Relation between Photogrammetry and Spinal Mouse for Lumbopelvic Assessment in Adolescents with Thoracic Kyphosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
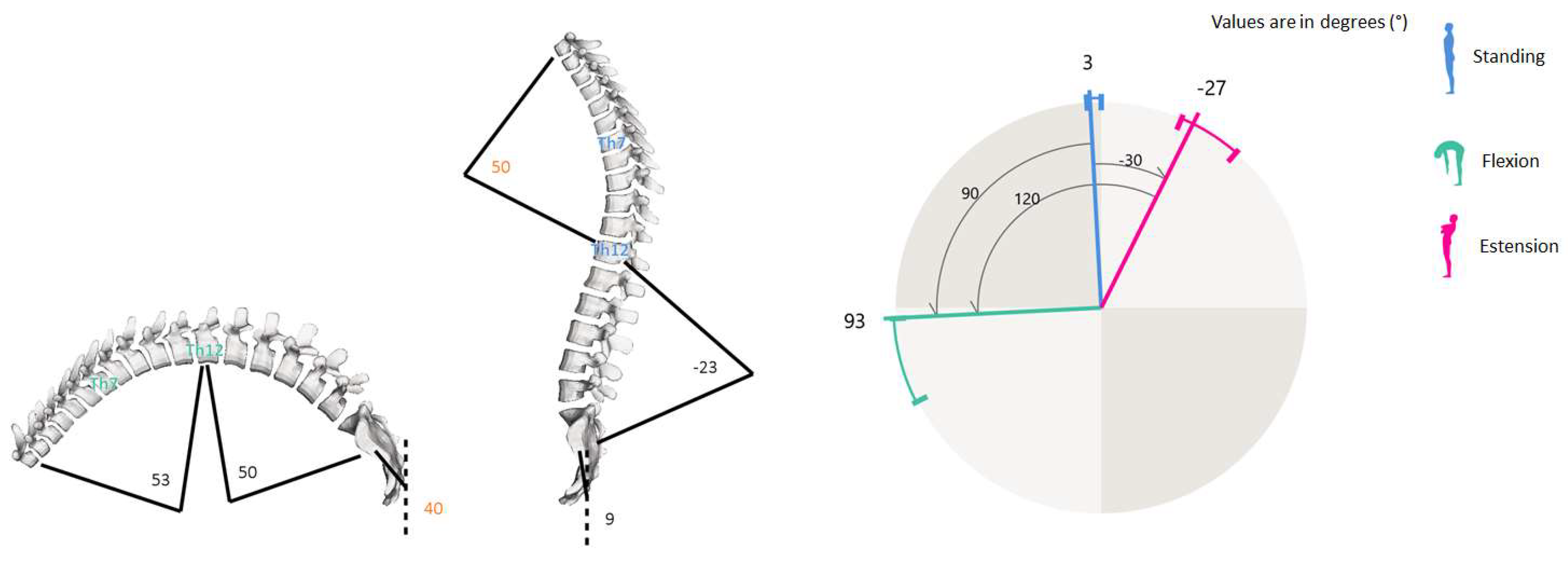
2.2. Measurement Instruments
2.2.1. Spine Analysis
2.2.2. Photogrammetric Postural Analysis
2.3. Statistical Analysis
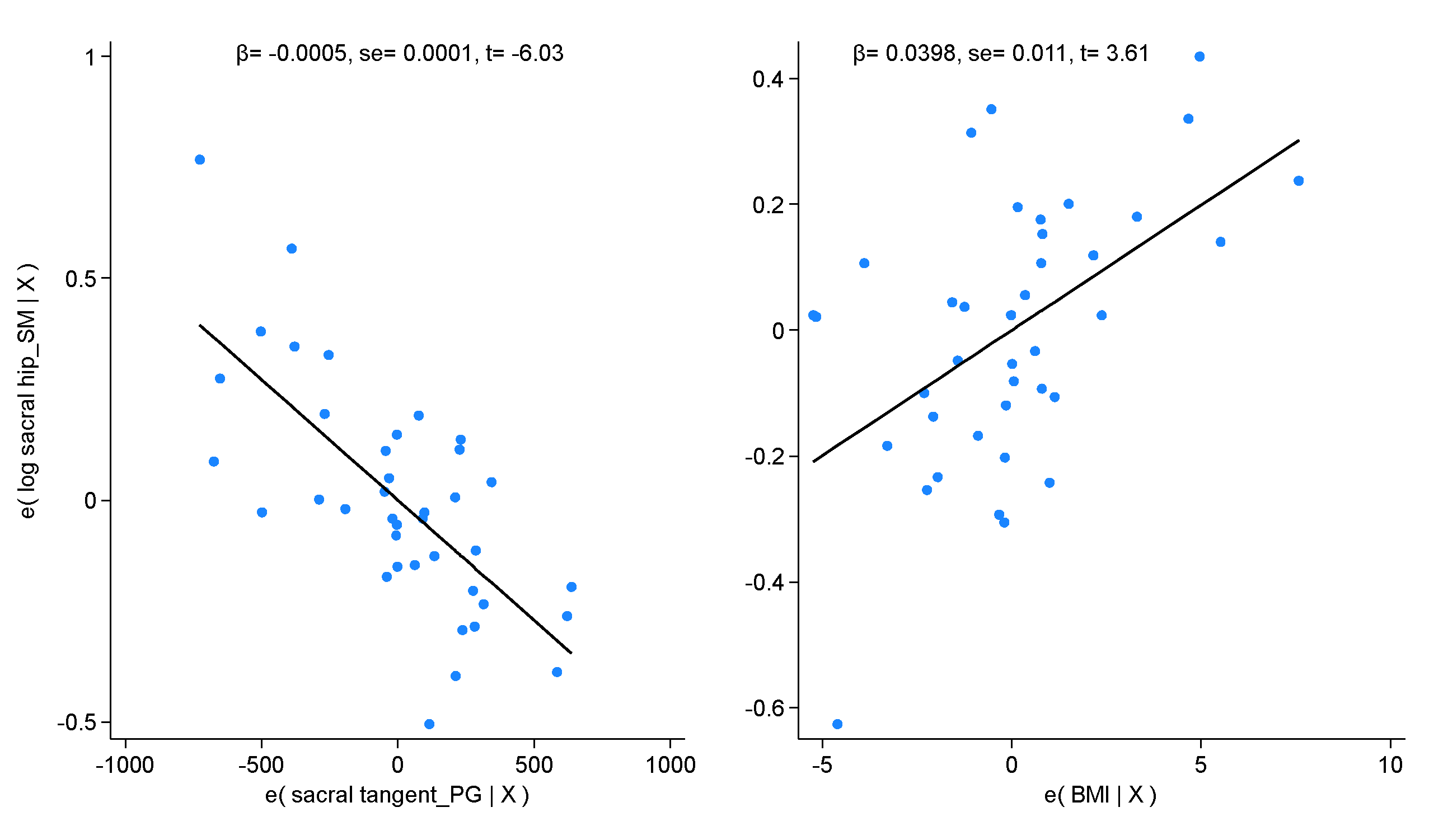
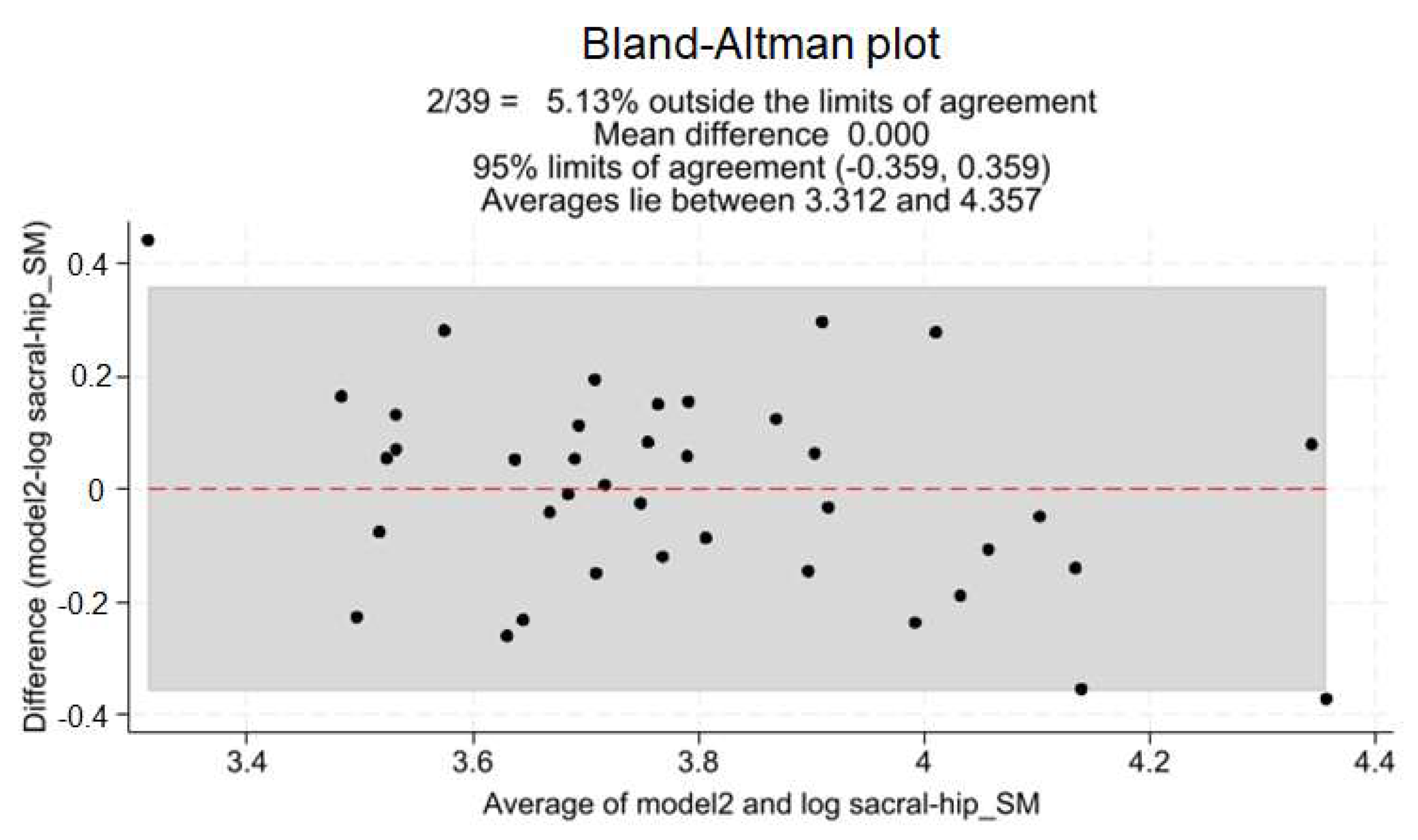
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sahrmann, S. Diagnosis and Treatment of Movement Impairment Syndromes, 1st ed.; Mosby: St. Louis, MO, USA, 2001; ISBN 978-0-8016-7205-7. [Google Scholar]
- Kibler, W.B.; Press, J.; Sciascia, A. The Role of Core Stability in Athletic Function. Sports Med. 2006, 36, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Willson, J.D.; Dougherty, C.P.; Ireland, M.L.; Davis, I.M. Core Stability and Its Relationship to Lower Extremity Function and Injury. J. Am. Acad. Orthop. Surg. 2005, 13, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.A.; Lucett, S.C.; Sutton, B.G. NASM Essentials of Corrective Exercise Training; Jones & Bartlett Learning: Burlington, MA, USA, 2013; ISBN 978-1-284-05025-7. [Google Scholar]
- Anderson, G.S.; Deluigi, F.; Belli, G.; Tentoni, C.; Gaetz, M.B. Training for Improved Neuro-Muscular Control of Balance in Middle Aged Females. J. Bodyw. Mov. Ther. 2016, 20, 10–18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zazulak, B.; Cholewicki, J.; Reeves, N.P. Neuromuscular Control of Trunk Stability: Clinical Implications for Sports Injury Prevention. J. Am. Acad. Orthop. Surg. 2008, 16, 497–505. [Google Scholar] [CrossRef] [PubMed]
- De Blaiser, C.; Roosen, P.; Willems, T.; Danneels, L.; Bossche, L.V.; De Ridder, R. Is Core Stability a Risk Factor for Lower Extremity Injuries in an Athletic Population? A Systematic Review. Phys. Ther. Sport 2018, 30, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Sun, Z.; Guo, Z.; Qi, Q.; Kim, S.D.; Zeng, Y.; Sun, C.; Chen, Z. Analysis of Spinopelvic Sagittal Alignment in Patients With Thoracic and Thoracolumbar Angular Kyphosis. Spine 2013, 38, E813–E818. [Google Scholar] [CrossRef] [PubMed]
- Le Huec, J.C.; Thompson, W.; Mohsinaly, Y.; Barrey, C.; Faundez, A. Sagittal Balance of the Spine. Eur. Spine J. 2019, 28, 1889–1905. [Google Scholar] [CrossRef]
- Charles, Y.P.; Lamas, V.; Ilharreborde, B.; Blondel, B.; Prost, S.; Bauduin, E.; Laouissat, F.; Riouallon, G.; Wolff, S.; Challier, V.; et al. Comparison of Spinopelvic Configuration and Roussouly Alignment Types Between Pediatric and Adult Populations. Spine 2022, 47, 1303–1313. [Google Scholar] [CrossRef]
- Prost, S.; Charles, Y.-P.; Ilharreborde, B.; Riouallon, G.; Pesenti, S.; Blondel, B.; on behalf of the French Spine Surgery Society (SFCR). Thoracolumbar Sagittal Shape Varies With Pelvic Morphology and Aging. Spine 2023, 48, 1726–1732. [Google Scholar] [CrossRef]
- Roussouly, P.; Nnadi, C. Sagittal Plane Deformity: An Overview of Interpretation and Management. Eur. Spine J. 2010, 19, 1824–1836. [Google Scholar] [CrossRef]
- Abelin-Genevois, K. Sagittal Balance of the Spine. Orthop. Traumatol. Surg. Res. 2021, 107, 102769. [Google Scholar] [CrossRef]
- Maria, C.-W.; Patryk, W.; Mateusz, Ż.; Marcin, T. Is Sagittal Spinopelvic Alignment a Cause of Low Back Pain in Pediatric Spine Pathologies? A Review. J. Child. Orthop. 2023, 17, 548–555. [Google Scholar] [CrossRef]
- Vrtovec, T.; Janssen, M.M.A.; Likar, B.; Castelein, R.M.; Viergever, M.A.; Pernuš, F. A Review of Methods for Evaluating the Quantitative Parameters of Sagittal Pelvic Alignment. Spine J. 2012, 12, 433–446. [Google Scholar] [CrossRef] [PubMed]
- Cohen, L.; Kobayashi, S.; Simic, M.; Dennis, S.; Refshauge, K.; Pappas, E. Non-Radiographic Methods of Measuring Global Sagittal Balance: A Systematic Review. Scoliosis 2017, 12, 30. [Google Scholar] [CrossRef]
- Molinaro, L.; Russo, L.; Cubelli, F.; Taborri, J.; Rossi, S. Reliability Analysis of an Innovative Technology for the Assessment of Spinal Abnormalities. In Proceedings of the 2022 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Messina, Italy, 22–24 June 2022; pp. 1–6. [Google Scholar]
- Belli, G.; Toselli, S.; Latessa, P.M.; Mauro, M. Evaluation of Self-Perceived Body Image in Adolescents with Mild Idiopathic Scoliosis. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 319–333. [Google Scholar] [CrossRef]
- Belli, G.; Toselli, S.; Mauro, M.; Maietta Latessa, P.; Russo, L. Relation between Photogrammetry and Spinal Mouse for Sagittal Imbalance Assessment in Adolescents with Thoracic Kyphosis. J. Funct. Morphol. Kinesiol. 2023, 8, 68. [Google Scholar] [CrossRef] [PubMed]
- Kellis, E.; Adamou, G.; Tzilios, G.; Emmanouilidou, M. Reliability of Spinal Range of Motion in Healthy Boys Using a Skin-Surface Device. J. Manip. Physiol. Ther. 2008, 31, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.; McCreesh, K.; Lewis, J. Reliability and Validity of Non-Radiographic Methods of Thoracic Kyphosis Measurement: A Systematic Review. Man. Ther. 2014, 19, 10–17. [Google Scholar] [CrossRef]
- Muyor, J.M.; López-Miñarro, P.A.; Alacid, F. The Relationship Between Hamstring Muscle Extensibility and Spinal Postures Varies with the Degree of Knee Extension. J. Appl. Biomech. 2013, 29, 678–686. [Google Scholar] [CrossRef]
- Muyor, J.M.; López-Miñarro, P.A. Comparison of Sagittal Spinal Curvatures and Pelvic Tilt in Highly Trained Athletes from Different Sport Disciplines. Kinesiology 2017, 49, 109–116. [Google Scholar] [CrossRef]
- Saad, K.R.; Colombo, A.S.; Ribeiro, A.P.; João, S.M.A. Reliability of Photogrammetry in the Evaluation of the Postural Aspects of Individuals with Structural Scoliosis. J. Bodyw. Mov. Ther. 2012, 16, 210–216. [Google Scholar] [CrossRef]
- Trovato, B.; Roggio, F.; Sortino, M.; Zanghì, M.; Petrigna, L.; Giuffrida, R.; Musumeci, G. Postural Evaluation in Young Healthy Adults through a Digital and Reproducible Method. J. Funct. Morphol. Kinesiol. 2022, 7, 98. [Google Scholar] [CrossRef] [PubMed]
- Krawczky, B.; Pacheco, A.G.; Mainenti, M.R.M. A Systematic Review of the Angular Values Obtained by Computerized Photogrammetry in Sagittal Plane: A Proposal for Reference Values. J. Manip. Physiol. Ther. 2014, 37, 269–275. [Google Scholar] [CrossRef]
- Mannion, A.F.; Knecht, K.; Balaban, G.; Dvorak, J.; Grob, D. A New Skin-Surface Device for Measuring the Curvature and Global and Segmental Ranges of Motion of the Spine: Reliability of Measurements and Comparison with Data Reviewed from the Literature. Eur. Spine J. 2004, 13, 122–136. [Google Scholar] [CrossRef]
- Post, R.B.; Leferink, V.J.M. Spinal Mobility: Sagittal Range of Motion Measured with the SpinalMouse, a New Non-Invasive Device. Arch. Orthop. Trauma Surg. 2004, 124, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Singla, D.; Veqar, Z.; Hussain, M.E. Photogrammetric Assessment of Upper Body Posture Using Postural Angles: A Literature Review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef]
- Azadinia, F.; Hosseinabadi, M.; Ebrahimi, I.; Mohseni-Bandpei, M.-A.; Ghandhari, H.; Yassin, M.; Behtash, H.; Ganjavian, M.-S. Validity and Test–Retest Reliability of Photogrammetry in Adolescents with Hyperkyphosis. Physiother. Theory Pract. 2022, 38, 3018–3026. [Google Scholar] [CrossRef]
- Stolinski, L.; Kozinoga, M.; Czaprowski, D.; Tyrakowski, M.; Cerny, P.; Suzuki, N.; Kotwicki, T. Two-Dimensional Digital Photography for Child Body Posture Evaluation: Standardized Technique, Reliable Parameters and Normative Data for Age 7-10 Years. Scoliosis 2017, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Dodge, Y. The Concise Encyclopedia of Statistics, 2010th ed.; Springer: Philadelphia, PA, USA, 2008; ISBN 978-0-397-51837-1. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Ludwig, O.; Dindorf, C.; Kelm, J.; Simon, S.; Nimmrichter, F.; Fröhlich, M. Reference Values for Sagittal Clinical Posture Assessment in People Aged 10 to 69 Years. Int. J. Environ. Res. Public Health 2023, 20, 4131. [Google Scholar] [CrossRef]
- Macedo Ribeiro, A.F.; Bergmann, A.; Lemos, T.; Pacheco, A.G.; Mello Russo, M.; Santos de Oliveira, L.A.; de Carvalho Rodrigues, E. Reference Values for Human Posture Measurements Based on Computerized Photogrammetry: A Systematic Review. J. Manip. Physiol. Ther. 2017, 40, 156–168. [Google Scholar] [CrossRef] [PubMed]
- Furlanetto, T.S.; Sedrez, J.A.; Candotti, C.T.; Loss, J.F. Photogrammetry as a Tool for the Postural Evaluation of the Spine: A Systematic Review. World J. Orthop. 2016, 7, 136–148. [Google Scholar] [CrossRef] [PubMed]
- Roghani, T.; Khalkhali Zavieh, M.; Rahimi, A.; Talebian, S.; Dehghan Manshadi, F.; Akbarzadeh Baghban, A.; King, N.; Katzman, W. The Reliability of Standing Sagittal Measurements of Spinal Curvature and Range of Motion in Older Women With and Without Hyperkyphosis Using a Skin-Surface Device. J. Manip. Physiol. Ther. 2017, 40, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Demir, E.; Güzel, N.; Çobanoğlu, G.; Kafa, N. The Reliability of Measurements with the Spinal Mouse Device in Frontal and Sagittal Planes in Asymptomatic Female Adolescents. Ann. Clin. Anal. Med. 2020, 11, 146–149. [Google Scholar] [CrossRef]
- Rabieezadeh, A.; Hovanloo, F.; Khaleghi, M.; Akbari, H. The relationship of height, weight and body mass index with curvature of spine kyphosis and lordosis in 12-15-year old male adolescents of Tehran. Turk. J. Sport Exerc. 2016, 18, 42–46. [Google Scholar]
- Cepková, A.; Zemková, E.; Šooš, Ľ.; Uvaček, M.; Muyor, J.M. Spinal Curvature in Female and Male University Students with Prolonged Bouts of Sedentary Behaviour. Available online: https://www.researchsquare.com/article/rs-1989231/v1 (accessed on 16 December 2023).
- Porto, A.B.; Okazaki, V.H.A. Thoracic Kyphosis and Lumbar Lordosis Assessment by Radiography and Photogrammetry: A Review of Normative Values and Reliability. J. Manip. Physiol. Ther. 2018, 41, 712–723. [Google Scholar] [CrossRef] [PubMed]
- Esola, M.A.; McClure, P.W.; Fitzgerald, G.K.; Siegler, S. Analysis of Lumbar Spine and Hip Motion during Forward Bending in Subjects with and without a History of Low Back Pain. Spine 1996, 21, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J. Historical Perspective: William Adams, the Forward Bending Test, and the Spine of Gideon Algernon Mantell. Spine 2004, 29, 1953–1955. [Google Scholar] [CrossRef] [PubMed]
- Senkoylu, A.; Ilhan, M.N.; Altun, N.; Samartzis, D.; Luk, K.D.K. A Simple Method for Assessing Rotational Flexibility in Adolescent Idiopathic Scoliosis: Modified Adam’s Forward Bending Test. Spine Deform. 2021, 9, 333–339. [Google Scholar] [CrossRef]
- Karachalios, T.; Sofianos, J.; Roidis, N.; Sapkas, G.; Korres, D.; Nikolopoulos, K. Ten-Year Follow-up Evaluation of a School Screening Program for Scoliosis. Is the Forward-Bending Test an Accurate Diagnostic Criterion for the Screening of Scoliosis? Spine 1999, 24, 2318–2324. [Google Scholar] [CrossRef]
- Carregaro, R.L.; Silva, L.; Gil Coury, H.J.C. Comparison between Two Clinical Tests for Evaluating the Flexibility of the Posterior Muscles of the Thigh. Braz. J. Phys. Ther. 2007, 11, 139–145. [Google Scholar] [CrossRef][Green Version]
- Guermazi, M.; Ghroubi, S.; Kassis, M.; Jaziri, O.; Keskes, H.; Kessomtini, W.; Ben Hammouda, I.; Elleuch, M.-H. Validité et reproductibilité du Spinal Mouse® pour l’étude de la mobilité en flexion du rachis lombaire. Ann. Réadaptation Médecine Phys. 2006, 49, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Muyor, J.M.; Vaquero-Cristóbal, R.; Alacid, F.; López-Miñarro, P.A. Criterion-Related Validity of Sit-and-Reach and Toe-Touch Tests as a Measure of Hamstring Extensibility in Athletes. J. Strength Cond. Res. 2014, 28, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.J.; O’Sullivan, P.B.; Beales, D.J.; de Klerk, N.; Straker, L.M. Trajectories of Childhood Body Mass Index Are Associated with Adolescent Sagittal Standing Posture. Int. J. Pediatr. Obes. 2011, 6, e97–e106. [Google Scholar] [CrossRef] [PubMed]
- Youdas, J.W.; Hollman, J.H.; Krause, D.A. The Effects of Gender, Age, and Body Mass Index on Standing Lumbar Curvature in Persons without Current Low Back Pain. Physiother. Theory Pract. 2006, 22, 229–237. [Google Scholar] [CrossRef]
- Young-Hyman, D.; Tanofsky-Kraff, M.; Yanovski, S.Z.; Keil, M.; Cohen, M.L.; Peyrot, M.; Yanovski, J.A. Psychological Status and Weight-Related Distress in Overweight or At-Risk-for-Overweight Children. Obesity 2006, 14, 2249–2258. [Google Scholar] [CrossRef]

| Gender | ||||
|---|---|---|---|---|
| Male (n = 25) | Female (n = 14) | |||
| Mean | SD | Mean | SD | |
| Age [year] | 13.04 | 2.11 | 13.57 | 1.22 |
| Stature [cm] | 159.52 | 14.67 | 158.79 | 6.48 |
| Body mass [kg] | 49.20 | 12.96 | 44.79 | 9.13 |
| BMI [kg/m2] | 19.02 | 2.82 | 17.66 | 2.54 |
| SIPS_SIAS St_PG [°] | 11.84 | 5.61 | 9.64 | 5.53 |
| Tragus-malleolus_PG [°] | 2.70 | 1.37 | 2.81 | 1.03 |
| Sacral-C7 Bd_PG [°] | 89.32 | 10.83 | 96.21 | 14.70 |
| Sacral tg Bd_PG [°] | 41.48 | 8.66 | 30.93 | 14.29 |
| Hip-malleolus Bd_PG [°] | 8.84 | 2.87 | 7.57 | 2.24 |
| FLASt_SM [°] | −28.52 | 10.88 | −34.57 | 11.88 |
| PLASt_SM [°] | −30.92 | 11.10 | −37.43 | 9.31 |
| FLABd_SM [°] | 38.68 | 13.05 | 32.07 | 12.72 |
| PLABd_SM [°] | 38.28 | 12.95 | 31.57 | 14.97 |
| Sacral-hip St_SM [°] | 14.72 | 8.37 | 18.29 | 6.22 |
| Sacral-hip Bd_SM [°] | 44.24 | 10.22 | 49.57 | 19.52 |
| I | II | III | IV | V | VI | VII | VIII | IX | X | XI | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (I) Sacral-hip Bd_SM | 1 | ||||||||||
| (II) Sacral-hip St_SM | 0.0905 | 1 | |||||||||
| (III) PLABd_SM | −0.3613 * | −0.1528 | 1 | ||||||||
| (IV) FLABd_SM | −0.3555 * | −0.3965 * | 0.7809 * | 1 | |||||||
| (V) PLASt_SM | 0.0202 | −0.8252 * | 0.2309 | 0.3649 * | 1 | ||||||
| (VI) FLASt_SM | 0.0253 | −0.8638 * | 0.2267 | 0.4560 * | 0.9439 * | 1 | |||||
| (VII) Sacral tg Bd_PG | −0.6595 * | −0.0878 | 0.0544 | −0.0182 | 0.0793 | −0.0061 | 1 | ||||
| (VIII) SIPS_SIAS St_PG | 0.0076 | 0.2713 | −0.0438 | −0.126 | −0.3283 * | −0.3791 * | 0.022 | 1 | |||
| (IX) Tragus-malleolus_PG | −0.0095 | 0.3094 | −0.1295 | −0.1621 | −0.3056 | −0.2643 | −0.0802 | 0.1711 | 1 | ||
| (X) Sacral-C7 Bd_PG | 0.4901 * | −0.0823 | 0.2982 | 0.4325 * | 0.0656 | 0.1889 | −0.8045 * | −0.0913 | −0.0204 | 1 | |
| (XI) Hip-malleolus Bd_PG | −0.0066 | −0.1252 | −0.2517 | −0.2366 | 0.2021 | 0.154 | 0.1716 | 0.2331 | −0.1322 | −0.4278 * | 1 |
| Variable | Model1 | Model2 |
|---|---|---|
| sacral tangent PG | −0.001 *** | −0.001 *** |
| BMI | 0.032 ** | 0.040 *** |
| Intercept | 3.572 *** | 3.454 *** |
| N | 36 | 39 |
| R2 | 0.583 | 0.585 |
| Adj. R2 | 0.557 | 0.562 |
| RMSE | 0.159 | 0.188 |
| AIC | 27.172 | 16.741 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belli, G.; Russo, L.; Mauro, M.; Toselli, S.; Maietta Latessa, P. Relation between Photogrammetry and Spinal Mouse for Lumbopelvic Assessment in Adolescents with Thoracic Kyphosis. Healthcare 2024, 12, 738. https://doi.org/10.3390/healthcare12070738
Belli G, Russo L, Mauro M, Toselli S, Maietta Latessa P. Relation between Photogrammetry and Spinal Mouse for Lumbopelvic Assessment in Adolescents with Thoracic Kyphosis. Healthcare. 2024; 12(7):738. https://doi.org/10.3390/healthcare12070738
Chicago/Turabian StyleBelli, Guido, Luca Russo, Mario Mauro, Stefania Toselli, and Pasqualino Maietta Latessa. 2024. "Relation between Photogrammetry and Spinal Mouse for Lumbopelvic Assessment in Adolescents with Thoracic Kyphosis" Healthcare 12, no. 7: 738. https://doi.org/10.3390/healthcare12070738
APA StyleBelli, G., Russo, L., Mauro, M., Toselli, S., & Maietta Latessa, P. (2024). Relation between Photogrammetry and Spinal Mouse for Lumbopelvic Assessment in Adolescents with Thoracic Kyphosis. Healthcare, 12(7), 738. https://doi.org/10.3390/healthcare12070738










