Abstract
This study explored the associations between personality dimensions, burnout, and psychopathology in healthcare professionals in intensive care units (ICUs). This study further aimed to discern the differences in these relationships when considering the variables of critical care experience (less than 5 years, 5–10 years, and more than 10 years), profession (nurses versus intensivists), and the urban size of the city where the ICU is located (metropolitan cities versus smaller urban cities). This cross-sectional investigation’s outcomes are based on data from 503 ICU personnel, including 155 intensivists and 348 nurses, in 31 ICU departments in Greece. Participants underwent a comprehensive assessment involving a sociodemographic questionnaire, the Eysenck Personality Questionnaire (EPQ), the Maslach Burnout Inventory (MBI), and the Symptom Checklist-90 (SCL-90). To analyze the interplay among critical care experience, burnout status, and psychopathology, a moderation analysis was conducted with personality dimensions (i.e., psychoticism, extraversion, and neuroticism) serving as the mediator variable. Profession and the urban size of the ICU location were considered as moderators influencing these relationships. Male healthcare professionals showed higher psychoticism levels than females, aligning with prior research. Experienced nurses reported lower personal achievement, hinting at potential motivation challenges for professional growth. Psychoticism predicted high depersonalization and low personal achievement. Neuroticism and psychoticism negatively impacted ICU personnel’s mental well-being, reflected in elevated psychopathology scores and burnout status. Psychoticism appears to be the primary factor influencing burnout among the three personality dimensions, particularly affecting intensivists. In contrast, nurses are more influenced by their critical care experience on their mental health status.
1. Introduction
The term “burnout” was coined by Freudenberger in 1974, who observed declining motivation and commitment among mental health clinic volunteers [1]. Maslach further advanced the concept, creating the widely used Maslach Burnout Inventory (MBI) [2]. According to this framework, burnout syndrome involves emotional exhaustion, physical fatigue, and cognitive weariness due to prolonged uncontrolled work-related stressors [3]. The syndrome comprises three main dimensions: high emotional exhaustion, high depersonalization, and low personal achievement [4]. High emotional exhaustion involves work-related fatigue, marked by feelings of energy depletion, whereas high depersonalization is a defense mechanism, leading to distancing from work through negativism or cynicism. Low personal achievement reflects frustration with work-related achievements, resulting in reduced professional efficiency [4].
Burnout is influenced by enduring personal and environmental stressors, such as major illness, family difficulties, or persistent adversity [5]. In healthcare, burnout syndrome and stress-related disorders are prevalent, impacting various roles like nurses [6,7], emergency room physicians [8], and intensive care unit (ICU) physicians [9,10]. Mental health professionals are also susceptible to high levels of burnout syndrome [11] due to the significant emotional and cognitive stress associated with their profession [12]. Factors associated with physician burnout include age, sex, marital status, personality traits, ICU work experience, work environment, workload, shift work, ethical issues, and end-of-life decision-making [13].
Notably, burnout in physicians is associated with increased risks of major medical errors, reduced patient care quality [14,15], absenteeism, decreased productivity [16,17,18], and impaired team relationships [19], leading to worsened care quality and higher healthcare costs [3,20]. Nurses often experience burnout due to factors like high workload, value incongruence, low job control, limited decision latitude, poor social climate/support, and insufficient rewards [21]. A common factor across all professions may be the problem of aggression faced by healthcare workers. This aggression, whether it comes from patients or workplace interactions, is considered a precursor to burnout [22,23,24].
Burnout has emerged as a pervasive issue among healthcare professionals [3]. For example, Woo et al. [25] found that 11.23% of nurses globally have experienced symptoms of burnout. In the field of emergency medicine, healthcare workers exhibit a burnout prevalence rate of 20–60% [26]. Similarly, 40% of mental health professionals have encountered burnout [11], and Rotenstein et al. [27] report that 67% of physicians have demonstrated overall burnout prevalence estimates. In the ICU setting, burnout is reported more prevalently among nurses than physicians [28,29], with direct implications for work, personal functionality, and overall healthcare services [30].
A challenge in current burnout research is the absence of agreed-upon terminology, as demonstrated by the numerous definitions identified, such as in the comprehensive review by Rotenstein et al. [27], covering 182 studies and 109,628 individuals across 45 countries. This lack of consensus leads to widely varying reported prevalence rates, with substantial fluctuations in burnout rates among physicians and within specific subscales [27]. The prevalence of burnout in the ICU setting also shows significant variability [13,31].
Personality traits significantly impact burnout experiences under similar work conditions [32]. Utilizing the dimensions of psychoticism (P), extraversion (E), and neuroticism (N), also known as Eysenck’s PEN model [33,34], this study defines personality through these three dimensions [35]. The PEN model posits that these dimensions represent fundamental aspects of an individual’s personality, influencing their behavior, cognition, and emotional responses [33,34,36]. Specifically, psychoticism is associated with traits such as disagreeableness, non-conscientiousness, and a propensity for risk-taking. Extraversion encompasses characteristics like sociability, assertiveness, positive emotions, and impulsivity, while neuroticism involves traits such as anxiety, depression, and self-doubt. Furthermore, these personality dimensions—P, E, and N—are considered orthogonal [37], indicating no correlation between them, thus contributing to a comprehensive understanding of various facets of an individual’s personality [36].
Neuroticism and lower extraversion are commonly associated with elevated burnout levels among nurses and physicians [29,38,39,40,41,42,43]. However, there is a notable scarcity of studies comparing personality traits between nurses and physicians [44], particularly within the ICU environment. Understanding such distinctions could have far-reaching implications for team dynamics, patient care, workplace satisfaction, and healthcare system improvement.
Personality differences are observed among rural and urban residents, with environmental factors influencing personality structure and exacerbating feelings of anxiety and depression [45,46]. Urban characteristics, such as exposure to heavy metals, pesticides, bisphenol A (BPA), noise pollution, and poor air quality, are linked to mental health conditions [47,48,49,50,51,52]. In Greek metropolitan areas like Athens and Thessaloniki, high population density and limited green spaces pose challenges [53]. Despite these, specialized hospitals in these regions serve wider areas in southern and northern Greece. The lower nurse-to-ICU bed ratio in metropolitan hospitals during COVID-19 [54] suggests an added psychological burden on ICU personnel, raising questions about the mental impact on healthcare workers in large urban areas compared to smaller cities.
Aim of the Study
This study delves into the intricate connections among socio-demographics, personality traits, psychopathology, and burnout in ICU personnel. Using a moderated mediation model, it explores the nuanced interplay involving critical care experience, personality dimensions, burnout, profession, and hospital location. Critical care experience serves as the independent variable, with personality dimensions mediating the relationship between experience and burnout. Additionally, the nurse or intensivist profession and the urban status of the hospital act as moderators, examining variations based on professional role and urban size. This design allows for assessing both direct and mediated effects as well as investigating whether the mediation process varies with moderator variables. In essence, we tested the moderated mediation model illustrated in Figure 1.
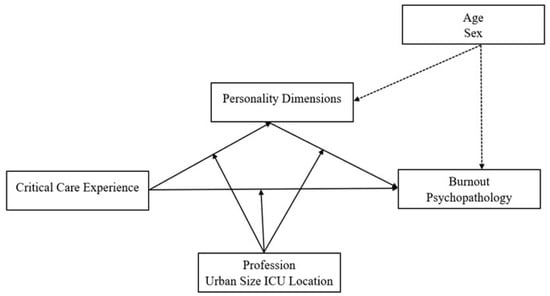
Figure 1.
Theoretical moderated mediation model. Notes: Personality dimensions are hypothesized to mediate the relationship between critical care experience and burnout/psychopathology. In contrast, profession, and urban size of ICU location (and potentially age and sex) are hypothesized to moderate the relationships within the model.
Among other inquiries, the model addresses the following research questions:
- How do personality dimensions differentiate as age increase?
- How do personality traits vary between male and female ICU personnel?
- What is the relationship between critical care experience, burnout, and psychopathology?
- Does the relationship between critical care experience, burnout, and psychopathology vary depending on the profession or the urban size of the ICU location?
- How do personality dimensions and profession interact in predicting burnout?
- Does the effect of critical care experience on burnout and psychopathology vary between nurses and intensivists or between ICU location in small and large cities?
Understanding these connections is vital for theoretical advancement and targeted interventions to improve the well-being of ICU personnel. This research has the potential to contribute to tailored support systems, addressing the unique needs of intensivists and nurses in high-stress environments.
2. Methods
2.1. Participants and Study Design
This study involved a cross-sectional investigation conducted with a sample of 573 respondents drawn from 31 ICUs in 10 cities across Greece. The sampling process took place between December 2021 and June 2022. Out of the total 573 ICU personnel, 23 individuals were excluded from subsequent analysis as they did not fit the roles of nurses or physicians. Additionally, from the remaining 550 participants, 47 were identified with at least one missing value in the required demographic or professional characteristics, leading to their exclusion from further analysis. Consequently, the results presented in this study are based on data obtained from the remaining 503 respondents, comprising 155 intensivists and 348 nurses.
2.2. Measurements
The participants were asked to anonymously complete a sociodemographic questionnaire, which encompassed necessary personal and professional information. Additionally, they were required to fill out the adapted to Greek-language versions of the Maslach Burnout Inventory (MBI) [55], the Eysenck Personality Questionnaire (EPQ) [56], and the Symptom Checklist 90 (SCL-90) [57].
The MBI, developed by Maslach and Jackson [2], assesses burnout through 22 items grouped into three subscales: emotional exhaustion, depersonalization, and personal achievement. Respondents rate each item on a 7-point Likert scale ranging from ‘never’ (0) to ‘daily’ (6). The scale has been translated into Greek and has shown satisfactory validity and reliability [55]. In this study, we used the established thresholds on the three subscales, based on the adapted Greek version by Zis et al. [58]. Specifically, burnout was identified for scores ≥ 34 in emotional exhaustion, ≥13 in depersonalization, and ≤29 in personal achievement.
The EPQ, developed by Eysenck and Eysenck [35], assesses personality traits using a 90-item questionnaire. It measures three primary dimensions: extraversion, neuroticism, and psychoticism. Respondents rate each item on a binary scale (yes/no response). The scale has been translated into Greek and has shown satisfactory validity and reliability [56].
The SCL-90, developed by Derogatis [59], assesses a wide range of psychological symptoms. It comprises 90 questions across 9 subscales, namely somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Participants rate items on a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely) based on distress level. Additionally, three global indices (global severity index [GSI], positive symptom distress index [PSDI], and positive symptom total [PST]) summarize psychological distress. The scale has been translated into Greek and validated for criterion and convergent validity [57]. This study reports data only for the GSI index, a measure that reflects the overall psychopathology. A higher GSI score indicates higher levels of psychological distress.
Participants provided verbal informed consent prior to their involvement in the study, and ethical approval was granted by the Ethics Committee of the University Hospital of Ioannina (protocol code 3263, dated 1 February 2019). Participants were also assigned unique identifiers to anonymize their data, and only authorized researchers had access to the raw data.
2.3. Statistical Analysis
Initial data analysis involved summarizing measures of central tendency and dispersion, with means and standard deviations reported for continuous variables and proportions for categorical ones. To compare groups, we employed independent samples t-tests, chi-squared tests of independence, and one-way ANOVA. To evaluate the internal consistency and reliability of the utilized scales—namely, the MBI, the EPQ, and the SCL-90—Cronbach’s alpha analysis was conducted [60]. Additionally, a Pearson correlation analysis was executed to examine the correlation matrix, encompassing age, personality traits, burnout, and psychopathology.
To evaluate the theoretical model, a moderated mediation approach was employed, wherein the relationship between critical care experience and burnout was mediated by three personality dimensions, while profession moderated this relationship (Figure 1). Model 76 of the PROCESS function for R, developed by Hayes [61], was utilized four times: once for each facet of burnout (i.e., emotional exhaustion, depersonalization, and personal achievement) [58] and once for the psychopathology, as indicated by the GSI [57]. This model was chosen for its robust capabilities in handling moderated mediation models [61].
Furthermore, we categorized critical care experience into three groups: less than 5 years, 5–10 years, and more than 10 years. Each group was compared to the preceding group using a sequential coding scheme [61]. This approach facilitated the comparison of successive levels of experience and enabled a nuanced exploration of the progressive nature of phenomena within the ICU setting. In both the moderation analysis of personality dimensions and the moderation analysis of burnout and psychopathology, main effects and interaction effects were examined. Bootstrap analysis was conducted to evaluate the indirect effects of the theoretical model. Unstandardized coefficients (B) and 95% confidence intervals were reported. Additionally, we reported the R2 for each model to assess the proportion of variance explained. Significant interaction effects were graphically illustrated. The statistical analysis was conducted under the guidance of a statistician to ensure accuracy and rigor in the interpretation of results.
A two-sided alpha level of 0.05 was set for determining statistical significance. All data were analyzed using the R (version 4.2.3) statistical language [62] equipped with the PROCESS function [61].
3. Results
3.1. Sample Demographics
Among the 503 respondents, nurses were notably younger (39.6 ± 7.8 vs. 45.7 ± 8.1, t (501) = 7.935, p < 0.001), more likely to be female (74.4% vs. 51.6%, c2(1) = 25.397, p < 0.001), and had less experience in the ICU environment compared to the intensivists (c2(2) = 20.579, p < 0.001).
3.2. Personality, Burnout, and Psychopathology Profiles
The psychometric scales used in this study demonstrated acceptable internal reliability, as evidenced by the examination of Cronbach’s alpha (a) coefficient (Table 1) [60]. The three personality traits were weakly correlated between them, confirming the assumed orthogonality [36,37]. Additionally, a notable positive correlation was reported between emotional exhaustion and depersonalization.

Table 1.
Correlation between personality traits and burnout facets of the examined sample.
Table 2 presents the descriptive statistics of personality traits, burnout scores, and psychopathology for the total sample as well as stratified by profession, sex, critical care experience, and urban size of ICU location.

Table 2.
Personality, burnout, and psychopathology of the examined sample.
As shown in Table 3, a total of 129 participants, 38 intensivists and 91 nurses, were classified as experiencing high emotional exhaustion. Additionally, 195 participants, 43 intensivists and 152 nurses, were identified as having low personal achievement. Furthermore, 188 participants, 59 intensivists and 129 nurses, were categorized as experiencing high levels of depersonalization (Table 3).

Table 3.
Concurrence among burnout facets of the examined sample.
The profession in the ICU was not related with the status of a high emotional exhaustion (c2(1) = 0.15, p = 0.699) and high depersonalization (c2(1) = 0.045, p = 0.831), while it was more probable for nurses to report a low personal achievement score (c2(1) = 11.473, p = 0.001). The GSI was significantly correlated with emotional exhaustion and depersonalization scores and exhibited a negative correlation with the personal achievement score. Specifically, the GSI was significantly higher among the respondents characterized as individuals experiencing high emotional exhaustion (1.37 vs. 0.72, t (501) = 9.508, p < 0.001) as well as among those characterized as individuals with high depersonalization (1.23 vs. 0.68, t (501) = 8.828, p < 0.001) or low personal achievement (1.05 vs. 0.79, t (501) = 4.098, p < 0.001).
3.3. Moderation Analysis of Personality Dimensions
The effect of demographics and the experience in the ICU environment on personality dimensions are presented in Table 4. Age was not found to have a significant effect on the three personality dimensions. Instead, a sex-based disparity was reported, with male healthcare professionals demonstrating markedly elevated levels of psychoticism compared to their female counterparts (M = 6.3 vs. M = 5.5, p < 0.001). A noteworthy main effect of profession on neuroticism emerged, indicating that nurses exhibited higher levels of neuroticism in comparison to intensivists (M = 11.1 vs. M = 9.9, p = 0.038).

Table 4.
Moderation analysis of personality dimensions of the examined sample.
Furthermore, our analysis showed some significant interaction effects (Table 2), which are further illustrated in Figure 2, Panel A–C. A noteworthy interaction between critical care experience and urban size of the ICU location concerning neuroticism was observed, suggesting that ICU personnel in minor cities tend to report higher levels of neuroticism across all experience levels than those in metropolitan cities, with the greatest difference seen in the group with more than 10 years of experience (Figure 2, Panel A). Additionally, the analysis revealed a significant interaction between critical care experience and profession regarding psychoticism and extraversion. Specifically, as experience in the ICU increases, nurses exhibited higher levels of psychoticism and lower levels of extraversion (Figure 2, Panel B,C).
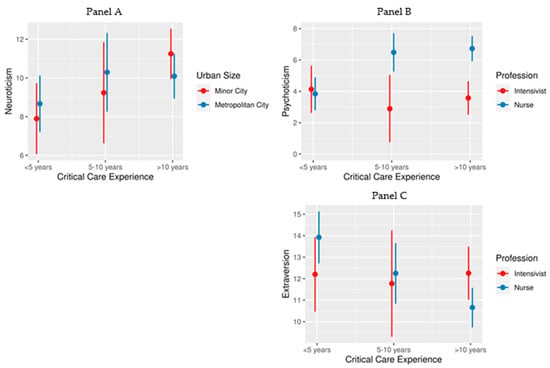
Figure 2.
Interaction effects of critical care experience, urban size of ICU location, and profession on the personality traits in the context of the examined model. Notes: The length of critical care experience was categorized into three groups: less than 5 years, 5–10 years, and more than 10 years. (Panel A) Differences in neuroticism were assessed across these groups by the urban size of ICU location categorized as ‘minor city’ and ‘metropolitan city’. Differences in psychoticism (Panel B) and extraversion (Panel C) were assessed across these groups by the profession categorized as ‘intensivist’ and ‘nurse’. Each dot represents the mean score for the respective group, while the error bars signify 95% confidence intervals.
3.4. Moderation Analysis of Burnout Facets and Psychopathology
The analysis uncovered notable associations between age and various dimensions of psychological well-being among the participants (Table 5). Specifically, a significant positive effect emerged between age and the likelihood of experiencing high emotional exhaustion (B = 0.037, p = 0.027), signifying a 1.4 times increase in the odds of high emotional exhaustion for each additional decade in the respondents’ age. Conversely, a negative relationship was identified between age and the likelihood of experiencing low personal accomplishment (B = −0.050, p = 0.004), suggesting a 0.6 times decrease in the odds of low personal accomplishment for each additional decade in the respondents’ age. Additionally, a noteworthy positive association was observed between age and the GSI (B = 0.009, p = 0.020), indicating a 0.09 increase in the GSI score for each additional decade in the respondents’ age. Furthermore, the personality trait of neuroticism (B = 0.082, p = 0.011) was identified as significant regressor of the GSI score, emphasizing its meaningful contribution to the overall psychological well-being of the participants (Table 5).

Table 5.
Moderation analysis of burnout and psychopathology of the examined sample.
Additionally, the analysis revealed significant interaction effects (Table 5) between psychoticism, critical care experience, profession, and the urban size of the ICU location, which are further illustrated in Figure 3, Panel A–D. Notably, with an increasing duration of critical care experience, nurses tended to report lower personal achievement scores, whereas intensivists showed an opposite trend (Figure 3, Panel A). Moreover, the relationship between psychoticism and psychopathology, as measured by the GSI, varied in strength depending on the urban size of the ICU location. Specifically, ICU personnel in larger metropolitan areas exhibited a more robust relationship between psychoticism and GSI scores than those in smaller urban settings (Figure 3, Panel B). Lastly, there was a significant association between psychoticism and both low personal achievement and high depersonalization scores. This relationship was particularly strong among intensivists when compared to nurses (Figure 3, Panel C,D).
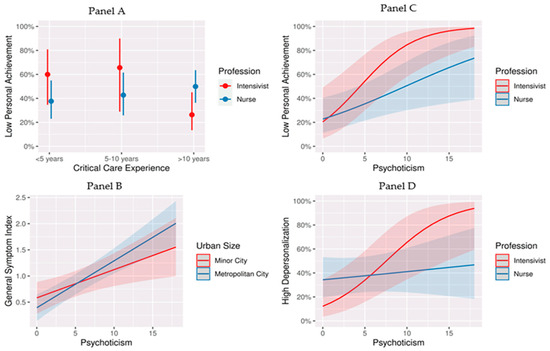
Figure 3.
Interaction effects of critical care experience, profession, and urban size of ICU location on the probability of burnout symptoms and psychopathology in the context of the examined model. Notes: (Panel A) The probability of low personal achievement across different levels of critical care experience for the two professions. Each dot represents the mean score for the respective group, while the error bars signify 95% confidence intervals. (Panel B) The psychopathology scores against levels of psychoticism for individuals in metropolitan versus minor cities. The shaded areas around the lines represent 95% confidence intervals, while the lines show that as psychoticism increased, so did the psychopathology score, with a stronger effect seen in metropolitan areas. (Panel C) The relationship between the personality trait of psychoticism and the probability of low personal achievement for intensivists and nurses. The shaded areas around the lines represent 95% confidence intervals. The upward trend for both lines suggests that as psychoticism increased, the likelihood of low personal achievement also increased, with a steeper slope for intensivists than for nurses. (Panel D) The probability of experiencing high depersonalization against the level of psychoticism for intensivists and nurses. The shaded areas around the lines represent 95% confidence intervals. The trend indicates that higher levels of psychoticism were associated with a higher probability of experiencing high depersonalization. The difference in slopes between the two professions suggests that the effect of psychoticism on depersonalization was more pronounced in intensivists.
3.5. Indirect Effects
In the context of the examined model, the bootstrap analysis showed that personality dimensions did not have a significant indirect effect on the relationship between critical care experience and both psychopathology and burnout.
4. Discussion
4.1. Personality Dimensions
The three personality traits exhibited weak correlations (Pearson’s r < 0.3), affirming the assumed orthogonality between psychoticism, extraversion, and neuroticism [36,37,63,64]. The observation that male healthcare professionals manifested notably elevated levels of psychoticism in comparison to their female counterparts substantiates the hypothesized association with psychoticism. In contrast, the inconclusive sex differences reported for extraversion align with analogous evidence in the literature [65,66], irrespective of the specific measurement instrument employed [36,67].
The extant literature lacks consensus regarding whether nurses lean towards extroversion or introversion, with several reports suggesting tendencies in either direction [44]. Particularly among ICU nurses, their personality traits were characterized by higher scores on dominance, rebelliousness, and self-sufficiency, coupled with lower scores on emotional sensitivity and imagination compared to nurses from other departments [68,69], predominantly indicative of elevated psychoticism. The observation that, with increasing experience in the ICU, nurses exhibit higher levels of psychoticism and diminished levels of extraversion further elucidates the reported relations. This suggests that in the high-pressure environment of an ICU, nurses may develop heightened psychoticism and reduced extraversion as adaptive coping mechanisms in response to stress and the demanding nature of their roles [70].
This phenomenon may be linked to challenges faced by nurses in establishing effective communication with patients who often experience objective communication difficulties [71,72] and frequently undergo negative emotional reactions such as frustration, stress, anxiety, and depression [73,74]. Given that effective human-level interaction forms the cornerstone of a positive working environment for nurses, it is plausible to posit that persistent challenges in communication may predispose nurses to heightened feelings of anxiety, depression, self-doubt, and other negative emotions, contributing to an elevated psychoticism score. In this context, previous assertions highlighting inferior personality factors linked to communication skills in ICU nurses compared to hospitalization unit nurses [75] should not be attributed to systematic personality variance among nurses. Instead, it is crucial to recognize that these disparities may originate from substantial barriers to effective communication [76].
Contrastingly, as experience in the ICU increases, intensivists experience heightened neuroticism, indicating an increased sense of responsibility and concern for patient outcomes. However, this also implies a higher emotional and psychosomatic toll in managing critically ill patients over time in the ICU. Given that elevated neuroticism is typically associated with an increased risk of mental illness [77] and, on average, poorer outcomes in terms of health and relationship satisfaction [78,79], a necessity emerges for a more palliative approach for long-term ICU doctors.
4.2. Burnout and Psychopathology
No overall significant differences were observed between nurses and intensivists regarding burnout status, aligning with prior research findings [80,81]. However, this stands in contrast to other studies [28,29]. This discrepancy in findings might be attributable to the specific samples and settings of the various studies. In relation to personal achievement, an inverse relationship between age and the likelihood of a low score status was identified, implying that with increasing age and experience, healthcare professionals acquire enhanced coping mechanisms for the emotional and physical stressors inherent in ICU settings [82]. However, an intriguing dynamic is suggested by the discovery that intensivists with lower ICU experience exhibit a higher probability of reporting low personal achievement compared to ICU nurses with equivalent experience. This pattern is reversed among intensivists and nurses with greater ICU experience. The origin of this phenomenon remains uncertain but may be attributed to distinct professional obligations in an ICU setting, with intensivists typically assuming more leadership and decision-making responsibilities than nurses [83]. Consequently, lower-experience intensivists may find these responsibilities overwhelming early in their careers, resulting in a sense of lower personal achievement. Nevertheless, with accumulated experience, they may become more adept at managing complex cases, leading to an improved sense of accomplishment. Conversely, experienced nurses may perceive stagnation in their careers, with limited opportunities for advancement, autonomy, or professional growth. The absence of well-defined career paths can foster a sense of being trapped in their current position, potentially leading to increased job stress and a diminished sense of accomplishment [84,85,86].
Interestingly, a positive correlation was found between age and personal achievement among ICU personnel, with increasing age associated with a lower likelihood of reporting low personal accomplishment. This trend suggests that with advancing age, there is a discernible decrease in reporting low levels of personal accomplishment, indicating that older ICU personnel may perceive their professional achievements more positively. This can largely be attributed to the cumulative effect of accrued experience over time in relation to job satisfaction [87], which ostensibly contributes to a more favorable self-assessment of accomplishments in the challenging ICU environment. Therefore, the career trajectory of healthcare professionals in such settings might be characterized by a gradual and steady increase in personal accomplishment, underpinned by the development of adaptive skills and psychological resilience.
In contrast, there was a significant negative correlation between age and emotional exhaustion and psychopathology, confirming a general trend towards an increased feeling of emotional exhaustion in older ICU personnel, as reported in various studies [88,89,90]. This finding is another manifestation of the mental burden derived from the recent health crisis, resulting in a significant psychological toll and high burnout rates in the global healthcare community [81,91,92], particularly among Greek healthcare professionals [93,94,95,96]. Accordingly, the commonly reported notion that accumulated work experience and resulting physical and mental fatigue contribute to a higher overall psychopathology is confirmed [92,97,98,99].
The adverse implications of high neuroticism or high psychoticism scores are further evident in their direct effects on the psychopathology, aligning with prior reports [77,100,101]. Additionally, the added effect of stressors related to urban living, such as long commutes and a high cost of living, is reflected in the stronger relationship of personality traits like psychoticism with general psychopathology symptoms. This amplification could be particularly pronounced in high-stress healthcare settings, where the additional urban stressors can intensify the psychological impact of already demanding jobs. Studies have shown that environmental factors like urban living conditions can significantly affect mental health, potentially exacerbating underlying personality traits [102,103]. Additionally, the role of organizational culture in hospitals, especially in metropolitan areas, is critical. A less supportive work environment and limited mental health resources can leave ICU personnel, particularly those with higher psychoticism scores, more vulnerable to psychological distress and less equipped to cope effectively. The importance of organizational support in mitigating the impact of stress on mental health has been emphasized in various studies [104,105,106,107].
Secondly, the personality dimension of psychoticism was highlighted as an important predictor of the probability of high depersonalization and low personal achievement scores, confirming previous reports [38,108]. Specifically, feelings within the psychotic spectrum, such as irritability and quick-tempered reactions, a tendency to be suspicious of others’ motives or actions, feelings of restlessness, and general inner tension are valid signs of less psychological resilience and are significantly associated with a higher likelihood of perceiving incompetence, unsuccessful outcomes in their work, and a cynical behavior toward colleagues and patients [109]. Further, the association between psychoticism and lower personal achievement and higher depersonalization may be more pronounced among intensivists due to the increased responsibility and decisional burden associated with their roles, documented to impact decreased job satisfaction and emotional and psychological burnout [110,111]. Specifically, psychoticism, with its resilience traits, might influence how intensivists cope with the emotional challenges, potentially exacerbating the negative outcomes observed. Furthermore, the hierarchical nature of healthcare settings, combined with the intense and challenging work environment of the ICU, may amplify the association between psychoticism and adverse outcomes among intensivists. Nurses, although impacted, might not experience the same level of intensity and pressure in their roles.
Finally, this study found that personality traits do not significantly influence the relationship between critical care experience, psychopathology, and burnout. Essentially, the direct effects of critical care experience on both psychopathology and burnout are substantial enough to explain their relationships without the need to consider personality traits as an explanatory factor. This suggests that the impact of critical care experience on psychopathology and burnout occurs independently of an individual’s personality traits.
5. Conclusions
This study explored the relationships between personality traits, burnout, and psychopathology among ICU personnel, considering the moderating effect of experience and workplace setting. Among ICU nurses, increasing experience was correlated with higher psychoticism and lower extraversion, potentially as a coping mechanism for communication difficulties. Intensivists with lower ICU experience reported higher burnout. Psychoticism and neuroticism had direct effects on psychopathology, with stronger relations in metropolitan areas. Psychoticism predicted high depersonalization and low personal achievement, particularly among intensivists, indicating potential implications for coping with emotional challenges and adverse outcomes in high-pressure healthcare settings.
The findings underscore the need for a holistic understanding of the psychosocial dynamics within ICU settings, acknowledging the impact of communication challenges and the evolving responsibilities of healthcare roles. It is important to note that the repercussions of high levels of burnout and psychopathology among ICU personnel are significant, impacting both the healthcare professionals themselves [3,6,112] and the quality of patient care [113]. Research indicates that healthcare personnel experiencing burnout are associated with adverse patient outcomes. This includes diminished patient safety [114,115], increased standardized mortality ratios, and prolonged hospitalization durations [116]. Additionally, there is a correlation between healthcare worker burnout and reduced patient satisfaction [117] as well as an increased incidence of medical errors and malpractice [14,15,113].
Our study, therefore, lays a foundation for future explorations into strategic interventions aimed at establishing specialized training programs and robust support frameworks within the ICU. These programs and support systems are envisioned to offer both emotional and professional assistance to ICU personnel, thereby enhancing their ability to effectively manage the intense stress characteristic of the ICU and urban environment. Such proactive measures are crucial for maintaining the mental well-being and professional efficacy of ICU personnel.
Limitations
It is imperative to acknowledge certain limitations in the interpretation and generalization of this study’s findings. Primarily, our results are based on a sample of ICU personnel from Greece, limiting generalizability beyond populations with similar cultural backgrounds, such as Mediterranean countries, cautioning against universal application to regions with distinct social structures. To enhance generalizability, future studies should include ICU personnel from various regions and cultural backgrounds. Conducting longitudinal research, as opposed to the cross-sectional approach used in this study, could offer insights into how these relationships evolve over time, particularly how personality traits interact with burnout and psychopathology in the long run. Additionally, comparing ICU personnel in urban versus rural settings, or in different healthcare systems, might reveal how environmental and systemic factors influence these relationships.
Secondly, the moderated mediation model employed in this research focused on the relationship between critical care experience, personality traits, burnout, and psychopathology. As such, the results are constrained by the specific pathways and variables within this model. While our study provides valuable insights into these particular associations, it does not capture the entirety of the complex interactions between personality dimensions and psychopathology. Other unexplored variables and pathways may exist, and the extent to which our findings can be extrapolated to a broader context may be limited. Exploring factors such as workplace environment, support systems, and personal life stressors could provide a more comprehensive understanding of the dynamics at play. Therefore, future research should consider additional factors and pathways to gain a more comprehensive understanding of the complex relationship between personality traits, burnout, and psychopathology in the context of ICU personnel. Finally, qualitative studies, such as interviews or focus groups, could provide deeper insights into the personal experiences and perspectives of ICU personnel, which might be missed in quantitative models.
Author Contributions
Conceptualization, V.K., M.G. and V.P.; methodology, V.K., G.P. and M.G.; software, M.G., D.T. and E.D.; validation, V.K., G.P. and D.T.; investigation, V.P.; writing—original draft preparation, V.P., D.T. and E.D.; writing—review and editing, V.K., G.P. and M.G.; visualization, M.G. and E.D.; supervision, V.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University Hospital of Ioannina (protocol code 3263, 1 February 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Freudenberger, H.J. Staff Burn-Out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory. In Evaluating Stress: A Book of Resources, 3rd ed.; Scarecrow Education: Lanham, MD, USA, 1997; pp. 191–218. [Google Scholar]
- Grossi, G.; Perski, A.; Osika, W.; Savic, I. Stress-related exhaustion disorder--clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand. J. Psychol. 2015, 56, 626–636. [Google Scholar] [CrossRef]
- Kelly, L.A.; Gee, P.M.; Butler, R.J. Impact of nurse burnout on organizational and position turnover. Nurs. Outlook 2021, 69, 96–102. [Google Scholar] [CrossRef]
- Khatatbeh, H.; Pakai, A.; Al-Dwaikat, T.; Onchonga, D.; Amer, F.; Prémusz, V.; Oláh, A. Nurses’ burnout and quality of life: A systematic review and critical analysis of measures used. Nurs. Open 2022, 9, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Bragard, I.; Dupuis, G.; Fleet, R. Quality of work life, burnout, and stress in emergency department physicians: A qualitative review. Eur. J. Emerg. Med. 2015, 22, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Sanfilippo, F.; Palumbo, G.J.; Noto, A.; Pennisi, S.; Mineri, M.; Vasile, F.; Dezio, V.; Busalacchi, D.; Murabito, P.; Astuto, M. Prevalence of burnout among intensive care physicians: A systematic review. Rev. Bras. Ter. Intensiv. 2020, 32, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef]
- O’Connor, K.; Muller Neff, D.; Pitman, S. Burnout in mental health professionals: A systematic review and meta-analysis of prevalence and determinants. Eur. Psychiatry 2018, 53, 74–99. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, R.; Christensen, A.E.; Pristed, S.G.; Jepsen, I.; Telléus, G.K. Burnout in Mental Health Care Professionals Working with Inpatients in Open or Closed Wards in Psychiatric Hospitals. Issues Ment. Health Nurs. 2021, 42, 1030–1037. [Google Scholar] [CrossRef]
- Chuang, C.H.; Tseng, P.C.; Lin, C.Y.; Lin, K.H.; Chen, Y.Y. Burnout in the intensive care unit professionals: A systematic review. Medicine 2016, 95, e5629. [Google Scholar] [CrossRef]
- Fahrenkopf, A.M.; Sectish, T.C.; Barger, L.K.; Sharek, P.J.; Lewin, D.; Chiang, V.W.; Edwards, S.; Wiedermann, B.L.; Landrigan, C.P. Rates of medication errors among depressed and burnt out residents: Prospective cohort study. BMJ 2008, 336, 488–491. [Google Scholar] [CrossRef]
- Tawfik, D.S.; Profit, J.; Morgenthaler, T.I.; Satele, D.V.; Sinsky, C.A.; Dyrbye, L.N.; Tutty, M.A.; West, C.P.; Shanafelt, T.D. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin. Proc. 2018, 93, 1571–1580. [Google Scholar] [CrossRef]
- Dewa, C.S.; Loong, D.; Bonato, S.; Thanh, N.X.; Jacobs, P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv. Res. 2014, 14, 325. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Massie, F.S., Jr.; Eacker, A.; Harper, W.; Power, D.; Durning, S.J.; Thomas, M.R.; Moutier, C.; Satele, D.; Sloan, J.; et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA 2010, 304, 1173–1180. [Google Scholar] [CrossRef] [PubMed]
- Rathert, C.; Williams, E.S.; Linhart, H. Evidence for the Quadruple Aim: A Systematic Review of the Literature on Physician Burnout and Patient Outcomes. Med. Care 2018, 56, 976–984. [Google Scholar] [CrossRef] [PubMed]
- Devi, S. Doctors in distress. Lancet 2011, 377, 454–455. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.S.; Skinner, A.C. Outcomes of physician job satisfaction: A narrative review, implications, and directions for future research. Health Care Manag. Rev. 2003, 28, 119–139. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Flannery, R.B., Jr.; Farley, E.; Tierney, T.; Walker, A.P. Characteristics of assaultive psychiatric patients: 20-year analysis of the Assaultive Staff Action Program (ASAP). Psychiatr. Q. 2011, 82, 1–10. [Google Scholar] [CrossRef]
- Mento, C.; Silvestri, M.C.; Bruno, A.; Muscatello, M.R.A.; Cedro, C.; Pandolfo, G.; Zoccali, R.A. Workplace violence against healthcare professionals: A systematic review. Aggress. Violent Behav. 2020, 51, 101381. [Google Scholar] [CrossRef]
- Mele, F.; Buongiorno, L.; Montalbò, D.; Ferorelli, D.; Solarino, B.; Zotti, F.; Carabellese, F.F.; Catanesi, R.; Bertolino, A.; Dell’Erba, A.; et al. Reporting Incidents in the Psychiatric Intensive Care Unit: A Retrospective Study in an Italian University Hospital. J. Nerv. Ment. Dis. 2022, 210, 622–628. [Google Scholar] [CrossRef]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Kimo Takayesu, J.; Ramoska, E.A.; Clark, T.R.; Hansoti, B.; Dougherty, J.; Freeman, W.; Weaver, K.R.; Chang, Y.; Gross, E. Factors associated with burnout during emergency medicine residency. Acad. Emerg. Med. 2014, 21, 1031–1035. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef] [PubMed]
- Dulko, D.; Zangaro, G.A. Comparison of Factors Associated with Physician and Nurse Burnout. Nurs. Clin. N. Am. 2022, 57, 53–66. [Google Scholar] [CrossRef]
- Ntantana, A.; Matamis, D.; Savvidou, S.; Marmanidou, K.; Giannakou, M.; Gouva, Μ.; Nakos, G.; Koulouras, V. The impact of healthcare professionals’ personality and religious beliefs on the decisions to forego life sustaining treatments: An observational, multicentre, cross-sectional study in Greek intensive care units. BMJ Open 2017, 7, e013916. [Google Scholar] [CrossRef]
- Sikioti, T.; Zartaloudi, A.; Pappa, D.; Mangoulia, P.; Fradelos, E.C.; Kourti, F.E.; Koutelekos, I.; Dousis, E.; Margari, N.; Stavropoulou, A.; et al. Stress and burnout among Greek critical care nurses during the COVID-19 pandemic. AIMS Public Health 2023, 10, 755–774. [Google Scholar] [CrossRef] [PubMed]
- van Mol, M.M.; Kompanje, E.J.; Benoit, D.D.; Bakker, J.; Nijkamp, M.D. The Prevalence of Compassion Fatigue and Burnout among Healthcare Professionals in Intensive Care Units: A Systematic Review. PLoS ONE 2015, 10, e0136955. [Google Scholar] [CrossRef]
- McManus, I.C.; Keeling, A.; Paice, E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: A twelve year longitudinal study of UK medical graduates. BMC Med. 2004, 2, 29. [Google Scholar] [CrossRef]
- Eysenck, H. Personality Psychology in Europe: Theoretical and Empirical Developments; Bonarius, H., Van Heck, G., Smid, N., Eds.; Swets & Zeitlinger: Lisse, The Netherlands, 1984. [Google Scholar]
- Maher, B.A.; Maher, W.B. Personality and psychopathology: A historical perspective. J. Abnorm. Psychol. 1994, 103, 72–77. [Google Scholar] [CrossRef]
- Eysenck, H.J.; Eysenck, S.B.G. Manual of the Eysenck Personality Questionnaire: (EPQ-R Adult); EdITS/Educational and Industrial Testing Service San Diego, Calif.: San Diego, CA, USA, 1994. [Google Scholar]
- Eysenck, H.J.; Eysenck, M.W. Personality and Individual Differences: A Natural Science Approach; Eysenck, H.J., Eysenck, M.W., Eds.; Plenum Press: New York, NY, USA, 1985. [Google Scholar]
- Eysenck, H.J.; Eysenck, S.B.G. The Orthogonality of Psychoticism and Neuroticism: A Factorial Study. Percept. Mot. Ski. 1971, 33, 461–462. [Google Scholar] [CrossRef]
- Angelini, G. Big five model personality traits and job burnout: A systematic literature review. BMC Psychol. 2023, 11, 49. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.A.; Slater, M.; Lofters, A. Personality and burnout among primary care physicians: An international study. Psychol. Res. Behav. Manag. 2019, 12, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Divinakumar, K.J.; Bhat, P.S.; Prakash, J.; Srivastava, K. Personality traits and its correlation to burnout in female nurses. Ind. Psychiatry J. 2019, 28, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Grigorescu, S.; Cazan, A.M.; Grigorescu, O.D.; Rogozea, L.M. The role of the personality traits and work characteristics in the prediction of the burnout syndrome among nurses—A new approach within predictive, preventive, and personalized medicine concept. EPMA J. 2018, 9, 355–365. [Google Scholar] [CrossRef]
- Narang, G.; Wymer, K.; Mi, L.; Wolter, C.; Humphreys, M.; Stern, K. Personality Traits and Burnout: A Survey of Practicing US Urologists. Urology 2022, 167, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Prins, D.J.; van Vendeloo, S.N.; Brand, P.L.P.; Van der Velpen, I.; de Jong, K.; van den Heijkant, F.; Van der Heijden, F.; Prins, J.T. The relationship between burnout, personality traits, and medical specialty. A national study among Dutch residents. Med. Teach. 2019, 41, 584–590. [Google Scholar] [CrossRef]
- Louwen, C.; Reidlinger, D.; Milne, N. Profiling health professionals’ personality traits, behaviour styles and emotional intelligence: A systematic review. BMC Med. Educ. 2023, 23, 120. [Google Scholar] [CrossRef]
- Atherton, O.E.; Willroth, E.C.; Graham, E.K.; Luo, J.; Mroczek, D.K.; Lewis-Thames, M.W. Rural-urban differences in personality traits and well-being in adulthood. J. Pers. 2024, 92, 73–87. [Google Scholar] [CrossRef]
- Weidmann, R.; Chopik, W.J. Explicating narrow and broad conceptualizations of environmental influences on personality. J. Pers. 2024, 92, 5–15. [Google Scholar] [CrossRef]
- Probst, J.C.; Laditka, S.B.; Moore, C.G.; Harun, N.; Powell, M.P.; Baxley, E.G. Rural-urban differences in depression prevalence: Implications for family medicine. Fam. Med. 2006, 38, 653–660. [Google Scholar]
- van den Bosch, M.; Meyer-Lindenberg, A. Environmental Exposures and Depression: Biological Mechanisms and Epidemiological Evidence. Annu. Rev. Public Health 2019, 40, 239–259. [Google Scholar] [CrossRef]
- van Os, J.; Kenis, G.; Rutten, B.P. The environment and schizophrenia. Nature 2010, 468, 203–212. [Google Scholar] [CrossRef]
- Szyszkowicz, M.; Rowe, B.H.; Colman, I. Air pollution and daily emergency department visits for depression. Int. J. Occup. Med. Environ. Health 2009, 22, 355–362. [Google Scholar] [CrossRef]
- Power, M.C.; Kioumourtzoglou, M.A.; Hart, J.E.; Okereke, O.I.; Laden, F.; Weisskopf, M.G. The relation between past exposure to fine particulate air pollution and prevalent anxiety: Observational cohort study. BMJ 2015, 350, h1111. [Google Scholar] [CrossRef] [PubMed]
- Newbury, J.B.; Arseneault, L.; Beevers, S.; Kitwiroon, N.; Roberts, S.; Pariante, C.M.; Kelly, F.J.; Fisher, H.L. Association of Air Pollution Exposure With Psychotic Experiences During Adolescence. JAMA Psychiatry 2019, 76, 614–623. [Google Scholar] [CrossRef] [PubMed]
- EEA-JRC. Environment and Human Health: Joint EEA-JRC Report; EUR-OP: Luxembourg, 2013. [Google Scholar]
- iMEdDLAB. Beds and Nursing Staff per COVID ICU. 2021. Available online: https://lab.imedd.org/ypostelexosi-meth-covid-thnitotita-plirotita-esy (accessed on 14 January 2024).
- Anagnostopoulos, F.; Papadatou, D. Factorial composition and internal consistency of the Greek version of the Maslach Burnout Inventory. Psychol. Them. 1992, 5, 183–202. [Google Scholar]
- Dimitriou, E. EPQ personality questionnaire. Greek validation in the Greek population. Engefalos 1986, 23, 41–54. [Google Scholar]
- Donias, S.; Karastergiou, A.; Manos, N. Standardization of the symptom checklist-90-R rating scale in a Greek population. Psychiatriki 1991, 2, 42–48. [Google Scholar]
- Zis, P.; Anagnostopoulos, F.; Sykioti, P. Burnout in medical residents: A study based on the job demands-resources model. Sci. World J. 2014, 2014, 673279. [Google Scholar] [CrossRef]
- Derogatis, L.R. SCL 90 R Administration, Scoring and Procedures Manual II for the Revised Version and Other Instruments of the Psychopathology Rating Scale Series; Clinical Psychometric Research: Towson, MD, USA, 1986. [Google Scholar]
- Cronbach, L.J.; Meehl, P.E. Construct validity in psychological tests. Psychol. Bull. 1955, 52, 281–302. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach (Methodology in the Social Sciences), 2nd ed.; The Guilford Press New York: New York, NY, USA, 2018. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: www.R-project.org (accessed on 14 January 2024).
- Aluja, A.; García, Ó.; García, L.F. A psychometric analysis of the revised Eysenck Personality Questionnaire short scale. Personal. Individ. Differ. 2003, 35, 449–460. [Google Scholar] [CrossRef]
- Lewis, C.A.; Francis, L.J.; Shevlin, M.; Forrest, S. Confirmatory factor analysis of the French translation of the abbreviated form of the revised Eysenck Personality Questionnaire (EPQR-A). Eur. J. Psychol. Assess. 2002, 18, 179–185. [Google Scholar] [CrossRef]
- Escorial, S.; Navas, M.J. Analysis of the Gender Variable in the Eysenck Personality Questionnaire–Revised Scales Using Differential Item Functioning Techniques. Educ. Psychol. Meas. 2007, 67, 990–1001. [Google Scholar] [CrossRef]
- Forrest, S.; Lewis, C.A.; Shevlin, M. Examining the factor structure and differential functioning of the Eysenck personality questionnaire revised–abbreviated. Personal. Individ. Differ. 2000, 29, 579–588. [Google Scholar] [CrossRef]
- Costa, P.T.; McCrae, R.R. Four ways five factors are basic. Personal. Individ. Differ. 1992, 13, 653–665. [Google Scholar] [CrossRef]
- Kennedy, B.; Curtis, K.; Waters, D. Is there a relationship between personality and choice of nursing specialty: An integrative literature review. BMC Nurs. 2014, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Levine, C.D.; Wilson, S.F.; Guido, G.W. Personality factors of critical care nurses. Heart Lung 1988, 17, 392–398. [Google Scholar] [PubMed]
- Scheepers, F.E.; de Mul, J.; Boer, F.; Hoogendijk, W.J. Psychosis as an Evolutionary Adaptive Mechanism to Changing Environments. Front. Psychiatry 2018, 9, 237. [Google Scholar] [CrossRef]
- Nyhagen, R.; Egerod, I.; Rustøen, T.; Lerdal, A.; Kirkevold, M. Unidentified communication challenges in the intensive care unit: A qualitative study using multiple triangulations. Aust. Crit. Care 2023, 36, 215–222. [Google Scholar] [CrossRef]
- Ten Hoorn, S.; Elbers, P.W.; Girbes, A.R.; Tuinman, P.R. Communicating with conscious and mechanically ventilated critically ill patients: A systematic review. Crit. Care 2016, 20, 333. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, M.; Poulsen, I. Patients’ experiences of being mechanically ventilated in an ICU: A qualitative metasynthesis. Scand. J. Caring Sci. 2015, 29, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, V.; Lindahl, B.; Bergbom, I. Patients’ statements and experiences concerning receiving mechanical ventilation: A prospective video-recorded study. Nurs. Inq. 2012, 19, 247–258. [Google Scholar] [CrossRef]
- Ayuso-Murillo, D.; Colomer-Sánchez, A.; Herrera-Peco, I. Communication skills in ICU and adult hospitalisation unit nursing staff. Enferm. Intensiv. 2017, 28, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.; Mannix, T.; Harrington, A. Nurses’ communication with families in the intensive care unit–a literature review. Nurs. Crit. Care 2017, 22, 70–80. [Google Scholar] [CrossRef]
- Ormel, J.; Jeronimus, B.F.; Kotov, R.; Riese, H.; Bos, E.H.; Hankin, B.; Rosmalen, J.G.M.; Oldehinkel, A.J. Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clin. Psychol. Rev. 2013, 33, 686–697. [Google Scholar] [CrossRef] [PubMed]
- Li, W.W.; Xie, G. Personality and job satisfaction among Chinese health practitioners: The mediating role of professional quality of life. Health Psychol. Open 2020, 7, 2055102920965053. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Zhang, F.; Tang, X.; Wang, L.; Zan, J.; Zhu, Y.; Feng, D. Do type A personality and neuroticism moderate the relationships of occupational stressors, job satisfaction and burnout among Chinese older nurses? A cross-sectional survey. BMC Nurs. 2022, 21, 88. [Google Scholar] [CrossRef]
- Myhren, H.; Ekeberg, O.; Stokland, O. Job Satisfaction and Burnout among Intensive Care Unit Nurses and Physicians. Crit. Care Res. Pract. 2013, 2013, 786176. [Google Scholar] [CrossRef] [PubMed]
- Papazian, L.; Hraiech, S.; Loundou, A.; Herridge, M.S.; Boyer, L. High-level burnout in physicians and nurses working in adult ICUs: A systematic review and meta-analysis. Intensive Care Med. 2023, 49, 387–400. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Elvira, S.; Romero-Béjar, J.L.; Suleiman-Martos, N.; Gómez-Urquiza, J.L.; Monsalve-Reyes, C.; Cañadas-De la Fuente, G.A.; Albendín-García, L. Prevalence, Risk Factors and Burnout Levels in Intensive Care Unit Nurses: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11432. [Google Scholar] [CrossRef] [PubMed]
- Leiter, M.P.; Spence Laschinger, H.K. Relationships of work and practice environment to professional burnout: Testing a causal model. Nurs. Res. 2006, 55, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Asl, R.G.; Taghinejad, R.; Parizad, N.; Jasemi, M. The Relationship Between Professional Autonomy and Job Stress Among Intensive Care Unit Nurses: A Descriptive Correlational Study. Iran. J. Nurs. Midwifery Res. 2022, 27, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Bégat, I.; Ellefsen, B.; Severinsson, E. Nurses’ satisfaction with their work environment and the outcomes of clinical nursing supervision on nurses’ experiences of well-being—A Norwegian study. J. Nurs. Manag. 2005, 13, 221–230. [Google Scholar] [CrossRef]
- Krukowska-Sitek, H.; Krupa, S.; Grad, I. The Impact of the COVID-19 Pandemic on the Professional Autonomy of Anesthesiological Nurses and Trust in the Therapeutic Team of Intensive Therapy Units-Polish Multicentre Study. Int. J. Environ. Res. Public Health 2022, 19, 12755. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-García, C.; Solano-Ruíz Mdel, C.; Martínez-Roche, M.E.; Gómez-García, C.I. Job satisfaction among health care workers: The role of gender and age. Rev. Lat. Am. Enferm. 2013, 21, 1314–1320. [Google Scholar] [CrossRef]
- Padilla Fortunatti, C.; Palmeiro-Silva, Y.K. Effort-Reward Imbalance and Burnout Among ICU Nursing Staff: A Cross-Sectional Study. Nurs. Res. 2017, 66, 410–416. [Google Scholar] [CrossRef]
- Poncet, M.C.; Toullic, P.; Papazian, L.; Kentish-Barnes, N.; Timsit, J.F.; Pochard, F.; Chevret, S.; Schlemmer, B.; Azoulay, E. Burnout syndrome in critical care nursing staff. Am. J. Respir. Crit. Care Med. 2007, 175, 698–704. [Google Scholar] [CrossRef]
- Kashtanov, A.; Molotok, E.; Yavorovskiy, A.; Boyarkov, A.; Vasil’ev, Y.; Alsaegh, A.; Dydykin, S.; Kytko, O.; Meylanova, R.; Enina, Y.; et al. A Comparative Cross-Sectional Study Assessing the Psycho-Emotional State of Intensive Care Units’ Physicians and Nurses of COVID-19 Hospitals of a Russian Metropolis. Int. J. Environ. Res. Public Health 2022, 19, 1828. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.E.; Milward, J.; Spoiala, C.; Bhogal, J.K.; Weston, D.; Potts, H.W.W.; Caulfield, T.; Toolan, M.; Kanga, K.; El-Sheikha, S.; et al. The mental health of staff working on intensive care units over the COVID-19 winter surge of 2020 in England: A cross sectional survey. Br. J. Anaesth. 2022, 128, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Dragioti, E.; Tsartsalis, D.; Mentis, M.; Mantzoukas, S.; Gouva, M. Impact of the COVID-19 pandemic on the mental health of hospital staff: An umbrella review of 44 meta-analyses. Int. J. Nurs. Stud. 2022, 131, 104272. [Google Scholar] [CrossRef] [PubMed]
- Aslanidis, V.; Tsolaki, V.; Papadonta, M.E.; Amanatidis, T.; Parisi, K.; Makris, D.; Zakynthinos, E. The Impact of the COVID-19 Pandemic on Mental Health and Quality of Life in COVID-19 Department Healthcare Workers in Central Greece. J. Pers. Med. 2023, 13, 250. [Google Scholar] [CrossRef]
- Blekas, A.; Voitsidis, P.; Athanasiadou, M.; Parlapani, E.; Chatzigeorgiou, A.F.; Skoupra, M.; Syngelakis, M.; Holeva, V.; Diakogiannis, I. COVID-19: PTSD symptoms in Greek health care professionals. Psychol. Trauma. 2020, 12, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Mavrovounis, G.; Mavrovouni, D.; Mermiri, M.; Papadaki, P.; Chalkias, A.; Zarogiannis, S.; Christodoulou, N.; Gourgoulianis, K.; Pantazopoulos, I. Watch Out for Burnout in COVID-19: A Greek Health Care Personnel Study. Inquiry 2022, 59, 469580221097829. [Google Scholar] [CrossRef]
- Milas, G.P.; Issaris, V.; Zareifopoulos, N. Burnout for medical professionals during the COVID-19 pandemic in Greece; the role of primary care. Hosp Pr. 2022, 50, 102–103. [Google Scholar] [CrossRef] [PubMed]
- Benincasa, V.; Passannante, M.; Perrini, F.; Carpinelli, L.; Moccia, G.; Marinaci, T.; Capunzo, M.; Pironti, C.; Genovese, A.; Savarese, G.; et al. Burnout and Psychological Vulnerability in First Responders: Monitoring Depersonalization and Phobic Anxiety during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2794. [Google Scholar] [CrossRef]
- Hou, J.; Xu, B.; Zhang, J.; Luo, L.; Pen, X.; Chen, S.; Ma, G.; Hu, Z.; Kong, X. Psychological Status and Job Burnout of Nurses Working in the Frontline of the Novel Coronavirus in China During the Delta Variant Outbreak: A Cross-Sectional Survey. Psychol. Res. Behav. Manag. 2022, 15, 533–546. [Google Scholar] [CrossRef]
- Rössler, W.; Hengartner, M.P.; Ajdacic-Gross, V.; Angst, J. Predictors of burnout: Results from a prospective community study. Eur. Arch. Psychiatry Clin. Neurosci. 2015, 265, 19–25. [Google Scholar] [CrossRef]
- Saulsman, L.M.; Page, A.C. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clin. Psychol. Rev. 2004, 23, 1055–1085. [Google Scholar] [CrossRef] [PubMed]
- Strickhouser, J.E.; Zell, E.; Krizan, Z. Does personality predict health and well-being? A metasynthesis. Health Psychol. 2017, 36, 797–810. [Google Scholar] [CrossRef] [PubMed]
- Lederbogen, F.; Kirsch, P.; Haddad, L.; Streit, F.; Tost, H.; Schuch, P.; Wüst, S.; Pruessner, J.C.; Rietschel, M.; Deuschle, M.; et al. City living and urban upbringing affect neural social stress processing in humans. Nature 2011, 474, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Peen, J.; Schoevers, R.A.; Beekman, A.T.; Dekker, J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 2010, 121, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Erwin, P.J.; Shanafelt, T.D. Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet 2016, 388, 2272–2281. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Sinsky, C.; Trockel, M.; Tutty, M.; Nedelec, L.; Carlasare, L.E.; Shanafelt, T.D. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw. Open 2020, 3, e209385. [Google Scholar] [CrossRef]
- West, C.P.; Shanafelt, T.D.; Kolars, J.C. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA 2011, 306, 952–960. [Google Scholar] [CrossRef]
- Xing, J.; Sun, N.; Xu, J.; Geng, S.; Li, Y. Study of the mental health status of medical personnel dealing with new coronavirus pneumonia. PLoS ONE 2020, 15, e0233145. [Google Scholar] [CrossRef]
- Pachi, A.; Kavourgia, E.; Bratis, D.; Fytsilis, K.; Papageorgiou, S.M.; Lekka, D.; Sikaras, C.; Tselebis, A. Anger and Aggression in Relation to Psychological Resilience and Alcohol Abuse among Health Professionals during the First Pandemic Wave. Healthcare 2023, 11, 2031. [Google Scholar] [CrossRef]
- Flannery, L.; Ramjan, L.M.; Peters, K. End-of-life decisions in the Intensive Care Unit (ICU)—Exploring the experiences of ICU nurses and doctors—A critical literature review. Aust. Crit. Care 2016, 29, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Van den Bulcke, B.; Metaxa, V.; Reyners, A.K.; Rusinova, K.; Jensen, H.I.; Malmgren, J.; Darmon, M.; Talmor, D.; Meert, A.P.; Cancelliere, L.; et al. Ethical climate and intention to leave among critical care clinicians: An observational study in 68 intensive care units across Europe and the United States. Intensive Care Med. 2020, 46, 46–56. [Google Scholar] [CrossRef]
- Moss, M.; Good, V.S.; Gozal, D.; Kleinpell, R.; Sessler, C.N. An Official Critical Care Societies Collaborative Statement-Burnout Syndrome in Critical Care Health-care Professionals: A Call for Action. Chest 2016, 150, 17–26. [Google Scholar] [CrossRef] [PubMed]
- De Hert, S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local. Reg. Anesth. 2020, 13, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Garcia, C.L.; Abreu, L.C.; Ramos, J.L.S.; Castro, C.F.D.; Smiderle, F.R.N.; Santos, J.A.D.; Bezerra, I.M.P. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina 2019, 55, 553. [Google Scholar] [CrossRef]
- Ryu, I.S.; Shim, J. The Influence of Burnout on Patient Safety Management Activities of Shift Nurses: The Mediating Effect of Compassion Satisfaction. Int. J. Environ. Res. Public Health 2021, 18, 12210. [Google Scholar] [CrossRef]
- Welp, A.; Meier, L.L.; Manser, T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Front. Psychol. 2014, 5, 1573. [Google Scholar] [CrossRef]
- Haas, J.S.; Cook, E.F.; Puopolo, A.L.; Burstin, H.R.; Cleary, P.D.; Brennan, T.A. Is the professional satisfaction of general internists associated with patient satisfaction? J. Gen. Intern. Med. 2000, 15, 122–128. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).