The Effects of Soft-Tissue Techniques and Exercise in the Treatment of Patellar Tendinopathy—Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Sources and Search
2.3. Study Selection Process and Eligibility Criteria
2.4. Data Extraction
2.5. Risk-of-Bias and Methodological Quality Assessment
2.6. Strength of Evidence
2.7. Statistical Analysis
3. Results
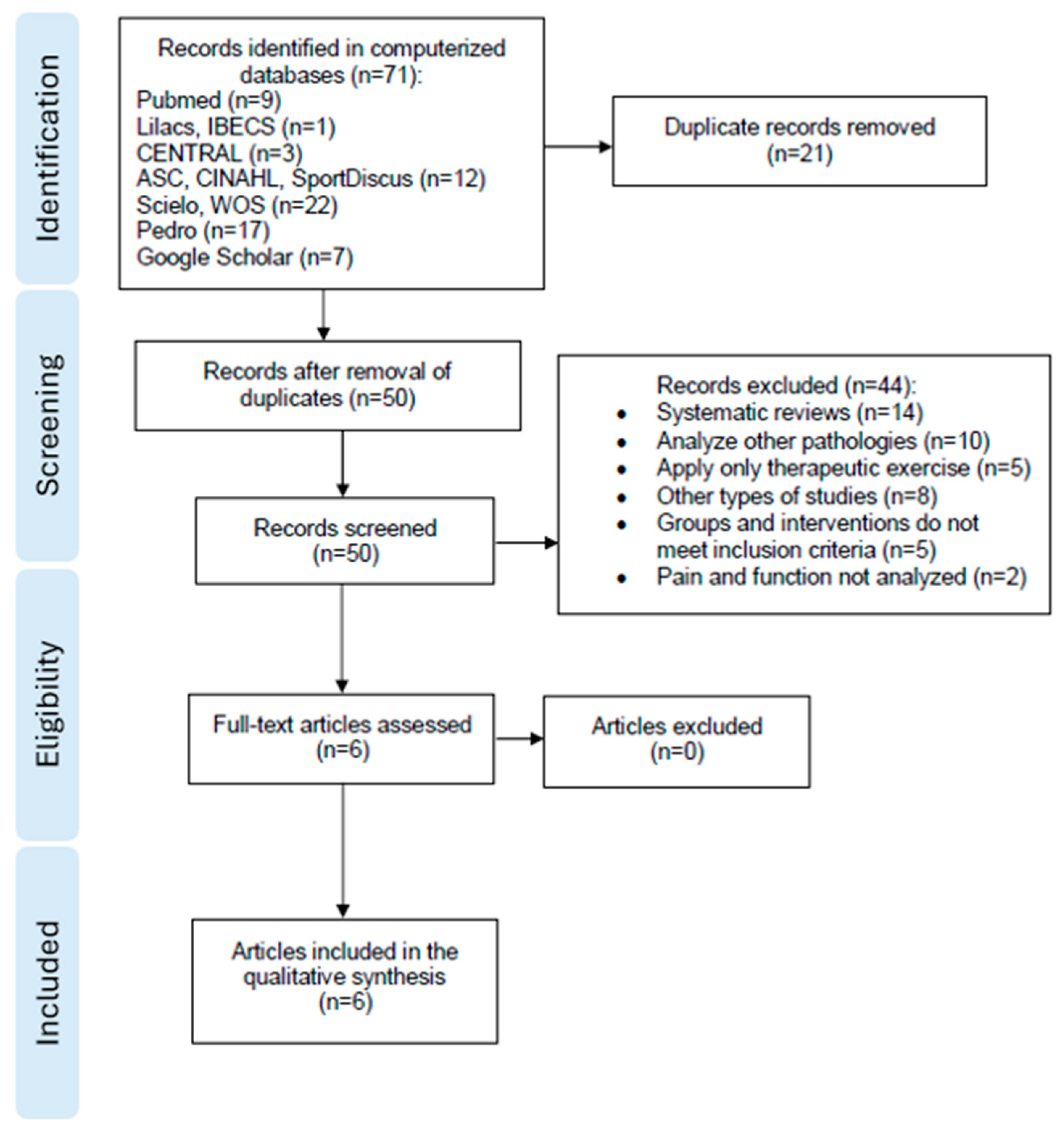
3.1. Study Selection
3.2. Quality and Risk of Bias
3.3. Participants
3.4. Quality of Evidence
3.5. Characteristics of the Intervention
3.5.1. Therapeutic Exercise
3.5.2. Soft-Tissue Techniques
3.5.3. Frequency and Duration of Intervention
3.6. Effectiveness of the Intervention
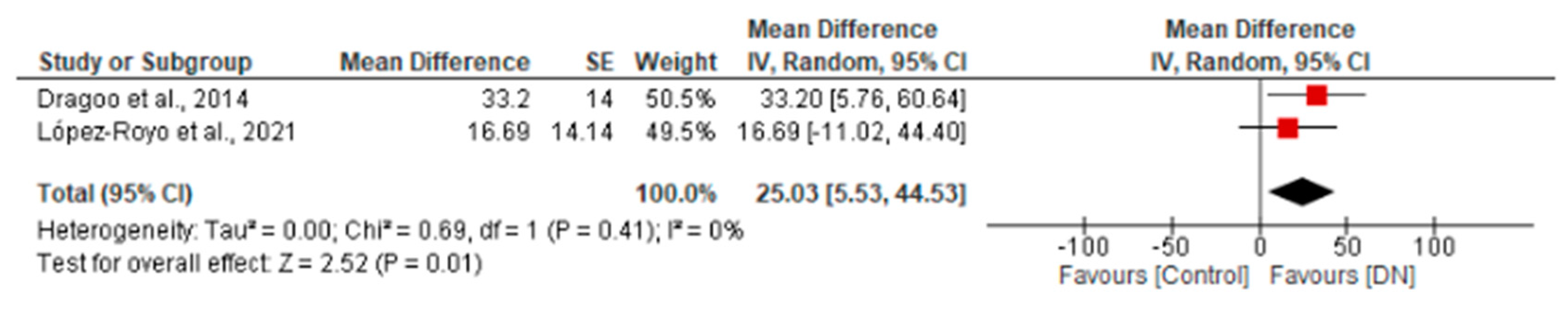
3.6.1. Severity of Symptoms
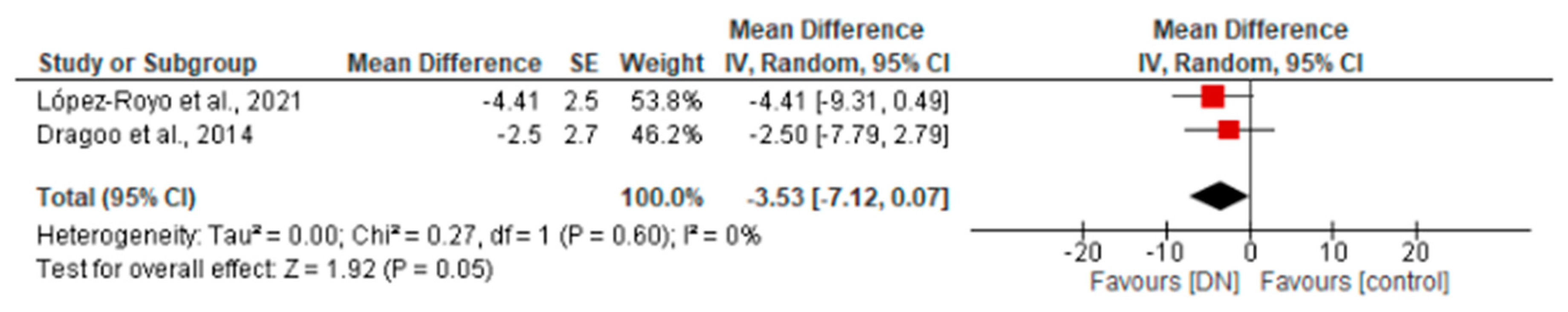
3.6.2. Pain Intensity
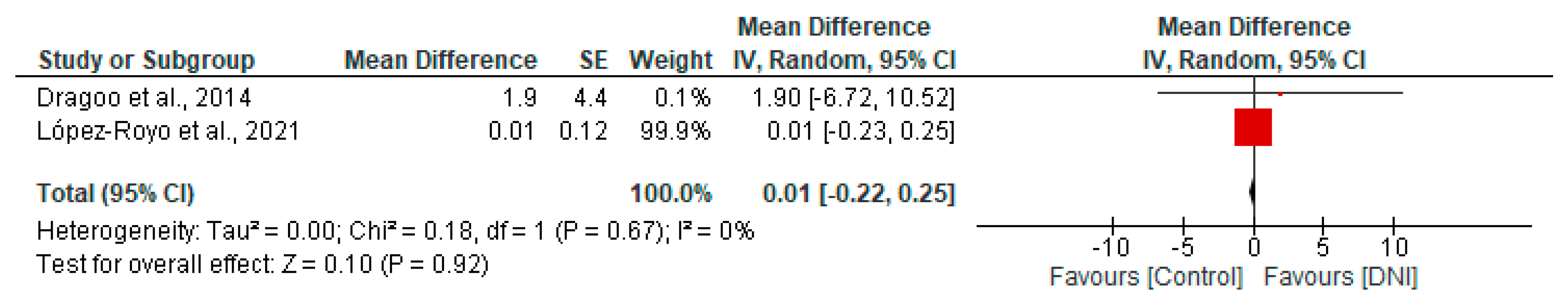
3.6.3. Quality of Life
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scott, A.; Squier, K.; Alfredson, H.; Bahr, R.; Cook, J.L.; Coombes, B.; de Vos, R.-J.; Fu, S.N.; Grimaldi, A.; Lewis, J.S.; et al. ICON 2019: International scientific tendinopathy symposium consensus: Clinical terminology. Br. J. Sports Med. 2020, 54, 260–262. [Google Scholar] [CrossRef]
- King, D.; Yakubek, G.; Chughtai, M.; Khlopas, A.; Saluan, P.; Mont, M.A.; Genin, J. Quadriceps tendinopathy: A review-part 1: Epidemiology and diagnosis. Ann. Transl. Med. 2019, 7, 71. [Google Scholar] [CrossRef]
- Hutchison, M.K.; Houck, J.; Cuddeford, T.; Dorociak, R.; Brumitt, J. Prevalence of patellar tendinopathy and patellar tendon abnormality in male collegiate basketball players: A cross-sectional study. J. Athl. Train. 2019, 54, 953–958. [Google Scholar] [CrossRef] [PubMed]
- Lian, O.B.; Engebretsen, L.; Bahr, R. Prevalence of jumper’s knee among elite athletes from different sports: A cross-sectional study. Am. J. Sports Med. 2005, 33, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Zwerver, J.; Bredeweg, S.W.; van den Akker-Scheek, I. Prevalence of Jumper’s knee among nonelite athletes from different sports: A cross-sectional survey: A cross-sectional survey. Am. J. Sports Med. 2011, 39, 1984–1988. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Rittweger, J.; Garau, G.; Radonic, B.; Gutwasser, C.; Gilliver, S.F.; Kusy, K.; Zieliński, J.; Felsenberg, D.; Maffulli, N. Patellar tendinopathy in master track and field athletes: Influence of impact profile, weight, height, age and gender. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Kettunen, J.A.; Kvist, M.; Alanen, E.; Kujala, U.M. Long-term prognosis for jumper’s knee in male athletes. A prospective follow-up study. Am. J. Sports Med. 2002, 30, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Cassel, M.; Risch, L.; Intziegianni, K.; Mueller, J.; Stoll, J.; Brecht, P.; Mayer, F. Incidence of Achilles and patellar tendinopathy in adolescent elite athletes. Int. J. Sports Med. 2018, 39, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Tayfur, A.; Haque, A.; Salles, J.I.; Malliaras, P.; Screen, H.; Morrissey, D. Are landing patterns in jumping athletes associated with patellar tendinopathy? A systematic review with evidence gap map and meta-analysis. Sports Med. 2022, 52, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, T.B.; Pizzari, T.; Kinsella, R.; Hope, D.; Cook, J.L. Current trends in tendinopathy management. Best Pract. Res. Clin. Rheumatol. 2019, 33, 122–140. [Google Scholar] [CrossRef]
- Mendonça, L.D.; Ocarino, J.M.; Bittencourt, N.F.N.; Macedo, L.G.; Fonseca, S.T. Association of hip and foot factors with patellar tendinopathy (jumper’s knee) in athletes. J. Orthop. Sports Phys. Ther. 2018, 48, 676–684. [Google Scholar] [CrossRef]
- Sprague, A.L.; Smith, A.H.; Knox, P.; Pohlig, R.T.; Grävare Silbernagel, K. Modifiable risk factors for patellar tendinopathy in athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1575–1585. [Google Scholar] [CrossRef] [PubMed]
- Morgan, S.; Janse van Vuuren, E.C.; Coetzee, F.F. Causative factors and rehabilitation of patellar tendinopathy: A systematic review. S. Afr. J. Physiother. 2016, 72, 338. [Google Scholar] [CrossRef] [PubMed]
- Gaida, J.E.; Cook, J. Treatment options for patellar tendinopathy: Critical review. Curr. Sports Med. Rep. 2011, 10, 255–270. [Google Scholar] [CrossRef] [PubMed]
- Stenroth, L.; Sefa, S.; Arokoski, J.; Töyräs, J. Does magnetic resonance imaging provide superior reliability for Achilles and patellar tendon cross-sectional area measurements compared with ultrasound imaging? Ultrasound Med. Biol. 2019, 45, 3186–3198. [Google Scholar] [CrossRef] [PubMed]
- Young, M.A.; Cook, J.L.; Purdam, C.R.; Kiss, Z.S.; Alfredson, H. Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br. J. Sports Med. 2005, 39, 102–105. [Google Scholar] [CrossRef]
- Couppé, C.; Svensson, R.B.; Silbernagel, K.G.; Langberg, H.; Magnusson, S.P. Eccentric or concentric exercises for the treatment of tendinopathies? J. Orthop. Sports Phys. Ther. 2015, 45, 853–863. [Google Scholar] [CrossRef]
- Willy, R.W.; Hoglund, L.T.; Barton, C.J.; Bolgla, L.A.; Scalzitti, D.A.; Logerstedt, D.S.; Lynch, A.D.; Snyder-Mackler, L.; McDonough, C.M. Patellofemoral pain: Clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American physical therapy association. J. Orthop. Sports Phys. Ther. 2019, 49, CPG1–CPG95. [Google Scholar] [CrossRef]
- Patellofemoral pain: Using the evidence to guide physical therapist practice. J. Orthop. Sports Phys. Ther. 2019, 49, 631–632. [CrossRef]
- Louwerens, J.K.G.; Sierevelt, I.N.; van Noort, A.; van den Bekerom, M.P.J. Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: A systematic review and meta-analysis. J. Shoulder Elb. Surg. 2014, 23, 1240–1249. [Google Scholar] [CrossRef]
- López-Royo, M.P.; Ríos-Díaz, J.; Galán-Díaz, R.M.; Herrero, P.; Gómez-Trullén, E.M. A Comparative Study of Treatment Interventions for Patellar Tendinopathy: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2021, 102, 967–975. [Google Scholar] [CrossRef] [PubMed]
- Irby, A.; Gutierrez, J.; Chamberlin, C.; Thomas, S.J.; Rosen, A.B. Clinical management of tendinopathy: A systematic review of systematic reviews evaluating the effectiveness of tendinopathy treatments. Scand. J. Med. Sci. Sports 2020, 30, 1810–1826. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.S.; Cole, D.; Sojka, J.H.; Higgins, J.D.; Magnussen, R.A.; Schmitt, L.C.; Flanigan, D.C. Treatment options for patellar tendinopathy: A systematic review. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 861–872. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, U.S.; Raja, R.; Sarala, S.R.; Sharath, U.R. A study to compare the efficacy of transverse friction massage versus cryotherapy with eccentric training on decline board in chronic patellar tendinopathy in volleyball and basketball players. Int. J. Appl. Health Sci. 2014, 1, 23–29. [Google Scholar]
- Dimitrios, S.; Pantelis, M.; Kalliopi, S. Comparing the effects of eccentric training with eccentric training and static stretching exercises in the treatment of patellar tendinopathy. A controlled clinical trial. Clin. Rehabil. 2012, 26, 423–430. [Google Scholar] [CrossRef]
- Stasinopoulos, D.; Stasinopoulos, I. Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin. Rehabil. 2004, 18, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Sanchez, S.; Hidalgo, M.D.; Gomez, A. Responsiveness of the VISA-P scale for patellar tendinopathy in athletes. Br. J. Sports Med. 2014, 48, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Escala PEDro-Español—Google Search. (s/f). Google.com. Available online: https://www.google.com/search?q=Escala+PEDro-Espa%C3%B1ol&oq=Escala+PEDro-Espa%C3%B1ol&aqs=chrome..69i57j69i64l2.145038j0j15&sourceid=chrome&ie=UTF-8 (accessed on 5 June 2023).
- Higgins, J.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions, 1st ed.; Higgins, J., Green, S., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2011; Available online: https://training.cochrane.org/handbook (accessed on 5 June 2023).
- Aguayo-Albasini, J.L.; Flores-Pastor, B.; Soria-Aledo, V. GRADE system: Classification of quality of evidence and strength of recommendation. Cirugía Española 2014, 92, 82–88. [Google Scholar] [CrossRef]
- Dragoo, J.L.; Wasterlain, A.S.; Braun, H.J.; Nead, K.T. Platelet-rich plasma as a treatment for patellar tendinopathy: A double-blind, randomized controlled trial: A double-blind, randomized controlled trial. Am. J. Sports Med. 2014, 42, 610–618. [Google Scholar] [CrossRef]
- Abat, F.; Sánchez-Sánchez, J.L.; Martín-Nogueras, A.M.; Calvo-Arenillas, J.I.; Yajeya, J.; Méndez-Sánchez, R.; Monllau, J.C.; Gelber, P.E. Randomized controlled trial comparing the effectiveness of the ultrasound-guided galvanic electrolysis technique (USGET) versus conventional electro-physiotherapeutic treatment on patellar tendinopathy. J. Exp. Orthop. 2016, 3, 34. [Google Scholar] [CrossRef]
- Sharif, F.; Ahmad, A.; Gilani, S.A. Effectiveness of ultrasound guided dry needling in management of jumper’s knee: A randomized controlled trial. Sci. Rep. 2023, 13, 4736. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.J.; Ng, G.Y.-F.; Lee, W.C.; Fu, S.N. Changes in morphological and elastic properties of patellar tendon in athletes with unilateral patellar tendinopathy and their relationships with pain and functional disability. PLoS ONE 2014, 9, e108337. [Google Scholar] [CrossRef] [PubMed]
- Pedrelli, A.; Stecco, C.; Day, J.A. Treating patellar tendinopathy with Fascial Manipulation. J. Bodyw. Mov. Ther. 2009, 13, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Cadellans-Arróniz, A.; Llurda-Almuzara, L.; Campos-Laredo, B.; Cabanas-Valdés, R.; Garcia-Sutil, A.; López-de-Celis, C. The effectiveness of diacutaneous fibrolysis on pain, range of motion and functionality in musculoskeletal disorders: A systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 481–491. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Khan, K.M.; Harcourt, P.R.; Grant, M.; Young, D.A.; Bonar, S.F. A cross sectional study of 100 athletes with jumper’s knee managed conservatively and surgically. The Victorian Institute of Sport Tendon Study Group. Br. J. Sports Med. 1997, 31, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Vetrano, M.; Castorina, A.; Vulpiani, M.C.; Baldini, R.; Pavan, A.; Ferretti, A. Platelet-rich plasma versus focused shock waves in the treatment of jumper’s knee in athletes. Am. J. Sports Med. 2013, 41, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Abat, F.D.W.; Gelber, P.E.; Polidori, F.; Monllau, J.C.; Sanchez-Ibañez, J.M. Effectiveness of the Intratissue Percutaneous Electrolysis (EPI®) technique and isoinertial eccentric exercise in the treatment of patellar tendinopathy at two years follow-up. Muscles Ligaments Tendons J. 2014, 14, 188–193. [Google Scholar] [CrossRef]
- de la Cruz Torres, B.; Albornoz Cabello, M.; García Bermejo, P.; Naranjo Orellana, J. Autonomic responses to ultrasound-guided percutaneous needle electrolysis of the patellar tendon in healthy male footballers. Acupunct. Med. J. Br. Med. Acupunct. Soc. 2016, 34, 275–279. [Google Scholar] [CrossRef]
- Abat, F.; Gelber, P.E.; Polidori, F.; Monllau, J.C.; Sanchez-Ibañez, J.M. Clinical results after ultrasound guided intratissue percutaneous electrolysis (EPI) and eccentric exercise in the treatment of patellar tendinopathy. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Palazón-Bru, A.; Tomás Rodríguez, M.I.; Mares-García, E.; Hernández-Sánchez, S.; Carbonell-Torregrosa, M.Á.; Gil-Guillén, V.F. The Victorian institute of sport assessment scale for patellar tendinopathy (VISA-P): A reliability generalization meta-analysis: A reliability generalization meta-analysis. Clin. J. Sport Med. 2021, 31, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Connell, D.; Datir, A.; Alyas, F.; Curtis, M. Treatment of lateral epicondylitis using skin-derived tenocyte-like cells. Br. J. Sports Med. 2009, 43, 293–298. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ragone, F.; Pérez-Guillén, S.; Carrasco-Uribarren, A.; Cabanillas-Barea, S.; Ceballos-Laita, L.; Rodríguez-Rubio, P.R.; Cabanas-Valdés, R. The Effects of Soft-Tissue Techniques and Exercise in the Treatment of Patellar Tendinopathy—Systematic Review and Meta-Analysis. Healthcare 2024, 12, 427. https://doi.org/10.3390/healthcare12040427
Ragone F, Pérez-Guillén S, Carrasco-Uribarren A, Cabanillas-Barea S, Ceballos-Laita L, Rodríguez-Rubio PR, Cabanas-Valdés R. The Effects of Soft-Tissue Techniques and Exercise in the Treatment of Patellar Tendinopathy—Systematic Review and Meta-Analysis. Healthcare. 2024; 12(4):427. https://doi.org/10.3390/healthcare12040427
Chicago/Turabian StyleRagone, Federico, Silvia Pérez-Guillén, Andoni Carrasco-Uribarren, Sara Cabanillas-Barea, Luis Ceballos-Laita, Pere Ramón Rodríguez-Rubio, and Rosa Cabanas-Valdés. 2024. "The Effects of Soft-Tissue Techniques and Exercise in the Treatment of Patellar Tendinopathy—Systematic Review and Meta-Analysis" Healthcare 12, no. 4: 427. https://doi.org/10.3390/healthcare12040427
APA StyleRagone, F., Pérez-Guillén, S., Carrasco-Uribarren, A., Cabanillas-Barea, S., Ceballos-Laita, L., Rodríguez-Rubio, P. R., & Cabanas-Valdés, R. (2024). The Effects of Soft-Tissue Techniques and Exercise in the Treatment of Patellar Tendinopathy—Systematic Review and Meta-Analysis. Healthcare, 12(4), 427. https://doi.org/10.3390/healthcare12040427