The Role of Artificial Intelligence in Improving Patient Outcomes and Future of Healthcare Delivery in Cardiology: A Narrative Review of the Literature
Abstract
1. Introduction
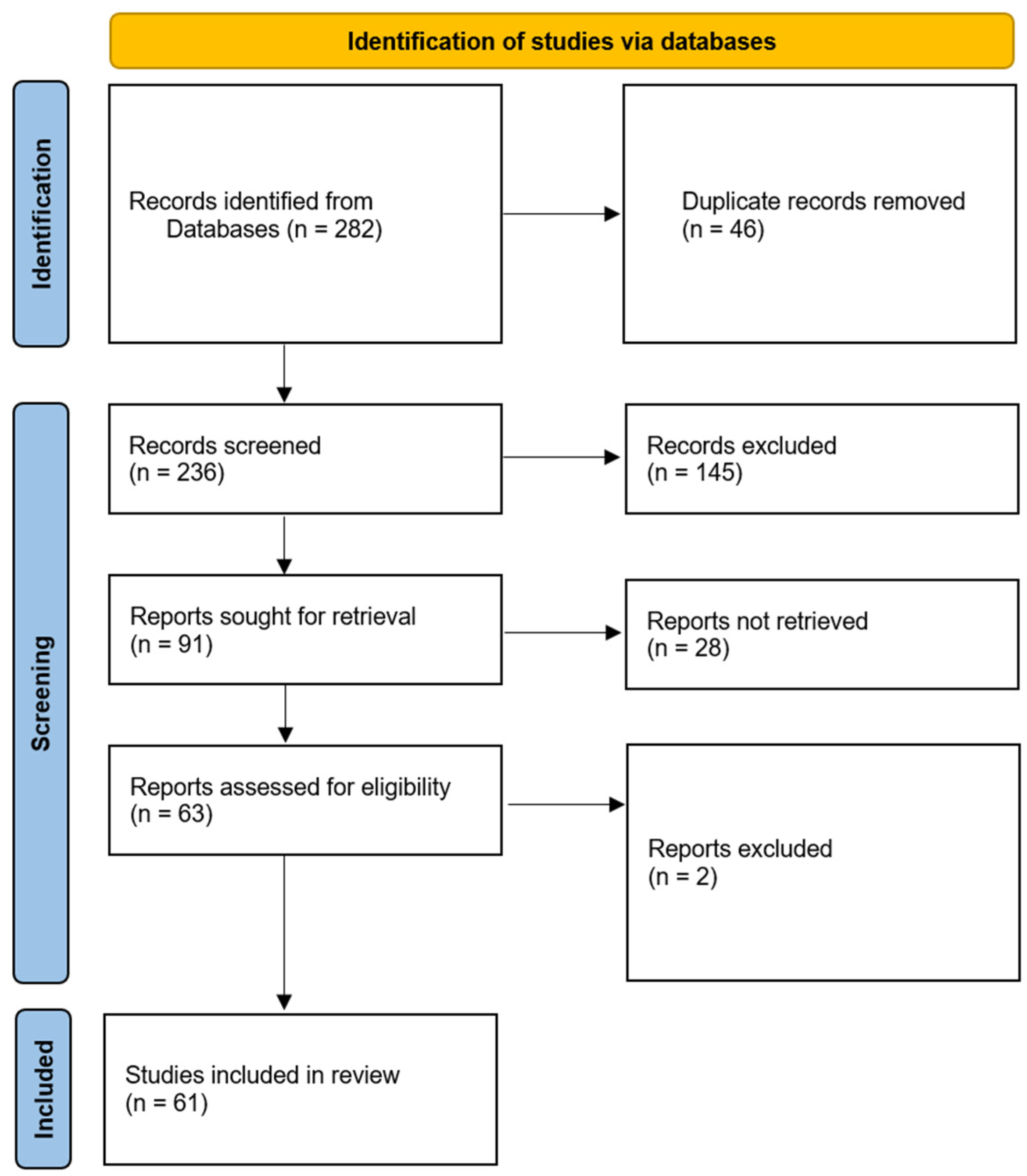
2. Methods
3. Accelerating Patient Benefits in Cardiology Using Artificial Intelligence
4. Decision Support Systems in Cardiovascular Health
5. Personalized Cardiology Using Machine Learning
6. Challenges and Future Directions
7. Conclusions
8. Key Points
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Winnige, P.; Vysoky, R.; Dosbaba, F.; Batalik, L. Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases. World J. Clin. Cases 2021, 9, 1761–1784. [Google Scholar] [CrossRef]
- Rippe, J.M. Lifestyle Strategies for Risk Factor Reduction, Prevention, and Treatment of Cardiovascular Disease. Am. J. Lifestyle Med. 2018, 13, 204–212. [Google Scholar] [CrossRef]
- Schwalm, J.; McKee, M.; Huffman, M.D.; Yusuf, S. Resource Effective Strategies to Prevent and Treat Cardiovascular Disease. Circ. 2016, 133, 742–755. [Google Scholar] [CrossRef]
- Gala, D.; Makaryus, A.N. The Utility of Language Models in Cardiology: A Narrative Review of the Benefits and Concerns of ChatGPT-4. Int. J. Environ. Res. Public Health 2023, 20, 6438. [Google Scholar] [CrossRef] [PubMed]
- Maddula, R.; MacLeod, J.; McLeish, T.; Painter, S.; Steward, A.; Berman, G.; Hamid, A.; Abdelrahim, M.; Whittle, J.; Brown, S.A.; et al. The role of digital health in the cardiovascular learning healthcare system. Front. Cardiovasc. Med. 2022, 9, 1008575. [Google Scholar] [CrossRef] [PubMed]
- Sarker, I.H. AI-Based Modeling: Techniques, Applications and Research Issues Towards Automation, Intelligent and Smart Systems. SN Comput. Sci. 2022, 3, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Sennott, S.C.; Akagi, L.; Lee, M.; Rhodes, A. AAC and Artificial Intelligence (AI). Top. Lang. Disord. 2019, 39, 389–403. [Google Scholar] [CrossRef]
- Xu, Y.; Liu, X.; Cao, X.; Huang, C.; Liu, E.; Qian, S.; Liu, X.; Wu, Y.; Dong, F.; Qiu, C.-W.; et al. Artificial intelligence: A powerful paradigm for scientific research. Innov. 2021, 2, 100179. [Google Scholar] [CrossRef] [PubMed]
- Poalelungi, D.G.; Musat, C.L.; Fulga, A.; Neagu, M.; Neagu, A.I.; Piraianu, A.I.; Fulga, I. Advancing Patient Care: How Artificial Intelligence Is Transforming Healthcare. J. Pers. Med. 2023, 13, 1214. [Google Scholar] [CrossRef] [PubMed]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef]
- Hossain, E.; Rana, R.; Higgins, N.; Soar, J.; Barua, P.D.; Pisani, A.R.; Turner, K. Natural Language Processing in Electronic Health Records in relation to healthcare decision-making: A systematic review. Comput. Biol. Med. 2023, 155, 106649. [Google Scholar] [CrossRef]
- Nadkarni, P.M.; Ohno-Machado, L.; Chapman, W.W. Natural language processing: An introduction. J. Am. Med. Inform. Assoc. 2011, 18, 544–551. [Google Scholar] [CrossRef]
- Nedadur, R.; Wang, B.; Yanagawa, B. The cardiac surgeon’s guide to artificial intelligence. Curr. Opin. Cardiol. 2021, 36, 637–643. [Google Scholar] [CrossRef]
- Doulamis, I.P.; Spartalis, E.; Machairas, N.; Schizas, D.; Patsouras, D.; Spartalis, M.; Tsilimigras, D.I.; Moris, D.; Iliopoulos, D.C.; Tzani, A.; et al. The role of robotics in cardiac surgery: A systematic review. J. Robot. Surg. 2018, 13, 41–52. [Google Scholar] [CrossRef]
- Kwan, A.C.; Salto, G.; Cheng, S.; Ouyang, D. Artificial Intelligence in Computer Vision: Cardiac MRI and Multimodality Imaging Segmentation. Curr. Cardiovasc. Risk Rep. 2021, 15, 1–8. [Google Scholar] [CrossRef]
- Dey, D.; Slomka, P.J.; Leeson, P.; Comaniciu, D.; Shrestha, S.; Sengupta, P.P.; Marwick, T.H. Artificial Intelligence in Cardiovascular Imaging: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 73, 1317–1335. [Google Scholar] [CrossRef]
- Luneski, A.; Konstantinidis, E.; Bamidis, P.D. Affective medicine. A review of affective computing efforts in medical informatics. Methods Inf. Med. 2010, 49, 207–218. [Google Scholar] [CrossRef]
- Aldosari, B.; Babsai, R.; Alanazi, A.; Aldosari, H.; Alanazi, A. The Progress of Speech Recognition in Health Care: Surgery as an Example. Stud. Health Technol. Inform. 2023, 305, 414–418. [Google Scholar]
- Dinari, F.; Bahaadinbeigy, K.; Bassiri, S.; Mashouf, E.; Bastaminejad, S.; Moulaei, K. Benefits, barriers, and facilitators of using speech recognition technology in nursing documentation and reporting: A cross-sectional study. Health Sci. Rep. 2023, 6, e1330. [Google Scholar] [CrossRef] [PubMed]
- Sotirakos, S.; Fouda, B.; Razif, N.A.M.; Cribben, N.; Mulhall, C.; O’Byrne, A.; Moran, B.; Connolly, R. Harnessing artificial intelligence in cardiac rehabilitation, a systematic review. Futur. Cardiol. 2022, 18, 154–164. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision Medicine, AI, and the Future of Personalized Health Care. Clin. Transl. Sci. 2020, 14, 86–93. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med Educ. 2023, 23, 1–15. [Google Scholar] [CrossRef]
- Jeyaraman, M.; Balaji, S.; Jeyaraman, N.; Yadav, S. Unraveling the Ethical Enigma: Artificial Intelligence in Healthcare. Cureus 2023, 15, e43262. [Google Scholar] [CrossRef]
- Patel, B.; Makaryus, A.N. Artificial Intelligence Advances in the World of Cardiovascular Imaging. Healthcare 2022, 10, 154. [Google Scholar] [CrossRef]
- Siontis, K.C.; Noseworthy, P.A.; Attia, Z.I.; Friedman, P.A. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat. Rev. Cardiol. 2021, 18, 465–478. [Google Scholar] [CrossRef]
- Hannun, A.Y.; Rajpurkar, P.; Haghpanahi, M.; Tison, G.H.; Bourn, C.; Turakhia, M.P.; Ng, A.Y. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat. Med. 2019, 25, 65–69. [Google Scholar] [CrossRef]
- I Attia, Z.; A Noseworthy, P.; Lopez-Jimenez, F.; Asirvatham, S.J.; Deshmukh, A.J.; Gersh, B.J.; E Carter, R.; Yao, X.; A Rabinstein, A.; Erickson, B.J.; et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: A retrospective analysis of outcome prediction. Lancet 2019, 394, 861–867. [Google Scholar] [CrossRef]
- Zhou, J.; Du, M.; Chang, S.; Chen, Z. Artificial intelligence in echocardiography: Detection, functional evaluation, and disease diagnosis. Cardiovasc. Ultrasound 2021, 19, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhu, Y.; Liu, M.; Zhang, Z.; Zhao, Y.; Yang, X.; Xie, M.; Zhang, L. Artificial Intelligence-Enhanced Echocardiography for Systolic Function Assessment. J. Clin. Med. 2022, 11, 2893. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Liu, S.; Cai, W.; Che, H.; Pujol, S.; Kikinis, R.; Feng, D.; Fulham, M.J.; ADNI. Multimodal neuroimaging feature learning for multiclass diagnosis of Alzheimer’s disease. IEEE Trans. Biomed. Eng. 2015, 62, 1132–1140. [Google Scholar] [CrossRef] [PubMed]
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G.; et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019, 25, 954–961. [Google Scholar] [CrossRef] [PubMed]
- Göçer, H.; Durukan, A.B. The use of artificial intelligence in interventional cardiology. Turk. J. Thorac. Cardiovasc. Surg. 2023, 31, 420–421. [Google Scholar] [CrossRef]
- Mohsen, F.; Al-Saadi, B.; Abdi, N.; Khan, S.; Shah, Z. Artificial Intelligence-Based Methods for Precision Cardiovascular Medicine. J. Pers. Med. 2023, 13, 1268. [Google Scholar] [CrossRef]
- Mega, J.L.; O Stitziel, N.; Smith, J.G.; I Chasman, D.; Caulfield, M.J.; Devlin, J.J.; Nordio, F.; Hyde, C.L.; Cannon, C.P.; Sacks, F.M.; et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: An analysis of primary and secondary prevention trials. Lancet 2015, 385, 2264–2271. [Google Scholar] [CrossRef]
- Adam, T.J.; Chi, C.L. Big Data Cohort Extraction for Personalized Statin Treatment and Machine Learning. Methods Mol. Biol. 2019, 1939, 255–272. [Google Scholar]
- Sethi, Y.; Patel, N.; Kaka, N.; Desai, A.; Kaiwan, O.; Sheth, M.; Sharma, R.; Huang, H.; Chopra, H.; Khandaker, M.U.; et al. Artificial Intelligence in Pediatric Cardiology: A Scoping Review. J. Clin. Med. 2022, 11, 7072. [Google Scholar] [CrossRef]
- Ahuja, A.S. The impact of artificial intelligence in medicine on the future role of the physician. PeerJ 2019, 7, e7702. [Google Scholar] [CrossRef]
- Chen, Z.; Liang, N.; Zhang, H.; Li, H.; Yang, Y.; Zong, X.; Chen, Y.; Wang, Y.; Shi, N. Harnessing the power of clinical decision support systems: Challenges and opportunities. Open Heart 2023, 10, e002432. [Google Scholar] [CrossRef]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Futur. Health J. 2019, 6, 94–98. [Google Scholar] [CrossRef]
- Ajami, S. Use of speech-to-text technology for documentation by healthcare providers. Natl. Med. J. India 2016, 29, 148–152. [Google Scholar]
- Pedro, A.R.; Dias, M.B.; Laranjo, L.; Cunha, A.S.; Cordeiro, J.V. Artificial intelligence in medicine: A comprehensive survey of medical doctor’s perspectives in Portugal. PLoS ONE 2023, 18, e0290613. [Google Scholar] [CrossRef]
- Bajwa, J.; Munir, U.; Nori, A.; Williams, B. Artificial intelligence in healthcare: Transforming the practice of medicine. Futur. Health J. 2021, 8, e188–e194. [Google Scholar] [CrossRef]
- Johnson, A.E.W.; Pollard, T.J.; Shen, L.; Lehman, L.-W.H.; Feng, M.; Ghassemi, M.; Moody, B.; Szolovits, P.; Celi, L.A.; Mark, R.G. MIMIC-III, a freely accessible critical care database. Sci. Data 2016, 3, 160035. [Google Scholar] [CrossRef]
- Staszak, K.; Tylkowski, B.; Staszak, M. From Data to Diagnosis: How Machine Learning Is Changing Heart Health Monitoring. Int. J. Environ. Res. Public Health 2023, 20, 4605. [Google Scholar] [CrossRef]
- Aziz, S.; Ahmed, S.; Alouini, M.-S. ECG-based machine-learning algorithms for heartbeat classification. Sci. Rep. 2021, 11, 1–14. [Google Scholar] [CrossRef]
- Karatzia, L.; Aung, N.; Aksentijevic, D. Artificial intelligence in cardiology: Hope for the future and power for the present. Front. Cardiovasc. Med. 2022, 9, 945726. [Google Scholar] [CrossRef]
- Rajkomar, A.; Oren, E.; Chen, K.; Dai, A.M.; Hajaj, N.; Hardt, M.; Liu, P.J.; Liu, X.; Marcus, J.; Sun, M.; et al. Scalable and accurate deep learning with electronic health records. NPJ Digit. Med. 2018, 1, 1–10. [Google Scholar] [CrossRef]
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. Can mobile health technologies transform health care? JAMA 2013, 310, 2395–2396. [Google Scholar] [CrossRef]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for success. NPJ Digit. Med. 2020, 3, 1–10. [Google Scholar] [CrossRef]
- Sim, I.; Gorman, P.; Greenes, R.A.; Haynes, R.B.; Kaplan, B.; Lehmann, H.; Tang, P.C. Clinical Decision Support Systems for the Practice of Evidence-based Medicine. J. Am. Med Informatics Assoc. 2001, 8, 527–534. [Google Scholar] [CrossRef]
- Wyatt, J.C. The Promises and Perils of Modelling Medical Reasoning. (Reflections on E.H. Shortliffe and B.G. Buchanan’s paper: A model of Inexact Reasoning in Medicine). Yearb. Med. Inform. 1999, 161–165. [Google Scholar] [CrossRef]
- Sittig, D.F.; Wright, A.; Middleton, B. Clinical Decision Support: A 25 Year Retrospective and a 25 Year Vision. Yearb. Med. Inform. 2016, 25, S103–S116. [Google Scholar] [CrossRef]
- Gore, J.C. Artificial intelligence in medical imaging. Magn. Reson. Imaging 2020, 68, A1–A4. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, K.; A Houlihan, C.; Balas, E.A.; Lobach, D.F. Improving clinical practice using clinical decision support systems: A systematic review of trials to identify features critical to success. BMJ 2005, 330, 765. [Google Scholar] [CrossRef] [PubMed]
- Islam, K.R.; Prithula, J.; Kumar, J.; Tan, T.L.; Reaz, M.B.I.; Sumon, S.I.; Chowdhury, M.E.H. Machine Learning-Based Early Prediction of Sepsis Using Electronic Health Records: A Systematic Review. J. Clin. Med. 2023, 12, 5658. [Google Scholar] [CrossRef]
- Mandair, D.; Tiwari, P.; Simon, S.; Colborn, K.L.; Rosenberg, M.A. Prediction of incident myocardial infarction using machine learning applied to harmonized electronic health record data. BMC Med. Informatics Decis. Mak. 2020, 20, 252. [Google Scholar] [CrossRef]
- Whiteson, H.Z.B.; Frishman, W.H. Artificial Intelligence in the Prevention and Detection of Cardiovascular Disease. Cardiol. Rev. 2023. [Google Scholar] [CrossRef]
- Stafie, C.S.; Sufaru, I.-G.; Ghiciuc, C.M.; Stafie, I.-I.; Sufaru, E.-C.; Solomon, S.M.; Hancianu, M. Exploring the Intersection of Artificial Intelligence and Clinical Healthcare: A Multidisciplinary Review. Diagnostics 2023, 13, 1995. [Google Scholar] [CrossRef] [PubMed]
- Uddin, S.; Khan, A.; Hossain, E.; Moni, M.A. Comparing different supervised machine learning algorithms for disease prediction. BMC Med. Inform. Decis. Mak. 2019, 19, 281. [Google Scholar] [CrossRef] [PubMed]
- Amann, J.; Vetter, D.; Blomberg, S.N.; Christensen, H.C.; Coffee, M.; Gerke, S.; Gilbert, T.K.; Hagendorff, T.; Holm, S.; Livne, M.; et al. To explain or not to explain?—Artificial intelligence explainability in clinical decision support systems. PLOS Digit. Health 2022, 1, e0000016. [Google Scholar] [CrossRef]
- Linardatos, P.; Papastefanopoulos, V.; Kotsiantis, S. Explainable AI: A Review of Machine Learning Interpretability Methods. Entropy 2020, 23, 18. [Google Scholar] [CrossRef]
- Hak, F.; Guimarães, T.; Santos, M. Towards effective clinical decision support systems: A systematic review. PLoS ONE 2022, 17, e0272846. [Google Scholar] [CrossRef]
- Akbar, S.; Lyell, D.; Magrabi, F. Automation in nursing decision support systems: A systematic review of effects on decision making, care delivery, and patient outcomes. J. Am. Med. Inform. Assoc. 2021, 28, 2502–2513. [Google Scholar] [CrossRef] [PubMed]
- Kopanitsa, G. Integration of Hospital Information and Clinical Decision Support Systems to Enable the Reuse of Electronic Health Record Data. Methods Inf. Med. 2017, 56, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Sacchi, L.; Lanzola, G.; Viani, N.; Quaglini, S. Personalization and Patient Involvement in Decision Support Systems: Current Trends. Yearb. Med. Inform. 2015, 24, 106–118. [Google Scholar] [CrossRef]
- Coiera, E.; Westbrook, J.; Wyatt, J. The safety and quality of decision support systems. Yearb. Med. Inform. 2006, 20–25. [Google Scholar]
- Payne, T.H. Computer decision support systems. Chest 2000, 118 (Suppl. S2), 47S–52S. [Google Scholar] [CrossRef]
- Lewkowicz, D.; Wohlbrandt, A.; Boettinger, E. Economic impact of clinical decision support interventions based on electronic health records. BMC Health Serv. Res. 2020, 20, 871. [Google Scholar] [CrossRef]
- Bezzina, C.R.; Lahrouchi, N.; Priori, S.G. Genetics of Sudden Cardiac Death. Circ. Res. 2015, 116, 1919–1936. [Google Scholar] [CrossRef] [PubMed]
- Jain, K.K. Personalized Management of Cardiovascular Disorders. Med. Princ. Pract. 2017, 26, 399–414. [Google Scholar] [CrossRef]
- Currie, G.; Delles, C. Precision Medicine and Personalized Medicine in Cardiovascular Disease. Adv. Exp. Med. Biol. 2018, 1065, 589–605. [Google Scholar]
- Shetty, M.K.; Kunal, S.; Girish, M.; Qamar, A.; Arora, S.; Hendrickson, M.; Mohanan, P.P.; Gupta, P.; Ramakrishnan, S.; Yadav, R.; et al. Machine learning based model for risk prediction after ST-Elevation myocardial infarction: Insights from the North India ST elevation myocardial infarction (NORIN-STEMI) registry. Int. J. Cardiol. 2022, 362, 6–13. [Google Scholar] [CrossRef]
- Bai, Z.; Lu, J.; Li, T.; Ma, Y.; Liu, Z.; Zhao, R.; Wang, Z.; Shi, B. Clinical Feature-Based Machine Learning Model for 1-Year Mortality Risk Prediction of ST-Segment Elevation Myocardial Infarction in Patients with Hyperuricemia: A Retrospective Study. Comput. Math. Methods Med. 2021, 2021, 7252280. [Google Scholar] [CrossRef]
- Backhaus, S.J.; Aldehayat, H.; Kowallick, J.T.; Evertz, R.; Lange, T.; Kutty, S.; Bigalke, B.; Gutberlet, M.; Hasenfuß, G.; Thiele, H.; et al. Artificial intelligence fully automated myocardial strain quantification for risk stratification following acute myocardial infarction. Sci. Rep. 2022, 12, 12220. [Google Scholar] [CrossRef]
- Nagarajan, V.D.; Lee, S.-L.; Robertus, J.-L.; A Nienaber, C.; A Trayanova, N.; Ernst, S. Artificial intelligence in the diagnosis and management of arrhythmias. Eur. Heart J. 2021, 42, 3904–3916. [Google Scholar] [CrossRef] [PubMed]
- Wolterink, J.M.; Leiner, T.; de Vos, B.D.; Coatrieux, J.-L.; Kelm, B.M.; Kondo, S.; Salgado, R.A.; Shahzad, R.; Shu, H.; Snoeren, M.; et al. An evaluation of automatic coronary artery calcium scoring methods with cardiac CT using the orCaScore framework. Med. Phys. 2016, 43, 2361–2373. [Google Scholar] [CrossRef] [PubMed]
- Wolterink, J.M.; Leiner, T.; de Vos, B.D.; van Hamersvelt, R.W.; Viergever, M.A.; Išgum, I. Automatic coronary artery calcium scoring in cardiac CT angiography using paired convolutional neural networks. Med. Image Anal. 2016, 34, 123–136. [Google Scholar] [CrossRef] [PubMed]
- van Smeden, M.; Reitsma, J.B.; Riley, R.D.; Collins, G.S.; Moons, K.G. Clinical prediction models: Diagnosis versus prognosis. J. Clin. Epidemiology 2021, 132, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Wannamethee, S.G.; Shaper, A.G.; Lennon, L.; Morris, R.W. Metabolic Syndrome vs Framingham Risk Score for Prediction of Coronary Heart Disease, Stroke, and Type 2 Diabetes Mellitus. Arch. Intern. Med. 2005, 165, 2644–2650. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.F.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef]
- Motwani, M.; Dey, D.; Berman, D.S.; Germano, G.; Achenbach, S.; Al-Mallah, M.H.; Andreini, D.; Budoff, M.J.; Cademartiri, F.; Callister, T.Q.; et al. Machine learning for prediction of all-cause mortality in patients with suspected coronary artery disease: A 5-year multicentre prospective registry analysis. Eur. Heart J. 2016, 38, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Javaid, A.; Zghyer, F.; Kim, C.; Spaulding, E.M.; Isakadze, N.; Ding, J.; Kargillis, D.; Gao, Y.; Rahman, F.; Brown, D.E.; et al. Medicine 2032: The future of cardiovascular disease prevention with machine learning and digital health technology. Am. J. Prev. Cardiol. 2022, 12, 100379. [Google Scholar] [CrossRef]
- Van Mens, K.; Lokkerbol, J.; Wijnen, B.; Janssen, R.; de Lange, R.; Tiemens, B. Predicting Undesired Treatment Outcomes With Machine Learning in Mental Health Care: Multisite Study. Psychopharmacol. 2023, 11, e44322. [Google Scholar] [CrossRef] [PubMed]
- Hassan, N.; Slight, R.; Morgan, G.; Bates, D.W.; Gallier, S.; Sapey, E.; Slight, S. Road map for clinicians to develop and evaluate AI predictive models to inform clinical decision-making. BMJ Health Care Informatics 2023, 30, e100784. [Google Scholar] [CrossRef] [PubMed]
- Norori, N.; Hu, Q.; Aellen, F.M.; Faraci, F.D.; Tzovara, A. Addressing bias in big data and AI for health care: A call for open science. Patterns 2021, 2, 100347. [Google Scholar] [CrossRef] [PubMed]
- Busnatu, S.; Niculescu, A.-G.; Bolocan, A.; Petrescu, G.E.D.; Păduraru, D.N.; Năstasă, I.; Lupușoru, M.; Geantă, M.; Andronic, O.; Grumezescu, A.M.; et al. Clinical Applications of Artificial Intelligence—An Updated Overview. J. Clin. Med. 2022, 11, 2265. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.J.; Karthikesalingam, A.; Suleyman, M.; Corrado, G.; King, D. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019, 17, 195. [Google Scholar] [CrossRef] [PubMed]
- Naik, N.; Hameed, B.M.Z.; Shetty, D.K.; Swain, D.; Shah, M.; Paul, R.; Aggarwal, K.; Ibrahim, S.; Patil, V.; Smriti, K.; et al. Legal and Ethical Consideration in Artificial Intelligence in Healthcare: Who Takes Responsibility? Front. Surg. 2022, 9, 862322. [Google Scholar] [CrossRef]
- Farhud, D.D.; Zokaei, S. Ethical Issues of Artificial Intelligence in Medicine and Healthcare. Iran. J. Public Health 2021, 50, I–V. [Google Scholar] [CrossRef]
- Makimoto, H.; Kohro, T. Adopting artificial intelligence in cardiovascular medicine: A scoping review. Hypertens. Res. 2023, 685–699. [Google Scholar] [CrossRef] [PubMed]
- Khanna, N.N.; Maindarkar, M.A.; Viswanathan, V.; E Fernandes, J.F.; Paul, S.; Bhagawati, M.; Ahluwalia, P.; Ruzsa, Z.; Sharma, A.; Kolluri, R.; et al. Economics of Artificial Intelligence in Healthcare: Diagnosis vs. Treatment. Healthcare 2022, 10, 2493. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Luo, B.; Zhao, C.; Zhang, H. Artificial intelligence healthcare service resources adoption by medical institutions based on TOE framework. Digit. Health 2022, 8, 20552076221126034. [Google Scholar] [CrossRef] [PubMed]
- Vandenberk, B.; Chew, D.S.; Prasana, D.; Gupta, S.; Exner, D.V. Successes and challenges of artificial intelligence in cardiology. Front. Digit. Health 2023, 5, 1201392. [Google Scholar] [CrossRef] [PubMed]
- Koulaouzidis, G.; Jadczyk, T.; Iakovidis, D.K.; Koulaouzidis, A.; Bisnaire, M.; Charisopoulou, D. Artificial Intelligence in Cardiology—A Narrative Review of Current Status. J. Clin. Med. 2022, 11, 3910. [Google Scholar] [CrossRef] [PubMed]
- Nazer, L.H.; Zatarah, R.; Waldrip, S.; Ke, J.X.C.; Moukheiber, M.; Khanna, A.K.; Hicklen, R.S.; Moukheiber, L.; Moukheiber, D.; Ma, H.; et al. Bias in artificial intelligence algorithms and recommendations for mitigation. PLOS Digit. Health 2023, 2, e0000278. [Google Scholar] [CrossRef] [PubMed]
- Panch, T.; Mattie, H.; Atun, R. Artificial intelligence and algorithmic bias: Implications for health systems. J. Glob. Health 2019, 9, 010318. [Google Scholar] [CrossRef]
- Khan, B.; Fatima, H.; Qureshi, A.; Kumar, S.; Hanan, A.; Hussain, J.; Abdullah, S. Drawbacks of Artificial Intelligence and Their Potential Solutions in the Healthcare Sector. Biomed. Mater. Devices 2023, 1, 731–738. [Google Scholar] [CrossRef]
- Choudhury, A.; Asan, O. Role of Artificial Intelligence in Patient Safety Outcomes: Systematic Literature Review. Psychopharmacology 2020, 8, e18599. [Google Scholar] [CrossRef]

| Study | AI Application | Diagnostic Modality | Performance Metrics | Future Considerations |
|---|---|---|---|---|
| [27] | Deep neural networks for ECG analysis | ECG | AUC: 0.97 and F1 score: 0.837 | Interpretability and collaboration between AI systems and clinical expertise |
| [28] | AI-enabled ECG for atrial fibrillation prediction | Wearable ECG monitors | AUC: 0.87, sensitivity: 79%, specificity: 79.5%, and accuracy: 79.4% | Considerations for undetected atrial fibrillation and prospective calibration before widespread application to a broader population |
| [33] | AI in coronary angiography and TAVR | Coronary angiography and TAVR | Procedure time and complication rate reduction | Enhancing AI algorithms’ adaptability to diverse procedural scenarios |
| Study | AI Application | CDSS in Clinical Settings | Performance Metrics | Future Considerations |
|---|---|---|---|---|
| [55] | AI-driven CDSS in clinical practice | Real-time recommendations based on patient data | 68% improvement in clinical practice | Disparity in assessing various AI-driven CDSS models |
| [56] | AI-driven CDSS for sepsis prediction | Predicting sepsis outcomes | Potential in early sepsis detection | Challenges in EHR data quality and standardization Prospective validation studies for clinical impact assessment. |
| [57] | AI-driven CDSS for myocardial infarction prediction | Predicting myocardial infarction outcomes | Moderate improvement over traditional methods; F1 Score: 0.092 and AUC: 0.835 | Calibration challenges due to overfitting from low-event frequency Adequate discrimination despite poor calibration |
| Study | Focus Area | Machine Learning Application | Performance Metrics | Future Considerations |
|---|---|---|---|---|
| [73] | Risk prediction in resource-limited countries | STEMI | Improved mortality prediction following STEMI Extra Tree ML model demonstrated best predictive ability (sensitivity: 85%, AUC: 79.7%, and accuracy: 75%) | Clinical applicability Generalizability across diverse patient populations Reducing biases in training data |
| [75] | Automated volume-derived cardiac functional evaluation | CMR imaging and automated strain assessment | GLS and GCS best predicted MACE with high accuracy | Time-consuming post-processing Validation in broader populations |
| [77] | (Semi)Automatic CAC identification in cardiac CT | Cardiac CT and automated CAC scoring | 1. Detection of 52% to 94% of CAC lesions. Positive predictive values between 65% and 96%. 2. Linearly weighted Cohen’s kappa for patient CVD risk categorization ranged from 0.80 to 1.00. | Missed lesions in distal coronary arteries False positive errors near coronary ostia Challenges in ambiguous locations |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gala, D.; Behl, H.; Shah, M.; Makaryus, A.N. The Role of Artificial Intelligence in Improving Patient Outcomes and Future of Healthcare Delivery in Cardiology: A Narrative Review of the Literature. Healthcare 2024, 12, 481. https://doi.org/10.3390/healthcare12040481
Gala D, Behl H, Shah M, Makaryus AN. The Role of Artificial Intelligence in Improving Patient Outcomes and Future of Healthcare Delivery in Cardiology: A Narrative Review of the Literature. Healthcare. 2024; 12(4):481. https://doi.org/10.3390/healthcare12040481
Chicago/Turabian StyleGala, Dhir, Haditya Behl, Mili Shah, and Amgad N. Makaryus. 2024. "The Role of Artificial Intelligence in Improving Patient Outcomes and Future of Healthcare Delivery in Cardiology: A Narrative Review of the Literature" Healthcare 12, no. 4: 481. https://doi.org/10.3390/healthcare12040481
APA StyleGala, D., Behl, H., Shah, M., & Makaryus, A. N. (2024). The Role of Artificial Intelligence in Improving Patient Outcomes and Future of Healthcare Delivery in Cardiology: A Narrative Review of the Literature. Healthcare, 12(4), 481. https://doi.org/10.3390/healthcare12040481








