, HPV Vaccination, and Practice Scope among Saudi Dental Students in the Western Region. Healthcare 2024, 12, 905. https://doi.org/10.3390/healthcare12090905
Alsharif MT, Alsahafi E. Assessing the Knowledge of HPV-Associated Oropharyngeal Squamous Cell Carcinoma, HPV Vaccination, and Practice Scope among Saudi Dental Students in the Western Region. Healthcare. 2024; 12(9):905. https://doi.org/10.3390/healthcare12090905
Chicago/Turabian StyleAlsharif, Maha T., and Elham Alsahafi. 2024. "Assessing the Knowledge of HPV-Associated Oropharyngeal Squamous Cell Carcinoma, HPV Vaccination, and Practice Scope among Saudi Dental Students in the Western Region" Healthcare 12, no. 9: 905. https://doi.org/10.3390/healthcare12090905
APA StyleAlsharif, M. T., & Alsahafi, E. (2024). Assessing the Knowledge of HPV-Associated Oropharyngeal Squamous Cell Carcinoma, HPV Vaccination, and Practice Scope among Saudi Dental Students in the Western Region. Healthcare, 12(9), 905. https://doi.org/10.3390/healthcare12090905






