Low Diet Quality and Nutritional Knowledge in Women with Endometriosis: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
2.2.1. Own Questions
2.2.2. Dietary Habits and Diet Quality
Adherence to Mediterranean Diet
2.2.3. Nutrition Knowledge
2.3. Statistical Analysis
3. Results
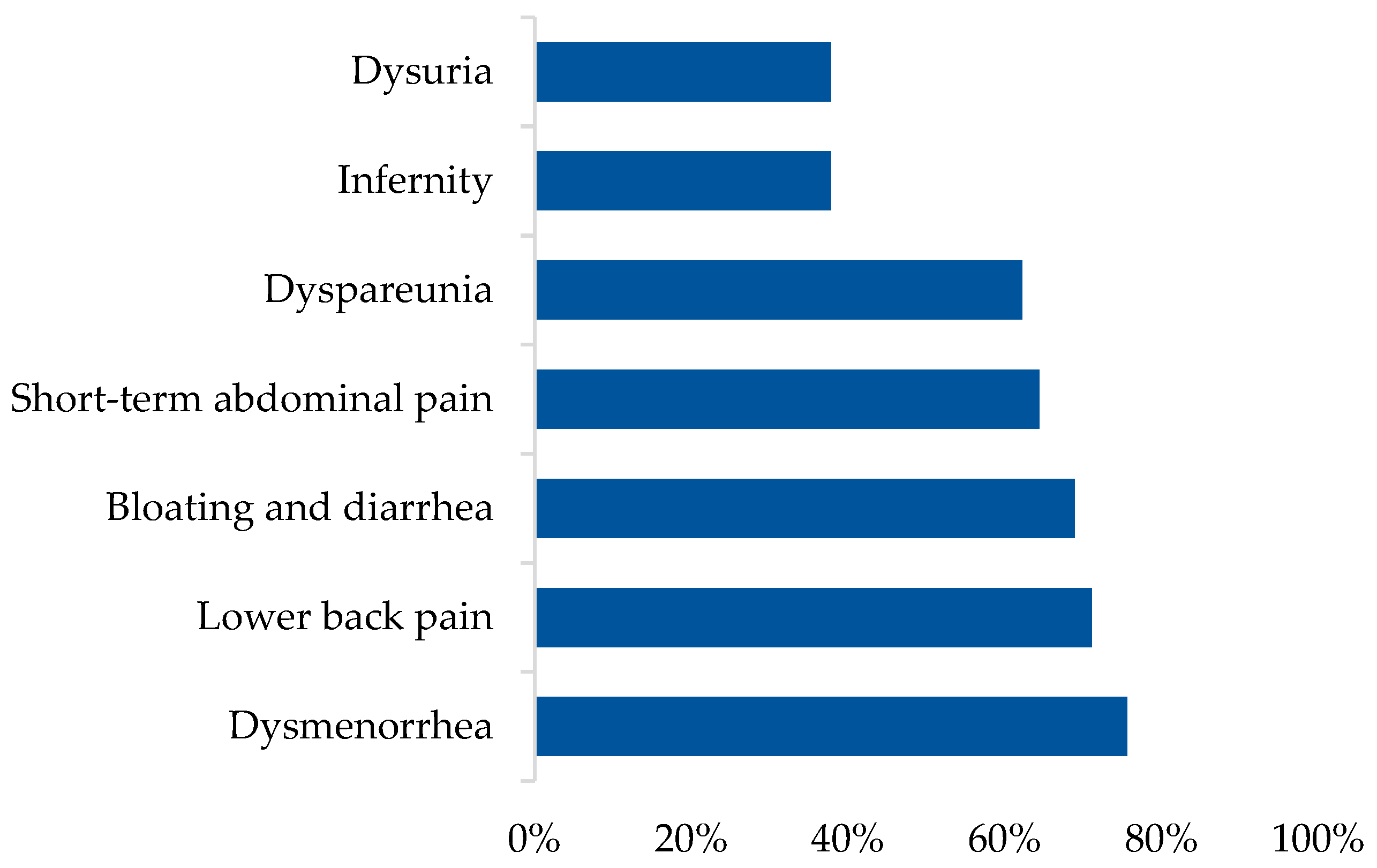
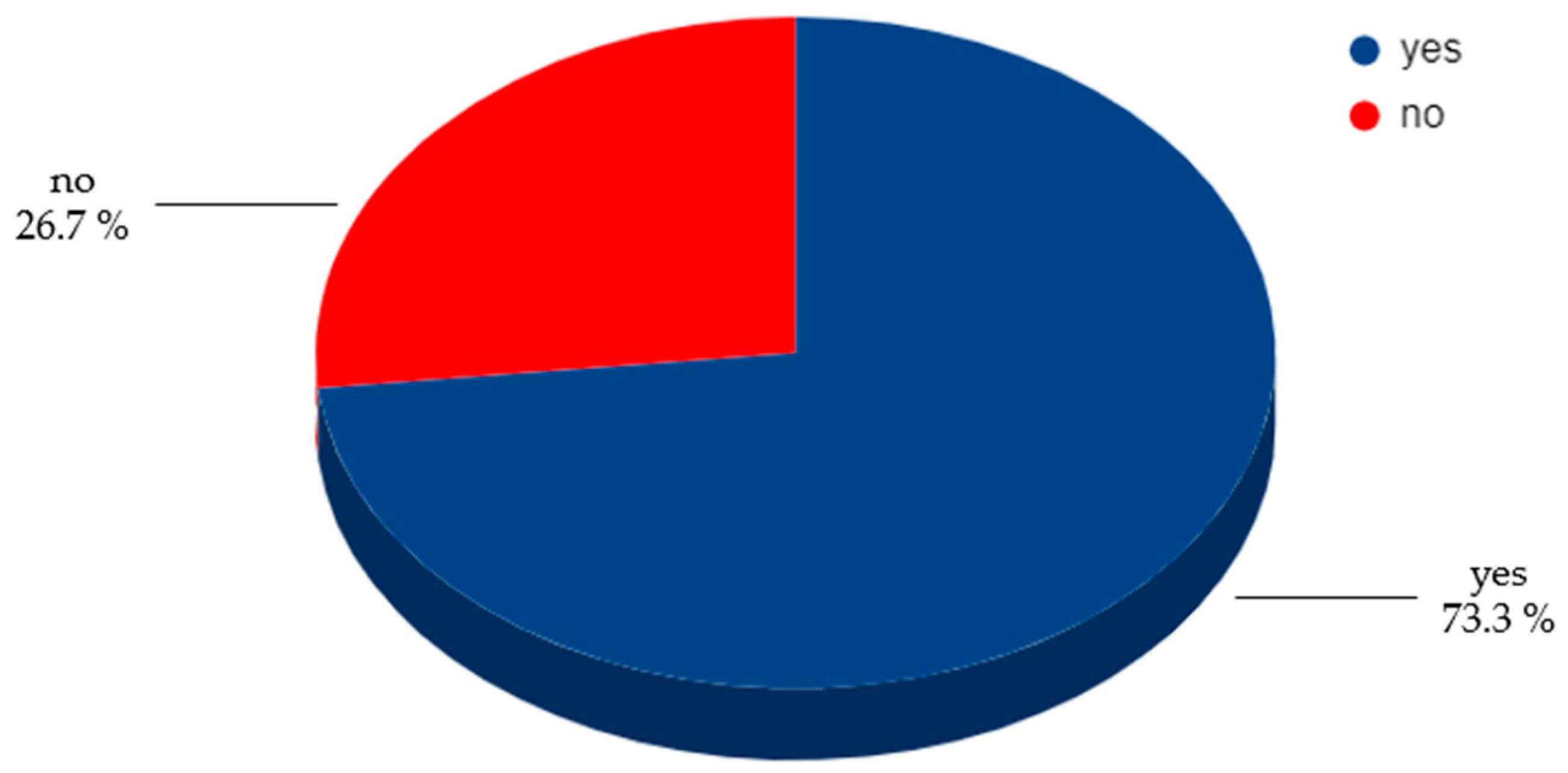
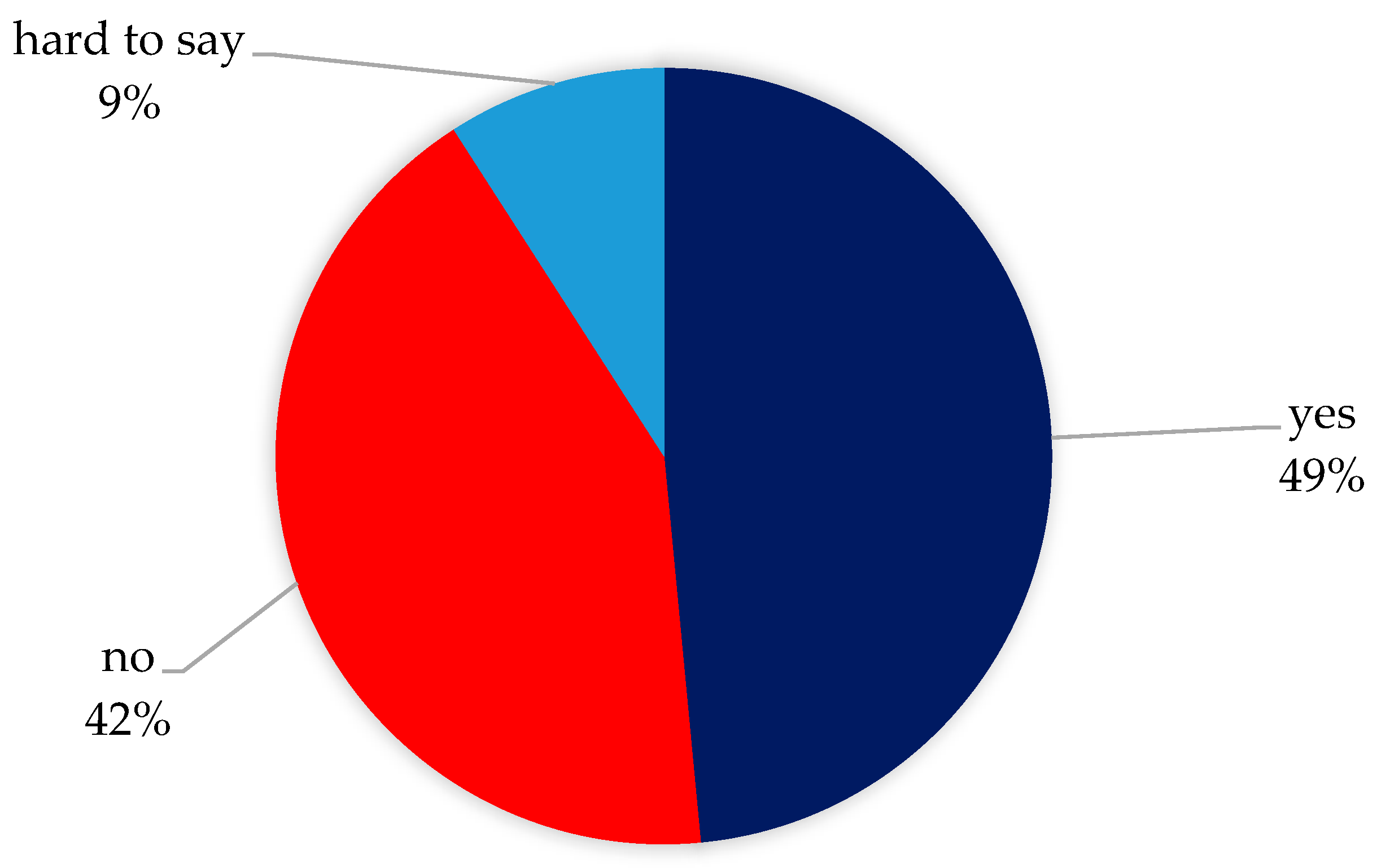
3.1. Characteristics of Study Group
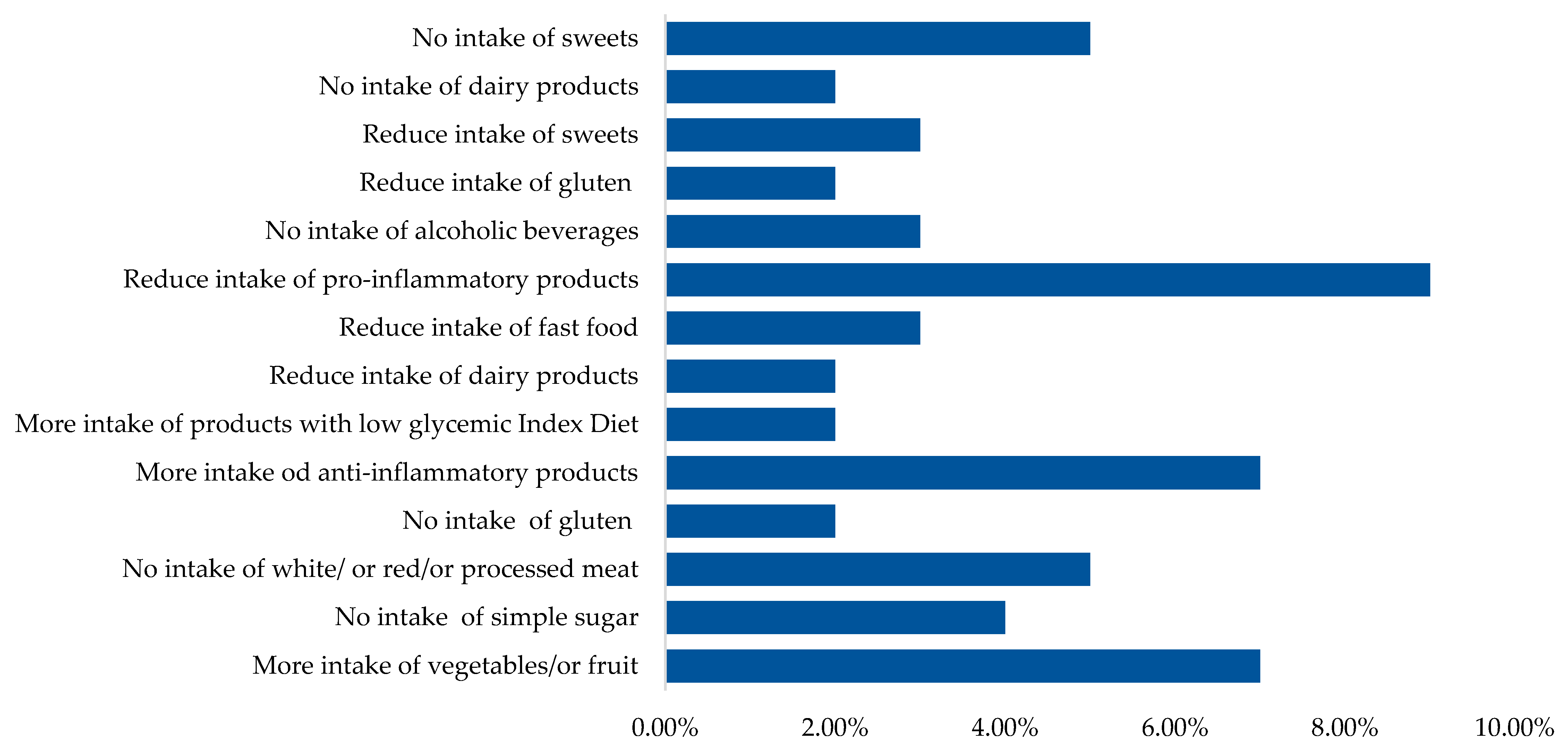
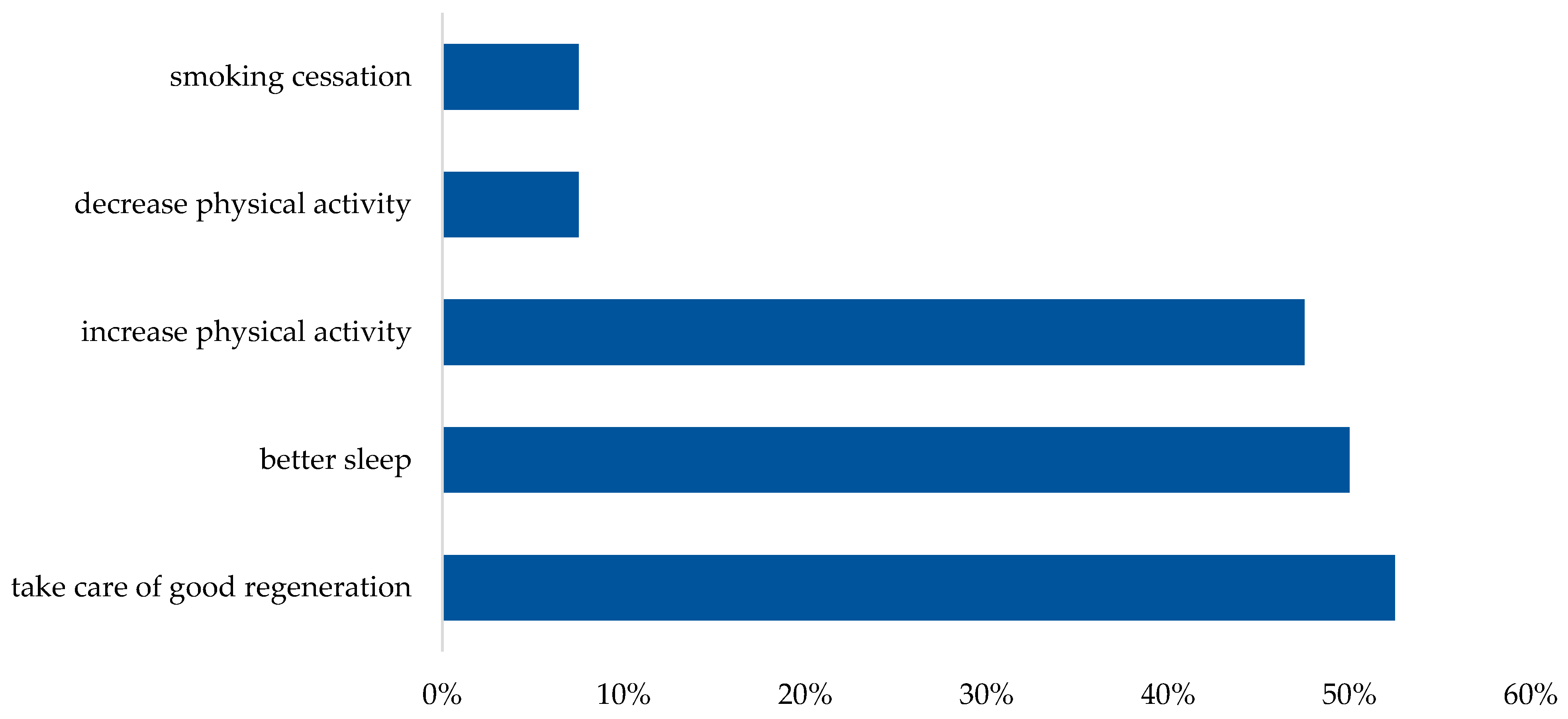
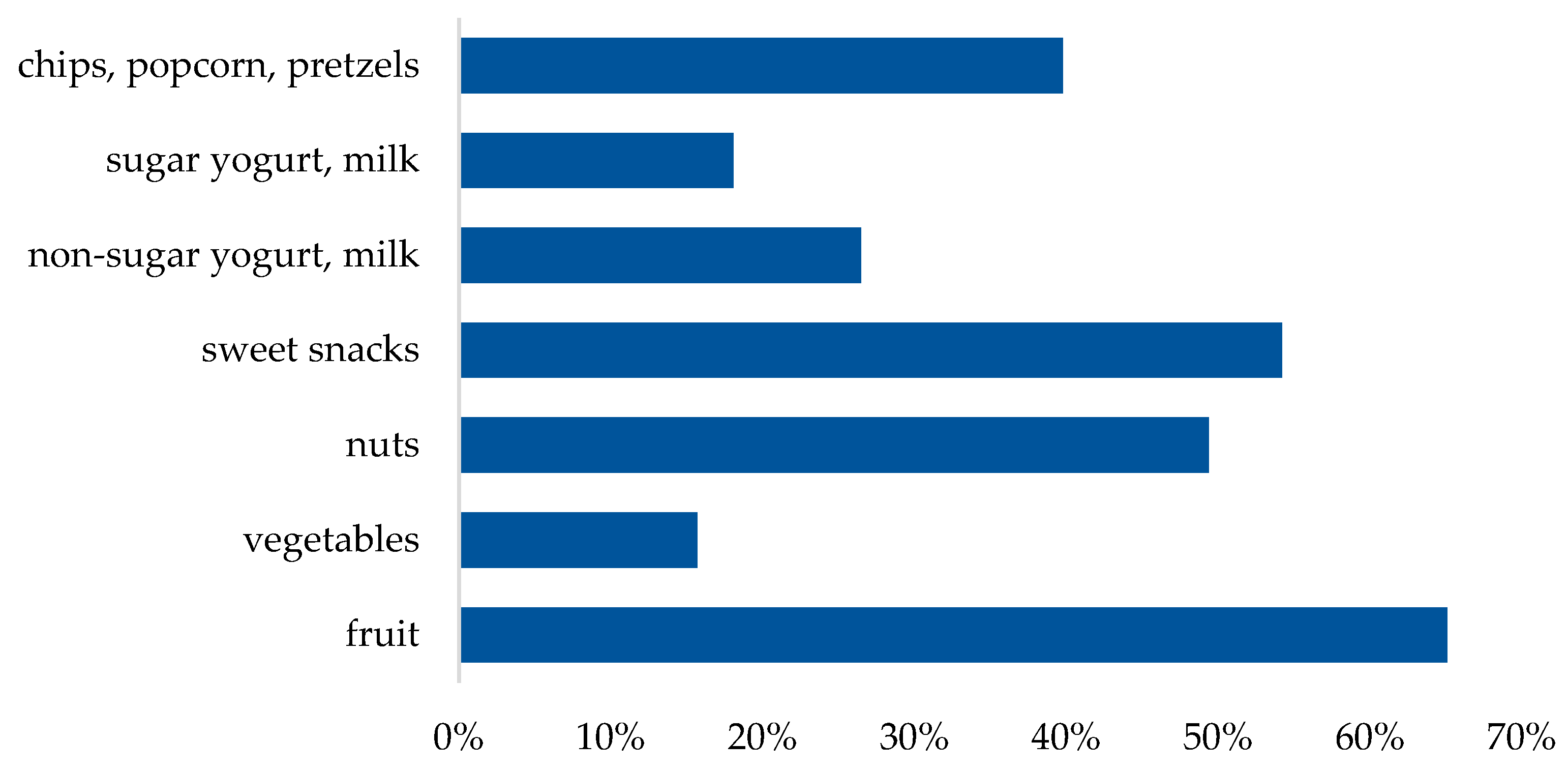
3.2. Frequency of Consumption of Selected Product Groups and Dietary Guidelines
3.3. Diet Quality
3.4. Nutritional Knowledge
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bulun, S.E.; Yilmaz, B.D.; Sison, C.; Miyazaki, K.; Bernardi, L.; Liu, S.; Kohlmeier, A.; Yin, P.; Milad, M.; Wei, J. Endometriosis. Endocr. Rev. 2019, 40, 1048–1079. [Google Scholar] [CrossRef]
- Taylor, H.S.; Kotlyar, A.M.; Flores, V.A. Endometriosis Is a Chronic Systemic Disease: Clinical Challenges and Novel Innovations. Lancet 2021, 397, 839–852. [Google Scholar] [CrossRef] [PubMed]
- Zondervan, K.T.; Becker, C.M.; Koga, K.; Missmer, S.A.; Taylor, R.N.; Viganò, P. Endometriosis. Nat. Rev. Dis. Primers 2018, 4, 9. [Google Scholar] [CrossRef] [PubMed]
- Czyzyk, A.; Podfigurna, A.; Szeliga, A.; Meczekalski, B. Update on Endometriosis Pathogenesis. Minerva Obstet. Gynecol. 2017, 69, 447–461. [Google Scholar] [CrossRef]
- Krakhotkin, D.V.; Silkina, M.N.; Chernylovskyi, V.A.; Gayvoronskaya, S.A. The Dienogest-Related Cystitis in Women with Endometriosis: A Prospective, Controlled, Comparative Study. J. Obstet. Gynaecol. 2022, 42, 2492–2497. [Google Scholar] [CrossRef] [PubMed]
- Smolarz, B.; Szyłło, K.; Romanowicz, H. Endometriosis: Epidemiology, Classification, Pathogenesis, Treatment and Genetics (Review of Literature). Int. J. Mol. Sci. 2021, 22, 10554. [Google Scholar] [CrossRef] [PubMed]
- Asghari, S.; Valizadeh, A.; Aghebati-Maleki, L.; Nouri, M.; Yousefi, M. Endometriosis: Perspective, Lights, and Shadows of Etiology. Biomed. Pharmacother. 2018, 106, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Litson, J.; Agnes, R.; Ravikumar, G. Histotyping and Grading of Endometriosis and Its Association with Clinico-Pathological Parameters. J. Obstet. Gynaecol. 2022, 42, 3628–3636. [Google Scholar] [CrossRef]
- Masciullo, L.; Viscardi, M.F.; Piacenti, I.; Scaramuzzino, S.; Cavalli, A.; Piccioni, M.G.; Porpora, M.G. A Deep Insight into Pelvic Pain and Endometriosis: A Review of the Literature from Pathophysiology to Clinical Expressions. Minerva Obstet. Gynecol. 2021, 73, 511–522. [Google Scholar] [CrossRef]
- Missmer, S.A.; Chavarro, J.E.; Malspeis, S.; Bertone-Johnson, E.R.; Hornstein, M.D.; Spiegelman, D.; Barbieri, R.L.; Willett, W.C.; Hankinson, S.E. A Prospective Study of Dietary Fat Consumption and Endometriosis Risk. Hum. Reproduct. 2010, 25, 1528–1535. [Google Scholar] [CrossRef]
- Marcinkowska, A.; Górnicka, M. The Role of Dietary Fats in the Development and Treatment of Endometriosis. Life 2023, 13, 654. [Google Scholar] [CrossRef]
- Jurkiewicz-Przondziono, J.; Lemm, M.; Kwiatkowska-Pamuła, A.; Ziółko, E.; Wójtowicz, M.K. Influence of Diet on the Risk of Developing Endometriosis. Ginekol. Pol. 2017, 88, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Signorile, P.G.; Viceconte, R.; Baldi, A. Novel Dietary Supplement Association Reduces Symptoms in Endometriosis Patients. J. Cell. Physiol. 2018, 233, 5920–5925. [Google Scholar] [CrossRef]
- Camuesco, D.; Gálvez, J.; Nieto, A.; Comalada, M.; Rodríguez-Cabezas, M.E.; Concha, A.; Xaus, J.; Zarzuelo, A. Dietary Olive Oil Supplemented with Fish Oil, Rich in EPA and DHA (n-3) Polyunsaturated Fatty Acids, Attenuates Colonic Inflammation in Rats with DSS-Induced Colitis. J. Nutr. 2005, 135, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Fjerbæk, A.; Knudsen, U.B. Endometriosis, Dysmenorrhea and Diet—What Is the Evidence? Eur. J. Obstet. Gynecol. Reprod. Biol. 2007, 132, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Bartiromo, L.; Schimberni, M.; Villanacci, R.; Ottolina, J.; Dolci, C.; Salmeri, N.; Viganò, P.; Candiani, M. Endometriosis and Phytoestrogens: Friends or Foes? A Systematic Review. Nutrients 2021, 13, 2532. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Liu, M.; Zhang, B.; Zhao, S.-J.; Jiang, S.-W. Phytoestrogens for the Management of Endometriosis: Findings and Issues. Pharmaceuticals 2021, 14, 569. [Google Scholar] [CrossRef]
- Attar, E.; Bulun, S.E. Aromatase and Other Steroidogenic Genes in Endometriosis: Translational Aspects. Hum. Reprod. Update 2006, 12, 49–56. [Google Scholar] [CrossRef]
- Tsubura, A.; Uehara, N.; Kiyozuka, Y.; Shikata, N. Dietary Factors Modifying Breast Cancer Risk and Relation to Time of Intake. J. Mammary Gland. Biol. Neoplasia 2005, 10, 87–100. [Google Scholar] [CrossRef]
- Huang, M.; Liu, J.; Lin, X.; Goto, A.; Song, Y.; Tinker, L.F.; Chan, K.K.; Liu, S. Relationship between Dietary Carbohydrates Intake and Circulating Sex Hormone-Binding Globulin Levels in Postmenopausal Women. J. Diabet. 2018, 10, 467–477. [Google Scholar] [CrossRef]
- Minihane, A.M.; Vinoy, S.; Russell, W.R.; Baka, A.; Roche, H.M.; Tuohy, K.M.; Teeling, J.L.; Blaak, E.E.; Fenech, M.; Vauzour, D.; et al. Low-Grade Inflammation, Diet Composition and Health: Current Research Evidence and Its Translation. Br. J. Nutr. 2015, 114, 999–1012. [Google Scholar] [CrossRef]
- Cirillo, M.; Argento, F.R.; Attanasio, M.; Becatti, M.; Ladisa, I.; Fiorillo, C.; Coccia, M.E.; Fatini, C. Atherosclerosis and Endometriosis: The Role of Diet and Oxidative Stress in a Gender-Specific Disorder. Biomedicines 2023, 11, 450. [Google Scholar] [CrossRef]
- Arab, A.; Karimi, E.; Vingrys, K.; Kelishadi, M.R.; Mehrabani, S.; Askari, G. Food Groups and Nutrients Consumption and Risk of Endometriosis: A Systematic Review and Meta-Analysis of Observational Studies. Nutr. J. 2022, 21, 58. [Google Scholar] [CrossRef]
- Sverrisdóttir, U.Á.; Hansen, S.; Rudnicki, M. Impact of Diet on Pain Perception in Women with Endometriosis: A Systematic Review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 271, 245–249. [Google Scholar] [CrossRef]
- Jeżewska-Zychowicz, M.; Gawęcki, J.; Wądołowska, L.; Czarnocińska, J.; Galiński, G.; Kołłajtis-Dołowy, A.; Roszkowski, W.; Wawrzyniak, A.; Przybyłowicz, K.; Krusińska, B.; et al. Dietary Habits and Nutrition Beliefs Questionnaire for people aged 16 to 65, version 1.1. In Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data (In Polish: Kwestionariusz do Badania Pogladów i Zwyczajów Żywieniowych oraz Procedura Opracowania Danych (KomPAN®)); Gawęcki, J., Ed.; Committee of Human Nutrition Science, Polish Academy of Science: Warsaw, Poland, 2014; pp. 3–20. Available online: http://www.knozc.pan.pl/ (accessed on 5 February 2023).
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-Item Mediterranean Diet Assessment Tool and Obesity Indexes among High-Risk Subjects: The PREDIMED Trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed]
- Branca, F.; Nikogosian, H.; Lobstein, T. The Challenge of Obesity in the WHO European Region and the Strategies for Response; World Health Organization, Ed.; WHO Regional Office for Europe: Copenhagen, Denmark, 2007. [Google Scholar]
- Ashwell, M.; Gibson, S. Waist-to-Height Ratio as an Indicator of ‘Early Health Risk’: Simpler and More Predictive than Using a ‘Matrix’ Based on BMI and Waist Circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef]
- Bieniek-Walenda, J.; Brończyk-Puzoń, A.; Jagielski, P. Ocena Poziomu Wiedzy Żywieniowej Za Pomocą Kwestionariusza komPAN Pacjentów Po Ostrym Zespole Wieńcowym Hospitalizowanych Na Oddziale Kardiologii Inwazyjnej. Doniesienie Wstępne. Fol. Cardiol. 2020, 15, 1–5. [Google Scholar] [CrossRef]
- Nodler, J.L.; DiVasta, A.D.; Vitonis, A.F.; Karevicius, S.; Malsch, M.; Sarda, V.; Fadayomi, A.; Harris, H.R.; Missmer, S.A. Supplementation with Vitamin D or ω-3 Fatty Acids in Adolescent Girls and Young Women with Endometriosis (SAGE): A Double-Blind, Randomized, Placebo-Controlled Trial. Am. J. Clin. Nutr. 2020, 112, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Harris, H.R.; Eke, A.C.; Chavarro, J.E.; Missmer, S.A. Fruit and Vegetable Consumption and Risk of Endometriosis. Hum. Reprod. 2018, 33, 715–727. [Google Scholar] [CrossRef] [PubMed]
- Nodler, J.L.; Harris, H.R.; Chavarro, J.E.; Frazier, A.L.; Missmer, S.A. Dairy Consumption during Adolescence and Endometriosis Risk. Am. J. Obstet. Gynecol. 2020, 222, e1–e257. [Google Scholar] [CrossRef]
- Barnard, N.D.; Holtz, D.N.; Schmidt, N.; Kolipaka, S.; Hata, E.; Sutton, M.; Znayenko-Miller, T.; Hazen, N.D.; Cobb, C.; Kahleova, H. Nutrition in the Prevention and Treatment of Endometriosis: A Review. Front. Nutr. 2023, 10, 1089891. [Google Scholar] [CrossRef] [PubMed]
- Velho, R.V.; Werner, F.; Mechsner, S. Endo Belly: What Is It and Why Does It Happen?—A Narrative Review. J. Clin. Med. 2023, 12, 7176. [Google Scholar] [CrossRef] [PubMed]
- Nap, A.; De Roos, N. Endometriosis and the Effects of Dietary Interventions: What Are We Looking For? Reprod. Fertil. 2022, 3, C14–C22. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, F. Selected Food Intake and Risk of Endometriosis. Hum. Reprod. 2004, 19, 1755–1759. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Holford, T.R.; Zhang, Y.; Boyle, P.; Mayne, S.T.; Dai, M.; Zheng, T. Dietary Fiber Intake and Risk of Breast Cancer by Menopausal and Estrogen Receptor Status. Eur. J. Nutr. 2013, 52, 217–223. [Google Scholar] [CrossRef]
- Zemel, M.B.; Sun, X. Dietary Calcium and Dairy Products Modulate Oxidative and Inflammatory Stress in Mice and Humans. J. Nutr. 2008, 138, 1047–1052. [Google Scholar] [CrossRef]
- Bedaiwy, M.A. Prediction of Endometriosis with Serum and Peritoneal Fluid Markers: A Prospective Controlled Trial. Hum. Reprod. 2002, 17, 426–431. [Google Scholar] [CrossRef]
- Gutiérrez, S.; Svahn, S.L.; Johansson, M.E. Effects of Omega-3 Fatty Acids on Immune Cells. Int. J. Mol. Sci. 2019, 20, 5028. [Google Scholar] [CrossRef]
- Krabbenborg, I.; De Roos, N.; Van Der Grinten, P.; Nap, A. Diet Quality and Perceived Effects of Dietary Changes in Dutch Endometriosis Patients: An Observational Study. Reprod. BioMed. Online 2021, 43, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Armour, M.; Sinclair, J.; Chalmers, K.J.; Smith, C.A. Self-management strategies amongst Australian women with endometriosis: A national online survey. BMC Complement. Altern. Med. 2019, 19, 17. [Google Scholar] [CrossRef]
- Mazza, E.; Troiano, E.; Mazza, S.; Ferro, Y.; Abbinante, A.; Agneta, M.T.; Montalcini, T.; Pujia, A. The Impact of Endometriosis on Dietary Choices and Activities of Everyday Life: A Cross-Sectional Study. Front. Nutr. 2023, 10, 1273976. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, R.; Stratopoulou, C.A.; Dolmans, M.-M. Pathogenesis of Endometriosis: New Insights into Prospective Therapies. Int. J. Mol. Sci. 2021, 22, 11700. [Google Scholar] [CrossRef] [PubMed]
- Dunselman, G.A.J.; Vermeulen, N.; Becker, C.; Calhaz-Jorge, C.; D’Hooghe, T.; De Bie, B.; Heikinheimo, O.; Horne, A.W.; Kiesel, L.; Nap, A.; et al. ESHRE Guideline: Management of Women with Endometriosis. Hum. Reprod. 2014, 29, 400–412. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, J.; Fialho, M.; Santos, R.; Peixoto-Plácido, C.; Madeira, T.; Sousa-Santos, N.; Virgolino, A.; Santos, O.; Vaz Carneiro, A. Is Olive Oil Good for You? A Systematic Review and Meta-Analysis on Anti-Inflammatory Benefits from Regular Dietary Intake. Nutrition 2020, 69, 110559. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, G.K.; Keast, R.S.J.; Morel, D.; Lin, J.; Pika, J.; Han, Q.; Lee, C.-H.; Smith, A.B.; Breslin, P.A.S. Ibuprofen-like Activity in Extra-Virgin Olive Oil. Nature 2005, 437, 45–46. [Google Scholar] [CrossRef] [PubMed]
- Kunnumakkara, A.B.; Sailo, B.L.; Banik, K.; Harsha, C.; Prasad, S.; Gupta, S.C.; Bharti, A.C.; Aggarwal, B.B. Chronic Diseases, Inflammation, and Spices: How Are They Linked? J. Transl. Med. 2018, 16, 14. [Google Scholar] [CrossRef] [PubMed]
- Opara, E.; Chohan, M. Culinary Herbs and Spices: Their Bioactive Properties, the Contribution of Polyphenols and the Challenges in Deducing Their True Health Benefits. Int. J. Mol. Sci. 2014, 15, 19183–19202. [Google Scholar] [CrossRef] [PubMed]
- Ott, J.; Nouri, K.; Hrebacka, D.; Gutschelhofer, S.; Huber, J.; Wenzl, R. Endometriosis and Nutrition-Recommending a Mediterranean Diet Decreases Endometriosis-Associated Pain: An Experimental Observational Study. J. Aging Res. Clin. Pract. 2012, 1, 162. [Google Scholar]
- Van Haaps, A.; Wijbers, J.; Schreurs, A.; Mijatovic, V. A Better Quality of Life Could Be Achieved by Applying the Endometriosis Diet: A Cross-Sectional Study in Dutch Endometriosis Patients. Reprod. BioMed. Online 2023, 46, 623–630. [Google Scholar] [CrossRef]
- Youseflu, S.; Sadatmahalleh, S.J.; Mottaghi, A.; Kazemnejad, A. Dietary Phytoestrogen Intake and The Risk of Endometriosis in Iranian Women: A Case-Control Study. Int. J. Fertil. Steril. 2020, 13, 296–300. [Google Scholar] [CrossRef]
- Noel, J.-C.; Anaf, V.; Fayt, I.; Wespes, E. Ureteral Mullerian Carcinosarcoma (Mixed Mullerian Tumor) Associated with Endometriosis Occurring in a Patient with a Concentrated Soy Isoflavones Supplementation. Arch. Gynecol. Obstet. 2006, 274, 389–392. [Google Scholar] [CrossRef]
- Van Haaps, A.P.; Wijbers, J.V.; Schreurs, A.M.F.; Vlek, S.; Tuynman, J.; De Bie, B.; De Vogel, A.L.; Van Wely, M.; Mijatovic, V. The Effect of Dietary Interventions on Pain and Quality of Life in Women Diagnosed with Endometriosis: A Prospective Study with Control Group. Hum. Reprod. 2023, 38, 2433–2446. [Google Scholar] [CrossRef]
- Ek, M.; Roth, B.; Ekström, P.; Valentin, L.; Bengtsson, M.; Ohlsson, B. Gastrointestinal Symptoms among Endometriosis Patients—A Case-Cohort Study. BMC Women’s Health 2015, 15, 59. [Google Scholar] [CrossRef] [PubMed]
- Brouns, F.; Van Haaps, A.; Keszthelyi, D.; Venema, K.; Bongers, M.; Maas, J.; Mijatovic, V. Diet Associations in Endometriosis: A Critical Narrative Assessment with Special Reference to Gluten. Front. Nutr. 2023, 10, 1166929. [Google Scholar] [CrossRef]
- Moore, J.S.; Gibson, P.R.; Perry, R.E.; Burgell, R.E. Endometriosis in Patients with Irritable Bowel Syndrome: Specific Symptomatic and Demographic Profile, and Response to the Low FODMAP Diet. Aust. N. Z. J. Obst. Gynaecol. 2017, 57, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Marziali, M.; Venza, M.; Lazzaro, S.; Lazzaro, A.; Micossi, C.; Stolfi, V.M. Gluten-Free Diet: A New Strategy for Management of Painful Endometriosis Related Symptoms? Minerva Chir. 2012, 67, 499–504. [Google Scholar]
- Borghini, R.; Porpora, M.G.; Casale, R.; Marino, M.; Palmieri, E.; Greco, N.; Donato, G.; Picarelli, A. Irritable Bowel Syndrome-Like Disorders in Endometriosis: Prevalence of Nickel Sensitivity and Effects of a Low-Nickel Diet. An Open-Label Pilot Study. Nutrients 2020, 12, 341. [Google Scholar] [CrossRef]
- Huijs, E.; Nap, A. The Effects of Nutrients on Symptoms in Women with Endometriosis: A Systematic Review. Reprod. BioMed. Online 2020, 41, 317–328. [Google Scholar] [CrossRef]
- Adler, H.; Lewis, M.; Ng, C.H.M.; Brooks, C.; Leonardi, M.; Mikocka-Walus, A.; Bush, D.; Semprini, A.; Wilkinson-Tomey, J.; Condous, G.; et al. Social Media, Endometriosis, and Evidence-Based Information: An Analysis of Instagram Content. Healthcare 2024, 12, 121. [Google Scholar] [CrossRef] [PubMed]
- Bykowska-Derda, A.; Czlapka-Matyasik, M.; Kaluzna, M.; Ruchala, M.; Ziemnicka, K. Diet Quality Scores in Relation to Fatness and Nutritional Knowledge in Women with Polycystic Ovary Syndrome: Case-Control Study. Public Health Nutr. 2021, 24, 3389–3398. [Google Scholar] [CrossRef]
- Yamamoto, A.; Harris, H.R.; Vitonis, A.F.; Chavarro, J.E.; Missmer, S.A. A Prospective Cohort Study of Meat and Fish Consumption and Endometriosis Risk. Am. J. Obstet. Gynecol. 2018, 219, e1–e178. [Google Scholar] [CrossRef]
- Nirgianakis, K.; Egger, K.; Kalaitzopoulos, D.R.; Lanz, S.; Bally, L.; Mueller, M.D. Effectiveness of Dietary Interventions in the Treatment of Endometriosis: A Systematic Review. Reprod. Sci. 2022, 29, 26–42. [Google Scholar] [CrossRef] [PubMed]
- Piecuch, M.; Garbicz, J.; Waliczek, M.; Malinowska-Borowska, J.; Rozentryt, P. I Am the 1 in 10—What Should I Eat? A Research Review of Nutrition in Endometriosis. Nutrients 2022, 14, 5283. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total | Endometriosis n = 45 | Non-Endometriosis n = 45 | p-Value * |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Age [y] | 31.55 ± 6.60 | 33.13 ± 5.78 | 29.98 ± 6.98 | 0.007 |
| Height [cm] | 165.96 ± 6.51 | 165.57 ± 6.88 | 166.33 ± 6.10 | ns |
| Body mass [kg] | 60.52 ± 10.51 | 59.60 ± 10.81 | 61.44 ± 10.12 | ns |
| BMI (kg/m2) | 21.96 ± 3.55 | 21.67 ± 3.21 | 22.26 ± 3.85 | ns |
| Self-reported health status | [n, %] | |||
| very good | 14 (15.6%) | 3 (6.7%) | 11 (24.4%) | 0.001 |
| good | 30 (33.3%) | 7 (15.6%) | 23 (51.1%) | |
| fair | 28 (31.1%) | 19 (42.2%) | 9 (20.0%) | |
| hard to say | 8 (8.9%) | 7 (15.6%) | 1 (2.2%) | |
| poor | 10 (11.1%) | 9 (20.0%) | 1 (2.2%) | |
| Physical activity | [n, %] | |||
| low | 53 (58.9%) | 25 (55.5%) | 28 (62.2%) | 0.563 |
| moderate | 25 (27.8%) | 13 (28.9%) | 12 (26.7%) | |
| vigorous | 12 (13.3%) | 7 (15.6%) | 5 (11.1%) | |
| Dietary Habits | Total n, % | Endometriosis n, % | Non-Endometriosis n, % | p-Value * |
|---|---|---|---|---|
| Number of meals | ||||
| 1–2 | 3 (3.3%) | 0 | 3 (6.7%) | 0.03 |
| 3–4 | 67 (74.5%) | 31 (68.9%) | 36 (80%) | |
| 5 | 20 (22.2%) | 14 (31.1%) | 6 (13.3%) | |
| Eating regularly | ||||
| Yes | 82 (91.1%) | 41 (91.1%) | 41 (91.1%) | ns |
| No | 8 (8.9%) | 4 (8.9%) | 4 (8.9%) | |
| Snacking | ||||
| Yes | 82 (91.1%) | 39 (91.1%) | 43 (95.6%) | ns |
| No | 8 (8.9%) | 6 (8.9%) | 2 (4.4%) | |
| Frequency of eating snacks | ||||
| several times a day | 6 (7.3%) | 2 (5.1%) | 4 (9.3%) | p < 0.001 |
| once a day | 11 (13.4%) | 3 (7.7%) | 8 (18.6%) | |
| several times a week | 36 (44.0%) | 14 (35.9%) | 22 (51.2%) | |
| once a week | 18 (21.9%) | 12 (30.8%) | 6 (14.0%) | |
| 1–3 times a month | 11 (13.4%) | 8 (20.5%) | 3 (6.9%) |
| Food Groups | Total n = 90 | Endometriosis n = 45 | Non-Endometriosis n = 45 | p-Value * |
|---|---|---|---|---|
| Mean ± SD Median | Mean ± SD Median | Mean ± SD Median | ||
| Vegetables | 5.54 ± 0.96 | 5.62 ± 0.82 | 5.46 ± 1.07 | ns |
| 6 | 6 | 6 | ||
| Fruits | 5.26 ± 1.04 | 5.33 ± 1.05 | 5.18 ± 1.02 | ns |
| 5 | 6 | 5 | ||
| Whole grain bread | 3.77 ± 1.57 | 3.77 ± 1.81 | 3.77 ± 1.27 | ns |
| 4 | 4 | 4 | ||
| White bread | 3.50 ± 1.60 | 3.07 ± 1.74 | 3.93 ± 1.32 | 0.015 |
| 4 | 3 | 4 | ||
| Whole grain cereals, oatmeal, whole grain pasta | 3.54 ± 1.26 | 3.80 ± 1.30 | 3.29 ± 1.17 | ns |
| 4 | 4 | 4 | ||
| White rice, noodles, finely ground groats | 3.17 ± 1.03 | 2.84 ± 1.02 | 3.49 ± 0.93 | 0.007 |
| 3 | 3 | 4 | ||
| Nuts | 2.53 ± 1.15 | 3.00 ± 1.03 | 2.07 ± 1.06 | 0.0002 |
| 3 | 3 | 3 | ||
| Legumes | 2.87 ± 1.27 | 3.13 ± 1.17 | 2.59 ± 1.30 | 0.032 |
| 3 | 3 | 2 | ||
| Fish | 2.46 ± 0.92 | 2.76 ± 0.95 | 2.18 ± 0.79 | 0.006 |
| 2 | 3 | 2 | ||
| Eggs | 3.63 ± 1.12 | 3.82 ± 1.12 | 3.44 ± 1.09 | ns |
| 4 | 4 | 4 | ||
| Vegetable oils | 3.68 ± 1.53 | 3.22 ± 1.69 | 4.13 ± 1.20 | 0.016 |
| 4 | 4 | 4 | ||
| Butter | 3.34 ± 1.80 | 3.39 ± 1.88 | 3.29 ± 1.73 | ns |
| 3 | 3 | 3 | ||
| Red meat | 2.36 ± 1.20 | 2.18 ± 1.08 | 2.53 ± 1.28 | ns |
| 2 | 2 | 3 | ||
| White meat | 3.26 ± 1.39 | 3.44 ± 1.40 | 3.07 ± 1.36 | ns |
| 4 | 4 | 4 | ||
| Milk | 3.27 ± 1.76 | 2.84 ± 1.73 | 3.80 ± 1.61 | 0.013 |
| 4 | 3 | 4 | ||
| Fermented milk drinks | 3.44 ± 1.38 | 3.16 ± 1.49 | 3.71 ± 1.20 | ns |
| 4 | 3 | 4 | ||
| Cottage cheese | 2.73 ± 1.37 | 2.47 ± 1.34 | 3.00 ± 1.35 | ns |
| 4 | 3 | 4 | ||
| Cheese | 3.11 ± 1.40 | 2.55 ± 1.34 | 3.67 ± 1.23 | 0.0001 |
| 3 | 2 | 4 | ||
| Fried dishes | 3.11 ± 1.06 | 2.84 ± 1.07 | 3.39 ± 0.98 | 0.026 |
| 3 | 3 | 4 | ||
| Fast food products | 2.0 ± 0.7 | 1.82 ± 0.7 | 2.18 ± 0.64 | 0.014 |
| 2 | 2 | 2 | ||
| Water | 5.86 ± 0.6 | 5.93 ± 0.33 | 5.78 ± 0.79 | ns |
| 6 | 6 | 6 |
| Diet Indexes | Total n = 90 | Endometriosis n = 45 | Non-Endometriosis n = 45 | p-Value * |
|---|---|---|---|---|
| Mean ± SD Median | Mean ± SD Median | Mean ± SD Median | ||
| pHDI-10 (%) | 31.4 ± 10.64 | 32.64 ± 11.47 | 30.1 ± 9.57 | ns |
| 29.75 | 30 | 29.50 | ||
| MDS (points) | 6.82 ± 1.78 | 7.55 ± 1.80 | 6.09 ± 1.44 | 0.0001 |
| 7 | 8 | 6 |
| Variables | Nutritional Knowledge Level | p-Value * | ||
|---|---|---|---|---|
| Insufficient | Sufficient | Good | ||
| Total group (n, %) | 2 (2.2%) | 36 (40%) | 52 (57.8%) | - |
| Endometriosis (n, %) | ||||
| Yes | 1 (1.1%) | 21 (46.7%) | 23 (51.1%) | p = 0.047 |
| No | 1 (2.2%) | 15 (33.3%) | 29 (64.4%) | |
| MDS | ns | |||
| ≤7 | 2 (100%) | 24 (66.7%) | 30 (57.7%) | |
| 8–9 | 0 | 10 (27.8%) | 17 (32.7%) | |
| ≥10 | 0 | 2 (5.56%) | 5 (9.6%) | |
| pHDI-10 (n, %) | ns | |||
| low | 0 | 32 (88.9%) | 40 (76. 9%) | |
| moderate | 0 | 4 (11.1%) | 12 (23.1%) | |
| high | 0 | 0 | 0 | |
| BMI (kg/m2) | 21.40 ± 0.83 | 22.67 ± 4.08 | 21.50 ± 3.13 | ns |
| Age | 37 ± 2 | 31.95 ± 6.26 | 32.14 ± 6.49 | ns |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bogusz, A.; Górnicka, M. Low Diet Quality and Nutritional Knowledge in Women with Endometriosis: A Pilot Study. Healthcare 2024, 12, 673. https://doi.org/10.3390/healthcare12060673
Bogusz A, Górnicka M. Low Diet Quality and Nutritional Knowledge in Women with Endometriosis: A Pilot Study. Healthcare. 2024; 12(6):673. https://doi.org/10.3390/healthcare12060673
Chicago/Turabian StyleBogusz, Angelika, and Magdalena Górnicka. 2024. "Low Diet Quality and Nutritional Knowledge in Women with Endometriosis: A Pilot Study" Healthcare 12, no. 6: 673. https://doi.org/10.3390/healthcare12060673
APA StyleBogusz, A., & Górnicka, M. (2024). Low Diet Quality and Nutritional Knowledge in Women with Endometriosis: A Pilot Study. Healthcare, 12(6), 673. https://doi.org/10.3390/healthcare12060673







