Association between Changes in Daily Life Due to COVID-19 and Depressive Symptoms in South Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. Independent Variables
2.2.1. Sociodemographic Characteristics
2.2.2. Health-Related Characteristics
2.2.3. Changes in Daily Life Due to the COVID-19 Pandemic
2.3. Dependent Variables: Depressive Symptoms
2.4. Statistical Analysis
3. Results
3.1. Depressive Symptoms according to Sociodemographic and Health-Related Characteristics
3.2. Depressive Symptoms according to Changes in Daily Life Due to COVID-19
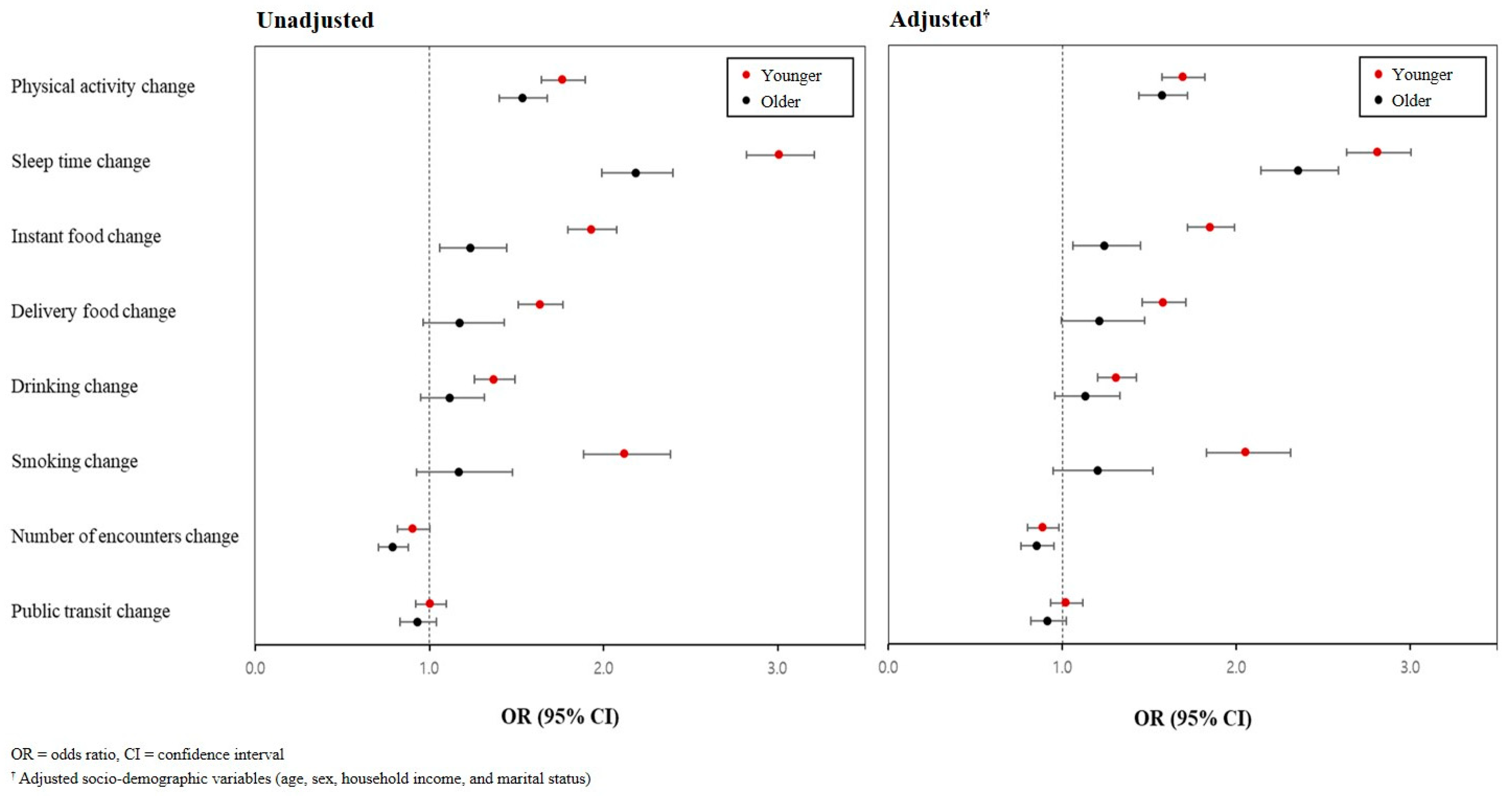
3.3. Factors Causing Changes in Daily Life Due to the COVID-19 Pandemic Associated with Depressive Symptoms
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Alzueta, E.; Perrin, P.; Baker, F.C.; Caffarra, S.; Ramos-Usuga, D.; Yuksel, D.; Arango-Lasprilla, J.C. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. J. Clin. Psychol. 2021, 77, 556–570. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, D.; Meldgaard, J.; Hulvej Rod, M. Altered self-observations, unclear risk perceptions and changes in relational everyday life: A qualitative study of psychosocial life with diabetes during the COVID-19 lockdown. Societies 2020, 10, 63. [Google Scholar] [CrossRef]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental health in the COVID-19 pandemic. Q. J. Med. 2020, 113, 311–312. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef] [PubMed]
- McKeever, A.; Agius, M.; Mohr, P. A Review of the epidemiology of major depressive disorder and of its consequences for society and the individual. Psychiatr Danub. 2017, 29 (Suppl. S3), 222–231. [Google Scholar] [PubMed]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef]
- Kim, S.W.; Park, I.H.; Kim, M.; Park, A.L.; Jhon, M.; Kim, J.W.; Kang, H.J.; Ryu, S.; Lee, J.Y.; Kim, J.M. Risk and protective factors of depression in the general population during the COVID-19 epidemic in Korea. BMC Psychiatry 2021, 21, 445. [Google Scholar] [CrossRef]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. Announcement of the Results of the “Corona 19 National Mental Health Survey” in the Second Quarter of 2021; Ministry of Health and Welfare: Seoul, Republic of Korea, 2021.
- Mihashi, M.; Otsubo, Y.; Yinjuan, X.; Nagatomi, K.; Hoshiko, M.; Ishitake, T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychol. 2009, 28, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.W.; Ko, Y.S.; Kim, Y.J.; Sung, K.M.; Kim, H.J.; Choi, H.Y.; Sung, C.; Jeong, E. Korea community health survey data profiles. Osong. Public Health Res. Perspect. 2015, 6, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.S.; Choi, J.H.; Park, K.H.; Joo, K.J.; Ga, H.; Ko, H.J.; Kim, S.R. Standardization of the Korean Version of Patient Health Questionnaire-9 as a Screening Instrument for Major Depressive Disorder. J. Korean Acad. Fam. Med. 2007, 28, 114–119. [Google Scholar]
- Shin, C.; Lee, S.H.; Han, K.M.; Yoon, H.K.; Han, C. Comparison of the usefulness of the PHQ-8 and PHQ-9 for screening for major depressive disorder: Analysis of psychiatric outpatient data. Psychiatry Investig. 2019, 16, 300–305. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Rebar, A.L.; Stanton, R.; Geard, D.; Short, C.; Duncan, M.J.; Vandelanotte, C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 2015, 9, 366–378. [Google Scholar] [CrossRef]
- Vorvolakos, T.; Leontidou, E.; Tsiptsios, D.; Mueller, C.; Serdari, A.; Terzoudi, A.; Nena, E.; Tsamakis, K.; Constantinidis, T.C.; Tripsianis, G. The association between sleep pathology and depression: A cross-sectional study among adults in Greece. Psychiatry Res. 2020, 294, 113502. [Google Scholar] [CrossRef]
- Fawale, M.B.; Ismaila, I.A.; Mustapha, A.F.; Komolafe, M.A.; Ibigbami, O. Correlates of sleep quality and sleep duration in a sample of urban-dwelling elderly Nigerian women. Sleep Health 2017, 3, 257–262. [Google Scholar] [CrossRef]
- Hisler, G.C.; Twenge, J.M. Sleep characteristics of U.S. adults before and during the COVID-19 pandemic. Soc. Sci. Med. 2021, 276, 113849. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004, 27, 1255–1273. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lv, M.R.; Wei, Y.J.; Sun, L.; Zhang, J.X.; Zhang, H.G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhou, Y.; Chen, K.; Jing, Y.; He, J.; Sun, H.; Hu, X. Dietary inflammatory index and depression: A meta-analysis. Public Health Nutr. 2019, 22, 654–660. [Google Scholar] [CrossRef]
- Kim, M.-H.; Yeon, J.-Y. Change of dietary habits and the use of home meal replacement and delivered foods due to COVID-19 among college students in Chungcheong province, Korea. J. Nutr. Health 2021, 54, 383–397. [Google Scholar] [CrossRef]
- Dvorak, R.D.; Sargent, E.M.; Kilwein, T.M.; Stevenson, B.L.; Kuvaas, N.J.; Williams, T.J. Alcohol use and alcohol-related consequences: Associations with emotion regulation difficulties. Am. J. Drug Alcohol Abus. 2014, 40, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Minichino, A.; Bersani, F.S.; Calò, W.K.; Spagnoli, F.; Francesconi, M.; Vicinanza, R.; Delle Chiaie, R.; Biondi, M. Smoking behaviour and mental health disorders--mutual influences and implications for therapy. Int. J. Environ. Res. Public Health 2013, 10, 4790–47811. [Google Scholar] [CrossRef] [PubMed]
- Busse, H.; Buck, C.; Stock, C.; Zeeb, H.; Pischke, C.R.; Fialho, P.M.M.; Wendt, C.; Helmer, S.M. Engagement in health risk behaviours before and during the COVID-19 pandemic in German university students: Results of a cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 1410. [Google Scholar] [CrossRef] [PubMed]
- Guignard, R.; Andler, R.; Quatremère, G.; Pasquereau, A.; du Roscoät, E.; Arwidson, P.; Berlin, I.; Nguyen-Thanh, V. Changes in smoking and alcohol consumption during COVID-19-related lockdown: A cross-sectional study in France. Eur. J. Public Health 2021, 31, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Clay, J.M.; Parker, M.O. Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? Lancet Public Health 2020, 5, e259. [Google Scholar] [CrossRef]
- Lee, S.Y.; Kim, S.; Kim, W.H.; Heo, J. Employment, economic, and sociodemographic factors associated with changes in smoking and drinking behaviors during the COVID-19 pandemic in South Korea. Int. J. Environ. Res. Public Health 2022, 19, 2802. [Google Scholar] [CrossRef]
| Variables | Younger (≤64 Years) | Older (≥65 Years) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Depressed | Non-Depressed | p-Value | Total | Depressed | Non-Depressed | p-Value | |||||
| N (Column %) | N | % | N | % | N (Column %) | N | % | N | % | |||
| Total (N = 228,485) | 156,150 | 3901 | 2.5 | 152,249 | 97.5 | 72,335 | 2535 | 3.5 | 69,800 | 96.5 | ||
| Sex | <0.001 | <0.001 | ||||||||||
| Male | 73,422 (47.0) | 1316 | 1.8 | 72,106 | 98.2 | 30,182 (41.7) | 700 | 2.3 | 29,482 | 97.7 | ||
| Female | 82,728 (53.0) | 2585 | 3.1 | 80,143 | 96.9 | 42,153 (58.3) | 1835 | 4.4 | 40,318 | 95.7 | ||
| Residence | <0.001 | <0.001 | ||||||||||
| Urban | 99,019 (63.4) | 2742 | 2.8 | 96,277 | 97.2 | 29,678 (41.0) | 1129 | 3.8 | 28,549 | 96.2 | ||
| Rural | 57,131 (36.6) | 1159 | 2.0 | 55,972 | 98.0 | 42,657 (59.0) | 1406 | 3.3 | 41,251 | 96.7 | ||
| Household income, monthly (KRW 10,000) | <0.001 | <0.001 | ||||||||||
| <300 | 38,499 (24.7) | 1552 | 4.0 | 36,947 | 96.0 | 50,466 (69.8) | 2021 | 4.0 | 48,445 | 96.0 | ||
| 300 to <500 | 37,173 (23.8) | 797 | 2.1 | 36,376 | 97.9 | 7462 (10.3) | 179 | 2.4 | 7283 | 97.6 | ||
| ≥500 | 80,478 (51.5) | 1552 | 1.9 | 78,926 | 98.1 | 14,407 (19.9) | 335 | 2.3 | 14,072 | 97.7 | ||
| Educational level | <0.001 | <0.001 | ||||||||||
| ≤Middle school | 21,360 (13.7) | 676 | 3.2 | 20,684 | 96.8 | 54,344 (75.1) | 2173 | 4.0 | 52,171 | 96.0 | ||
| High school | 54,240 (34.7) | 1475 | 2.7 | 52,765 | 97.3 | 12,165 (16.8) | 275 | 2.3 | 11,890 | 97.7 | ||
| ≥College | 80,383 (51.5) | 1747 | 2.2 | 78,636 | 97.8 | 5731 (7.9) | 85 | 1.5 | 5646 | 98.5 | ||
| Marital status | <0.001 | <0.001 | ||||||||||
| Living with spouse | 98,115 (62.8) | 1777 | 1.8 | 96,338 | 98.2 | 44,949 (62.1) | 1125 | 2.5 | 43,824 | 97.5 | ||
| Living without spouse | 57,943 (37.1) | 2119 | 3.7 | 55,824 | 96.3 | 27,358 (37.8) | 1409 | 5.2 | 25,949 | 94.9 | ||
| Smoking (current) | <0.001 | 0.804 | ||||||||||
| No | 124,933 (80.0) | 2855 | 2.3 | 122,078 | 97.7 | 66,233 (91.6) | 2318 | 3.5 | 63,915 | 96.5 | ||
| Yes | 31,201 (20.0) | 1046 | 3.4 | 30,155 | 96.7 | 6094 (8.4) | 217 | 3.6 | 5877 | 96.4 | ||
| Drinking (current) | 0.049 | <0.001 | ||||||||||
| No | 47,836 (30.6) | 1251 | 2.6 | 46,585 | 97.4 | 48,558 (67.1) | 2010 | 4.1 | 46,548 | 95.9 | ||
| Yes | 108,302 (69.4) | 2650 | 2.5 | 105,652 | 97.6 | 23,772 (32.9) | 525 | 2.2 | 23,247 | 97.8 | ||
| Hypertension | <0.001 | <0.001 | ||||||||||
| No | 131,430 (84.2) | 3186 | 2.4 | 128,244 | 97.6 | 33,337 (46.1) | 1031 | 3.1 | 32,306 | 96.9 | ||
| Yes | 24,710 (15.8) | 714 | 2.9 | 23,996 | 97.1 | 38,985 (53.9) | 1503 | 3.9 | 37,482 | 96.1 | ||
| Diabetes Mellitus | <0.001 | <0.001 | ||||||||||
| No | 145,444 (93.1) | 3490 | 2.4 | 141,954 | 97.6 | 56,325 (77.9) | 1825 | 3.2 | 54,500 | 96.8 | ||
| Yes | 10,697 (6.9) | 411 | 3.8 | 10,286 | 96.2 | 15,998 (22.1) | 708 | 4.4 | 15,290 | 95.6 | ||
| Eating breakfast | <0.001 | <0.001 | ||||||||||
| >2 times/week | 53,730 (34.4) | 1977 | 3.7 | 51,753 | 96.3 | 2568 (3.6) | 216 | 8.4 | 2352 | 91.6 | ||
| ≤2 times/week | 102,416 (65.6) | 1923 | 1.9 | 100,493 | 98.1 | 69,767 (96.4) | 2319 | 3.3 | 67,448 | 96.7 | ||
| Moderate to vigorous physical activity | <0.001 | <0.001 | ||||||||||
| ≥150 min/week | 47,809 (30.6) | 986 | 2.1 | 46,823 | 97.9 | 15,314 (21.2) | 265 | 1.7 | 15,049 | 98.3 | ||
| <150 min/week | 108,278 (69.3) | 2914 | 2.7 | 105,364 | 97.3 | 56,933 (78.7) | 2267 | 4.0 | 54,666 | 96.0 | ||
| Sleep time (weekdays) | <0.001 | <0.001 | ||||||||||
| ≥7 h | 90,686 (58.1) | 1629 | 1.8 | 89,057 | 98.2 | 38,900 (53.8) | 875 | 2.3 | 38,025 | 97.8 | ||
| <7 h | 65,464 (41.9) | 2272 | 3.5 | 63,192 | 96.5 | 33,435 (46.2) | 1660 | 5.0 | 31,775 | 95.0 | ||
| Perceived stress | <0.001 | <0.001 | ||||||||||
| Low | 115,756 (74.1) | 734 | 0.6 | 115,022 | 99.4 | 62,144 (85.9) | 1055 | 1.7 | 61,089 | 98.3 | ||
| High | 40,386 (25.9) | 3166 | 7.8 | 37,220 | 92.2 | 10,161 (14.0) | 1475 | 14.5 | 8686 | 85.5 | ||
| Variables | Younger (≤64 Years) | Older (≥65 Years) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Depressed | Non-Depressed | p-Value | Total | Depressed | Non-Depressed | p-Value | |||||
| N (Column %) | N | % | N | % | N (Column %) | N | % | N | % | |||
| Total (N = 228,485) | 156,150 | 3901 | 2.5 | 152,249 | 97.5 | 72,335 | 2535 | 3.5 | 69,800 | 96.5 | ||
| Physical activity | <0.001 | <0.001 | ||||||||||
| Increased | 8961 (5.7) | 210 | 2.3 | 8751 | 97.7 | 2762 (3.8) | 57 | 2.1 | 2705 | 97.9 | ||
| Similar | 63,331 (40.6) | 1086 | 1.7 | 62,245 | 98.3 | 38,829 (53.7) | 1006 | 2.6 | 37,823 | 97.4 | ||
| Decreased | 74,056 (47.4) | 2268 | 3.1 | 71,788 | 96.9 | 22,688 (31.4) | 939 | 4.1 | 21,749 | 95.9 | ||
| Not applicable | 9792 (6.3) | 336 | 3.4 | 9456 | 96.6 | 8038 (11.1) | 530 | 6.6 | 7508 | 93.4 | ||
| Sleep time | <0.001 | <0.001 | ||||||||||
| Increased | 18,321 (11.7) | 642 | 3.5 | 17,679 | 96.5 | 5030 (7.0) | 200 | 4.0 | 4830 | 96.0 | ||
| Similar | 122,930 (78.7) | 2185 | 1.8 | 120,745 | 98.2 | 62,795 (86.8) | 1920 | 3.1 | 60,875 | 96.9 | ||
| Decreased | 14,892 (9.5) | 1073 | 7.2 | 13,819 | 92.8 | 4502 (6.2) | 414 | 9.2 | 4088 | 90.8 | ||
| Instant food | <0.001 | <0.001 | ||||||||||
| Increased | 26,467 (16.9) | 1109 | 4.2 | 25,358 | 95.8 | 992 (1.4) | 56 | 5.7 | 936 | 94.4 | ||
| Similar | 76,362 (48.9) | 1479 | 1.9 | 74,883 | 98.1 | 22,216 (30.7) | 663 | 3.0 | 21,553 | 97.0 | ||
| Decreased | 14,818 (9.5) | 408 | 2.8 | 14,410 | 97.3 | 5044 (7.0) | 165 | 3.3 | 4879 | 96.7 | ||
| Not applicable | 38,469 (24.6) | 904 | 2.4 | 37,565 | 97.7 | 44,046 (60.9) | 1651 | 3.8 | 42,395 | 96.3 | ||
| Delivery food | <0.001 | <0.001 | ||||||||||
| Increased | 45,114 (28.9) | 1438 | 3.2 | 43,676 | 96.8 | 1440 (2.0) | 52 | 3.6 | 1388 | 96.4 | ||
| Similar | 52,380 (33.5) | 1001 | 1.9 | 51,379 | 98.1 | 12,090 (16.7) | 323 | 2.7 | 11,767 | 97.3 | ||
| Decreased | 11,978 (7.7) | 324 | 2.7 | 11,654 | 97.3 | 3430 (4.7) | 100 | 2.9 | 3330 | 97.1 | ||
| Not applicable | 46,650 (29.9) | 1138 | 2.4 | 45,512 | 97.6 | 55,330 (76.5) | 2059 | 3.7 | 53,271 | 96.3 | ||
| Drinking | <0.001 | <0.001 | ||||||||||
| Increased | 6921 (4.4) | 426 | 6.2 | 6495 | 93.8 | 594 (0.8) | 30 | 5.1 | 564 | 95.0 | ||
| Similar | 48,524 (31.1) | 961 | 2.0 | 47,563 | 98.0 | 14,065 (19.4) | 322 | 2.3 | 13,743 | 97.7 | ||
| Decreased | 42,457 (27.2) | 904 | 2.1 | 41,553 | 97.9 | 10,111 (14.0) | 243 | 2.4 | 9868 | 97.6 | ||
| Not applicable | 58,209 (37.3) | 1608 | 2.8 | 56,601 | 97.2 | 47,528 (65.7) | 1939 | 4.1 | 45,589 | 95.9 | ||
| Smoking | <0.001 | 0.003 | ||||||||||
| Increased | 3630 (2.3) | 317 | 8.7 | 3313 | 91.3 | 334 (0.5) | 16 | 4.8 | 318 | 95.2 | ||
| Similar | 28,881 (18.5) | 682 | 2.4 | 28,199 | 97.6 | 6924 (9.6) | 196 | 2.8 | 6728 | 97.2 | ||
| Decreased | 6987 (4.5) | 201 | 2.9 | 6786 | 97.1 | 3160 (4.4) | 99 | 3.1 | 3061 | 96.9 | ||
| Not applicable | 116,605 (74.7) | 2699 | 2.3 | 113,906 | 97.7 | 61,878 (85.5) | 2223 | 3.6 | 59,655 | 96.4 | ||
| Number of encounters | <0.001 | <0.001 | ||||||||||
| Increased | 479 (0.3) | 26 | 5.4 | 453 | 94.6 | 228 (0.3) | 9 | 4.0 | 219 | 96.1 | ||
| Similar | 16,768 (10.7) | 431 | 2.6 | 16,337 | 97.4 | 11,178 (15.5) | 425 | 3.8 | 10,753 | 96.2 | ||
| Decreased | 131,948 (84.5) | 3060 | 2.3 | 128,888 | 97.7 | 55,197 (76.3) | 1660 | 3.0 | 53,537 | 97.0 | ||
| Not applicable | 6946 (4.4) | 384 | 5.5 | 6562 | 94.5 | 5723 (7.9) | 441 | 7.7 | 5282 | 92.3 | ||
| Public transit | <0.001 | 0.024 | ||||||||||
| Increased | 1149 (0.7) | 69 | 6.0 | 1080 | 94.0 | 267 (0.4) | 15 | 5.6 | 252 | 94.4 | ||
| Similar | 26,606 (17.0) | 776 | 2.9 | 25,830 | 97.1 | 12,014 (16.6) | 457 | 3.8 | 11,557 | 96.2 | ||
| Decreased | 45,973 (29.4) | 1311 | 2.9 | 44,662 | 97.2 | 32,305 (44.7) | 1140 | 3.5 | 31,165 | 96.5 | ||
| Not applicable | 82,412 (52.8) | 1745 | 2.1 | 80,667 | 97.9 | 27,741 (38.4) | 922 | 3.3 | 26,819 | 96.7 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Son, H.-E.; Hong, Y.-S.; Son, H. Association between Changes in Daily Life Due to COVID-19 and Depressive Symptoms in South Korea. Healthcare 2024, 12, 840. https://doi.org/10.3390/healthcare12080840
Son H-E, Hong Y-S, Son H. Association between Changes in Daily Life Due to COVID-19 and Depressive Symptoms in South Korea. Healthcare. 2024; 12(8):840. https://doi.org/10.3390/healthcare12080840
Chicago/Turabian StyleSon, Ha-Eun, Young-Seoub Hong, and Hyunjin Son. 2024. "Association between Changes in Daily Life Due to COVID-19 and Depressive Symptoms in South Korea" Healthcare 12, no. 8: 840. https://doi.org/10.3390/healthcare12080840
APA StyleSon, H.-E., Hong, Y.-S., & Son, H. (2024). Association between Changes in Daily Life Due to COVID-19 and Depressive Symptoms in South Korea. Healthcare, 12(8), 840. https://doi.org/10.3390/healthcare12080840







