Association between Organizational Support and Turnover Intention in Nurses: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Methods
2.2. Selection Process
2.3. Quality Appraisal
2.4. Data Abstraction
2.5. Synthesis
3. Results
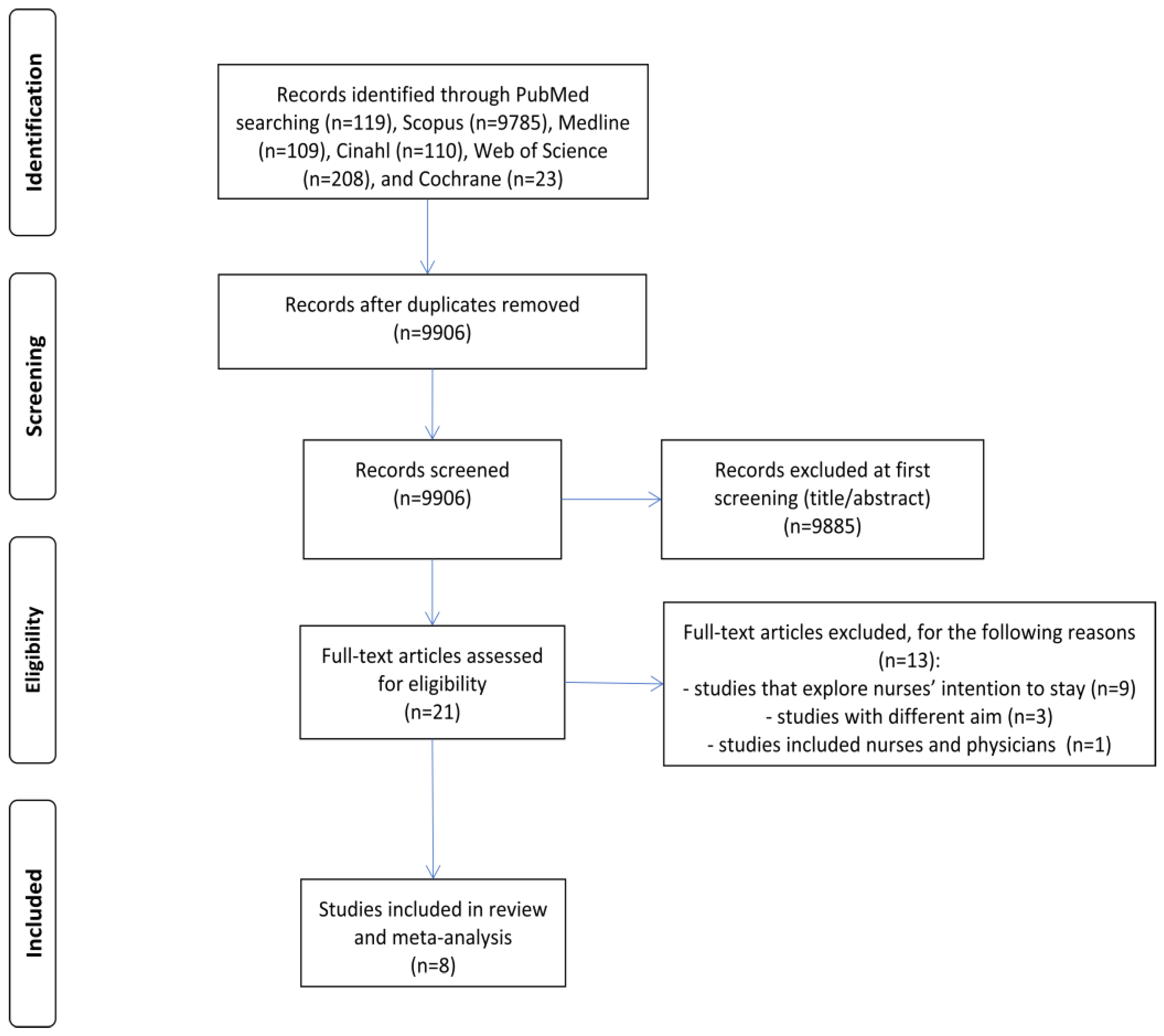
3.1. Identification and Selection of Studies
3.2. Characteristics of the Studies
3.3. Quality Assessment
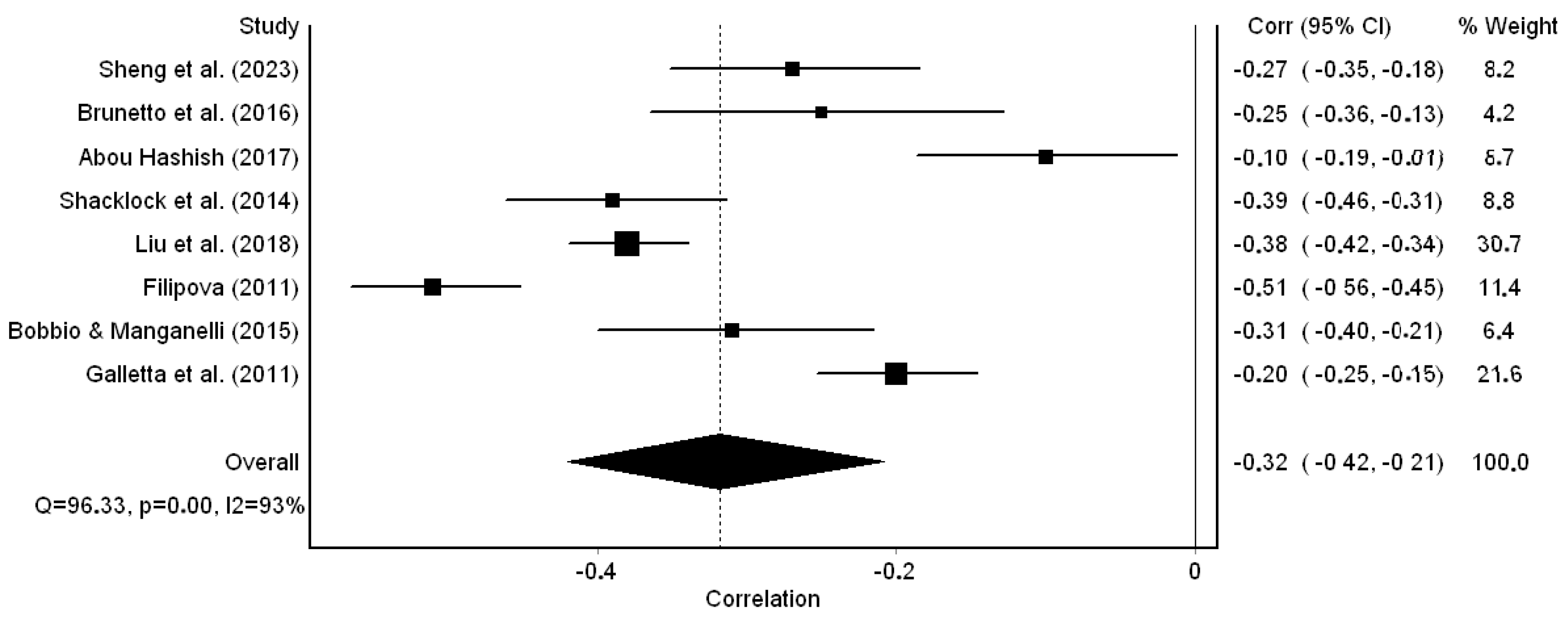
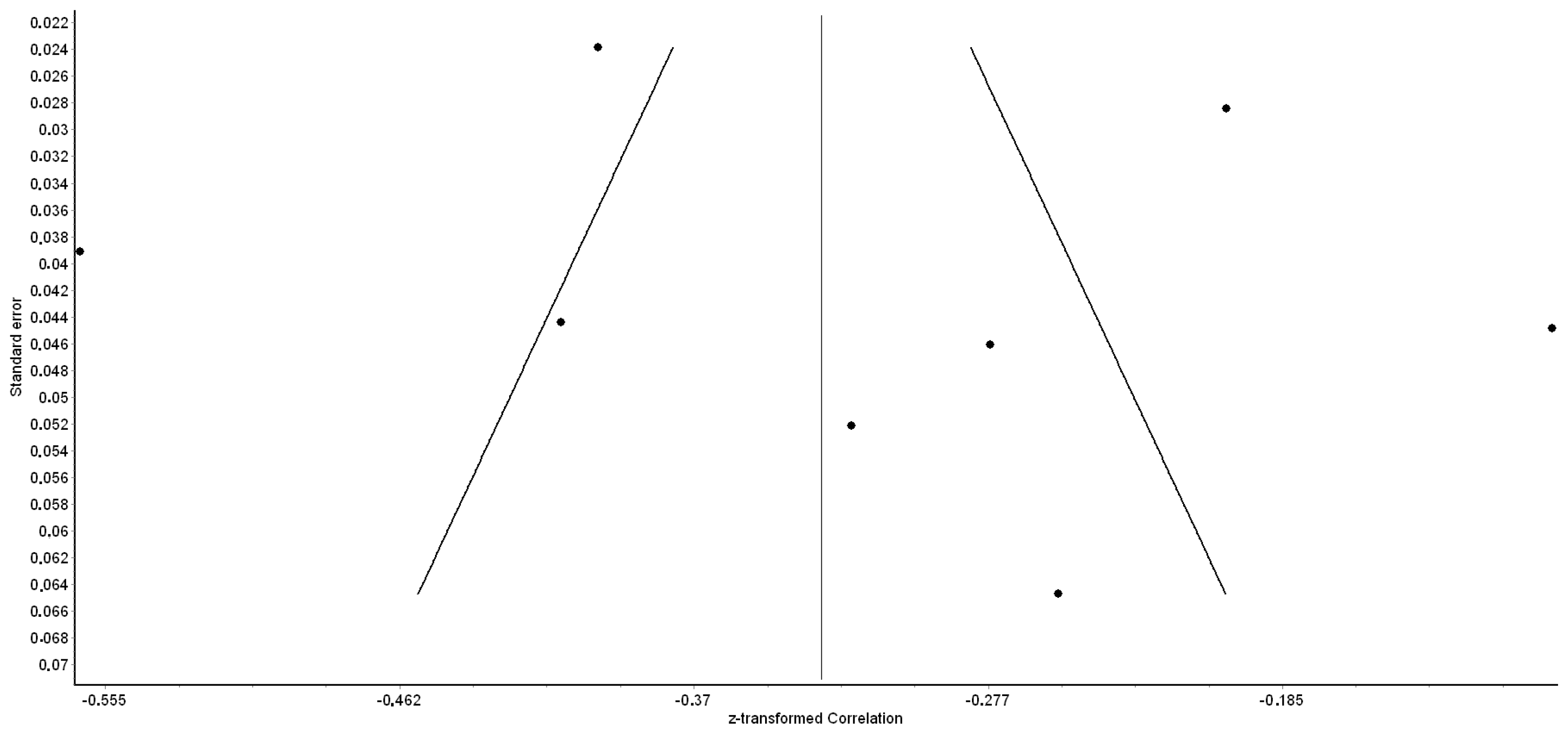
3.4. Meta-Analysis
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Westbrook, J.I.; Duffield, C.; Li, L.; Creswick, N.J. How Much Time Do Nurses Have for Patients? A Longitudinal Study Quantifying Hospital Nurses’ Patterns of Task Time Distribution and Interactions with Health Professionals. BMC Health Serv. Res. 2011, 11, 319. [Google Scholar] [CrossRef] [PubMed]
- Kieft, R.A.M.M.; De Brouwer, B.B.J.M.; Francke, A.L.; Delnoij, D.M.J. How Nurses and Their Work Environment Affect Patient Experiences of the Quality of Care: A Qualitative Study. BMC Health Serv. Res. 2014, 14, 249. [Google Scholar] [CrossRef]
- Karaca, A.; Durna, Z. Patient Satisfaction with the Quality of Nursing Care. Nurs. Open 2019, 6, 545. [Google Scholar] [CrossRef] [PubMed]
- Sloane, D.M.; Smith, H.L.; McHugh, M.D.; Aiken, L.H. Effect of Changes in Hospital Nursing Resources on Improvements in Patient Safety and Quality of Care: A Panel Study. Med. Care 2018, 56, 1008. [Google Scholar] [CrossRef] [PubMed]
- Lasater, K.B.; Aiken, L.H.; Sloane, D.M.; French, R.; Martin, B.; Reneau, K.; Alexander, M.; McHugh, M.D. Chronic Hospital Nurse Understaffing Meets COVID-19: An Observational Study. BMJ Qual. Saf. 2021, 30, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Robaee, N.; Atashzadeh-Shoorideh, F.; Ashktorab, T.; Baghestani, A.; Barkhordari-Sharifabad, M. Perceived Organizational Support and Moral Distress among Nurses. BMC Nurs. 2018, 17, 2. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Agarwal, U.A.; Khatri, N. The Relationships between Perceived Organizational Support, Affective Commitment, Psychological Contract Breach, Organizational Citizenship Behaviour and Work Engagement. J. Adv. Nurs. 2016, 72, 2806–2817. [Google Scholar] [CrossRef]
- Leone, C.; Bruyneel, L.; Anderson, J.E.; Murrells, T.; Dussault, G.; Henriques de Jesus, É.; Sermeus, W.; Aiken, L.; Rafferty, A.M. Work Environment Issues and Intention-to-Leave in Portuguese Nurses: A Cross-Sectional Study. Health Policy 2015, 119, 1584–1592. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Nurses’ Burnout and Associated Risk Factors during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Adv. Nurs. 2021, 77, 3286–3302. [Google Scholar] [CrossRef]
- Falatah, R. The Impact of the Coronavirus Disease (COVID-19) Pandemic on Nurses’ Turnover Intention: An Integrative Review. Nurs. Rep. 2021, 11, 787–810. [Google Scholar] [CrossRef]
- Hayes, L.J.; O’Brien-Pallas, L.; Duffield, C.; Shamian, J.; Buchan, J.; Hughes, F.; Spence Laschinger, H.K.; North, N.; Stone, P.W. Nurse Turnover: A Literature Review. Int. J. Nurs. Stud. 2006, 43, 237–263. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; De los Santos, J.A.A.; Falguera, C.C.; Nwafor, C.E.; Galabay, J.R.; Rosales, R.A.; Firmo, C.N. Predictors of Nurses’ Turnover Intention at One and Five Years’ Time. Int. Nurs. Rev. 2020, 67, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Said, R.M.; El-Shafei, D.A. Occupational Stress, Job Satisfaction, and Intent to Leave: Nurses Working on Front Lines during COVID-19 Pandemic in Zagazig City, Egypt. Environ. Sci. Pollut. Res. 2021, 28, 8791–8801. [Google Scholar] [CrossRef] [PubMed]
- Rotenstein, L.S.; Brown, R.; Sinsky, C.; Linzer, M. The Association of Work Overload with Burnout and Intent to Leave the Job Across the Healthcare Workforce During COVID-19. J. Gen. Intern. Med. 2023, 38, 1920–1927. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, G.; Li, M.; Lyu, L.; Zhang, T. A Cross-Sectional Study on Nurse Turnover Intention and Influencing Factors in Jiangsu Province, China. Int. J. Nurs. Sci. 2018, 5, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Bruyneel, A.; Bouckaert, N.; Maertens de Noordhout, C.; Detollenaere, J.; Kohn, L.; Pirson, M.; Sermeus, W.; Van den Heede, K. Association of Burnout and Intention-to-Leave the Profession with Work Environment: A Nationwide Cross-Sectional Study among Belgian Intensive Care Nurses after Two Years of Pandemic. Int. J. Nurs. Stud. 2023, 137, 104385. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.K.; Kim, J.S. Nursing Stress Factors Affecting Turnover Intention among Hospital Nurses. Int. J. Nurs. Pract. 2020, 26, e12819. [Google Scholar] [CrossRef]
- Lee, E.; Jang, I. Nurses’ Fatigue, Job Stress, Organizational Culture, and Turnover Intention: A Culture–Work–Health Model. West J. Nurs. Res. 2019, 42, 108–116. [Google Scholar] [CrossRef]
- Arslan Yürümezoğlu, H.; Kocaman, G.; Mert Haydarİ, S. Predicting Nurses’ Organizational and Professional Turnover Intentions. Jpn. J. Nurs. Sci. 2019, 16, 274–285. [Google Scholar] [CrossRef]
- Pang, Y.; Dan, H.; Jung, H.; Bae, N.; Kim, O. Depressive Symptoms, Professional Quality of Life and Turnover Intention in Korean Nurses. Int. Nurs. Rev. 2020, 67, 387–394. [Google Scholar] [CrossRef]
- Kim, H.; Kim, E.G. A Meta-Analysis on Predictors of Turnover Intention of Hospital Nurses in South Korea (2000–2020). Nurs. Open 2021, 8, 2406–2418. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; Gloe, D.S.; McEnroe-Petitte, D.M.; Tsaras, K.; Colet, P.C. Factors Influencing Turnover Intention among Registered Nurses in Samar Philippines. Appl. Nurs. Res. 2018, 39, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Moisoglou, I.; Katsiroumpa, A.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Meimeti, E.; Kaitelidou, D. Increased Job Burnout and Reduced Job Satisfaction for Nurses Compared to Other Healthcare Workers after the COVID-19 Pandemic. Nurs. Rep. 2023, 13, 1090–1100. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Katsiroumpa, A.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsoulas, T.; Moisoglou, I.; Gallos, P.; Kaitelidou, D. Nurses Quietly Quit Their Job More Often than Other Healthcare Workers: An Alarming Issue for Healthcare Services. Res. Sq. 2023; preprint. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Katsiroumpa, A.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsoulas, T.; Moisoglou, I.; Gallos, P.; Kaitelidou, D. The Influence of Job Burnout on Quiet Quitting among Nurses: The Mediating Effect of Job Satisfaction. Res. Sq. 2023; preprint. [Google Scholar] [CrossRef]
- Galanis, P.; Moisoglou, I.; Malliarou, M.; Papathanasiou, I.V.; Katsiroumpa, A.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Kaitelidou, D. Quiet Quitting among Nurses Increases Their Turnover Intention: Evidence from Greece in the Post-COVID-19 Era. Healthcare 2024, 12, 79. [Google Scholar] [CrossRef] [PubMed]
- Griffeth, R.W.; Hom, P.W.; Gaertner, S. A Meta-Analysis of Antecedents and Correlates of Employee Turnover: Update, Moderator Tests, and Research Implications for the next Millennium. J. Manag. 2000, 26, 463–488. [Google Scholar] [CrossRef]
- Tett, R.P.; Meyer, J.P. Job Satisfaction, Organizational Commitment, Turnover Intention, and Turnover: Path Analyses Based on Meta-Analytic Findings. Pers. Psychol. 1993, 46, 259–293. [Google Scholar] [CrossRef]
- Eisenberger, R.; Huntington, R.; Hutchison, S.; Sowa, D. Perceived Organizational Support. J. Appl. Psychol. 1986, 71, 500–507. [Google Scholar] [CrossRef]
- Rhoades, L.; Eisenberger, R. Perceived Organizational Support: A Review of the Literature. J. Appl. Psychol. 2002, 87, 698–714. [Google Scholar] [CrossRef]
- Qi, L.; Liu, B.; Wei, X.; Hu, Y. Impact of Inclusive Leadership on Employee Innovative Behavior: Perceived Organizational Support as a Mediator. PLoS ONE 2019, 14, e0212091. [Google Scholar] [CrossRef]
- Sharma, J.; Dhar, R.L. Factors Influencing Job Performance of Nursing Staff: Mediating Role of Affective Commitment. Pers. Rev. 2016, 45, 161–182. [Google Scholar] [CrossRef]
- Tang, Y.; Wang, Y.; Zhou, H.; Wang, J.; Zhang, R.; Lu, Q. The Relationship between Psychiatric Nurses’ Perceived Organizational Support and Job Burnout: Mediating Role of Psychological Capital. Front. Psychol. 2023, 14, 1099687. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; De los Santos, J.A.A. COVID-19 Anxiety among Front-Line Nurses: Predictive Role of Organisational Support, Personal Resilience and Social Support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Pahlevan Sharif, S.; Ahadzadeh, A.S.; Sharif Nia, H. Mediating Role of Psychological Well-Being in the Relationship between Organizational Support and Nurses’ Outcomes: A Cross-Sectional Study. J. Adv. Nurs. 2018, 74, 887–899. [Google Scholar] [CrossRef] [PubMed]
- Abou Hashish, E.A. Relationship between Ethical Work Climate and Nurses’ Perception of Organizational Support, Commitment, Job Satisfaction and Turnover Intent. Nurs. Ethics 2017, 24, 151–166. [Google Scholar] [CrossRef]
- Ma, Y.; Chen, F.; Xing, D.; Meng, Q.; Zhang, Y. Study on the Associated Factors of Turnover Intention among Emergency Nurses in China and the Relationship between Major Factors. Int. Emerg. Nurs. 2022, 60, 101106. [Google Scholar] [CrossRef]
- Pahlevan Sharif, S.; Bolt, E.E.T.; Ahadzadeh, A.S.; Turner, J.J.; Sharif Nia, H. Organisational Support and Turnover Intentions: A Moderated Mediation Approach. Nurs. Open 2021, 8, 3615. [Google Scholar] [CrossRef]
- Nei, D.; Snyder, L.A.; Litwiller, B.J. Promoting Retention of Nurses: A Meta-Analytic Examination of Causes of Nurse Turnover. Health Care Manag. Rev. 2015, 40, 237–253. [Google Scholar] [CrossRef]
- Boniol, M.; Kunjumen, T.; Nair, T.S.; Siyam, A.; Campbell, J.; Diallo, K. The Global Health Workforce Stock and Distribution in 2020 and 2030: A Threat to Equity and “universal” Health Coverage? BMJ Glob. Health 2022, 7, 009316. [Google Scholar] [CrossRef]
- Sheng, H.; Tian, D.; Sun, L.; Hou, Y.; Liu, X. Nurse Practice Environment, Perceived Organizational Support, General Well-Being, Occupational Burnout and Turnover Intention: A Moderated Multi-Mediation Model. Nurs. Open 2023, 10, 3828–3839. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Zhao, S.; Shi, L.; Zhang, Z.; Liu, X.; Li, L.; Duan, X.; Li, G.; Lou, F.; Jia, X.; et al. Workplace Violence, Job Satisfaction, Burnout, Perceived Organisational Support and Their Effects on Turnover Intention among Chinese Nurses in Tertiary Hospitals: A Cross-Sectional Study. BMJ Open 2018, 8, e019525. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, W.M.; Secoli, S.R.; Püschel, V.A. de A. The Joanna Briggs Institute Approach for Systematic. Rev. Lat. Am. Enfermagem. 2018, 26, e3074. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Academic Press: Cambridge, MA, USA, 2013; ISBN 1483276481. [Google Scholar]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Wallace, B.C.; Schmid, C.H.; Lau, J.; Trikalinos, T.A. Meta-Analyst: Software for Meta-Analysis of Binary, Continuous and Diagnostic Data. BMC Med. Res. Methodol. 2009, 9, 80. [Google Scholar] [CrossRef] [PubMed]
- Bobbio, A.; Manganelli, A.M. Antecedents of Hospital Nurses’ Intention to Leave the Organization: A Cross Sectional Survey. Int. J. Nurs. Stud. 2015, 52, 1180–1192. [Google Scholar] [CrossRef]
- Brunetto, Y.; Rodwell, J.; Shacklock, K.; Farr-Wharton, R.; Demir, D. The Impact of Individual and Organizational Resources on Nurse Outcomes and Intent to Quit. J. Adv. Nurs. 2016, 72, 3093–3103. [Google Scholar] [CrossRef]
- Filipova, A.A. Relationships Among Ethical Climates, Perceived Organizational Support, and Intent-to-Leave for Licensed Nurses in Skilled Nursing Facilities. J. Appl. Gerontol. 2010, 30, 44–66. [Google Scholar] [CrossRef]
- Galletta, M.; Portoghese, I.; Penna, M.P.; Battistelli, A.; Saiani, L. Turnover Intention among Italian Nurses: The Moderating Roles of Supervisor Support and Organizational Support. Nurs. Health Sci. 2011, 13, 184–191. [Google Scholar] [CrossRef]
- Shacklock, K.; Brunetto, Y.; Teo, S.; Farr-Wharton, R. The Role of Support Antecedents in Nurses’ Intentions to Quit: The Case of Australia. J. Adv. Nurs. 2014, 70, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.H. Noneconomic and Economic Impacts of Nurse Turnover in Hospitals: A Systematic Review. Int. Nurs. Rev. 2022, 69, 392–404. [Google Scholar] [CrossRef] [PubMed]
- Roche, M.A.; Duffield, C.M.; Homer, C.; Buchan, J.; Dimitrelis, S. The Rate and Cost of Nurse Turnover in Australia. Collegian 2015, 22, 353–358. [Google Scholar] [CrossRef]
- Makary, M.A.; Daniel, M. Medical Error-the Third Leading Cause of Death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef] [PubMed]
- Cranage, K.; Foster, K. Mental Health Nurses’ Experience of Challenging Workplace Situations: A Qualitative Descriptive Study. Int. J. Ment. Health Nurs. 2022, 31, 665–676. [Google Scholar] [CrossRef] [PubMed]
- Takase, M. A Concept Analysis of Turnover Intention: Implications for Nursing Management. Collegian 2010, 17, 3–12. [Google Scholar] [CrossRef]
- Moisoglou, I.; Meimeti, E.; Arvanitidou, E.; Galanis, P.; Ntavoni, G.; Zavras, D. Job Satisfaction in Primary Health Care in Athens, Greece: A Pilot Study. Int. J. Caring Sci. 2021, 14, 166–173. [Google Scholar]
- Dilig-Ruiz, A.; MacDonald, I.; Demery Varin, M.; Vandyk, A.; Graham, I.D.; Squires, J.E. Job Satisfaction among Critical Care Nurses: A Systematic Review. Int. J. Nurs. Stud. 2018, 88, 123–134. [Google Scholar] [CrossRef]
- De Simone, S.; Planta, A.; Cicotto, G. The Role of Job Satisfaction, Work Engagement, Self-Efficacy and Agentic Capacities on Nurses’ Turnover Intention and Patient Satisfaction. Appl. Nurs. Res. 2018, 39, 130–140. [Google Scholar] [CrossRef]
- Yasin, Y.M.; Kerr, M.S.; Wong, C.A.; Bélanger, C.H. Factors Affecting Nurses’ Job Satisfaction in Rural and Urban Acute Care Settings: A PRISMA Systematic Review. J. Adv. Nurs. 2020, 76, 963–979. [Google Scholar] [CrossRef]
- Al Maqbali, M.A. Factors That Influence Nurses’ Job Satisfaction: A Literature Review. Nurs. Manag. 2015, 22, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Kurtessis, J.N.; Eisenberger, R.; Ford, M.T.; Buffardi, L.C.; Stewart, K.A.; Adis, C.S. Perceived Organizational Support: A Meta-Analytic Evaluation of Organizational Support Theory. J. Manag. 2015, 43, 1854–1884. [Google Scholar] [CrossRef]
- Gómez-Urquiza, J.L.; De la Fuente-Solana, E.I.; Albendín-García, L.; Vargas-Pecino, C.; Ortega-Campos, E.M.; Cañadas-De la Fuente, G.A. Prevalence of Burnout Syndrome in Emergency Nurses: A Meta-Analysis. Crit. Care Nurse 2017, 37, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Ran, L.; Chen, X.; Peng, S.; Zheng, F.; Tan, X.; Duan, R. Job Burnout and Turnover Intention among Chinese Primary Healthcare Staff: The Mediating Effect of Satisfaction. BMJ Open 2020, 10, e036702. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.K.; Gandrakota, N.; Cimiotti, J.P.; Ghose, N.; Moore, M.; Ali, M.K. Prevalence of and Factors Associated with Nurse Burnout in the US. JAMA Netw. Open 2021, 4, e2036469. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in Nursing: A Theoretical Review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Moisoglou, I.; Yfantis, A.; Tsiouma, E.; Galanis, P. The Work Environment of Haemodialysis Nurses and Its Mediating Role in Burnout. J. Ren. Care 2021, 47, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Bobbio, A.; Bellan, M.; Manganelli, A.M. Empowering Leadership, Perceived Organizational Support, Trust, and Job Burnout for Nurses: A Study in an Italian General Hospital. Health Care Manag. Rev. 2012, 37, 77–87. [Google Scholar] [CrossRef]
- Chung, H.C.; Chen, Y.C.; Chang, S.C.; Hsu, W.L.; Hsieh, T.C. Nurses’ Well-Being, Health-Promoting Lifestyle and Work Environment Satisfaction Correlation: A Psychometric Study for Development of Nursing Health and Job Satisfaction Model and Scale. Int. J. Environ. Res. Public Health 2020, 17, 3582. [Google Scholar] [CrossRef]
- Shen, X.; Zou, X.; Zhong, X.; Yan, J.; Li, L. Psychological Stress of ICU Nurses in the Time of COVID-19. Crit. Care 2020, 24, 200. [Google Scholar] [CrossRef]
- Tan, B.Y.Q.; Chew, N.W.S.; Lee, G.K.H.; Jing, M.; Goh, Y.; Yeo, L.L.L.; Zhang, K.; Chin, H.K.; Ahmad, A.; Khan, F.A.; et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Ann. Intern. Med. 2020, 173, 317–320. [Google Scholar] [CrossRef]
- Maharaj, S.; Lees, T.; Lal, S. Prevalence and Risk Factors of Depression, Anxiety, and Stress in a Cohort of Australian Nurses. Int. J. Environ. Res. Public Health 2019, 16, 61. [Google Scholar] [CrossRef] [PubMed]
- Mirzaei, A.; Rezakhani Moghaddam, H.; Habibi Soola, A. Identifying the Predictors of Turnover Intention Based on Psychosocial Factors of Nurses during the COVID-19 Outbreak. Nurs. Open 2021, 8, 3469–3476. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Young, B.; Mccallum, L.; Rattray, J.; Ramsay, P.; Salisbury, L.; Scott, T.; Hull, A.; Cole, S.; Pollard, B.; et al. “Like Fighting a Fire with a Water Pistol”: A Qualitative Study of the Work Experiences of Critical Care Nurses during the COVID-19 Pandemic. J. Adv. Nurs. 2023, 80, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Jung, S.Y.; Lee, M.H.; Kim, M.S. Assessing the Presence of Post-Traumatic Stress and Turnover Intention Among Nurses Post–Middle East Respiratory Syndrome Outbreak: The Importance of Supervisor Support. Workplace Health Saf. 2020, 68, 337–345. [Google Scholar] [CrossRef]
- Byon, H.D.; Sagherian, K.; Kim, Y.; Lipscomb, J.; Crandall, M.; Steege, L. Nurses’ Experience With Type II Workplace Violence and Underreporting During the COVID-19 Pandemic. Workplace Health Saf. 2021, 70, 412–420. [Google Scholar] [CrossRef]
- Li, N.; Zhang, L.; Xiao, G.; Chen, J.; Lu, Q. The Relationship between Workplace Violence, Job Satisfaction and Turnover Intention in Emergency Nurses. Int. Emerg. Nurs. 2019, 45, 50–55. [Google Scholar] [CrossRef]
- Ayasreh, I.R.; Hayajneh, F.A. Workplace Violence Against Emergency Nurses: A Literature Review. Crit. Care Nurs. Q. 2021, 44, 187–202. [Google Scholar] [CrossRef]
- Vento, S.; Cainelli, F.; Vallone, A. Violence Against Healthcare Workers: A Worldwide Phenomenon With Serious Consequences. Front. Public Health 2020, 8, 570459. [Google Scholar] [CrossRef]
- Cakal, H.; Keshavarzi, S.; Ruhani, A.; Dakhil-Abbasi, G. Workplace Violence and Turnover Intentions among Nurses: The Moderating Roles of Invulnerability and Organisational Support—A Cross-Sectional Study. J. Clin. Nurs. 2021; preprint. [Google Scholar] [CrossRef]
- Baird, K.M.; Tung, A.; Yu, Y. Employee Organizational Commitment and Hospital Performance. Health Care Manag. Rev. 2019, 44, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Vagharseyyedin, S. An Integrative Review of Literature on Determinants of Nurses’ Organizational Commitment. Iran. J. Nurs. Midwifery Res. 2016, 21, 117. [Google Scholar] [CrossRef] [PubMed]
- Albalawi, A.S.; Naughton, S.; Elayan, M.B.; Sleimi, M.T. Perceived Organizational Support, Alternative Job Opportunity, Organizational Commitment, Job Satisfaction and Turnover Intention: A Moderated-Mediated Model. Organizacija 2019, 52, 310–324. [Google Scholar] [CrossRef]
- Sokhanvar, M.; Kakemam, E.; Chegini, Z.; Sarbakhsh, P. Hospital Nurses’ Job Security and Turnover Intention and Factors Contributing to Their Turnover Intention: A Cross-Sectional Study. Nurs. Midwifery Stud. 2018, 7, 133–140. [Google Scholar]
| Reference | Country | Data Collection Time | Females (%) | Age, Mean (SD) | Sample Size (n) | Study Design | Sampling Method | Clinical Settings | Assessment Tool for Organizational Support | Assessment Tool for Turnover Intention | Response Rate (%) | Correlation Coefficient (p-Value) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Sheng et al., 2023) [41] | China | 2020–2021 | 96.2 | 27.0 (3.9) | 474 | Cross-sectional | Convenience | Hospitals | SPOS | TIS | 96.3 | −0.27 (<0.01) |
| (Brunetto et al., 2016) [49] | Australia | 2013 | 83.2 | 41–60 years: 64.8% | 242 | Cross-sectional | Convenience | Hospitals | SPOS | Eight-item scale | 33.0 | −0.25 (<0.01) |
| (Abou Hashish, 2017) [36] | Egypt | NR | NR | ≤29 years: 47.2%; 30–40: 33.0%; ≥41: 19.8% | 500 | Cross-sectional | Convenience | Hospitals | SPOS | TIS | 78.5 | −0.10 (0.16) |
| (Shacklock et al., 2014) [52] | Australia | 2010–2011 | 93.7 | 46.5 (10.4) | 510 | Cross-sectional | Convenience | Hospitals | SPOS | Three-item scale | 31.5 | −0.39 (<0.001) |
| (Liu et al., 2018) [42] | China | 2016–2017 | 96.6 | ≤30 years: 51.1%; 31–50: 45.0%; ≥51: 3.9% | 1761 | Cross-sectional | Purposive | Hospitals | POS-SVS | TIS | 85.2 | −0.38 (<0.001) |
| (Filipova, 2011) [50] | USA | 2010 | 94.0 | 44–53 years: 37.0% | 656 | Cross-sectional | Convenience | Hospitals | SPOS | Three-item scale | 21.4 | −0.51 (<0.001) |
| (Bobbio & Manganelli, 2015) [48] | Italy | 2012 | 79.0 | 42.3 (8.1) | 371 | Cross-sectional | Convenience | Hospitals | SPOS | Three-item scale | 41.0 | −0.31 (<0.01) |
| (Galletta et al., 2011) [51] | France | 2010 | 81.5 | 37.0 (7.9) | 1240 | Cross-sectional | Convenience | Hospitals | SPOS | Two-item scale | 64.0 | −0.20 (<0.001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galanis, P.; Moisoglou, I.; Papathanasiou, I.V.; Malliarou, M.; Katsiroumpa, A.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Kaitelidou, D. Association between Organizational Support and Turnover Intention in Nurses: A Systematic Review and Meta-Analysis. Healthcare 2024, 12, 291. https://doi.org/10.3390/healthcare12030291
Galanis P, Moisoglou I, Papathanasiou IV, Malliarou M, Katsiroumpa A, Vraka I, Siskou O, Konstantakopoulou O, Kaitelidou D. Association between Organizational Support and Turnover Intention in Nurses: A Systematic Review and Meta-Analysis. Healthcare. 2024; 12(3):291. https://doi.org/10.3390/healthcare12030291
Chicago/Turabian StyleGalanis, Petros, Ioannis Moisoglou, Ioanna V. Papathanasiou, Maria Malliarou, Aglaia Katsiroumpa, Irene Vraka, Olga Siskou, Olympia Konstantakopoulou, and Daphne Kaitelidou. 2024. "Association between Organizational Support and Turnover Intention in Nurses: A Systematic Review and Meta-Analysis" Healthcare 12, no. 3: 291. https://doi.org/10.3390/healthcare12030291
APA StyleGalanis, P., Moisoglou, I., Papathanasiou, I. V., Malliarou, M., Katsiroumpa, A., Vraka, I., Siskou, O., Konstantakopoulou, O., & Kaitelidou, D. (2024). Association between Organizational Support and Turnover Intention in Nurses: A Systematic Review and Meta-Analysis. Healthcare, 12(3), 291. https://doi.org/10.3390/healthcare12030291













