Impact of Rapid Response Teams on Pediatric Care: An Interrupted Time Series Analysis of Unplanned PICU Admissions and Cardiac Arrests
Abstract
1. Introduction
Background
2. Methods
2.1. Study Design and Setting
2.2. Participants and Inclusion Criteria
2.3. Ethical Considerations
2.4. Composition of the Pediatric Rapid Response Team (RRT)
2.5. Activation and Scoring Mechanism
2.6. Data Acquisition
2.7. Outcome Measures
2.8. Statistical Analysis
3. Results
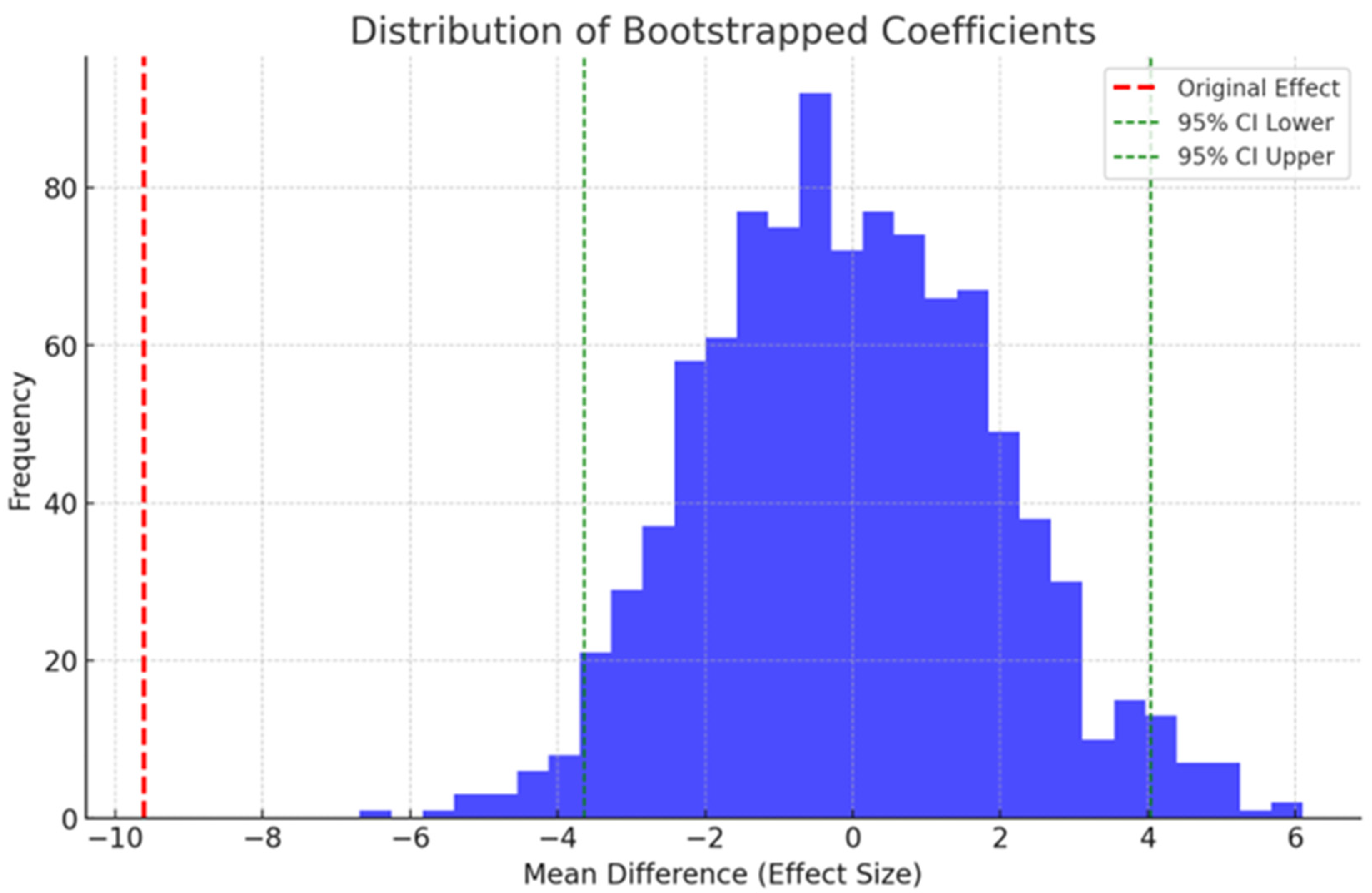
Sensitivity Test
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cohen, E.; Kuo, D.Z.; Agrawal, R.; Berry, J.G.; Bhagat, S.K.M.; Simon, T.D.; Srivastava, R. Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics 2011, 127, 529–538. [Google Scholar] [CrossRef]
- Barnert, E.S.; Coller, R.J.; Nelson, B.B.; Thompson, L.R.; Chan, V.; Padilla, C.; Klitzner, T.S.; Szilagyi, M.; Chung, P.J. Experts’ Perspectives toward a Population Health Approach for Children with Medical Complexity. Acad. Pediatr. 2017, 17, 672–677. [Google Scholar] [CrossRef]
- Prutsky, G.J.; Padhya, D.; Ahmed, A.T.; Almasri, J.; Farah, W.H.; Prokop, L.J.; Murad, M.H.; Alsawas, M. Is unplanned PICU readmission a proper quality indicator? A systematic review and meta-Analysis. Hosp. Pediatr. 2021, 11, 167–174. [Google Scholar] [CrossRef]
- Dewan, T.; Cohen, E. Children with medical complexity in Canada. Paediatr. Child Health 2013, 18, 518–522. [Google Scholar] [CrossRef]
- Hillman, K.M.; Bristow, P.J.; Chey, T.; Daffurn, K.; Jacques, T.; Norman, S.L.; Bishop, G.F.; Simmons, G. Duration of life-threatening antecedents prior to intensive care admission. Intensive Care Med. 2002, 28, 1629–1634. [Google Scholar] [CrossRef]
- Kause, J.; Smith, G.; Prytherch, D.; Parr, M.; Flabouris, A.; Hillman, K. A comparison of Antecedents to Cardiac Arrests, Deaths and EMergency Intensive care Admissions in Australia and New Zealand, and the United Kingdom—The ACADEMIA study. Resuscitation 2004, 62, 275–282. [Google Scholar] [CrossRef]
- Sandquist, M.; Tegtmeyer, K. No more pediatric code blues on the floor: Evolution of pediatric rapid response teams and situational awareness plans. Transl. Pediatr. 2018, 7, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Suominen, P.; Olkkola, K.T.; Voipio, V.; Korpela, R.; Palo, R.; Räsänen, J. Utstein style reporting of in-hospital paediatric cardiopulmonary resuscitation. Resuscitation 2000, 45, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Chen, S.; Liu, Y.; He, N.; Mo, D.; Lan, B.; Gao, Y. A prospective investigation into the epidemiology of in-hospital cardiopulmonary resuscitation using the international Utstein reporting style. Hong Kong J. Emerg. Med. 2011, 18, 391–396. [Google Scholar] [CrossRef]
- Zeng, J.; Qian, S.; Zheng, M.; Wang, Y.; Zhou, G.; Wang, H. The epidemiology and resuscitation effects of cardiopulmonary arrest among hospitalized children and adolescents in Beijing: An observational study. Resuscitation 2013, 84, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- Latif, A.; Holzmueller, C.G.; Pronovost, P.J. Evaluating Safety Initiatives in Healthcare. Curr. Anesth. Rep. 2014, 4, 100–106. [Google Scholar] [CrossRef][Green Version]
- Rathore, V.; Bansal, A.; Singhi, S.C.; Singhi, P.; Muralidharan, J. Survival and neurological outcome following in-hospital paediatric cardiopulmonary resuscitation in North India. Paediatr. Int. Child. Health 2016, 36, 141–147. [Google Scholar] [CrossRef]
- Turek, J.W.; Andersen, N.D.; Lawson, D.S.; Bonadonna, D.; Turley, R.S.; Peters, M.A.; Jaggers, J.; Lodge, A.J. Outcomes before and after implementation of a pediatric rapid-response extracorporeal membrane oxygenation program. Ann. Thorac. Surg. 2013, 95, 2140–2147. [Google Scholar] [CrossRef]
- Mansel, K.O.; Chen, S.W.; Mathews, A.A.; Gothard, M.D.; Bigham, M.T. Here and Gone: Rapid Transfer From the General Care Floor to the PICU. Hosp. Pediatr. 2018, 8, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, P.S.L.; De Aguiar, V.E.; Machado Fonseca, M.C. Risk factors and outcomes of unplanned PICU postoperative admissions: A nested case-control study. Pediatr. Crit. Care Med. 2013, 14, 420–428. [Google Scholar] [CrossRef]
- Krmpotic, K.; Lobos, A.T. Clinical Profile of Children Requiring Early Unplanned Admission to the PICU. Hosp. Pediatr. 2013, 3, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Odetola, F.O.; Rosenberg, A.L.; Davis, M.M.; Clark, S.J.; Dechert, R.E.; Shanley, T.P. Do outcomes vary according to the source of admission to the pediatric intensive care unit? Pediatr. Crit. Care Med. 2008, 9, 20–25. [Google Scholar] [CrossRef]
- El Halal, M.G.D.S.; Barbieri, E.; Filho, R.; Trotta, E.; Carvalho, P. Admission source and mortality in a pediatric intensive care unit. Indian J. Crit. Care Med. 2012, 16, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, S.; Kim, M. Outcome Differences Between Direct Admissions to the PICU From ED and Escalations From Floor. Hosp. Pediatr. 2021, 11, 1237–1249. [Google Scholar] [CrossRef]
- Palatnik, A.M. To err IS human. In Nursing Critical Care; Wiley Online Library: Hoboken, NJ, USA, 2016; Volume 11, 4p. [Google Scholar]
- Bates, D.W.; Singh, H. Two decades since to err is human: An assessment of progress and emerging priorities in patient safety. Health Aff. 2018, 37, 1736–1743. [Google Scholar] [CrossRef]
- Hayes, L.W.; Dobyns, E.L.; DiGiovine, B.; Brown, A.-M.; Jacobson, S.; Randall, K.H.; Wathen, B.; Schwab, C.; Duncan, K.D.; Thrasher, J.; et al. A multicenter collaborative approach to reducing pediatric codes outside the ICU. Pediatrics 2012, 129, e785–e791. [Google Scholar] [CrossRef]
- NHS England and NHS Improvement. Implementing the NHS Patient Safety Strategy: Safer Culture, Safer Systems, Safer Patients. 2019, pp. 1–82. Available online: https://www.england.nhs.uk/wp-content/uploads/2020/08/190708_Patient_Safety_Strategy_for_website_v4.pdf (accessed on 1 January 2024).
- Jha, A.K.; Larizgoitia, I.; Audera-Lopez, C.; Prasopa-Plaizier, N.; Waters, H.; Bates, D.W. The global burden of unsafe medical care: Analytic modelling of observational studies. BMJ Qual. Saf. 2013, 22, 809–815. [Google Scholar] [CrossRef]
- Thomas, K.; Force, M.V.; Rasmussen, D.; Dodd, D.; Whildin, S. Rapid Response Team. Crit. Care Nurse 2007, 27, 20–27. [Google Scholar] [CrossRef]
- Accreditation Canada. Required Organizational Practices. 2020, pp. 33–34. Available online: https://www.rqhealth.ca/rqhr-service-lines-files/accreditation-canada-antimicrobial-stewardship-rop (accessed on 1 January 2024).
- Kutty, S.; Jones, P.G.; Karels, Q.; Joseph, N.; Spertus, J.A.; Chan, P.S. Association of pediatric medical emergency teams with hospital mortality. Circulation 2018, 137, 38–46. [Google Scholar] [CrossRef]
- Hanson, C.C.; Randolph, G.D.; Erickson, J.A.; Mayer, C.M.; Bruckel, J.T.; Harris, B.D.; Willis, T.S. A reduction in cardiac arrests and duration of clinical instability after implementation of a paediatric rapid response system. Postgrad. Med. J. 2010, 86, 314–318. [Google Scholar] [CrossRef]
- Bavare, A.C.; Rafie, K.S.; Bastero, P.X.; Hagan, J.L.; Checchia, P.A. Acute decompensation in pediatric cardiac patients: Outcomes after rapid response events. Pediatr. Crit. Care Med. 2017, 18, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.-J.; Kwon, O.; Kwon, J.-M.; Lee, Y.; Park, H.; Jeon, K.-H.; Kim, K.-H.; Park, J.; Oh, B.-H. Detecting patient deterioration using artificial intelligence in a rapid response system. Crit. Care Med. 2020, 48, E285–E289. [Google Scholar] [CrossRef] [PubMed]
- Parshuram, C.S.; Dryden-Palmer, K.; Farrell, C.; Gottesman, R.; Gray, M.; Hutchison, J.S.; Helfaer, M.; Hunt, E.A.; Joffe, A.R.; Lacroix, J.; et al. Effect of a pediatric early warning system on all-cause mortality in Hospitalized pediatric patients: The epoch randomized clinical trial. JAMA—J. Am. Med. Assoc. 2018, 319, 1002–1012. [Google Scholar] [CrossRef]
- Mills, D.; Schmid, A.; Najajreh, M.; Al Nasser, A.; Awwad, Y.; Qattush, K.; Monuteaux, M.C.; Hudgins, J.; Salman, Z.; Niescierenko, M. Implementation of a pediatric early warning score tool in a pediatric oncology Ward in Palestine. BMC Health Serv. Res. 2021, 21, 1159. [Google Scholar] [CrossRef] [PubMed]
- Tibballs, J.; Kinney, S.; Bellomo, R. A prospective before-and-after trial of a medical emergency team. Med. J. Aust. 2004, 180, 308–310. [Google Scholar] [CrossRef]
- Bellomo, R.; Goldsmith, D.; Uchino, S.; Buckmaster, J.; Hart, G.; Opdam, H.; Silvester, W.; Doolan, L.; Gutteridge, G. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit. Care Med. 2004, 32, 916–921. [Google Scholar] [CrossRef] [PubMed]
- Buist, M.D.; Moore, G.E.; Bernard, S.A.; Waxman, B.P.; Anderson, J.N.; Nguyen, T.V. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: Preliminary study. Br. Med. J. 2002, 324, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Parshuram, C.S.; Hutchison, J.; Middaugh, K. Development and initial validation of the Bedside Paediatric Early Warning System score. Crit. Care 2009, 13, R135. [Google Scholar] [CrossRef] [PubMed]
- Breslin, K.; Marx, J.; Hoffman, H.; McBeth, R.; Pavuluri, P. Pediatric early warning score at time of emergency department disposition is associated with level of care. Pediatr. Emerg. Care 2014, 30, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Fuijkschot, J.; Vernhout, B.; Lemson, J.; Draaisma, J.M.T.; Loeffen, J.L.C.M. Validation of a paediatric early warning score: First results and implications of usage. Eur. J. Pediatr. 2015, 174, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Vredebregt, S.J.; Moll, H.A.; Smit, F.J.; Verhoeven, J.J. Recognizing critically ill children with a modified pediatric early warning score at the emergency department, a feasibility study. Eur. J. Pediatr. 2019, 178, 229–234. [Google Scholar] [CrossRef]
- Sharek, P.J.; Parast, L.M.; Leong, K.; Coombs, J.; Earnest, K.; Sullivan, J.; Frankel, L.R.; Roth, S.J. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a Children’s Hospital. JAMA 2007, 298, 2267–2274. [Google Scholar] [CrossRef]
- Kukreti, V.; Gaiteiro, R.; Mohseni-Bod, H. Implementation of a pediatric rapid response team: Experience of the Hospital for Sick Children in Toronto. Indian Pediatr. 2014, 51, 11–15. [Google Scholar] [CrossRef]
- McKeta, A.S.; Hlavacek, A.M.; Chowdhury, S.M.; Scheurer, M.; Graham, E.M.; Zyblewski, S.C.; Buckley, J.R. Improved outcomes after implementation of a specialized pediatric cardiac rapid response team. Cardiol. Young 2022, 31, 1582–1588. [Google Scholar] [CrossRef] [PubMed]
- Meulmester, K.M.; Coss-Bu, J.A.; Meskill, S.D.; Wakefield, B.M.; Moore, R.H.; Vachani, J.G.; Bavare, A.C. Characteristics and Outcomes of Pediatric Rapid Response with a Respiratory Trigger. Hosp. Pediatr. 2021, 11, 806–807. [Google Scholar] [CrossRef] [PubMed]
- White, K.; Scott, I.A.; Bernard, A.; McCulloch, K.; Vaux, A.; Joyce, C.; Sullivan, C.M. Patient characteristics, interventions and outcomes of 1151 rapid response team activations in a tertiary hospital: A prospective study. Intern. Med. J. 2016, 46, 1398–1406. [Google Scholar] [CrossRef]
- Lockwood, J.M.; Ziniel, S.I.; Bonafide, C.P.; Brady, P.W.; O’leary, S.T.; Reese, J.; Wathen, B.; Dempsey, A.F. Characteristics of Pediatric Rapid Response Systems: Results From a Survey of PRIS Hospitals. Hosp. Pediatr. 2021, 11, 144–152. [Google Scholar] [CrossRef]
- Jung, B.; Daurat, A.; De Jong, A.; Chanques, G.; Mahul, M.; Monnin, M.; Molinari, N.; Jaber, S. Rapid response team and hospital mortality in hospitalized patients. Intensive Care Med. 2016, 42, 494–504. [Google Scholar] [CrossRef]
- Likosky, D.S. Clinical Microsystems: A Critical Framework for Crossing the Quality Chasm. J. Extracorpor. Technol. 2014, 46, 33–37. [Google Scholar] [CrossRef]
- Gill, F.J.; Leslie, G.D.; Marshall, A.P. Family initiated escalation of care for the deteriorating patient in hospital: Family centred care or just “box ticking”. Aust. Crit. Care 2016, 29, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Cox, E.D.; Jacobsohn, G.C.; Rajamanickam, V.P.; Carayon, P.; Kelly, M.M.; Wetterneck, T.B.; Rathouz, P.J.; Brown, R.L. A Family-Centered Rounds Checklist, Family Engagement, and Patient Safety: A Randomized Trial. Pediatrics 2017, 139, 20161688. [Google Scholar] [CrossRef]
- Bavare, A.C.; Thomas, J.K.; Elliott, E.P.; Morgan, A.C.; Graf, J.M. Family-Initiated Pediatric Rapid Response: Characteristics, Impetus, and Outcomes. J. Health Qual. 2018, 40, 2018. [Google Scholar] [CrossRef] [PubMed]
- Gill, F.J.; Leslie, G.D.; Marshall, A.P. The Impact of Implementation of Family-Initiated Escalation of Care for the Deteriorating Patient in Hospital: A Systematic Review. Worldviews Evid. Based Nurs. 2016, 13, 10–11. [Google Scholar] [CrossRef] [PubMed]
- Brady, P.W.; Zix, J.; Brilli, R.; Wheeler, D.S.; Griffith, K.; Giaccone, M.J.; Dressman, K.; Kotagal, U.; Muething, S.; Tegtmeyer, K. Developing and evaluating the success of a family activated medical emergency team: A quality improvement report. BMJ Qual. Saf. 2015, 24, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Albutt, A.K.; O’Hara, J.K.; Conner, M.T.; Fletcher, S.J.; Lawton, R.J. Is there a role for patients and their relatives in escalating clinical deterioration in hospital? A systematic review. Health Expect. 2017, 20, 818–825. [Google Scholar] [CrossRef]
- Penfold, R.B.; Zhang, F. Use of Interrupted Time Series Analysis in Evaluating Health Care Quality Improvements a brief description of its analysis. Acad. Pediatr. 2013, 13, S38–S44. [Google Scholar] [CrossRef] [PubMed]
- Wachter, R.M.; Pronovost, P.J. The 100,000 lives campaign: A scientific and policy review. Jt. Comm. J. Qual. Patient Saf. 2006, 32, 621–627. [Google Scholar] [CrossRef]
- Lyons, P.G.; Edelson, D.P.; Churpek, M.M. Rapid response systems. Resuscitation 2018, 128, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Winters, B.D.; Pham, J.C.; Hunt, E.A.; Guallar, E.; Berenholtz, S.; Pronovost, P.J. Rapid response systems: A systematic review. Crit. Care Med. 2007, 35, 1238–1243. [Google Scholar] [CrossRef]
- Hillman, K.; Chen, J.; Cretikos, M.; Bellomo, R.; Brown, D.; Finfer, S.; Flabouris, A.; MERIT Study Investigators. Introduction of the medical emergency team (MET) system: A cluster-randomised controlled trial. Lancet 2005, 366, 1164. [Google Scholar]
- Taylor, N.; Hendron, E.; Manning, J.C. Paediatric family activated rapid response interventions; qualitative systematic review. Intensive Crit. Care Nurs. 2023, 75, 103363. [Google Scholar]
- Humphreys, S.; Humphreys, S. Rapid Response Team Calls and Unplanned Transfers to the Pediatric Intensive Care Unit in a Pediatric Hospital. Am. J. Crit. Care 2016, 25, e9–e13. [Google Scholar] [CrossRef]
- Bonafide, C.P.; Localio, A.R.; Roberts, K.E.; Nadkarni, V.M.; Weirich, C.M.; Keren, R. Impact of rapid response system implementation on critical deterioration events in children. JAMA Pediatr. 2014, 168, 25–33. [Google Scholar] [CrossRef]
- Panesar, R.; Polikoff, L.A.; Harris, D.; Mills, B.; Messina, C.; Parker, M.M. Characteristics and outcomes of pediatric rapid response teams before and after mandatory triggering by an elevated Pediatric Early Warning System (PEWS) score. Hosp. Pediatr. 2014, 4, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Kolovos, N.S.; Gill, J.; Michelson, P.H.; Doctor, A.; Hartman, M.E. Reduction in mortality following pediatric rapid response team implementation. Pediatr. Crit. Care Med. 2018, 19, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Kinney, S.; Tibballs, J.; Johnston, L.; Duke, T. Clinical profile of hospitalized children provided with urgent assistance from a medical emergency team. Pediatrics 2008, 121, 1577–1584. [Google Scholar] [CrossRef] [PubMed]
- Tibballs, J.; Kinney, S. Reduction of hospital mortality and of preventable cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatr. Crit. Care Med. 2009, 10, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Berrens, Z.J.; Gosdin, C.H.; Brady, P.W. Efficacy and safety of pediatric critical care physician telemedicine involvement in rapid response team and code response in a satellite facility. Pediatr. Crit. Care Med. 2019, 20, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Peatfield, R.C.; Taylor, D.; Sillett, R.W.; McNicol, M.W. Survival after cardiac arrest in hospital. Lancet 1977, 309, 92435. [Google Scholar] [CrossRef] [PubMed]
- Bimerew, M.; Wondmieneh, A.; Gedefaw, G.; Gebremeskel, T.; Demis, A.; Getie, A. Survival of pediatric patients after cardiopulmonary resuscitation for in-hospital cardiac arrest: A systematic review and meta-analysis. Ital. J. Pediatr. 2021, 47, 118. [Google Scholar] [CrossRef] [PubMed]
- Girotra, S.; Nallamothu, B.K.; Spertus, J.A.; Li, Y.; Krumholz, H.M.; Chan, P.S. Trends in Survival after In-Hospital Cardiac Arrest. N. Engl. J. Med. 2012, 367, 1912–1920. [Google Scholar] [CrossRef] [PubMed]
- Weaver, W.D.; Cobb, L.A.; Hallstrom, A.P.; Fahrenbruch, C.; Copass, M.K.; Ray, R. Factors influencing survival after out-of-hospital cardiac arrest. J. Am. Coll. Cardiol. 1986, 7, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Schein, R.M.; Hazday, N.; Pena, M.; Ruben, B.H.; Sprung, C.L. Clinical Antecedents to In-Hospital Cardiopulmonary Arrest. Chest 1990, 98, 1388–1392. [Google Scholar] [CrossRef]
- Franklin, C.; Mathew, J. Developing strategies to prevent inhospital cardiac arrest: Analyzing responses of physicians and nurses in the hours before the event. Crit. Care Med. 1994, 22, 7–8. [Google Scholar] [CrossRef]
- McLellan, M.C.; Gauvreau, K.; Connor, J.A. Validation of the Children’s Hospital Early Warning System for Critical Deterioration Recognition. J. Pediatr. Nurs. 2017, 32, 52–58. [Google Scholar] [CrossRef]
- Brilli, R.J.M.; Gibson, R.R.; Luria, J.W.M.; Wheeler, T.A.M.; Shaw, J.M.; Linam, M.; Kheir, J.; McLain, P.R.; Lingsch, T.R.; Hall-Haering, A.R.; et al. Implementation of a medical emergency team in a large pediatric teaching hospital prevents respiratory and cardiopulmonary arrests outside the intensive care unit. Pediatr. Crit. Care Med. 2007, 8, 236–246. [Google Scholar] [CrossRef] [PubMed]
- Mueller, S.S. Rapid-Response Systems as a Patient Safety Strategy. Physiol. Behav. 2018, 176, 139–148. [Google Scholar]
- Maharaj, R.; Raffaele, I.; Wendon, J. Rapid response systems: A systematic review and meta-analysis. Crit. Care 2015, 19, 254. [Google Scholar] [CrossRef] [PubMed]
- TTrubey, R.; Huang, C.; Lugg-Widger, F.V.; Hood, K.; Allen, D.; Edwards, D.; Lacy, D.; Lloyd, A.; Mann, M.; Mason, B.; et al. Validity and effectiveness of paediatric early warning systems and track and trigger tools for identifying and reducing clinical deterioration in hospitalised children: A systematic review. BMJ Open 2019, 9, e022105. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.-L.; Goh, M.S.L.; Ong, G.Y.-K.; Acworth, J.; Sultana, R.; Yao, S.H.W.; Ng, K.C.; Scholefield, B.; Aickin, R.; Maconochie, I.; et al. Do paediatric early warning systems reduce mortality and critical deterioration events among children? A systematic review and meta-analysis. Resusc. Plus 2022, 11, 100262. [Google Scholar] [CrossRef] [PubMed]
- Al-Qahtani, S.M.; Al-Dorzi, H.M.; Tamim, H.M.; Hussain, S.M.; Fong, L.; Taher, S.M.; Al-Knawy, B.A.M.; Arabi, Y.M. Impact of an intensivist-led multidisciplinary extended rapid response team on hospital-wide cardiopulmonary arrests and mortality. Crit. Care Med. 2013, 41, 506–517. [Google Scholar] [CrossRef]
- Joffe, A.R.; Anton, N.R.; Burkholder, S.C. Reduction in Hospital Mortality over Time in a Hospital without a Pediatric Medical Emergency Team. Arch. Pediatr. Adolesc. Med. 2011, 165, 419–423. [Google Scholar] [CrossRef]
- Sandhu, E.J. Rapid response teams. Am. J. Nurs. 2015, 115, 13. [Google Scholar] [CrossRef]
- Gong, X.-Y.; Wang, Y.-G.; Shao, H.-Y.; Lan, P.; Yan, R.-S.; Pan, K.-H.; Zhou, J.-C. A rapid response team is associated with reduced overall hospital mortality in a Chinese tertiary hospital: A 9-year cohort study. Ann. Transl. Med. 2020, 8, 317. [Google Scholar] [CrossRef]
- Solomon, R.S.; Corwin, G.S.; Barclay, D.C.; Quddusi, S.F.; Dannenberg, M.D. Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: A systematic review and meta-analysis. J. Hosp. Med. 2016, 11, 438–445. [Google Scholar] [CrossRef]
| Score = 0–3 | Score = 4–6 | Score ≥ 7 |
|---|---|---|
|
|
|
| Variable | Pre-Intervention | Post-Intervention | p-Value |
|---|---|---|---|
| Date range | 1 January 2014 to 30 August 2015 | 1 September 2015 to 30 July 2017 | x |
| Total number of months | 22 | 21 | x |
| PEWS score (median [IQR]) | 6.00 [5.00, 6.75] | 6.00 [5.00, 7.00] | 0.217 |
| Age, median (IQR) | 6 (IQR 2–12) | 7 (IQR 3–24) | 0.31 |
| Gender, Female (%) | 725 (45.2%) | 780 (46.5%) | 0.45 |
| Ward admission (median [IQR]) | 72.50 [67.25, 79.75] | 80.00 [78.00, 82.00] | 0.009 |
| WdToPICUAd (median [IQR]) | 21.50 [20.25, 25.75] | 13.00 [10.00, 18.00] | <0.001 |
| inPtcode (median [IQR]) | 2.00 [0.25, 3.00] | 0.00 [0.00, 0.00] | <0.001 |
| PICU Mortality (median [IQR]) | 3.00 [2.00, 3.00] | 1.00 [1.00, 2.00] | 0.001 |
| MortalityWAd (median [IQR]) | 2.00 [0.25, 2.00] | 0.00 [0.00, 0.00] | <0.001 |
| PICU Admission | Non PICU Admission | Total | |
|---|---|---|---|
| Exposed (Post Intervention) | 281 | 1396 | 1677 |
| Un-Exposed (Pre-Intervention) | 487 | 1117 | 1604 |
| Total | 768 | 2513 | 3281 |
| Results: Estimate 0.552, 95% CI (0.485–0.628), p-value 0.0001 | |||
| College | Cardiopulmonary Arrest | No Cardiopulmonary Arrest | Total |
|---|---|---|---|
| Pre-Intervention | 24 | 1580 | 1604 |
| Post-Intervention | 0 | 1674 | 1674 |
| Total | 24 | 3254 | 3278 |
| Results: Since there are 0 events in the post-intervention group, the RR would be 0. This indicates a complete reduction in the event rate (non-ICU cardiopulmonary arrest) post-intervention. | |||
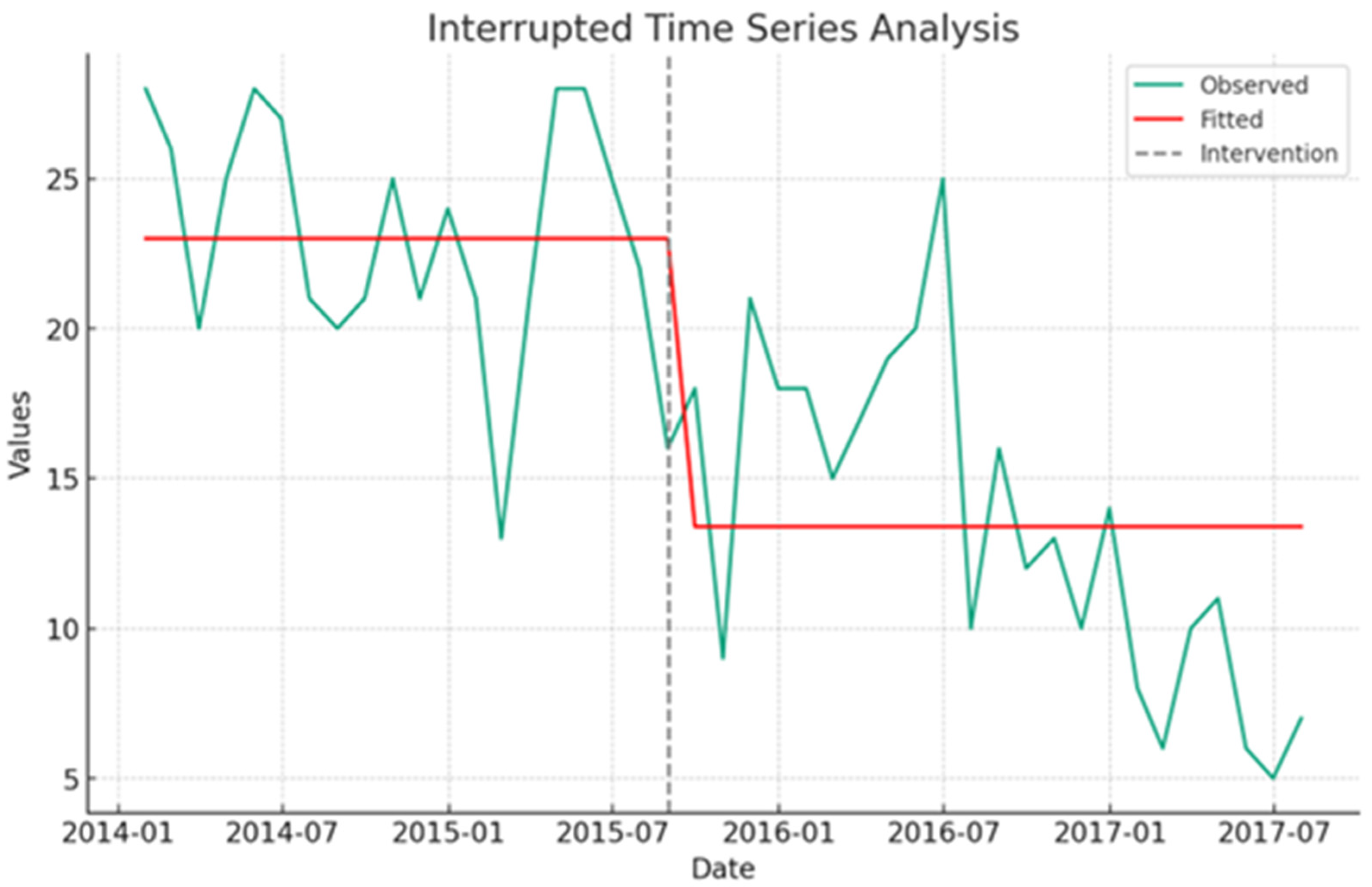
| Variable | Coefficient | Std Error | t-Value | 95% CI | p-Value |
|---|---|---|---|---|---|
| Unplanned PICU Admission | |||||
| Intercept | 23.00 | 1.100 | 20.97 | 20.78–25.22 | <0.001 |
| RRTs action | −9.61 | 1.504 | −6.391 | −12.65 to −6.57 | <0.001 |
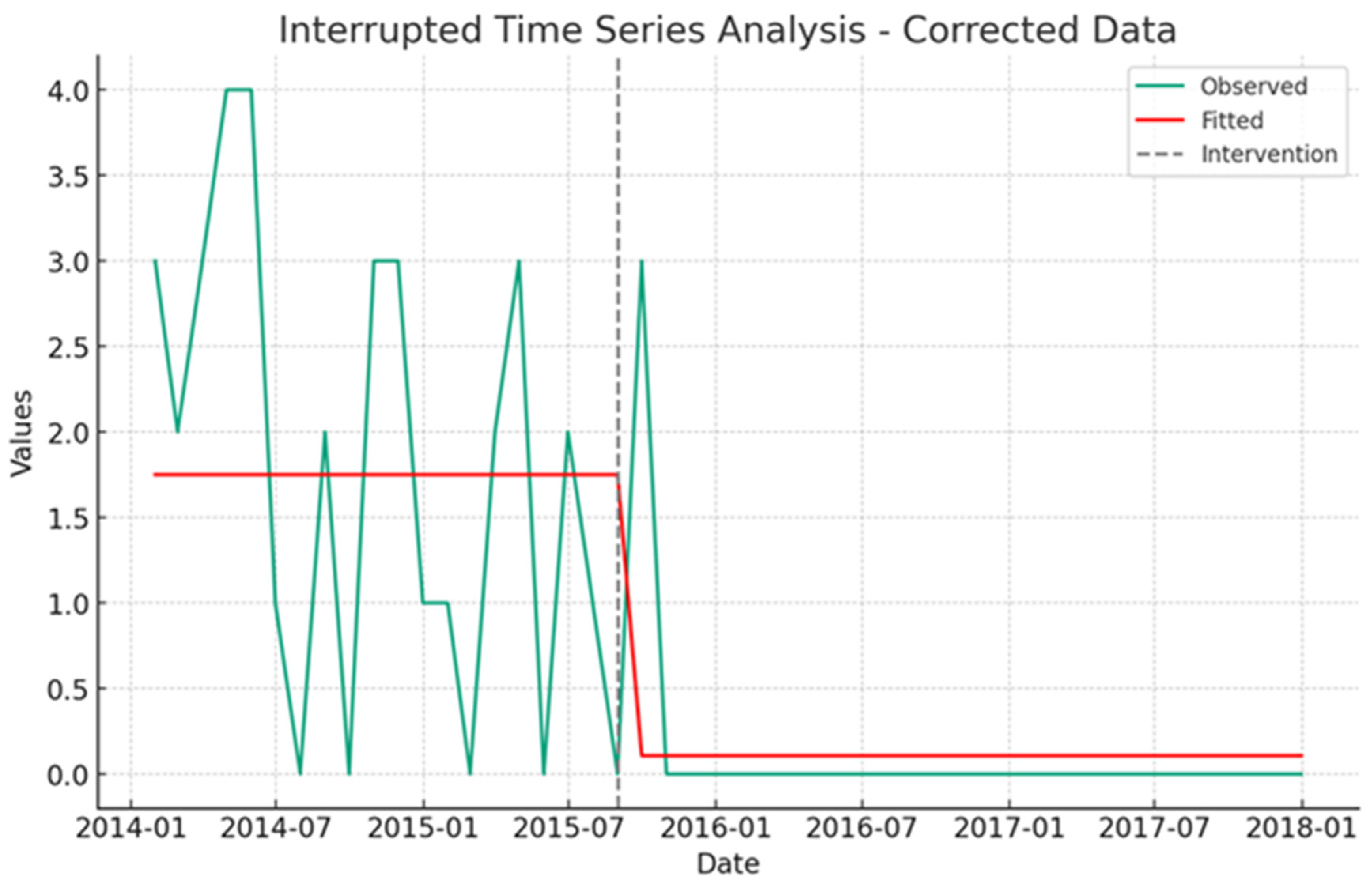
| Non-ICU Cardiopulmonary Arrest (Code Blue) | |||||
| Intercept | 1.750 | 0.220 | 7.963 | 1.31–2.19 | <0.001 |
| RRTs action | −1.641 | 0.288 | −5.71 | −2.22 to −1.06 | <−0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Harbi, S. Impact of Rapid Response Teams on Pediatric Care: An Interrupted Time Series Analysis of Unplanned PICU Admissions and Cardiac Arrests. Healthcare 2024, 12, 518. https://doi.org/10.3390/healthcare12050518
Al-Harbi S. Impact of Rapid Response Teams on Pediatric Care: An Interrupted Time Series Analysis of Unplanned PICU Admissions and Cardiac Arrests. Healthcare. 2024; 12(5):518. https://doi.org/10.3390/healthcare12050518
Chicago/Turabian StyleAl-Harbi, Samah. 2024. "Impact of Rapid Response Teams on Pediatric Care: An Interrupted Time Series Analysis of Unplanned PICU Admissions and Cardiac Arrests" Healthcare 12, no. 5: 518. https://doi.org/10.3390/healthcare12050518
APA StyleAl-Harbi, S. (2024). Impact of Rapid Response Teams on Pediatric Care: An Interrupted Time Series Analysis of Unplanned PICU Admissions and Cardiac Arrests. Healthcare, 12(5), 518. https://doi.org/10.3390/healthcare12050518






