Inguinoscrotal Hernia, a Possible Cause of Rapidly Developing Fetal Scrotal Mass: Case Report and Literature Update
Abstract
1. Introduction
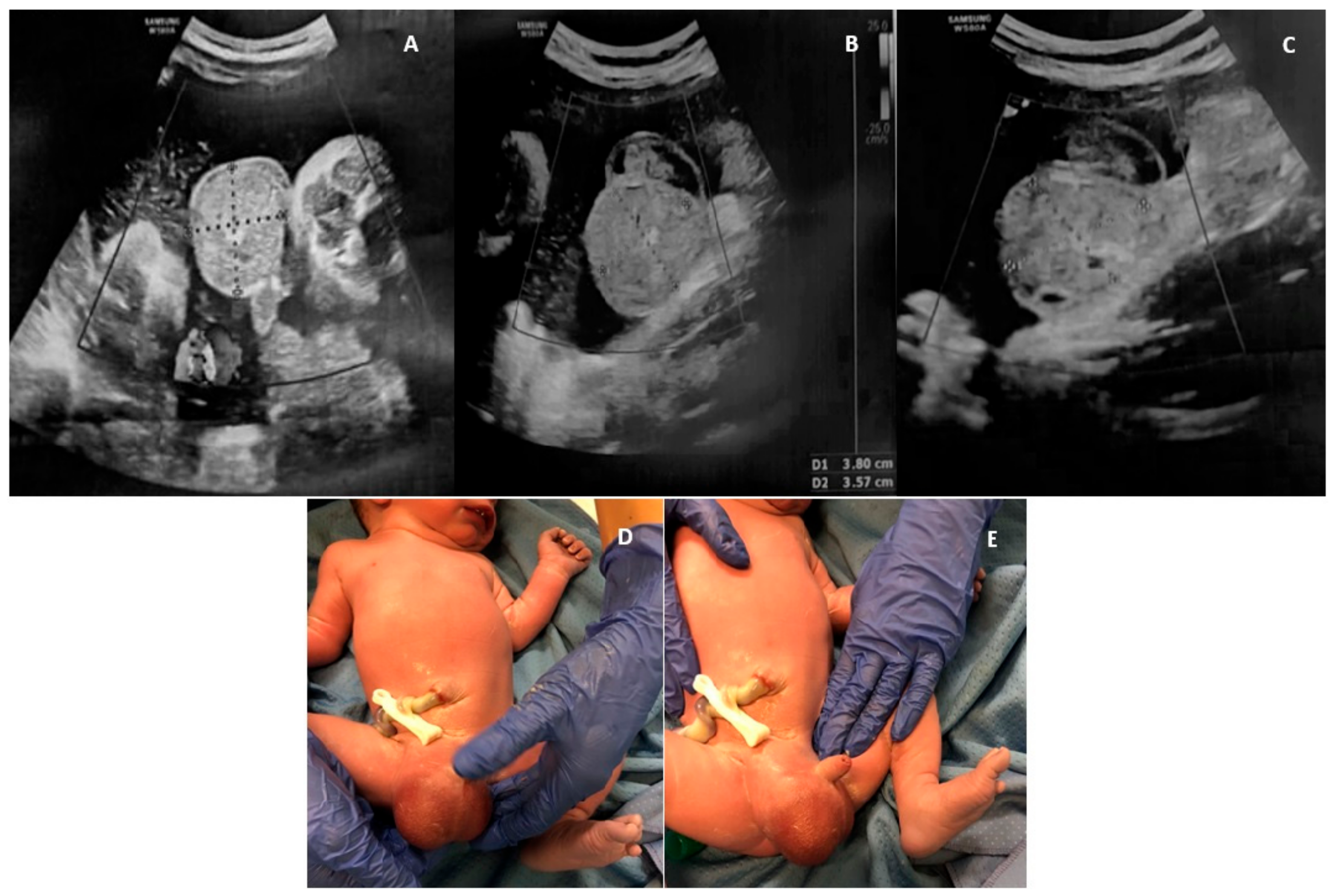
2. Case Report
3. Methods
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grosfelf, J. Current concept in inguinal hernia in infants and children. World J. Surg. 1989, 13, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Galifer, R.B.; Bosc, O. Les anomalies congénitales du canal péritonéo-vaginal [Congenital abnormalities of the peritoneo-vaginal process]. Pediatrie 1987, 42, 103–109. [Google Scholar]
- Chen, L.; Wang, J.; Yue, Q.; Wen, H. Two cases of fetal inguinoscrotal hernia and review of the literature. Niger. J. Clin. Pract. 2022, 25, 2062–2066. [Google Scholar] [PubMed]
- Kithir Mohamed, A.S. Foetal inguinoscrotal hernia-its prenatal diagnosis and its spontaneous regression. BJR Case Rep. 2016, 2, 20150277. [Google Scholar] [CrossRef] [PubMed]
- Ronzoni, S.; Melamed, N.; Kingdom, J.C.; Ryan, G.; Jaeggi, E.; Windrim, R.C. Prenatal diagnosis of inguinoscrotal hernia associated with bowel dilatation: A pathogenetic hypothesis. Prenat. Diagn. 2015, 35, 1151–1153. [Google Scholar] [CrossRef]
- Basaran, A.; Deren, O.; Onderoglu, L.S. Prenatal diagnosis of Jarcho-Levin syndrome in combination with inguinoscrotal hernia. Am. J. Perinatol. 2010, 27, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Frati, A.; Ducarme, G.; Vuillard, E.; Pecastaing, A.; Yver, C.; Pejoan, H.; Luton, D. Prenatal evaluation of a scrotal mass using a high-frequency probe in the diagnosis of inguinoscrotal hernia. Ultrasound Obstetr. Gynecol. 2008, 32, 949–950. [Google Scholar] [CrossRef]
- Caserta, L.; Giorlandino, M.; Tiezzi, A.; Giorlandino, C.; Cignini, P. Atypical presentation of fetal inguino-scrotal hernia at 21 weeks of gestation: A case report. J. Prenat. Med. 2007, 1, 35–36. [Google Scholar]
- Allen, L.M.; Nosovitch, J.T.; Silverman, R.K., Jr.; Folk, J.J. Prenatal diagnosis of an inguinoscrotal hernia in a fetus with cystic fibrosis. J. Ultrasound Med. 2004, 23, 1391–1394. [Google Scholar] [CrossRef]
- Sharma, S.; Perni, S.C.; Predanic, M.; Kalish, R.B.; Zervoudakis, I.A.; Chasen, S.T. Atypical sonographic presentation of fetal unilateral inguinoscrotal hernia in a multiple gestation. J. Perinat. Med. 2004, 32, 378–380. [Google Scholar] [CrossRef]
- Kesby, G.; Beilby, R.; Petroni, M. Fetal inguinoscrotal hernia: Sonographic diagnosis and obstetric management. Ultrasound Obstet. Gynecol. 1997, 10, 359–361. [Google Scholar] [CrossRef]
- Paladini, D.; Palmieri, S.; Morelli, P.M.; Forleo, F.; Morra, T.; Salviati, M.; Zampella, C.; D’Angelo, A.; Martinelli, P. Fetal inguinoscrotal hernia: Prenatal ultrasound diagnosis and pathogenetic evaluation. Ultrasound Obstet. Gynecol. 1996, 7, 145–146. [Google Scholar] [CrossRef]
- Bohlmann, M.K.; Abele, H.; Gille, C.; Wallwiener, D.; Tekesin, I. Pränatale Diagnose einer Skrotalhernie bei einem Feten mit Trisomie 18 [Prenatal diagnosis of an inguino-scrotal hernia in a fetus with trisomy 18]. Ultraschall Med. 2009, 30, 490–491. [Google Scholar] [CrossRef]
- Ji, E.K.; Yoon, C.S.; Pretorius, D.H. Prenatal diagnosis of an inguinoscrotal hernia: Sonographic and magnetic resonance imaging findings. J. Ultrasound Med. 2005, 24, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Khatib, N.; Goldstein, I.; Vitner, D.; Ganem, N.; Livoff, A.; Wiener, Z. Prenatal diagnosis of scrotal inguinal hernia: Two case reports and review of the English literature. Eur. J. Obstetr. Gynecol. Reprod. Biol. 2013, 171, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Massaro, G.; Sglavo, G.; Cavallaro, A.; Pastore, G.; Nappi, C.; Di Carlo, C. Ultrasound prenatal diagnosis of inguinal scrotal hernia and contralateral hydrocele. Case Rep. Obstet. Gynecol. 2013, 2013, 764579. [Google Scholar] [CrossRef] [PubMed]
- Shipp, T.D.; Benacerraf, B.R. Scrotal inguinal hernia in a fetus: Sonographic diagnosis. AJR Am. J. Roentgenol. 1995, 165, 1494–1495. [Google Scholar] [CrossRef]
- Meizner, I.; Levy, A.; Katz, M.; Simhon, T.; Glezerman, M. Prenatal ultrasonographic diagnosis of fetal scrotal inguinal hernia. Am. J. Obstet. Gynecol. 1992, 166, 907–909. [Google Scholar] [CrossRef]
- Herman, A.; Schvimer, M.; Tovbin, J.; Sandbank, J.; Bukovski, I.; Strauss, S. Antenatal sonographic diagnosis of testicular torsion. Ultrasound Obstet. Gynecol. 2002, 20, 522–524. [Google Scholar] [CrossRef]
- Siu, S.S.; Leung, T.N.; Leung, T.Y.; Ng, S.W.; Yeung, C.K.; Lau, T.K. Prenatal diagnosis of intra-abdominal mature testicular teratoma. J. Ultrasound Med. 2001, 20, 1257–1260. [Google Scholar] [CrossRef]
- Shi, H.H.; Teng, R.J.; Yau, K.I.; Lin, H.H.; Hsieh, F.J.; Chen, C.C. Mature teratoma arising from an intra-abdominal undescended testis presenting as a fetal abdominal mass. Ultrasound Obstet. Gynecol. 1997, 10, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Mboyo, A.; Foulet, A.; Hocine, S.; Cheve, M.T.; Plat, M.; Weil, D. Teratoma in an undescended testis detected prenatally. J. Urol. 1997, 158, 200–201. [Google Scholar] [CrossRef] [PubMed]
- Aiken, J.J.; Oldham, K.T. Inguinal hernia: Kliegman RM, Stanton BMD. In Nelson Textbook of Paediatrics, 19th ed.; St. Geme, J., Schor, N., Bherman, R.E., Eds.; Elsevier Saunders: Philadelphia, PA, USA, 2012; Volume II, p. 1362. [Google Scholar]

| Ref. | Sample Size | N° | GA at Diagnosis (W) | Side | Bowel Peristalsis | Size (cm) | Blood Flow Signal | US Findings | Bowel Abdominal Dilatation | Fetal Comorbidities | MRI Findings | Treatment | Mode of Delivery | GA at Birth (W) | Postnatal Treatment | Post-Operative Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [3] | 2 | 1 | 39 | Right | Present and bidirectional | 4.6 × 3.5 × 3 | Present | Mass with nonhomogeneous echotexture, predominantly solid, with few small echo-free cystic areas | Present (16 mm) | N | Signal intensity similar to SB that extended from the abdominal cavity into the scrotum | CS the day after for suspicion of intestinal obstruction and incarcerated hernia (bidirectional bowel peristalsis within the scrotum) | Urgent CS (prevention of strangulation) | 39 | Surgical correction at 8 M | U |
| 2 | 36 | Right | Present | ND | Present | Enlarged scrotum with an echogenic mass inside | ND | N | Scrotum filled with SB which presented as hyperintense | ND | VD | 38 | Surgical correction at 1 M | U | ||
| [4] | 1 | 3 | 37 | Right | Present | 2.9 × 1.7 | ND | Heterogeneous echotexture. Displacement of homolateral testis. Irregular contours of the scrotum due to movements of intrascrotal echoes | ND | N | N | ND | VD | 39 | Spontaneous regression after birth | - |
| [5] | 1 | 4 | 31 | Right | Present | ND | ND | Evidence of bowel loops within the scrotum | Present (13–17 mm) | CAVB, low anorectal malformation with a perineal fistula, bowel dilatation, mild polyhydramnios | N | US FU | Urgent CS (fetal Doppler abnormalities) | 34 | Surgical correction at 6 M | ND |
| [6] | 1 | 5 | 33 | Left | Present | ND | ND | Hyperechogenic scrotal mass. Sagittal view showed herniation of the bowel through the ventral abdominal wall into the scrotum | ND | Spondylocostal dysostosis (Jarcho–Levin syndrome) | N | ND | VD | 40 | Died on day 3 due to RDS | - |
| [7] | 1 | 6 | 35 | Right | Present (noted at II examination) | 5.5 | Present | Heterogeneous scrotal mass containing echogenic areas | Absent | Mild bilateral pyelectasis | N | US FU | VD | 40 | Surgical correction at 4 D | U |
| [8] | 1 | 7 | 21 | Right | Present (noted 2 W after I examination) | 21 W → 3.3 × 3.0 36 W → 4.1 × 4.7 × 4.8 | Absent | Mass with complex echogenicity, predominantly solid with scattered small echo-free/cystic components. Homolateral testis not identified, contralateral testis displaced peripherally | Absent | N | N | US FU | CS (non-reassuring FHR on CTG) | 37 | Surgical correction after birth | U |
| [9] | 1 | 8 | 34 | Left | Present | 34 W → 3.6 × 3.0 37 W → 4.8 × 3.2 | ND | Complex mass with peristalsis; homolateral testis not identified | Present (bowel dilated and filled with echogenic meconium) | Cystic fibrosis | N | US FU | VD | ND | Surgical correction at 3 W | U |
| [10] | 1 | 9 | 34 | Right | Absent | 3.2 × 2.7 | Absent | Nonhomogeneous echogenicity, homolateral testis not clearly identified. Contralateral testis displaced peripherally | Absent | N | N | ND | CS (pPROM) | 36 | Surgical correction at 3 D | U |
| [11] | 1 | 10 | 36 | Right | Present (noted at II examination performed the day after) | 36 W → 4.6 × 5.1 × 5.3 39 W → 6.7 × 5.5 × 5.1 | Absent | Homolateral testis not identified; contralateral testis displaced peripherally. Mass with complex echogenicity, predominantly solid with scattered small echo-free components | Present. Single dilated loop of SB measuring 5.5 × 3.0 × 3.2 cm was noted at 39 W within the fetal abdomen | N | N | Weekly US FU | VD | ND | Surgical correction at 13 D | Development of a large reducible left-sided indirect inguinal hernia, which was operated on at 28 D |
| [12] | 1 | 11 | 30 | Right | Present | 4.2 | ND | Mass with mixed echostructure, with small fluid filled cystic spaces | ND | IUGR polyhydramnios, Trisomy 18, (omphalocele, clubfeet, clenched hands, large atrioventricular septal defect with a common atrioventricular valve) | N | US follow up (4 W after) | VD | 37 | Died 3 h after birth | - |
| [13] | 1 | 12 | 33 | Right | Present | ND | ND | Appearance of right scrotal tumor | Absent | IUGR, polyhydramnios Trisomy 18 (ventricular septal defect, an omphalocele, brachycephaly, bilateral clubfeet and hand abnormalities with crossed fingers, micropenis) | N | ND | VD | 35 | Died within 1 h | - |
| [14] | 1 | 13 | 36 | Left | Absent | 4.2 × 5 × 3.8 | Present | Solid mass, predominantly echogenic without a cyst. Homolateral testis not identified; the contralateral displaced laterally | Absent | Various left foot deformities | Signal intensity similar; SB on both longitudinal and transverse relaxation time-weighted imaging | ND | CS | 37 | Died at 5 D (multiple joint contractures and failure to thrive) | - |
| [15] | 2 | 14 | 36 | Bilateral | Present | 4.2 × 3.0 | Present | Bilateral scrotal masses, visualization of bowel peristalsis | Absent | Mild polyhydramnios | N | ND | VD | 38 | Operated 1 M | U |
| 15 | 24 | ND | Present | ND | ND | Swollen, enlarged scrotum with an echogenic mass inside the scrotum | ND | N | N | ND | ND | ND | Operated at 1 M | U | ||
| [16] | 1 | 16 | 37 | Right | Present (noted at II examination performed 1 W later) | 5.0 × 4.6 | Present | Echogenic mass, mixed echostructure and regular walls, containing a few small echo-free cystic areas. Hydrocele in the contralateral side | Absent | N | N | US FU | CS (breech presentation) | 38 | Operated at 10 D | U |
| [17] | 1 | 17 | 39 | Right | Present | 4 | Present | Complex, solid-appearing mass. Normal contralateral testis | ND | N | N | ND | VD | ND | Surgical repair of hernia and excision of contralateral torsed testis in the neonatal period | ND |
| [18] | 1 | 18 | 33 | Left | Present | 6.5 × 5.6 × 6.4 | ND | Moving, echo-free, cyst-like structures in an enlarged scrotum | Absent | N | N | US FU (2 W intervals) | VD | 40 | Operated at 4 D | ND |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montironi, R.; Giannubilo, S.R.; Cappanera, I.; Battistoni, G.I.; Mancinelli, R.; Ciavattini, A. Inguinoscrotal Hernia, a Possible Cause of Rapidly Developing Fetal Scrotal Mass: Case Report and Literature Update. Healthcare 2024, 12, 583. https://doi.org/10.3390/healthcare12050583
Montironi R, Giannubilo SR, Cappanera I, Battistoni GI, Mancinelli R, Ciavattini A. Inguinoscrotal Hernia, a Possible Cause of Rapidly Developing Fetal Scrotal Mass: Case Report and Literature Update. Healthcare. 2024; 12(5):583. https://doi.org/10.3390/healthcare12050583
Chicago/Turabian StyleMontironi, Ramona, Stefano Raffaele Giannubilo, Irene Cappanera, Giovanna Irene Battistoni, Romina Mancinelli, and Andrea Ciavattini. 2024. "Inguinoscrotal Hernia, a Possible Cause of Rapidly Developing Fetal Scrotal Mass: Case Report and Literature Update" Healthcare 12, no. 5: 583. https://doi.org/10.3390/healthcare12050583
APA StyleMontironi, R., Giannubilo, S. R., Cappanera, I., Battistoni, G. I., Mancinelli, R., & Ciavattini, A. (2024). Inguinoscrotal Hernia, a Possible Cause of Rapidly Developing Fetal Scrotal Mass: Case Report and Literature Update. Healthcare, 12(5), 583. https://doi.org/10.3390/healthcare12050583



_MD__MPH_PhD.png)




