Effects of Online Health Promotion Program to Improve the Health and Wellbeing of Healthcare Students: A Feasibility Study
Abstract
1. Introduction
- to evaluate the preliminary effects of the integrated interventions of laughter exercises and MHFA training in promoting the healthcare students’ health and wellbeing;
- to examine the feasibility of a future full-scale randomized controlled trial (RCT) study;
- to illustrate their experiences and feedback on the online health promotion program’s effects, contents, and activities arrangements.
- Will the integrated interventions of laughter exercise and MHFA training promote the healthcare students’ health and wellbeing?
- What are the experiences and feedback of healthcare students regarding the effects, content, and activity arrangements of the online health promotion program?
2. Materials and Methods
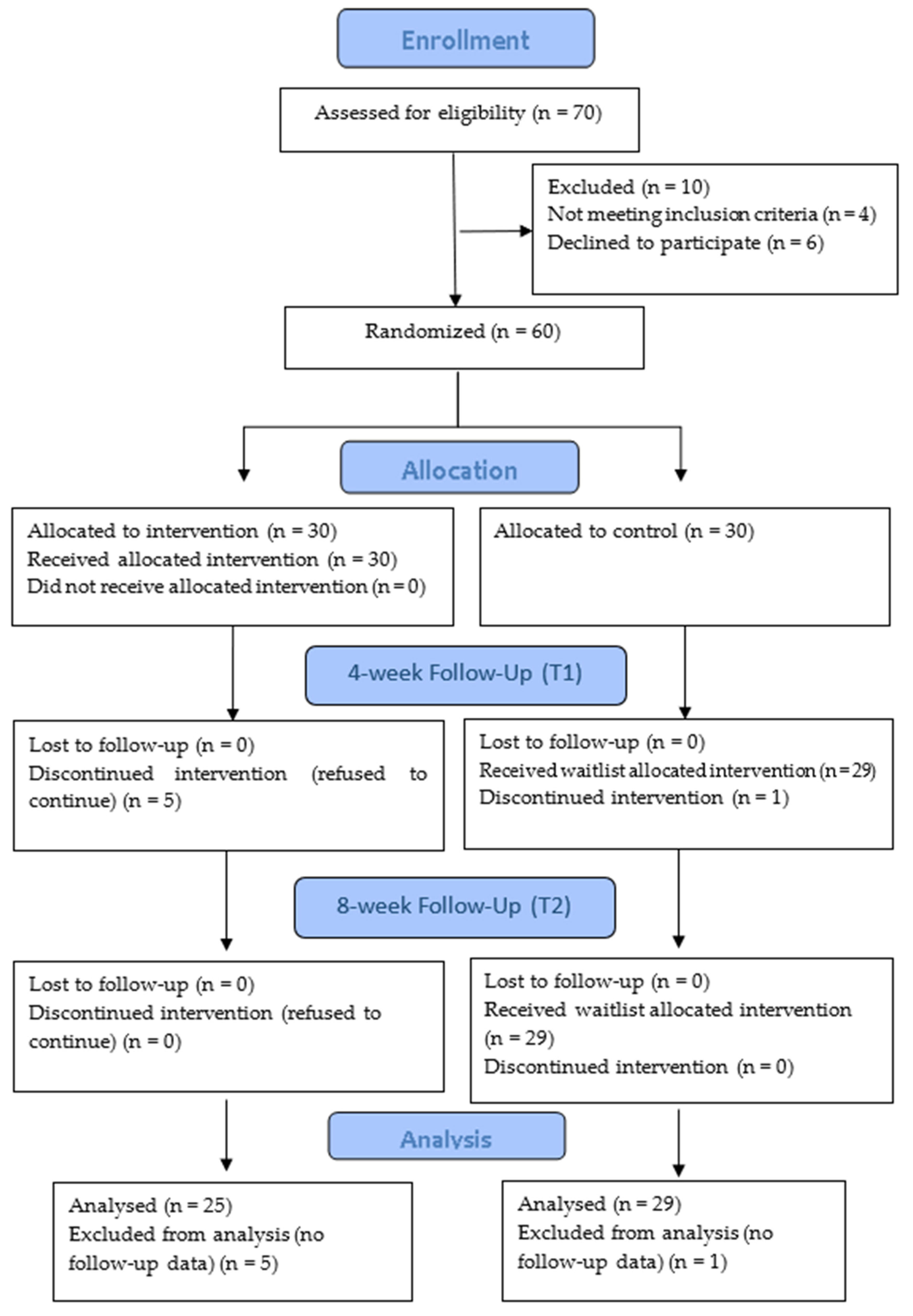
2.1. Study Design
2.2. Participants and Sampling
2.3. Ethical Considerations
2.4. Recruitment and Interventions
2.5. Outcome Measures
2.6. Data Collection and Analysis
3. Results
3.1. Quantitative Results
3.1.1. Baseline Sociodemographic Characteristics and Background
3.1.2. Ratings of DASS-21, PWI, and WHOQOL-BREF, and between the Intervention and Control Groups
3.2. Qualitative Results
3.2.1. Baseline Sociodemographic Characteristics and Background
3.2.2. Effects on Health and Wellbeing—Increased Self-Awareness of Health and Wellbeing
“The most significant and impressive message I appreciated was ‘to take good self-care before caring for others’. I learned mental health knowledge and could identify the warning signs of different mental disorders. I became more alert and aware of my health and emotions than before. When I was not in a good mood or encountered academic stress, laughter and breathing exercises helped me relax and calm my emotions.” (Group 4 Participant 3)
Physiological Fitness and Health Improvement
“Since joining, I have had daily self-practice of laughter, breathing, or relaxation exercises after dinner for about 20 min, feeling relaxed and refreshed after activities. I could start studying again, feel more energetic and effective, lessen stress, improve my insomnia, and sleep better.” (Group 4 Participant 2)
“Through daily practice of laughter and breathing exercises, I feel my heart becoming robust and my lung capacity increasing. It’s effective in improving my physical health.” (Group 3 Participant 2)
Psychological and Emotional Balance
“Initially, I didn’t understand how to make a false laugh into a true one. But it really happens when practice. I experienced and felt myself relaxed and happier. After doing laughing and breathing exercises, I find myself with decreased anxiety and can concentrate more on my studies without distraction.” (Group 3 Participant 3)
“I used to have low EQ (Emotional Intelligence Quotient). I’m easy to get agitated, especially when I am under stress due to my study. After learning the MHFA and the laughter activities, I know more about relaxing and stabilizing my emotions.” (Group 4 Participant 3)
Social Wellbeing and Connection
“I practice the activities with my classmates before our project presentations or assessments. The slogan, ‘Very good, Very good, yeah! Hoho, Hahaha!’ It’s upbeat and helpful for self and others’ encouragement. It can boost our mood and confidence.” (Group 3 Participant 2)
“The unconditional laughter and childlike playfulness exercises are so funny and stress relieving. I do it with my friends when we have time, whether stressed or not in a good mood. We like laughing together for joy, better morale, and rapport.” (Group 1 Participant 1)
Attitudinal Change in Health Concepts
“If I’m sad, I cry; if I’m happy, I laugh. Though I know emotions could affect behavior and vice versa. The laughter exercises embarrassed me initially, and I was too shy to laugh without reason. After daily practice of laughter exercises and writing down grateful and happy events, I enjoy and treasure it. After this study, I really experienced that if you ‘pretend’ to laugh, your mimic laugh will gradually become true, as the laughter yoga leader said. You can easily change your mood to be happy, promoting your mental wellbeing. It’s true.” (Group 3 Participant 1)
“My friend has anxiety and depression and recently suffered from OCD (Obsessive Compulsive Disorder) also. Her emotions were not so stable. The MHFA clarified my concepts, allowing me to understand her problems better and how to communicate with her appropriately. I will try to offer help or advise her what to do.” (Group 2 Participant 4)
3.2.3. Feedback on Contents and Activities—Enjoyed Diversified and Complementary Content Activities Arrangement
“Um, the contents and activities are diversified, interrelated, and complementary. Laughing yoga exercises remind us of ‘self-care’ for our health. It can strengthen our physical health and maintain emotional balance. Daily records of three grateful events and happy moments can improve life satisfaction. Through MHFA, our awareness and mental health knowledge increased as we recognized more about common mental disorders, not just benefiting ourselves but also can assist our family or friends who have mental health problems.” (Group 3 Participant 3)
Enjoyed in Funny Laughter Yoga Exercise
“I was shy during the first laughter yoga session but could enjoy the following sessions. The different exercises were fun and exciting. I found myself becoming more involved and gradually feeling relaxed. I didn’t mind others’ views; I just did what I liked. The exercises uplifted my mood and improved my self-confidence. It helped me a lot. I would be nervous and anxious about the project presentation, but I am no longer nervous now.” (Group1 Participant 2)
“The teacher is an experienced and innovative leader. We learned how to be happy through the childlike, playful exercises. She encouraged each of us to design and take the lead in a laughter exercise. It’s so funny and pleasurable. I liked breathing and relaxing exercises also. “Humming” (a type of breathing exercise) is helpful. I have mood swings easily, but I can relax and calm down after practicing it, even when stressed preparing for clinical practicum.” (Group 2 Participant 3)
Appreciated Grateful and Happy Events’ Daily Records
“I enjoy recording happy moments daily, though sometimes I forget. It reminds me of the events I have nearly neglected but can make me happy. The idea of compliments also makes me and others happy. It’s nice!” (Group 2 Participant 4)
“I like the log sheet. My daily life is filled with study stress and anxiety. I seldom think of happy moments. When thinking about and recording the ‘three daily grateful and happy issues,’ I realize I have some inner changes. Daily appreciation can change my mood and life attitude to be more positive and enthusiastic. It reminds me of life’s meaning and satisfaction with positive thinking.” (Group 3 Participant 4).
Structured and Informative Mental Health Knowledge
“We learned different common mental disorders and increased our self-awareness of the warning signs and risk factors. The MHFA strengthened our understanding of identifying and initiating help for those with mental problems and referring professional help. We had opportunities to practice communication using different scenarios. It’s practical.” (Group 3 Participant 4)
“I think the contents were good and adequately presented. Self-e-learning is informative with texts, videos, and quizzes and is easy to follow. The two teacher-led consolidation sessions allowed us to ask questions and clarify our concerns. Local case scenarios help to illustrate different situations. The supplementary local resources with contact details are useful. It was a good online learning experience.” (Group 4 Participant 2)
Facilitated Flexible Participation Arrangements
“The study conducted in the summer term, including teacher-led and self-practice activities, is acceptable. The weekly online laughter yoga exercises on weekday evenings with daily self-practice of 20 min were feasible. The two weeks of MHFA self-e-learning could be accessed flexibly, and the following two weekends of teacher-led consolidation online sessions were also convenient.” (Group 3 Participant 2)
“I like online and e-learning modes that are time-saving and convenient. As Hong Kongers are usually busily engaged, reserving a fixed date, time, and venue to attend regular activities is not easy. It may cause inconvenience to somebodies. Nighttime is a good time for relaxing. After showering, I can sleep right away. If we attend laughter exercises outside, we must return home first.” (Group 3 Participant 3)
“I agree that online mode is innovative and time-saving. But I felt a bit goofy and strange, laughing at the monitor. My home was small, and my family was watching around and feeling embarrassed. I believe face-to-face mode would be more interactive and better communication.” (Group 2 Participant 2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Official Records of the World Health Organization nº2. In Proceedings of International Health Conference, New York, NY, USA, 19–22 June 1948. [Google Scholar]
- Caltabiano, M.L.; Ricciardelli, L. Applied Topics in Health Psychology; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- Bartos, L.J.; Funes, M.J.; Ouellet, M.; Posadas, M.P.; Immink, M.A.; Krägeloh, C. A feasibility study of a program integrating mindfulness, yoga, positive psychology, and emotional intelligence in tertiary-level student musicians. Mindfulness 2022, 13, 2507–2528. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Chen, T.; Lucock, M. The mental health of university students during the COVID-19 pandemic: An online survey in the UK. PLoS ONE 2022, 17, e0262562. [Google Scholar] [CrossRef]
- Ho, K.H.; Mak, A.K.; Chung, R.W.; Leung, D.Y.; Chiang, V.C.; Cheung, D.S. Implications of COVID-19 on the loneliness of older adults in residential care homes. Qual. Health Res. 2022, 32, 279–290. [Google Scholar] [CrossRef]
- Hung, M.S.Y.; Chan, L.C.K.; Liu, S.P.S. The health impacts and life challenges caused by the COVID-19 pandemic on Hong Kong Chinese women. Int. J. Environ. Res. Public Health 2022, 19, 5115. [Google Scholar] [CrossRef]
- Li, Y.; Wang, A.; Wu, Y.; Han, N.; Huang, H. Impact of the COVID-19 pandemic on the mental health of college students: A systematic review and meta-analysis. Front. Psychol. 2021, 12, 669119. [Google Scholar] [CrossRef]
- Shek, D.T.; Dou, D.; Zhu, X. Prevalence and correlates of mental health of university students in Hong Kong: What happened one year after the occurrence of COVID-19? Front. Public Health 2022, 10, 857147. [Google Scholar] [CrossRef]
- World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief, 2 March 2022 (No. WHO/2019-nCoV/Sci_Brief/Mental_health/2022.1). Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 (accessed on 15 November 2023).
- Hung, M.S.Y.; Lam, S.K.K.; Chan, L.C.K.; Liu, S.P.S.; Chow, M.C.M. The psychological and quality of life impacts on women in Hong Kong during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 6734. [Google Scholar] [CrossRef]
- Ribeiro, Í.J.; Pereira, R.; Freire, I.V.; de Oliveira, B.G.; Casotti, C.A.; Boery, E.N. Stress and quality of life among university students: A systematic literature review. Health Prof. Educ. 2018, 4, 70–77. [Google Scholar] [CrossRef]
- Ching, S.S.Y.; Cheung, K. Factors affecting resilience of nursing, optometry, radiography and medical laboratory science students. Int. J. Environ. Res. Public Health 2021, 18, 3867. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.-S.; Hasson, F. Resilience, stress, and psychological well-being in nursing students: A systematic review. Nurse Educ. Today 2020, 90, 104440. [Google Scholar] [CrossRef]
- Gao, J.; Wang, F.; Guo, S.; Hu, F. Mental health of nursing students amid coronavirus disease 2019 pandemic. Front. Psychol. 2021, 12, 699558. [Google Scholar] [CrossRef]
- Goni-Fuste, B.; Wennberg, L.; Martin-Delgado, L.; Alfonso-Arias, C.; Martin-Ferreres, M.L.; Monforte-Royo, C. Experiences and needs of nursing students during pandemic outbreaks: A systematic overview of the literature. J. Prof. Nurs. 2021, 37, 53–64. [Google Scholar] [CrossRef]
- Li, D.; Zou, L.; Zhang, Z.; Zhang, P.; Zhang, J.; Fu, W.; Mao, J.; Cao, S. The psychological effect of COVID-19 on home-quarantined nursing students in China. Front. Psychiatry 2021, 12, 652296. [Google Scholar] [CrossRef]
- Mishra, J.; Samanta, P.; Panigrahi, A.; Dash, K.; Behera, M.R.; Das, R. Mental health status, coping strategies during COVID-19 pandemic among undergraduate students of healthcare profession. Int. J. Ment. Health Addict. 2023, 21, 562–574. [Google Scholar] [CrossRef]
- Mulyadi, M.; Tonapa, S.I.; Luneto, S.; Lin, W.-T.; Lee, B.-O. Prevalence of mental health problems and sleep disturbances in nursing students during the COVID-19 pandemic: A systematic review and meta-analysis. Nurse Educ. Pract. 2021, 57, 103228. [Google Scholar] [CrossRef] [PubMed]
- Purnama, A.; Susaldi, S.; Mukhlida, H.Z.; Maulida, H.H.; Purwati, N.H. Mental health in health students during Coronavirus Disease-19: Systematic review. Open Access Maced. J. Med. Sci. 2021, 9, 205–210. [Google Scholar] [CrossRef]
- Tejoyuwono, A.A.T.; Nugraha, R.P.; Fahdi, F.K. The effect of mental health status on the quality of life of faculty of medicine students during the pandemic coronavirus disease 2019 period. Open Access Maced. J. Med. Sci. 2021, 9, 645–652. [Google Scholar] [CrossRef]
- Barisone, M.; Ghirotto, L.; Busca, E.; Crescitelli, M.E.D.; Casalino, M.; Chilin, G.; Milani, S.; Sanvito, P.; Suardi, B.; Follenzi, A. Nursing students’ clinical placement experiences during the COVID-19 pandemic: A phenomenological study. Nurse Educ. Pract. 2022, 59, 103297. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.S.Y.; Ng, W.W.M.; Choi, E.K.Y. The Impacts of the COVID-19 Pandemic on Hong Kong Nursing Students’ Mental Health and Quality of Life. Int. J. Environ. Res. Public Health 2022, 19, 15117. [Google Scholar] [CrossRef] [PubMed]
- Jia, Q.; Qu, Y.; Sun, H.; Huo, H.; Yin, H.; You, D. Mental health among medical students during COVID-19: A systematic review and meta-analysis. Front. Psychol. 2022, 13, 846789. [Google Scholar] [CrossRef]
- Skevington, S.M.; Lotfy, M.; O’Connell, K.A. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.L.; Young, B.; Lui, B.S.C.; Leung, A.W.Y.; So, J.L.T. Professional quality of life and resilience in emergency department healthcare professionals during COVID-19 in Hong Kong: A cross-sectional study. Hong Kong J. Emerg. Med. 2022, 29, 168–176. [Google Scholar] [CrossRef]
- Worsley, J.D.; Pennington, A.; Corcoran, R. Supporting mental health and wellbeing of university and college students: A systematic review of review-level evidence of interventions. PLoS ONE 2022, 17, e0266725. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, M.; Hammond, T.; Cummins, R. The impact of laughter yoga on subjective well-being: A pilot study. Eur. J. Humour Res. 2014, 1, 25–34. [Google Scholar] [CrossRef]
- van der Wal, C.N.; Kok, R.N. Laughter-inducing therapies: Systematic review and meta-analysis. Soc. Sci. Med. 2019, 232, 473–488. [Google Scholar] [CrossRef] [PubMed]
- Gonot-Schoupinsky, F.N.; Garip, G.; Sheffield, D. Laughter and humour for personal development: A systematic scoping review of the evidence. Eur. J. Integr. Med. 2020, 37, 101144. [Google Scholar] [CrossRef]
- Lynes, L.; Kawar, L.; Valdez, R.M. Can laughter yoga provide stress relief for clinical nurses? Nurs. Manag. 2019, 50, 30–37. [Google Scholar] [CrossRef]
- Shattla, S.I.; Mabrouk, S.M.; Abed, G.A. Effectiveness of laughter yoga therapy on job burnout syndromes among psychiatric nurses. Int. J. Nurs. 2019, 6, 33–47. [Google Scholar] [CrossRef]
- Yim, J. Therapeutic benefits of laughter in mental health: A theoretical review. Tohoku J. Exp. Med. 2016, 239, 243–249. [Google Scholar] [CrossRef]
- Jorm, A.F.; Kitchener, B.; Lam, A.; Wong, F.N. Mental Health First Aid: An International Early Intervention Training Program for Members of the Public. Hong Kong J. Ment. Health 2011, 37, 31–38. [Google Scholar]
- Kitchener, B.A.; Jorm, A.; Kelly, C. Mental Health First Aid Manual, 4th ed.; Mental Health Association of Hong Kong: Hong Kong, China, 2017. [Google Scholar]
- Costa, T.F.O.; Sampaio, F.M.C.; Sequeira, C.A.d.C.; Ribeiro, I.M.O.C.; Parola, V.S.d.O. Review of Mental health first aid programs. West J. Nurs. Res. 2021, 43, 1146–1156. [Google Scholar] [CrossRef]
- The Mental Health Association. Mental Health First Aid. What Is Mental Health First Aid? Available online: https://www.mhfa.org.hk/articles/2 (accessed on 11 March 2024).
- Wong, D.F.; Lau, Y.; Kwok, S.; Wong, P.; Tori, C. Evaluating the effectiveness of mental health first aid program for Chinese people in Hong Kong. Res. Soc. Work Pract. 2017, 27, 59–67. [Google Scholar] [CrossRef]
- Hung, M.S.; Lam, S.K.; Chow, M.C. Nursing students’ experiences of mental health first aid training: A qualitative descriptive study. Collegian 2019, 26, 534–540. [Google Scholar] [CrossRef]
- Hung, M.S.; Chow, M.C.; Chien, W.T.; Wong, P.Y. Effectiveness of the Mental Health First Aid programme for general nursing students in Hong Kong: A randomised controlled trial. Collegian 2021, 28, 106–113. [Google Scholar] [CrossRef]
- Bond, K.S.; Jorm, A.F.; Kitchener, B.A.; Reavley, N.J. Mental health first aid training for Australian medical and nursing students: An evaluation study. BMC Psychol. 2015, 3, 11. [Google Scholar] [CrossRef] [PubMed]
- Crespo-Gonzalez, C.; Dineen-Griffin, S.; Rae, J.; Hill, R.A. Mental health training programs for community pharmacists, pharmacy staff and students: A systematic review. Res. Soc. Adm. Pharm. 2022, 18, 3895–3910. [Google Scholar] [CrossRef] [PubMed]
- Davies, E.B.; Beever, E.; Glazebrook, C. A pilot randomised controlled study of the mental health first aid eLearning course with UK medical students. BMC Med. Educ. 2018, 18, 45. [Google Scholar] [CrossRef]
- Edgar, S.; Connaughton, J. Using mental health first aid training to improve the mental health literacy of physiotherapy students. Physiother. Can. 2021, 73, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Hadlaczky, G.; Hökby, S.; Mkrtchian, A.; Carli, V.; Wasserman, D. Mental Health First Aid is an effective public health intervention for improving knowledge, attitudes, and behaviour: A meta-analysis. Int. Rev. Psychiatry 2014, 26, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Maslowski, A.K.; LaCaille, R.A.; LaCaille, L.J.; Reich, C.M.; Klingner, J. Effectiveness of mental health first aid: A meta-analysis. Ment. Health Rev. 2019, 24, 245–261. [Google Scholar] [CrossRef]
- Morgan, A.J.; Ross, A.; Reavley, N.J. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. PLoS ONE 2018, 13, e0197102. [Google Scholar] [CrossRef] [PubMed]
- Ostrowski, J.L.; Sampson, S.; McGoldrick, E.; Karabin, C.; Shields, K. Effects of Mental Health First Aid Course: Knowledge, Confidence, and Stigma Among Occupational Therapy Students. J. Occup. Ther. Educ. 2023, 7, 5. [Google Scholar] [CrossRef]
- Burns, S.; Crawford, G.; Hallett, J.; Hunt, K.; Chih, H.J.; Tilley, P.M. What’s wrong with John? A randomised controlled trial of Mental Health First Aid (MHFA) training with nursing students. BMC Psychiatry 2017, 17, 111. [Google Scholar] [CrossRef] [PubMed]
- Positive Psychology Center. PERMATM Theory of Well-Being and PERMA Workshops. Available online: https://ppc.sas.upenn.edu/learn-more/perma-theory-well-being-and-perma-workshops (accessed on 5 February 2024).
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Creswell, J.W.; Clark, V.L.P. Designing and Conducting Mixed Methods Research; Sage Publications: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Wasti, S.P.; Simkhada, P.; van Teijlingen, E.R.; Sathian, B.; Banerjee, I. The growing importance of mixed-methods research in health. Nepal J. Epidemiol. 2022, 12, 1175. [Google Scholar] [CrossRef]
- Whitehead, A.L.; Julious, S.A.; Cooper, C.L.; Campbell, M.J. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat. Methods Med. Res. 2016, 25, 1057–1073. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. Jahrb. Wiss. Ethik 2009, 14, 233–238. [Google Scholar]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef]
- Gong, X.; Xie, X.Y.; Xu, R.; Luo, Y.J. Psychometric properties of the Chinese versions of DASS-21 in Chinese college students. Chin. J. Clin. Psychol. 2010, 18, 443–446. [Google Scholar]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales; Psychology Foundation of Australia: Sydney, Australia, 1996; pp. 30–37. [Google Scholar]
- International Wellbeing Group. Personal Wellbeing Index—Adult (Cantonese); The Australian Centre on Quality of Life, Deakin University: Burwood, Australia, 2024. [Google Scholar]
- World Health Organization. The World Health Organization Quality of Life (WHOQOL)—BREF. 2012 Revision. Available online: https://apps.who.int/iris/handle/10665/77773 (accessed on 1 December 2023).
- Lau, A.L.; Cummins, R.A.; Mcpherson, W. An investigation into the cross-cultural equivalence of the Personal Wellbeing Index. Soc. Indic. Res. 2005, 72, 403–430. [Google Scholar] [CrossRef]
- Xia, P.; Li, N.; Hau, K.-T.; Liu, C.; Lu, Y. Quality of life of Chinese urban community residents: A psychometric study of the mainland Chinese version of the WHOQOL-BREF. BMC Med. Res. Methodol. 2012, 12, 37. [Google Scholar] [CrossRef]
- Curry, L.A.; Nembhard, I.M.; Bradley, E.H. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation 2009, 119, 1442–1452. [Google Scholar] [CrossRef] [PubMed]
- Guest, G.; Namey, E.; Taylor, J.; Eley, N.; McKenna, K. Comparing focus groups and individual interviews: Findings from a randomized study. Int. J. Soc. Res. Methodol. 2017, 20, 693–708. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative Research & Evaluation Methods: Integrating Theory and Practice; Sage Publications: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Giacalone, M.; Agata, Z.; Cozzucoli, P.C.; Alibrandi, A. Bonferroni-Holm and permutation tests to compare health data: Methodological and applicative issues. BMC Med. Res. Methodol. 2018, 18, 81. [Google Scholar] [CrossRef] [PubMed]
- Doody, O.; Slevin, E.; Taggart, L. Focus group interviews part 3: Analysis. Br. J. Nurs. 2013, 22, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Parahoo, K. Nursing Research: Principles, Process and Issues, 2nd ed.; Bloomsbury Publishing: London, UK, 2014. [Google Scholar]
- Guba, E.G. Criteria for assessing the trustworthiness of naturalistic inquiries. ECTJ 1981, 29, 75–91. [Google Scholar] [CrossRef]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage Publications: Thousand Oaks, CA, USA, 1985. [Google Scholar]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 11th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2021. [Google Scholar]
- Housing Bureau HKSAR. Housing Bureau, HKSAR 2022. Available online: https://www.hb.gov.hk/eng/publications/housing/HIF2022.pdf (accessed on 10 March 2024).
- The Government of the HKSAR. Government Extends Existing Social Distancing Measures. Available online: https://www.info.gov.hk/gia/general/202207/12/P2022071200565.htm (accessed on 10 March 2024).
- Kataria, M. Laugh for No Reason, 4th ed.; Madhuri International: Mumbai, India, 2011. [Google Scholar]
- Bahari, K.; Lorica, J.D. The effects of laughter therapy on mental health: An integrative literature review. Malays. J. Nurs. 2019, 10, 55–61. [Google Scholar] [CrossRef]
- Mbiriri, M. Laughter Therapy as an Intervention to Promote Psychological Well-Being. J. Humanit. Soc. Policy 2020, 6, 2020. [Google Scholar]
- Mongrain, M.; Anselmo-Matthews, T. Do positive psychology exercises work? A replication of Seligman et al. J. Clin. Psychol. 2012, 68, 382–389. [Google Scholar] [CrossRef]
- Martínez-Martí, M.L.; Avia, M.D.; Hernández-Lloreda, M.J. The effects of counting blessings on subjective well-being: A gratitude intervention in a Spanish sample. Span. J. Psychol. 2010, 13, 886–896. [Google Scholar] [CrossRef]
- Manthey, L.; Vehreschild, V.; Renner, K.-H. Effectiveness of two cognitive interventions promoting happiness with video-based online instructions. J. Happiness Stud. 2016, 17, 319–339. [Google Scholar] [CrossRef]
- Herbert, H.S.; Manjula, M. Resilience based intervention to promote mental health of college students: A preliminary feasibility study from India. Ment. Health Prev. 2022, 26, 200239. [Google Scholar] [CrossRef]
- Long, R.; Kennedy, M.; Malloy Spink, K.; Lengua, L.J. Evaluation of the implementation of a well-being promotion program for college students. Front. Psychiatry 2021, 12, 610931. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, M.C.; Dash, S.; Klepac Pogrmilovic, B.; Patten, R.K.; Parker, A.G. The engagement of tertiary students with an online mental health intervention during the coronavirus disease 2019 pandemic: A feasibility study. Digit. Health 2022, 8, 20552076221117746. [Google Scholar] [CrossRef] [PubMed]
- Aminoff, V.; Sellén, M.; Sörliden, E.; Ludvigsson, M.; Berg, M.; Andersson, G. Internet-based cognitive behavioral therapy for psychological distress associated with the COVID-19 pandemic: A pilot randomized controlled trial. Front. Psychol. 2021, 12, 684540. [Google Scholar] [CrossRef] [PubMed]
- Eraydin, C.; Alpar, S.E. The effect of laughter therapy on nursing students’ anxiety, satisfaction with life, and psychological well-being during the COVID-19 pandemic: Randomized controlled study. Adv. Integr. Med. 2022, 9, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.S.T.; Wong, R.S.M.; Mak, Y.-W.; Yip, Y.T.; Mak, H. Brief take-home laughter yoga practice (B-TLYP): Impact on multi-dimensional affects among Chinese adults in Hong Kong. Adv. Ment. Health 2019, 17, 124–134. [Google Scholar] [CrossRef]
- Kataria, M. The inner spirit of laughter: Five secrets from the laughing guru. In Dr. Kataria School of Laughter Yoga; Penguin Life: London, UK, 2012. [Google Scholar]
- Hong Kong Free Press. 37 Hong Kong Students Took Own Lives This Year; Health Official Says Trend Causes ‘Serious Alarm’. Available online: https://hongkongfp.com/2023/11/17/37-hong-kong-students-took-own-lives-this-year-health-official-says-trend-causes-serious-alarm/ (accessed on 1 December 2023).
- Hong Kong Free Press. Hong Kong Schools Report 27 Suspected Student Suicides in First 10 Months of 2023. Available online: https://hongkongfp.com/2023/11/22/hong-kong-schools-report-27-suspected-student-suicides-in-first-10-months-of-2023/ (accessed on 1 December 2023).
| Variable | All Participants (n = 54) | Intervention Group (n = 25) | Control Group (n = 29) | p-Value |
|---|---|---|---|---|
| Gender | 0.95 c | |||
| Male | 11 (20.4%) | 5 (20%) | 6 (20.7%) | |
| Female | 43 (79.6%) | 20 (80%) | 23 (79.3%) | |
| Age (Mean ± SD) | 22.11 ± 4.74 | 22.20 ± 5.17 | 22.03 ± 4.43 | 0.9 t |
| Educational level | 0.241 c | |||
| Associate | 10 (18.5%) | 5 (20%) | 5 (17.2%) | |
| Higher Diploma | 9 (31.0%) | 3 (12%) | 9 (31%) | |
| Bachelor | 15 (51.7%) | 17 (68%) | 15 (51.7%) | |
| Major study | 1 f | |||
| Health Studies | 9 (16.7%) | 4 (16%) | 5 (17.2%) | |
| Nursing | 45 (83.3%) | 21 (84%) | 24 (82.8%) | |
| Year of study | 0.693 f | |||
| Year 1 | 21 (38.9%) | 9 (36%) | 12 (41.4%) | |
| Year 2 | 15 (27.8%) | 6 (24%) | 9 (31%) | |
| Year 3 | 8 (14.8%) | 4 (16%) | 4 (13.8%) | |
| Year 4 | 7 (13.0%) | 5 (20%) | 2 (6.9%) | |
| Year 5 | 3 (5.6%) | 1 (4%) | 2 (6.9%) | |
| Any clinical internship during COVID-19? | 0.109 c | |||
| Yes | 12 (22.2%) | 8 (32%) | 4 (13.8%) | |
| No | 42 (77.8%) | 17 (68%) | 25 (86.2%) | |
| Can MHFA improve your health? | ||||
| Yes | 54 (100%) | 25 (100%) | 29 (100%) | |
| Can Laughter Yoga exercise improve your health? | 1 f | |||
| Yes | 51 (94.4%) | 24 (96%) | 27 (93.1%) | |
| No | 3 (5.6%) | 1 (4%) | 2 (6.9%) |
| Baseline (T1) | Week 4 (T2) | Week 8 (T3) | ||||
|---|---|---|---|---|---|---|
| DASS 21 | Median (25th–75th Percentile) | Median (25th–75th Percentile) | Median (25th–75th Percentile) | p (T1 vs. T2) | p (T1 vs. T3) | p (T2 vs. T3) |
| DASS 21-depression | ||||||
| Intervention group | 12.00 (6.00–16.00) | 6.00 (2.00–14.00) | 4.00 (1.00–8.00) | 0.053 | * 0.001 | * 0.016 |
| Control group | 12.00 (6.00–17.00) | 10.00 (6.00–14.00) | 8.00 (3.00–15.00) | 0.075 | 0.029 | 0.333 |
| p (between-group difference) | 0.149 | * 0.023 | ||||
| DASS 21-anxiety | ||||||
| Intervention group | 8.00 (4.00–12.00) | 6.00 (3.00–10.00) | 4.00 (1.00–9.00) | * 0.01 | * 0.004 | 0.753 |
| Control group | 8.00 (4.00–13.00) | 6.00 (2.00–14.00) | 4.00 (2.00–14.00) | 0.157 | 0.031 | 0.362 |
| p (between-group difference) | 0.376 | 0.446 | ||||
| DASS 21-stress | ||||||
| Intervention group | 16.00 (10.00–19.00) | 10.00 (5.00–18.00) | 8.00 (2.00–13.00) | * 0.005 | * <0.001 | * 0.035 |
| Control group | 16.00 (8.00–19.00) | 14.00 (6.00–18.00) | 14.00 (5.00–18.00) | 0.142 | 0.417 | 0.828 |
| p (between-group difference) | 0.378 | 0.058 |
| Baseline (T1) | Week 4 (T2) | Week 8 (T3) | ||||
|---|---|---|---|---|---|---|
| PWI | Median (25th–75th Percentile) | Median (25th–75th Percentile) | Median (25th–75th Percentile) | p (T1 vs. T2) | p (T1 vs. T3) | p (T2 vs. T3) |
| PWI-Average subjective wellbeing | ||||||
| Intervention group | 55.00 (44.38–61.25) | 65.00 (48.13–71.88) | 66.25 (50.63–75.63) | * 0.004 | * 0.004 | 0.338 |
| Control group | 52.50 (43.75–67.50) | 58.75 (44.38–66.25) | 55.00 (43.75–66.88) | 0.698 | 0.547 | 0.346 |
| p (between-group difference) | 0.092 | 0.056 |
| Baseline (T1) | Week 4 (T2) | Week 8 (T3) | ||||
|---|---|---|---|---|---|---|
| WHOQOL-BREF (HK Version) | Median (25th–75th Percentile) | Median (25th–75th Percentile) | Median (25th–75th Percentile) | p (T1 vs. T2) | p (T1 vs. T3) | p (T2 vs. T3) |
| Physical Health | ||||||
| Intervention group | 13.71 (11.14–15.14) | 14.86 (12.29–16.86) | 14.86 (13.14–17.14) | * 0.024 | * 0.002 | 0.137 |
| Control group | 14.86 (13.14–16.29) | 14.29 (12.00–16.00) | 14.86 (12.29–16.00) | 0.141 | 0.614 | 0.612 |
| p (between-group difference) | 0.519 | 0.343 | ||||
| Psychological | ||||||
| Intervention group | 12.50 (10.25–13.50) | 14.00 (12.00–14.75) | 14.00 (12.50–15.75) | * 0.016 | * 0.001 | * 0.007 |
| Control group | 13.00 (11.00–14.75) | 12.00 (11.50–14.50) | 13.00 (11.25–14.50) | 0.318 | 0.969 | 0.242 |
| p (between-group difference) | 0.292 | 0.053 | ||||
| Social Relationships | ||||||
| Intervention group | 13.33 (10.67–13.33) | 13.33 (11.33–14.67) | 14.67 (12.67–16.00) | 0.053 | * 0.003 | 0.068 |
| Control group | 13.33 (12.00–14.67) | 12.00 (11.33–14.67) | 13.33 (12.00–14.67) | 0.061 | 0.849 | 0.019 |
| p (between-group difference) | 0.073 | 0.031 | ||||
| Environment | ||||||
| Intervention group | 12.50 (11.00–16.00) | 14.00 (13.00–15.75) | 14.50 (12.75–16.50) | 0.126 | 0.179 | 0.465 |
| Control group | 13.00 (11.25–14.75) | 13.00 (11.75–14.50) | 13.50 (11.75–15.00) | 0.848 | 0.259 | 0.417 |
| p (between-group difference) | 0.102 | 0.102 |
| Themes | Categories | Codes (Examples) |
|---|---|---|
| Increased self-awareness of health and wellbeing |
|
|
| Enjoyed diversified and complementary content and activities |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, M.S.Y.; Ng, W.W.M.; Choi, E.K.Y. Effects of Online Health Promotion Program to Improve the Health and Wellbeing of Healthcare Students: A Feasibility Study. Healthcare 2024, 12, 682. https://doi.org/10.3390/healthcare12060682
Hung MSY, Ng WWM, Choi EKY. Effects of Online Health Promotion Program to Improve the Health and Wellbeing of Healthcare Students: A Feasibility Study. Healthcare. 2024; 12(6):682. https://doi.org/10.3390/healthcare12060682
Chicago/Turabian StyleHung, Maria Shuk Yu, Winnie Wing Man Ng, and Edward Kwok Yiu Choi. 2024. "Effects of Online Health Promotion Program to Improve the Health and Wellbeing of Healthcare Students: A Feasibility Study" Healthcare 12, no. 6: 682. https://doi.org/10.3390/healthcare12060682
APA StyleHung, M. S. Y., Ng, W. W. M., & Choi, E. K. Y. (2024). Effects of Online Health Promotion Program to Improve the Health and Wellbeing of Healthcare Students: A Feasibility Study. Healthcare, 12(6), 682. https://doi.org/10.3390/healthcare12060682






