Reliability, Knowledge Translation, and Implementability of the Spanish Version of the Hammersmith Infant Neurological Examination
Abstract
1. Introduction
2. Materials and Methods
2.1. Description of HINE
2.2. Cross-Cultural Translation and Adaptation
2.3. Participants
2.4. Evaluation of Intra- and Inter-Examiner Reliability
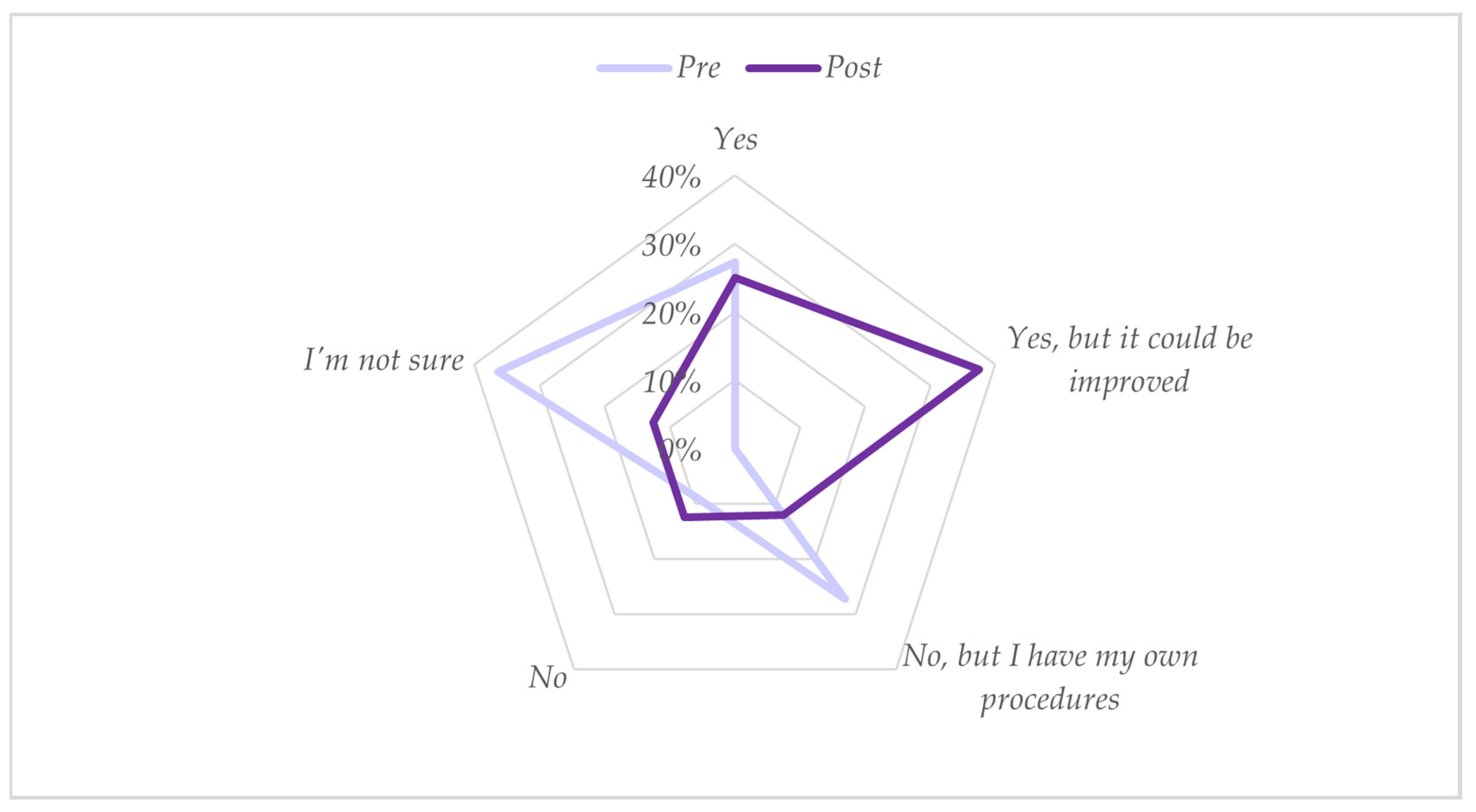
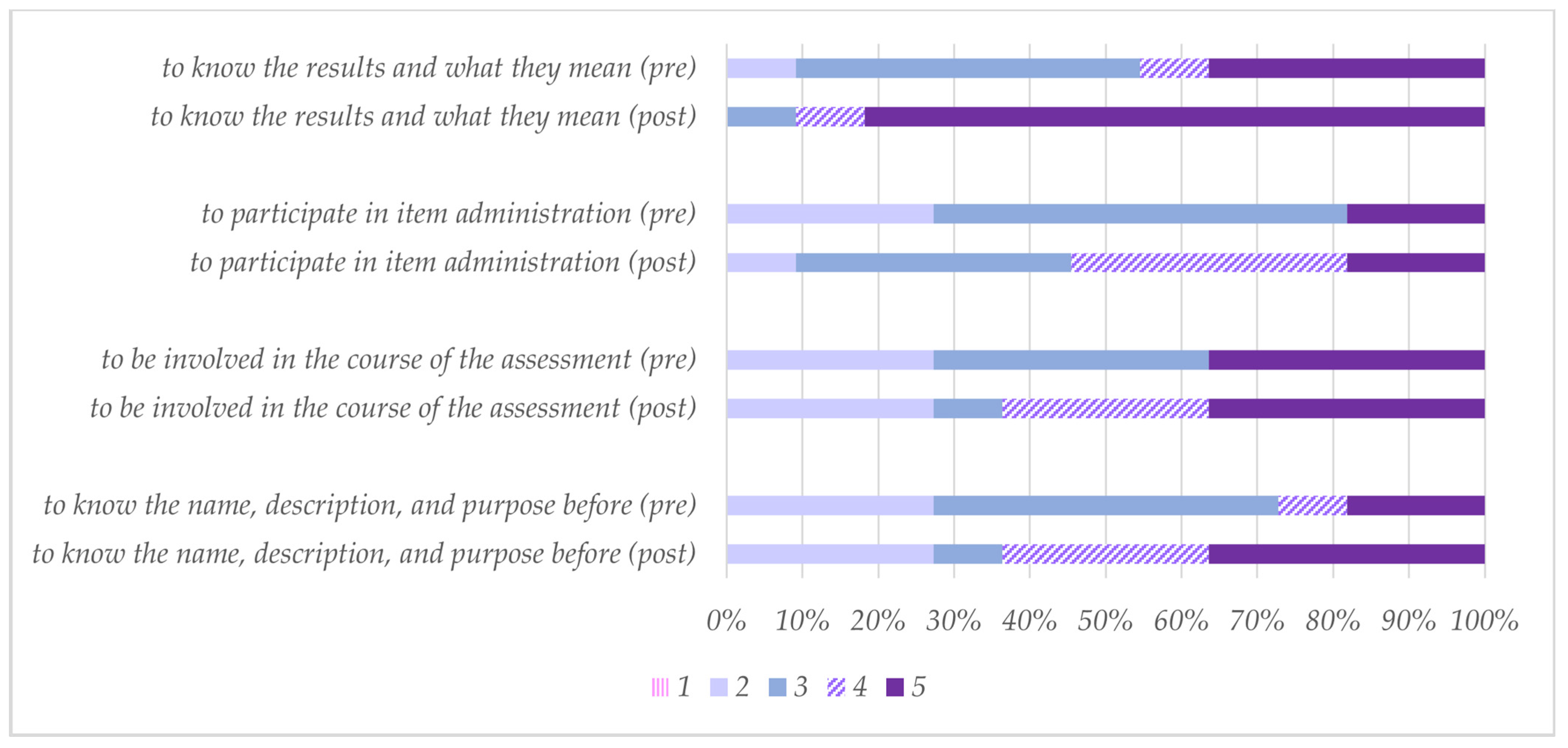
2.5. Training Program and Development of the Recommendation Guidelines for Evaluation with HINE in Spanish
2.6. Statistical Analysis
3. Results
3.1. Cross-Cultural Translation and Adaptation
3.2. Participants
3.3. Evaluation of Intra- and Inter-Examiner Reliability
3.4. Evaluation of Implementation and Inter-Examiner Reliability One Year after the Training Program
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McIntyre, S.; Goldsmith, S.; Webb, A.; Ehlinger, V.; Hollung, S.J.; McConnell, K.; Arnaud, C.; Smithers-Sheedy, H.; Oskoui, M.; Khandaker, G.; et al. Global prevalence of cerebral palsy: A systematic analysis. Dev. Med. Child Neurol. 2022, 64, 1494–1506. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Conesa, A.; Suarez-Serrano, C. Parálisis cerebral infantil. Panorama de su prevalencia en España. Fisioterapia 2017, 39, 185–186. [Google Scholar] [CrossRef]
- Cancho Candela, R.; Fernández Alonso, J.E.; Lanza Fernández, E.; Lozano Domínguez, M.A.; Andrés De Llano, J.M.; Folgado Toranzo, I. Estimación de la prevalencia de parálisis cerebral en la comunidad de Castilla y León mediante el registro de minusvalías. An. Pediatr. 2006, 65, 97–100. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.-C.; et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Monica, T.; Catherine, M.; Iona, N. New Screening Tool for Term-Born Infants Enables Update to the Clinical Practice Guideline for Early Diagnosis of Cerebral Palsy. JAMA Pediatr. 2023, 177, 115–117. [Google Scholar] [CrossRef] [PubMed]
- Maitre, N.L.; Byrne, R.; Duncan, A.; Dusing, S.; Gaebler-Spira, D.; Rosenbaum, P.; CP EDI Consensus Group. High-risk for cerebral palsy” designation: A clinical consensus statement. J. Pediatr. Rehabil. Med. 2022, 15, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Maitre, N.L.; Chorna, O.; Romeo, D.M.; Guzzetta, A. Implementation of the Hammersmith Infant Neurological Exam in a High-Risk Infant Follow-Up Program. Pediatr. Neurology 2016, 65, 31–38. [Google Scholar] [CrossRef]
- Romeo, D.M.; Ricci, D.; Brogna, C.; Mercuri, E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: A critical review of the literature. Dev. Med. Child Neurol. 2015, 58, 240–245. [Google Scholar] [CrossRef]
- Morgan, C.; Romeo, D.M.; Chorna, O.; Novak, I.; Galea, C.; Del Secco, S.; Guzzetta, A. The Pooled Diagnostic Accuracy of Neuroimaging, General Movements, and Neurological Examination for Diagnosing Cerebral Palsy Early in High-Risk Infants: A Case Control Study. J. Clin. Med. 2019, 8, 1879. [Google Scholar] [CrossRef]
- Haataja, L.; Mercuri, E.; Regev, R.; Cowan, F.; Rutherford, M.; Dubowitz, V.; Dubowitz, L. Optimality score for the neurologic examination of the infant at 12 and 18 months of age. J. Pediatr. 1999, 135 Pt 1, 153–161. [Google Scholar] [CrossRef]
- Tedla, J.S.; Bajaj, A.; Joshua, A.; Kamath, G. Psychometric Properties of Hammersmith Infant Neurological Examination in 12 Months Old High-Risk Infants: A Cross Sectional Study. Indian J. Physiother. Occup. Ther. Int. J. 2014, 8, 169–177. [Google Scholar] [CrossRef]
- Adıgüzel, H.; Sarıkabadayı, Y.Ü.; Apaydın, U.; Kırmacı, Z.İ.K.; Gücüyener, K.; Karadeniz, P.G.; Elbasan, B. Turkish Validity and Reliability of the Hammersmith Infant Neurological Examination (HINE) with High-Risk Infant Group: A Preliminary Study. Turk. Arch. Pediatr. 2022, 57, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Harpster, K.; Merhar, S.; Priyanka Illapani, V.S.; Peyton, C.; Kline-Fath, B.; Parikh, N.A. Associations Between Early Structural Magnetic Resonance Imaging, Hammersmith Infant Neurological Examination, and General Movements Assessment in Infants Born Very Preterm. J. Pediatr. 2021, 232, 80–86.e2. [Google Scholar] [CrossRef] [PubMed]
- Romeo, D.M.; Apicella, M.; Velli, C.; Brogna, C.; Ricci, D.; Pede, E.; Sini, F.; Coratti, G.; Gallini, F.; Cota, F.; et al. Hammersmith Infant Neurological Examination in low-risk infants born very preterm: A longitudinal prospective study. Dev. Med. Child Neurol. 2022, 64, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Ljungblad, U.W.; Paulsen, H.; Tangeraas, T.; Evensen, K.A.I. Reference Material for Hammersmith Infant Neurologic Examination Scores Based on Healthy, Term Infants Age 3–7 Months. J. Pediatr. 2022, 244, 79–85.e12. [Google Scholar] [CrossRef] [PubMed]
- Patrick, D.L.; Pennifer, E. Health Status and Health Policy: Quality of Life in Health Care Evaluation and Resource Allocation; Oxford University Press: Oxford, UK, 1993; 478p. [Google Scholar]
- Dubowitz, L.; Ricciw, D.; Mercuri, E. The Dubowitz neurological examination of the full-term newborn. Ment. Retard. Dev. Disabil. Res. Rev. 2005, 11, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J. Anaesth. 2017, 11 (Suppl. 1), S80–S89. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Zou, G.Y. Sample size formulas for estimating intraclass correlation coefficients with precision and assurance. Stat. Med. 2012, 31, 3972–3981. [Google Scholar] [CrossRef]
- Sim, J.; Wright, C.C. The Kappa Statistic in Reliability Studies: Use, Interpretation, and Sample Size Requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Hay, K.; Nelin, M.; Carey, H.; Chorna, O.; Moore-Clingenpeel, M.M.; Maitre, N. Hammersmith Infant Neurological Examination Asymmetry Score Distinguishes Hemiplegic Cerebral Palsy From Typical Development. Pediatr. Neurol. 2018, 87, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Pietruszewski, L.; Nelin, M.A.; Batterson, N.O.; Less, J.; Moore-Clingenpeel, M.M.; Lewandowski, D.; Levengood, K.; Maitre, N.L. Hammersmith Infant Neurological Examination Clinical Use to Recommend Therapist Assessment of Functional Hand Asymmetries. Pediatr. Phys. Ther. 2021, 33, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Heathcock, J.C.; Lobo, M.; Galloway, J.C. Movement training advances the emergence of reaching in infants born at less than 33 weeks of gestational age: A randomized clinical trial. Phys. Ther. 2008, 88, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Maitre, N.L.; Benninger, K.L.; Neel, M.L.; Haase, J.A.; Pietruszewski, L.; Levengood, K.; Adderley, K.M.; Batterson, N.O.; Hague, K.M.; Lightfoot, M.M.-B.; et al. Standardized Neurodevelopmental Surveillance of High-risk Infants Using Telehealth: Implementation Study during COVID-19. Pediatr. Qual. Saf. 2021, 6, e439. [Google Scholar] [CrossRef]
- Coxon, M.L.; Hoyt, C.R.; Smith, A.E.; Hadders-Algra, M. Going Beyond Conventional Assessment of Developmental Motor Disorders: Exploring Video Methods for Early Identification Among Children 0 to 3 Years. Adv. Rehabilitation Sci. Pract. 2023, 12. [Google Scholar] [CrossRef]
- Dey, P.; Dogra, D.P.; Roy, P.P.; Bhaskar, H. Autonomous vision-guided approach for the analysis and grading of vertical suspension tests during Hammersmith Infant Neurological Examination (HINE). In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 863–866. Available online: http://www.ncbi.nlm.nih.gov/pubmed/28268460 (accessed on 29 June 2019).
- Pizzardi, A.; Romeo, D.M.M.; Cioni, M.; Romeo, M.G.; Guzzetta, A. Infant Neurological Examination from 3 to 12 Months: Predictive Value of the Single Items. Neuropediatrics 2008, 39, 344–346. [Google Scholar] [CrossRef]
- Kwong, A.K.L.; Eeles, A.L.; Olsen, J.E.; Cheong, J.L.Y.; Doyle, L.W.; Spittle, A.J. The Baby Moves smartphone app for General Movements Assessment: Engagement amongst extremely preterm and term-born infants in a state-wide geographical study. J. Paediatr. Child Health 2018, 55, 548–554. [Google Scholar] [CrossRef]
- Boonzaaijer, M.; Van Dam, E.; Van Haastert, I.C.; Nuysink, J. Concurrent validity between live and home video observations using the Alberta infant motor scale. Pediatr. Phys. Ther. 2017, 29, 146–151. [Google Scholar] [CrossRef]
- Chagas, P.S.C.; Rosenbaum, P.; Wright, F.V.; Pritchard, L.; Wright, M.; Toledo, A.M.; Camargos, A.C.R.; Longo, E.; Leite, H.R. Development of the Gross Motor Function Family Report (GMF-FR) for Children with Cerebral Palsy. Physiother. Can. 2022, 75, 83–91. [Google Scholar] [CrossRef]
- Amiel-Tison, C.; Grenier, A. Neurological Assessment during the First Years of Life; Oxford University Press: New York, NY, USA, 1986. [Google Scholar]
- Touwen, B.C.L. Examination of the Child with Minor Neurological Dysfunction. In Clinics in Developmental Medicine; Spastics International Medical Publications: London, UK, 1979. [Google Scholar]
- Dubowitz, L.; Dubowitz, V.; Mercuri, E. The Neurological Assessment of the Preterm and Full-term Newborn Infant, 2nd ed.; Heinemann, Ed.; Clinics in Developmental Medicine: London, UK, 1999. [Google Scholar]
- McGready, R.; Simpson, J.; Panyavudhikrai, S.; Loo, S.; Mercuri, E.; Haataja, L.; Kolatat, T.; Nosten, F.; Dubowitz, L. Neonatal neurological testing in resource-poor settings. Ann. Trop. Paediatr. 2000, 20, 323–336. [Google Scholar] [CrossRef]
- Lata, K.; Jindal, P.; Verma, A.; Dochania, K.; Batra, R. Comparison between trained specialist and medical student in performing neurological assessment of high-risk infant by Hammersmith infant neurological examination (HINE). J. Fam. Med. Prim. Care 2020, 9, 6297–6298. [Google Scholar] [CrossRef]
- Merino-Andrés, J.; Hidalgo-Robles, Á.; Pérez-Nombela, S.; Williams, S.A.; Paleg, G.; Fernández-Rego, F.J. Tool Use for Early Detection of Cerebral Palsy: A Survey of Spanish Pediatric Physical Therapists. Pediatr. Phys. Ther. 2022, 34, 202–210. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.; Duncan, A.; Pickar, T.; Burkhardt, S.; Boyd, R.N.; Neel, M.L.; Maitre, N.L. Comparing parent and provider priorities in discussions of early detection and intervention for infants with and at risk of cerebral palsy. Child Care Health Dev. 2019, 45, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Romeo, D.M.M.; Cioni, M.; Scoto, M.; Mazzone, L.; Palermo, F.; Romeo, M.G. Neuromotor development in infants with cerebral palsy investigated by the Hammersmith Infant Neurological Examination during the first year of age. Eur. J. Paediatr. Neurol. 2008, 12, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Maitre, N.L.; Burton, V.J.; Duncan, A.F.; Iyer, S.; Ostrander, B.; Winter, S.; Ayala, L.; Burkhardt, S.; Gerner, G.; Getachew, R.; et al. Network Implementation of Guideline for Early Detection Decreases Age at Cerebral Palsy Diagnosis. Pediatrics 2020, 145, e20192126. [Google Scholar] [CrossRef] [PubMed]
- McNamara, L.M.; Scott, K.M.; Boyd, R.N.; Webb, A.E.; Taifalos, C.J.; Novak, I.E. Effectiveness of early diagnosis of cerebral palsy guideline implementation: A systematic review. Minerva Pediatr. 2023. [Google Scholar] [CrossRef]


| Training Elements | Duration |
|---|---|
| Reading the scientific literature supporting the use of HINE | 30 min |
| Review of the administration and scoring of individual HINE items | 45 min |
| HINE demonstrations with video recordings and face-to-face assessments (different ages and health statuses) | 15 min per patient |
| Review of video recordings and discussion of HINE administration and scoring | 20 min per patient |
| Item | Subsection | Possible Comprehension Errors |
|---|---|---|
| Auditory response | Cranial nerves | The Spanish translation should clarify the concept of “dubious reaction” to the stimulus. |
| Hands | Posture | In the Spanish translation, there should be the concept of “fisting”. |
| Quality | Movements | In the Spanish translation, there should be a word conceptually equivalent to “spasmodic”. |
| Lateral suspension | Reflexes and reactions | The Spanish translation should make it clear that the movement is “towards” the horizontal, not in the full horizontal position. |
| Characteristic | Total Study Population (n = 25) |
|---|---|
| Gestational age mean (SD) (minimum, maximum), wks | 30.3 (4.5) (24.4–41.0) |
| Birth weight mean (SD) (minimum, maximum), g | 1512.6 (741.1) (720–3450) |
| Head circumference, mean (SD) (minimum, maximum), cm | 27.8 (4.1) (21.5–35) |
| Apgar 1′ mean (SD) (minimum, maximum); Apgar 1′ mean (SD) (minimum, maximum) | 6.5 (1.9) (2–9); 8.1 (1.6) (4–10) |
| Multiple birth, n (%) | 8 (32) |
| Preterm birth (<37 wks gestation), n (%) | 23 (92) |
| HIE, n (%) | 1 (4) |
| BPD, n (%) | 2 (8) |
| Major brain pathologies in neuroimaging a, n (%) | 3 (12) |
| Age at HINE assessment mean (SD) (minimum, maximum), mo | 8.8 (3.0) (3.5–15.0) |
| 3 to 5 mo, n (%) | 4 (16) |
| 6 to 8 mo, n (%) | 9 (36) |
| 9 to 15 mo, n (%) | 12 (48) |
| Intra-Examiner Reliability | Cranial Nerves | Posture | Movements | Tone | Reflexes and Reactions | Asymmetries | Total Score |
|---|---|---|---|---|---|---|---|
| MR-M | 0.904 | 0.955 | 0.980 | 0.918 | 0.972 | 0.959 | 0.981 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Inter-Examiner Reliability | |||||||
| MR-R, AH-R | 0.817 | 0.818 | 0.990 | 0.868 | 0.914 | 0.507 | 0.968 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.003 | <0.001 | |
| MR-R, JM-A | 0.854 | 0.868 | 0.794 | 0.970 | 0.888 | 0.451 | 0.975 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.050 | <0.001 | |
| AH-R, JM-A | 0.786 | 0.832 | 0.816 | 0.868 | 0.867 | 0.489 | 0.976 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.037 | <0.001 | |
| MR-R, AH-R, JM-A | 0.870 | 0.887 | 0.903 | 0.936 | 0.924 | 0.583 | 0.982 |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | <0.001 |
| Inter-Examiner Reliability MR-R, AH-R | Cranial nerve function | Facial appearance | Eye movements | Visual response | Auditory response | Sucking/swallowing | |||
| 0.359 | 0.468 | 0.490 | 0.917 | 0.370 | |||||
| 0.022 | 0.001 | 0.004 | <0.001 | 0.006 | |||||
| Posture | Head | Trunk | Arms | Hands | Legs | Feet | |||
| 0.419 | 0.596 | 0.648 | 0.259 | 0.545 | 0.527 | ||||
| 0.006 | <0.001 | 0.001 | 0.080 | <0.001 | <0.001 | ||||
| Movements | Quantity | Quality | |||||||
| 0.684 | 0.855 | ||||||||
| <0.001 | <0.001 | ||||||||
| Tone | Scarf sign | Passive shoulder elevation | Pronation/supination | Hip adductors | Popliteal angle | Ankle dorsiflexion | Pull to sit | Ventral suspension | |
| 0.658 | 0.648 | 0.648 | 0.468 | 0.552 | 0.416 | 0.779 | 0.795 | ||
| <0.001 | 0.001 | 0.001 | 0.006 | 0.001 | 0.007 | <0.001 | <0.001 | ||
| Reflexes and reactions | Arm protection | Vertical suspension | Lateral tilting | Forward parachute | Tendon reflexes | ||||
| 0.627 | 0.172 | 0.663 | 0.631 | 0.479 | |||||
| <0.001 | 0.380 | <0.001 | <0.001 | 0.001 |
| Inter-Examiner Reliability | Cranial Nerves | Posture | Movements | Tone | Reflexes and Reactions | Asymmetries | Total Score |
|---|---|---|---|---|---|---|---|
| AH-R, IA-G, CB-M, AMF-T | 0.945 | 0.973 | 0.790 | 0.856 | 0.980 | 0.618 | 0.988 |
| Total score | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.026 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hidalgo-Robles, Á.; Merino-Andrés, J.; Rodríguez-Fernández, Á.L.; Gutiérrez-Ortega, M.; León-Estrada, I.; Ródenas-Martínez, M. Reliability, Knowledge Translation, and Implementability of the Spanish Version of the Hammersmith Infant Neurological Examination. Healthcare 2024, 12, 380. https://doi.org/10.3390/healthcare12030380
Hidalgo-Robles Á, Merino-Andrés J, Rodríguez-Fernández ÁL, Gutiérrez-Ortega M, León-Estrada I, Ródenas-Martínez M. Reliability, Knowledge Translation, and Implementability of the Spanish Version of the Hammersmith Infant Neurological Examination. Healthcare. 2024; 12(3):380. https://doi.org/10.3390/healthcare12030380
Chicago/Turabian StyleHidalgo-Robles, Álvaro, Javier Merino-Andrés, Ángel Luis Rodríguez-Fernández, Mónica Gutiérrez-Ortega, Irene León-Estrada, and Maribel Ródenas-Martínez. 2024. "Reliability, Knowledge Translation, and Implementability of the Spanish Version of the Hammersmith Infant Neurological Examination" Healthcare 12, no. 3: 380. https://doi.org/10.3390/healthcare12030380
APA StyleHidalgo-Robles, Á., Merino-Andrés, J., Rodríguez-Fernández, Á. L., Gutiérrez-Ortega, M., León-Estrada, I., & Ródenas-Martínez, M. (2024). Reliability, Knowledge Translation, and Implementability of the Spanish Version of the Hammersmith Infant Neurological Examination. Healthcare, 12(3), 380. https://doi.org/10.3390/healthcare12030380







