Physical Activity Levels of Community-Dwelling Older Adults During Daily Life Activities: A Descriptive Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Physical Activity Parameters
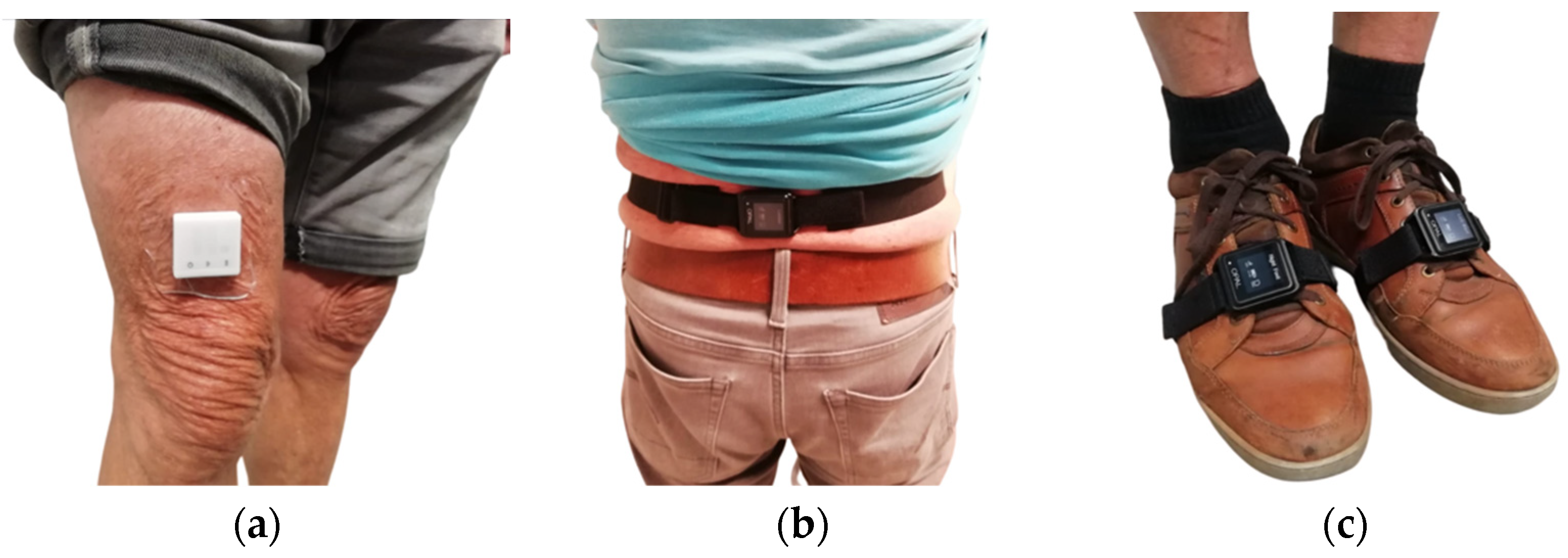
2.3. Wearable Devices
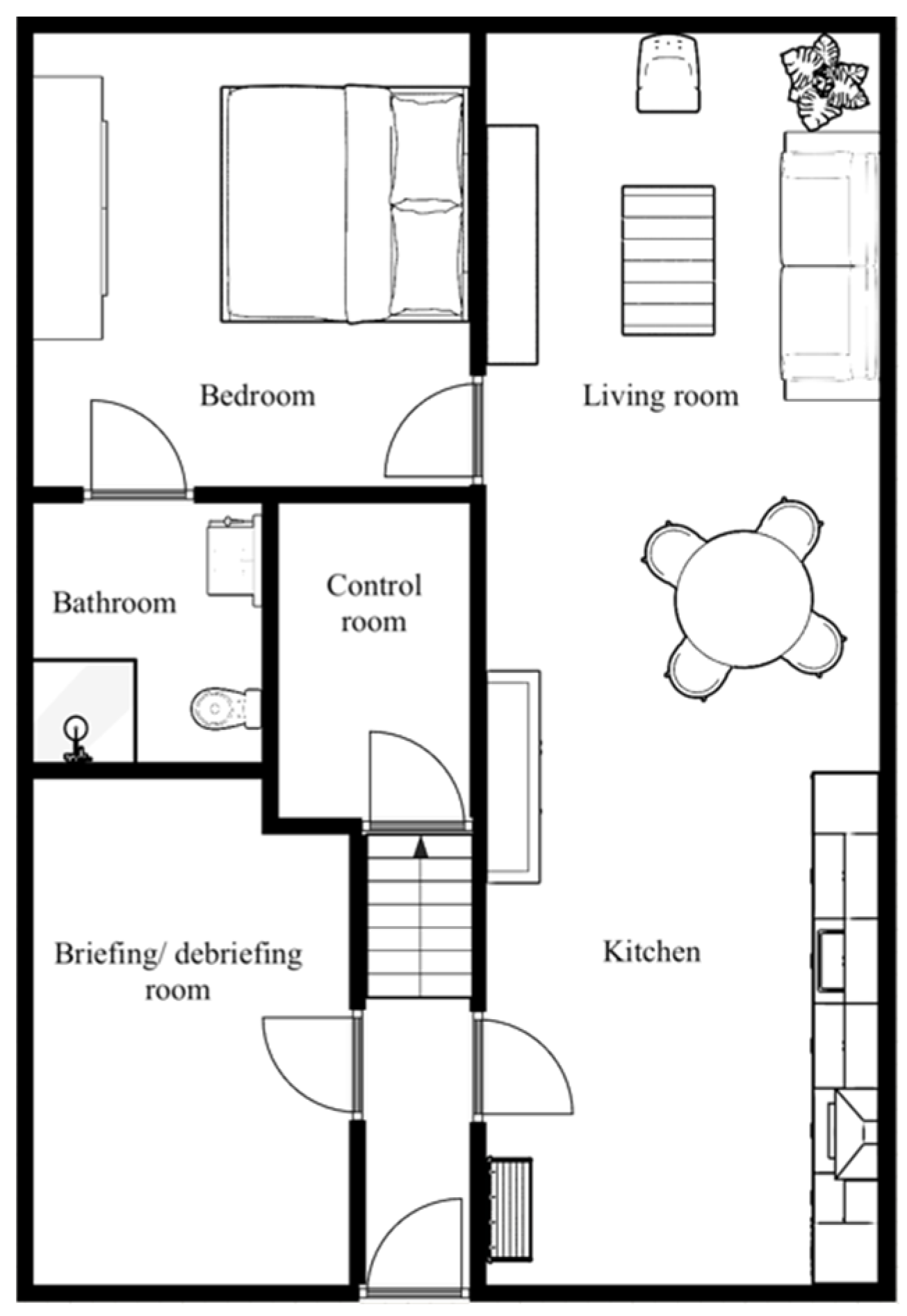
2.4. Study Procedure
2.5. Data Analyses
2.6. Descriptive Analyses
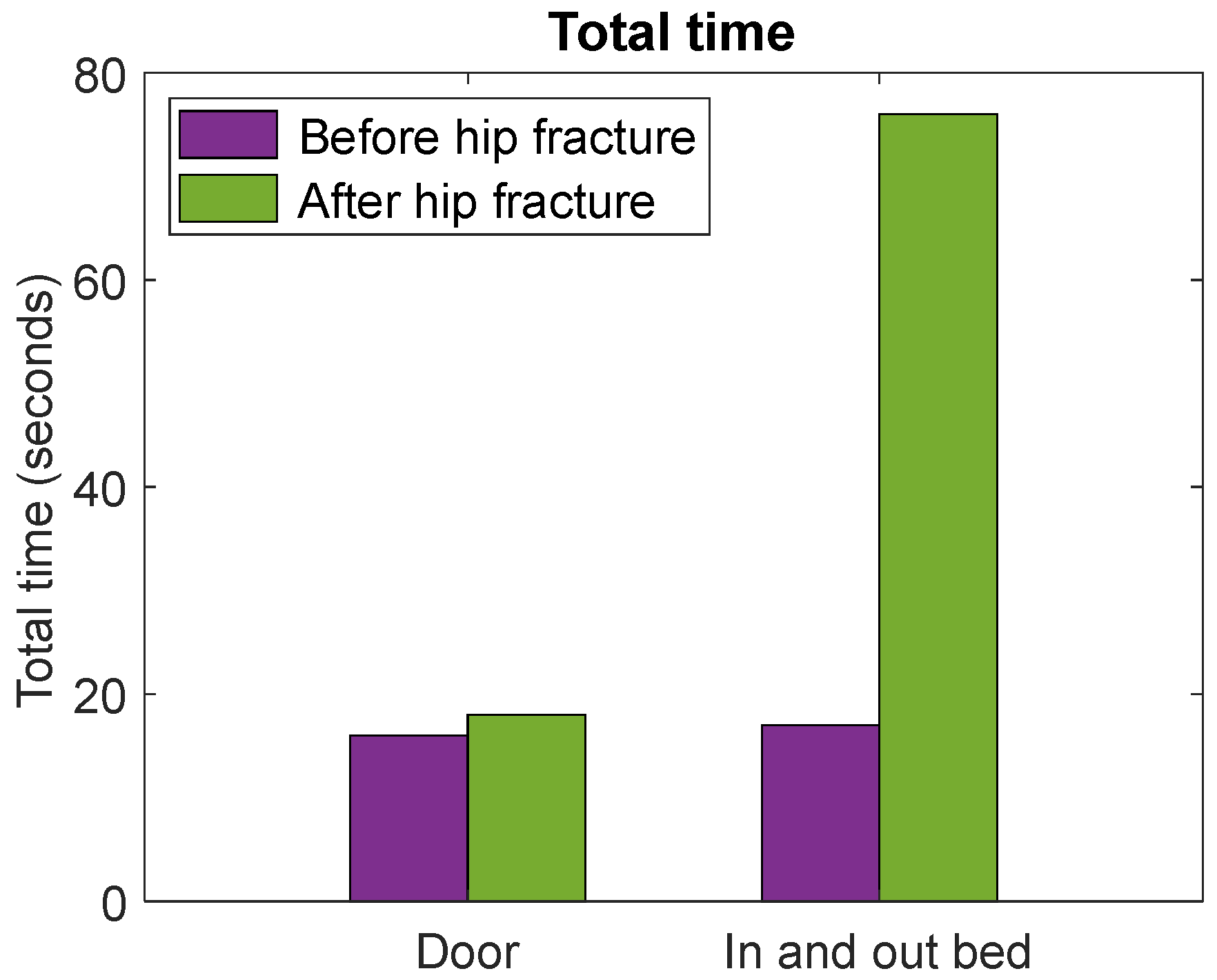
2.7. Case Study
3. Results
3.1. Participants
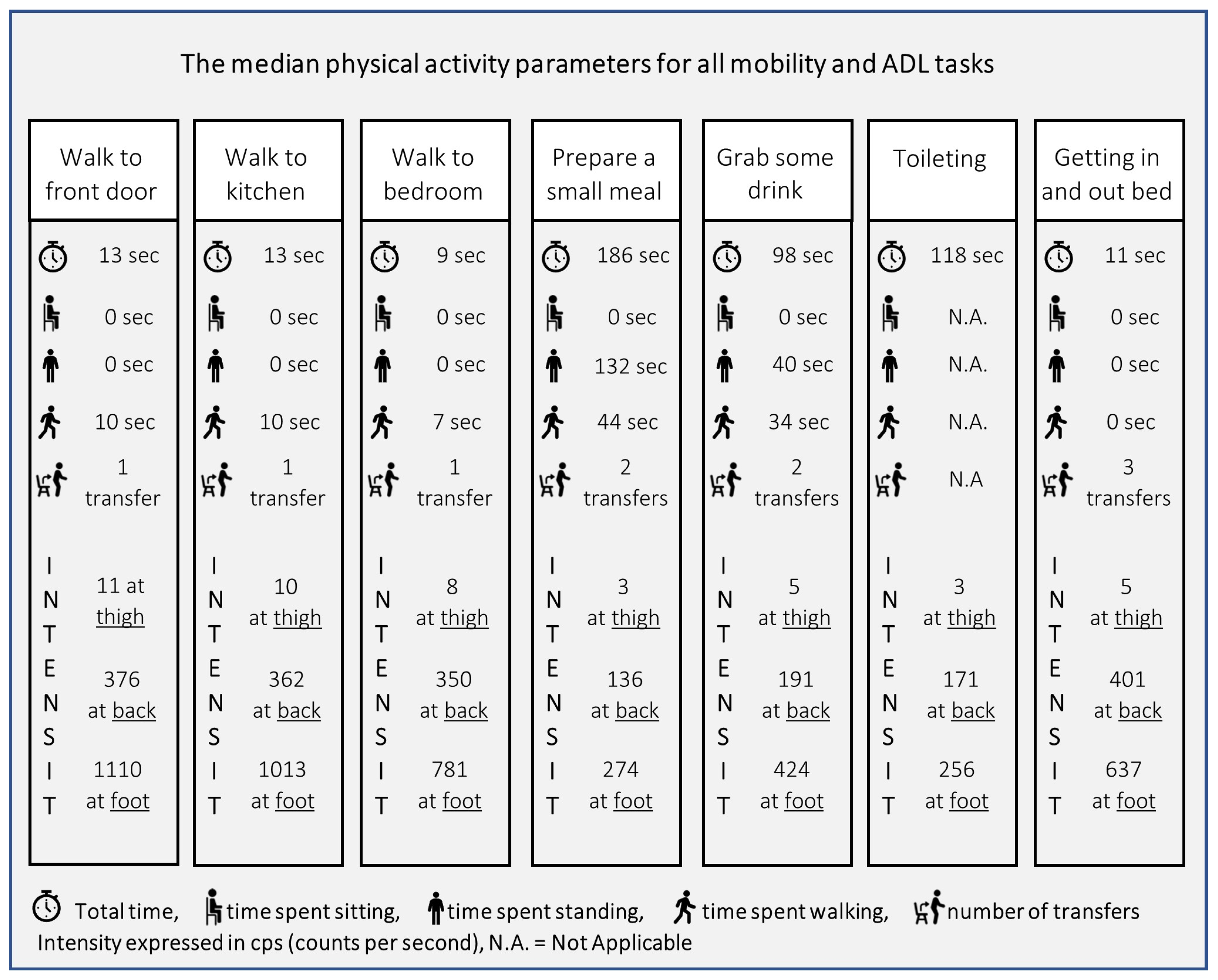
3.2. Physical Activity Parameters
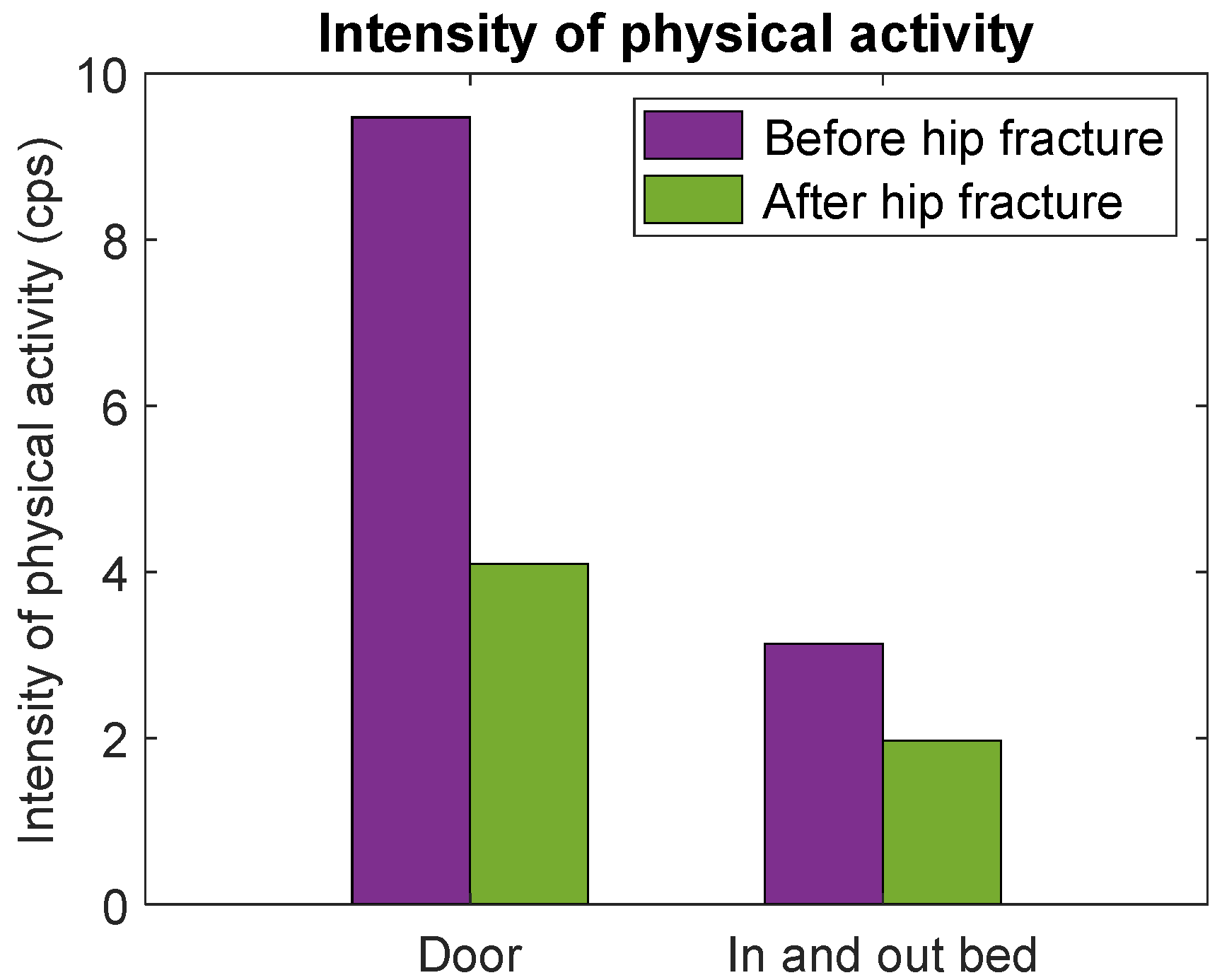
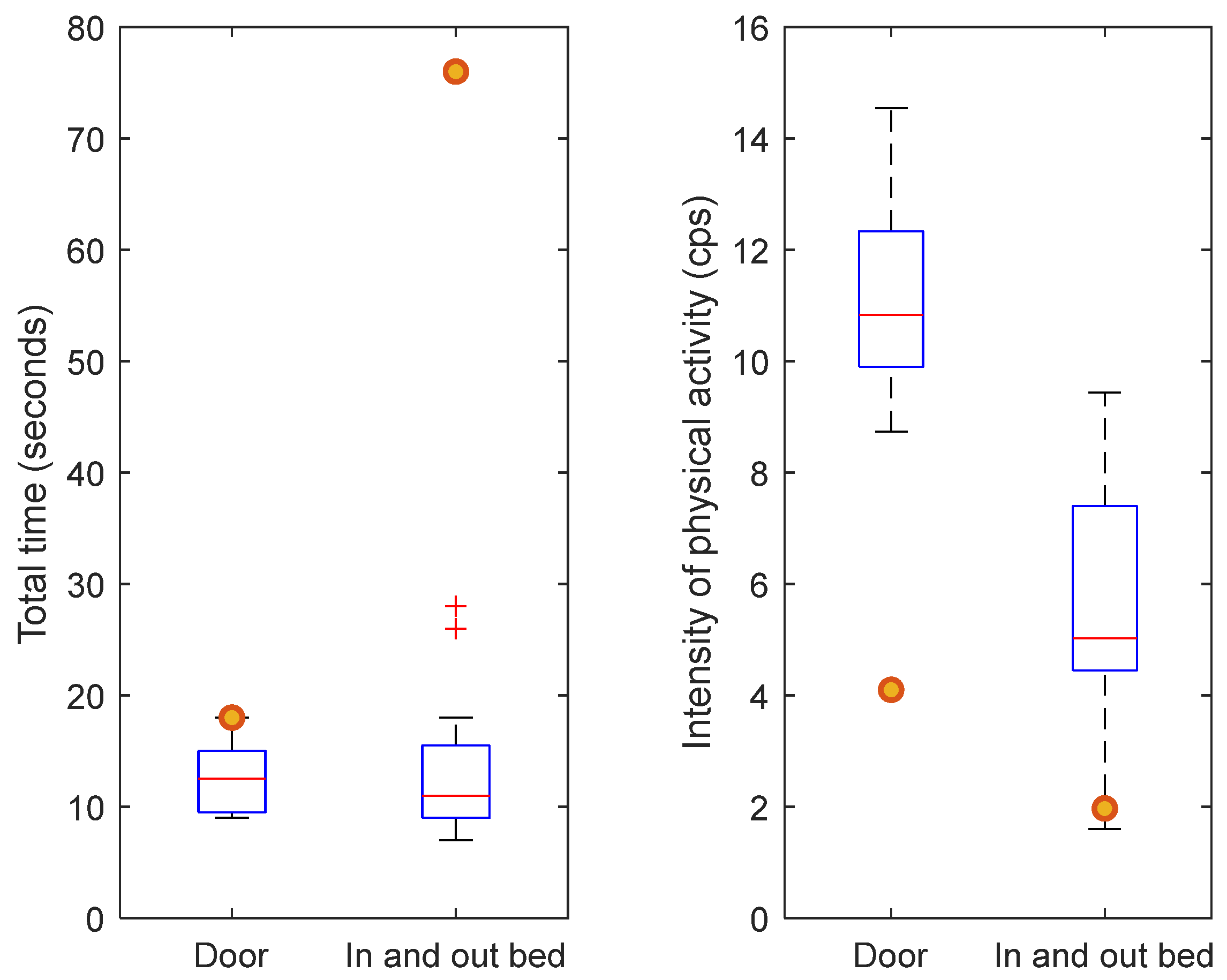
3.3. Case Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kampe, K.; Pfeiffer, K.; Lindemann, U.; Schoene, D.; Taraldsen, K.; Rapp, K.; Becker, C.; Klenk, J. Change of physical activity parameters of hip and pelvic fracture patients during inpatient rehabilitation and after discharge: Analysis of global and in-depth parameters. Eur. Rev. Aging Phys. Act. 2021, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.F.; Peiris, C.L.; Thompson, A.L.; Prendergast, L.A.; Harding, K.E.; Hau, R.; Shields, N. Association between physical activity and short-term physical function changes after hip fracture: An observational study. Physiother. Res. Int. 2021, 26, e1876. [Google Scholar] [CrossRef] [PubMed]
- van Dartel, D.; Wang, Y.; Hegeman, J.H.; Vermeer, M.; Vollenbroek-Hutten, M.M.R.; Broersma, B.; Brouwer, K.; Folbert, E.C.; Gerrits, T.; Gommers, S.M.; et al. Patterns of physical activity over time in older patients rehabilitating after hip fracture surgery: A preliminary observational study. BMC Geriatr. 2023, 23, 373. [Google Scholar] [CrossRef] [PubMed]
- van Dartel, D.; Hegeman, J.H.; Vollenbroek-Hutten, M.M.R. Feasibility and usability of wearable devices for ambulatory monitoring of the rehabilitation process of older patients after hip fracture surgery. In Proceedings of the 18th International Conference on Wireless Networks and Mobile Systems, WINSYS 2021, Online, 7–9 July 2021; SciTePress: Setúbal, Portugal, 2021; Volume 1, pp. 59–66. [Google Scholar]
- Talkowski, J.B.; Lenze, E.J.; Munin, M.C.; Harrison, C.; Brach, J.S. Patient participation and physical activity during rehabilitation and future functional outcomes in patients after hip fracture. Arch. Phys. Med. Rehabil. 2009, 90, 618–622. [Google Scholar] [CrossRef]
- Willems, E.; Visschedijk, J.; Balen, R.; Achterberg, W. Physical Activity, Physical Function and Fear of Falling After Hip Fracture. J. Orthop. Res. Physiother. 2017, 3, 031. [Google Scholar] [CrossRef]
- Taylor, N.F.; Peiris, C.L.; Kennedy, G.; Shields, N. Walking tolerance of patients recovering from hip fracture: A phase I trial. Disabil. Rehabil. 2016, 38, 1900–1908. [Google Scholar] [CrossRef]
- Benzinger, P.; Lindemann, U.; Becker, C.; Aminian, K.; Jamour, M.; Flick, S. Geriatric rehabilitation after hip fracture. Z. Für Gerontol. Geriatr. 2014, 47, 236–242. [Google Scholar] [CrossRef]
- Keppler, A.M.; Holzschuh, J.; Pfeufer, D.; Neuerburg, C.; Kammerlander, C.; Böcker, W.; Fürmetz, J. Postoperative physical activity in orthogeriatric patients–new insights with continuous monitoring. Injury 2020, 51, 628–632. [Google Scholar] [CrossRef]
- Fleig, L.; McAllister, M.M.; Brasher, P.; Cook, W.L.; Guy, P.; Puyat, J.H.; Khan, K.M.; McKay, H.A.; Ashe, M.C. Sedentary behavior and physical activity patterns in older adults after hip fracture: A call to action. J. Aging Phys. Act. 2016, 24, 79–84. [Google Scholar] [CrossRef]
- Klenk, J.; Wekenmann, S.; Schwickert, L.; Lindemann, U.; Becker, C.; Rapp, K. Change of objectively-measured physical activity during geriatric rehabilitation. Sensors 2019, 19, 5451. [Google Scholar] [CrossRef]
- Resnick, B.; Galik, E.; Boltz, M.; Hawkes, W.; Shardell, M.; Orwig, D.; Magaziner, J. Physical activity in the post-hip-fracture period. J. Aging Phys. Act. 2011, 19, 373–387. [Google Scholar] [CrossRef] [PubMed]
- Taraldsen, K.; Vereijken, B.; Thingstad, P.; Sletvold, O.; Helbostad, J.L. Multiple days of monitoring are needed to obtain a reliable estimate of physical activity in hip-fracture patients. J. Aging Phys. Act. 2014, 22, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Kronborg, L.; Bandholm, T.; Palm, H.; Kehlet, H.; Kristensen, M.T. Physical activity in the acute ward following hip fracture surgery is associated with less fear of falling. J. Aging Phys. Act. 2016, 24, 525–532. [Google Scholar] [CrossRef]
- Davenport, S.J.; Arnold, M.; Hua, C.; Schenck, A.; Batten, S.; Taylor, N.F. Physical activity levels during acute inpatient admission after hip fracture are very low. Physiother. Res. Int. 2015, 20, 174–181. [Google Scholar] [CrossRef]
- Taraldsen, K.; Sletvold, O.; Thingstad, P.; Saltvedt, I.; Granat, M.H.; Lydersen, S.; Helbostad, J.L. Physical behavior and function early after hip fracture surgery in patients receiving comprehensive geriatric care or orthopedic care—A randomized controlled trial. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2014, 69, 338–345. [Google Scholar] [CrossRef]
- Zusman, E.Z.; Dawes, M.G.; Edwards, N.; Ashe, M.C. A systematic review of evidence for older adults’ sedentary behavior and physical activity after hip fracture. Clin. Rehabil. 2018, 32, 679–691. [Google Scholar] [CrossRef]
- Keith, R.; Granger, C.; Hamilton, B. The functional independence measure: A new tool for rehabilitstion. Adv. Clin. Rehabil. 1987, 1, 6–18. [Google Scholar]
- Semel, J.; Gray, J.M.; Ahn, H.J.; Nasr, H.; Chen, J.J. Predictors of outcome following hip fracture rehabilitation. Phys. Med. Rehabil. 2010, 2, 799–805. [Google Scholar] [CrossRef]
- Mizrahi, E.; Harel, N.; Heymann, A.; Lubart, E.; Leibovitz, A.; Gadot, E.M.; Barkan, R. The relation between gain in cognition during rehabilitation on functional outcome among hip fracture adult patients with and without pre-hip fracture dementia. Arch. Gerontol. Geriatr. 2018, 78, 177–180. [Google Scholar] [CrossRef]
- McGilton, K.S.; Chu, C.H.; Naglie, G.; van Wyk, P.M.; Stewart, S.; Davis, A.M. Factors influencing outcomes of older adults after undergoing rehabilitation for hip fracture. J. Am. Geriatr. Soc. 2016, 64, 1601–1609. [Google Scholar] [CrossRef]
- Arinzon, Z.; Fidelman, Z.; Zuta, A.; Peisakh, A.; Berner, Y.N. Functional recovery after hip fracture in old-old elderly patients. Arch. Gerontol. Geriatr. 2005, 40, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Hershkovitz, A.; Beloosesky, Y.; Brill, S. Mobility assessment of hip fracture patients during a post-acute rehabilitation program. Arch. Gerontol. Geriatr. 2012, 55, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Hutchings, L.; Fox, R.; Chesser, T. Proximal femoral fractures in the elderly: How are we measuring outcome? Injury 2011, 42, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.A.; Aquilina, A.L.; Costa, M.L. Outcome score measurement and clinical trials for hip fracture patients. Orthop. Trauma. 2016, 30, 159–163. [Google Scholar] [CrossRef]
- de la Torre-García, M.; Hernández-Santana, A.; Moreno-Moreu, N.; Luis-Jacinto, R.; Deive-Maggiolo, J.; Rodríguez, J. Use of the Barthel Index to measure functional recovery in an elderly population after hip fracture. Rev. Española Cirugía Ortopédica Y Traumatol. Engl. Ed. 2011, 55, 263–269. [Google Scholar] [CrossRef]
- Bouwstra, H.; Smit, E.B.; Wattel, E.M.; van der Wouden, J.C.; Hertogh, C.M.; Terluin, B.; Terwee, C.B. Measurement properties of the Barthel Index in geriatric rehabilitation. J. Am. Med. Dir. Assoc. 2019, 20, 420–425, e421. [Google Scholar] [CrossRef]
- Uriz-Otano, F.; Uriz-Otano, J.I.; Malafarina, V. Factors associated with short-term functional recovery in elderly people with a hip fracture. Influence of cognitive impairment. J. Am. Med. Dir. Assoc. 2015, 16, 215–220. [Google Scholar] [CrossRef]
- Bliemel, C.; Buecking, B.; Oberkircher, L.; Knobe, M.; Ruchholtz, S.; Eschbach, D. The impact of pre-existing conditions on functional outcome and mortality in geriatric hip fracture patients. Int. Orthop. 2017, 41, 1995–2000. [Google Scholar] [CrossRef]
- Morandi, A.; Mazzone, A.; Bernardini, B.; Suardi, T.; Prina, R.; Pozzi, C.; Gentile, S.; Trabucchi, M.; Bellelli, G. Association between delirium, adverse clinical events and functional outcomes in older patients admitted to rehabilitation settings after a hip fracture: A multicenter retrospective cohort study. Geriatr. Gerontol. Int. 2019, 19, 404–408. [Google Scholar] [CrossRef]
- Landi, F.; Calvani, R.; Ortolani, E.; Salini, S.; Martone, A.M.; Santoro, L.; Santoliquido, A.; Sisto, A.; Picca, A.; Marzetti, E. The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos. Int. 2017, 28, 1569–1576. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md. State Med. J. 1965, 14, 56–61. [Google Scholar]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Hoang-Kim, A.; Schemitsch, E.; Bhandari, M.; Kulkarni, A.; Beaton, D. Outcome assessment in hip fracture: Evaluation of the practicality of commonly-used outcomes in hip fracture studies. Arch. Orthop. Trauma Surg. 2011, 131, 1687–1695. [Google Scholar] [CrossRef] [PubMed]
- Nygard, H.; Matre, K.; Fevang, J.M. Evaluation of Timed Up and Go Test as a tool to measure postoperative function and prediction of one year walking ability for patients with hip fracture. Clin. Rehabil. 2016, 30, 472–480. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Foss, N.B.; Kehlet, H. Timed “up & go” test as a predictor of falls within 6 months after hip fracture surgery. Phys. Ther. 2007, 87, 24–30. [Google Scholar]
- Nguyen, H.; Lebel, K.; Bogard, S.; Goubault, E.; Boissy, P.; Duval, C. Using inertial sensors to automatically detect and segment activities of daily living in people with Parkinson’s disease. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 26, 197–204. [Google Scholar] [CrossRef]
- Hegde, N.; Bries, M.; Swibas, T.; Melanson, E.; Sazonov, E. Automatic recognition of activities of daily living utilizing insole-based and wrist-worn wearable sensors. IEEE J. Biomed. Health Inform. 2017, 22, 979–988. [Google Scholar] [CrossRef]
- Attal, F.; Mohammed, S.; Dedabrishvili, M.; Chamroukhi, F.; Oukhellou, L.; Amirat, Y. Physical human activity recognition using wearable sensors. Sensors 2015, 15, 31314–31338. [Google Scholar] [CrossRef]
- Bidargaddi, N.; Sarela, A. Ambulatory monitor derived clinical measures for continuous assessment of cardiac rehabilitation patients in a community care model. In Proceedings of the 2008 Second International Conference on Pervasive Computing Technologies for Healthcare, Tampere, Finland, 30 January–1 February 2008; IEEE: Piscataway, NJ, USA, 2008; pp. 232–236. [Google Scholar]
- Spenkelink, C.; Hutten, M.M.; Hermens, H.; Greitemann, B.O. Assessment of activities of daily living with an ambulatory monitoring system: A comparative study in patients with chronic low back pain and nonsymptomatic controls. Clin. Rehabil. 2002, 16, 16–26. [Google Scholar] [CrossRef]
- Sun, V.; Dumitra, S.; Ruel, N.; Lee, B.; Melstrom, L.; Melstrom, K.; Woo, Y.; Sentovich, S.; Singh, G.; Fong, Y. Wireless Monitoring Program of Patient-Centered Outcomes and Recovery Before and After Major Abdominal Cancer Surgery. JAMA Surg. 2017, 152, 852–859. [Google Scholar] [CrossRef]
- Maastricht Instrument BV. Hospital Fit. Available online: https://www.accelerometry.eu/hospital-fit/ (accessed on 29 November 2020).
- APDM. Mobility Lab. Available online: https://www.apdm.com/mobility/ (accessed on 29 November 2020).
- (LASA), L.A.S.A. Sedentary Behavior Differences. Available online: https://lasa-vu.nl/en/lasa-main-study/lsn/sedentair_diff/ (accessed on 3 November 2024).
- Bijnens, W.; Aarts, J.; Stevens, A.; Ummels, D.; Meijer, K. Optimization and validation of an adjustable activity classification algorithm for assessment of physical behavior in elderly. Sensors 2019, 19, 5344. [Google Scholar] [CrossRef] [PubMed]
- Mathie, M.J.; Coster, A.C.; Lovell, N.H.; Celler, B.G. Accelerometry: Providing an integrated, practical method for long-term, ambulatory monitoring of human movement. Physiol. Meas. 2004, 25, R1-20. [Google Scholar] [CrossRef] [PubMed]
- Preece, S.J.; Goulermas, J.Y.; Kenney, L.P.; Howard, D.; Meijer, K.; Crompton, R. Activity identification using body-mounted sensors—A review of classification techniques. Physiol. Meas. 2009, 30, R1-33. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, Q.D.; Moodie, E.M.; Forget, M.-F.; Desmarais, P.; Keezer, M.R.; Wolfson, C. Health Heterogeneity in Older Adults: Exploration in the Canadian Longitudinal Study on Aging. J. Am. Geriatr. Soc. 2021, 69, 678–687. [Google Scholar] [CrossRef] [PubMed]
- Nijmeijer, W.S.; van Dartel, D.; de Groot, R.; Woudsma, S.; Folbert, E.C.; den Braber, N.; Vermeer, M.; Hegeman, J.H.; Vollenbroek-Hutten, M.M. Transparency in hip fracture recovery over institutional boundaries: The transmural monitoring pathway. Clin. Rehabil. 2023, 37, 1406–1419. [Google Scholar] [CrossRef]
- Mayoral, A.P.; Ibarz, E.; Gracia, L.; Mateo, J.; Herrera, A. The use of Barthel index for the assessment of the functional recovery after osteoporotic hip fracture: One year follow-up. PLoS ONE 2019, 14, e0212000. [Google Scholar] [CrossRef]
- Amata, O.; Panella, L.; Incorvaia, C.; Tomba, A.; Gervasoni, F.; Caserta, A.V.; Callegari, C. Role of frailty in functional recovery after hip fracture, the variable impact in restoring autonomy. Acta Biomed. 2022, 92, e2021387. [Google Scholar] [CrossRef]
- World Health Organization. Physical Activity. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 24 November 2022).
- Ramsey, K.A.; Rojer, A.G.; D’Andrea, L.; Otten, R.H.; Heymans, M.W.; Trappenburg, M.C.; Verlaan, S.; Whittaker, A.C.; Meskers, C.G.; Maier, A.B. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2021, 67, 101266. [Google Scholar] [CrossRef]
- Marzetti, E.; Calvani, R.; Tosato, M.; Cesari, M.; Di Bari, M.; Cherubini, A.; Broccatelli, M.; Savera, G.; D’Elia, M.; Pahor, M. Physical activity and exercise as countermeasures to physical frailty and sarcopenia. Aging Clin. Exp. Res. 2017, 29, 35–42. [Google Scholar] [CrossRef]
- Tolley, A.P.L.; Ramsey, K.A.; Rojer, A.G.M.; Reijnierse, E.M.; Maier, A.B. Objectively measured physical activity is associated with frailty in community-dwelling older adults: A systematic review. J. Clin. Epidemiol. 2021, 137, 218–230. [Google Scholar] [CrossRef]
- Marks, R.; Allegrante, J.P.; MacKenzie, C.R.; Lane, J.M. Hip fractures among the elderly: Causes, consequences and control. Ageing Res. Rev. 2003, 2, 57–93. [Google Scholar] [CrossRef] [PubMed]
- van Dartel, D.; Vermeer, M.; Folbert, E.C.; Arends, A.J.; Vollenbroek-Hutten, M.M.; Hegeman, J.H.; Arends, A.; Blom, B.; Calf, A.; van Eijk, M. Early Predictors for Discharge to Geriatric Rehabilitation after Hip Fracture Treatment of Older Patients. J. Am. Med. Dir. Assoc. 2021, 22, 2454–2460. [Google Scholar] [CrossRef] [PubMed]
Needed activity for toileting: |
Needed activity for moving around the house:  |
Needed activity for getting in and out of bed: |
Needed activity for preparing a meal:  |
| Walk to the Front Door a | Walk to Kitchen b | Walk to Bedroom c | Prepare a Small Meal d | Grab a Drink e | Toileting f | Getting in an Out Bed | ||
|---|---|---|---|---|---|---|---|---|
| Total time (seconds) | Median | 13 | 13 | 9 | 186 | 98 | 118 | 11 |
| IQR | 10–15 | 11–15 | 8–11 | 141–201 | 72–151 | 77–144 | 9–16 | |
| Min | 9 | 9 | 7 | 94 | 26 | 37 | 7 | |
| Max | 18 | 35 | 19 | 326 | 324 | 229 | 28 | |
| Time spent sitting (seconds) | Median | 0 | 0 | 0 | 0 | 0 | N.A. | 0 |
| IQR | 0-0 | 0-0 | 0-0 | 0-0 | 0-0 | N.A. | 0–4 | |
| Min | 0 | 0 | 0 | 0 | 0 | N.A. | 0 | |
| Max | 0 | 0 | 0 | 0 | 0 | N.A. | 14 | |
| Time spent standing (seconds) | Median | 0 | 0 | 0 | 132 | 40 | N.A. | 0 |
| IQR | 0-0 | 0–2 | 0-0 | 93–153 | 31–82 | N.A. | 0-0 | |
| Min | 0 | 0 | 0 | 47 | 5 | N.A. | 0 | |
| Max | 2 | 20 | 6 | 262 | 220 | N.A. | 0 | |
| Time spent walking (seconds) | Median | 10 | 10 | 7 | 44 | 34 | N.A. | 0 |
| IQR | 8–12 | 8–10 | 6–8 | 34–54 | 27–48 | N.A. | 0-0 | |
| Min | 7 | 6 | 5 | 23 | 15 | N.A. | 0 | |
| Max | 14 | 13 | 9 | 64 | 114 | N.A. | 0 | |
| Number of transfers (n) | Median | 1 | 1 | 1 | 2 | 2 | N.A. | 3 |
| IQR | 1-1 | 1-1 | 1-1 | 2-2 | 2-2 | N.A. | 2-3 | |
| Min | 1 | 1 | 1 | 2 | 2 | N.A. | 2 | |
| Max | 1 | 1 | 1 | 2 | 2 | N.A. | 4 | |
| Mean intensity of physical activity thigh (cps) | Median | 11 | 10 | 8 | 3 | 5 | 3 | 5 |
| IQR | 10–12 | 9–11 | 8–11 | 3–4 | 4–6 | 3–4 | 4–7 | |
| Min | 9 | 3 | 6 | 2 | 2 | 2 | 2 | |
| Max | 15 | 13 | 15 | 6 | 10 | 6 | 9 | |
| Mean intensity of physical activity lower back (cps) | Median | 376 | 362 | 350 | 136 | 191 | 171 | 401 |
| IQR | 319–420 | 314–386 | 333–391 | 115–151 | 162–239 | 136–203 | 321–444 | |
| Min | 276 | 144 | 265 | 72 | 85 | 96 | 156 | |
| Max | 508 | 489 | 546 | 192 | 332 | 267 | 679 | |
| Mean intensity of physical activity on the right foot (cps) | Median | 1110 | 1013 | 781 | 274 | 424 | 256 | 637 |
| IQR | 1011–1237 | 917–1191 | 656–955 | 243–358 | 404–582 | 192–329 | 542–821 | |
| Min | 854 | 259 | 537 | 112 | 182 | 125 | 143 | |
| Max | 1559 | 1584 | 1510 | 495 | 1070 | 596 | 1130 | |
| Walk to the Front Door a | Walk to Kitchen b | Walk to Bedroom c | Prepare a Small Meal d | Grab A Drink e | Toileting f | Getting in an Out Bed | ||
|---|---|---|---|---|---|---|---|---|
| Total time; median (seconds) | Group 1 | 9 | 10 | 9 | 153 | 88 | 91 | 9 |
| Group 2 | 14 | 13 | 10 | 194 | 98 | 120 | 13 | |
| Number of transfers; median (n) | Group 1 | 1 | 1 | 1 | 2 | 2 | N.A. | 2 |
| Group 2 | 1 | 1 | 1 | 2 | 2 | N.A. | 3 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Dartel, D.; Wang, Y.; Hegeman, J.H.; Vollenbroek-Hutten, M.M.R. Physical Activity Levels of Community-Dwelling Older Adults During Daily Life Activities: A Descriptive Study. Healthcare 2024, 12, 2575. https://doi.org/10.3390/healthcare12242575
van Dartel D, Wang Y, Hegeman JH, Vollenbroek-Hutten MMR. Physical Activity Levels of Community-Dwelling Older Adults During Daily Life Activities: A Descriptive Study. Healthcare. 2024; 12(24):2575. https://doi.org/10.3390/healthcare12242575
Chicago/Turabian Stylevan Dartel, Dieuwke, Ying Wang, Johannes H. Hegeman, and Miriam M. R. Vollenbroek-Hutten. 2024. "Physical Activity Levels of Community-Dwelling Older Adults During Daily Life Activities: A Descriptive Study" Healthcare 12, no. 24: 2575. https://doi.org/10.3390/healthcare12242575
APA Stylevan Dartel, D., Wang, Y., Hegeman, J. H., & Vollenbroek-Hutten, M. M. R. (2024). Physical Activity Levels of Community-Dwelling Older Adults During Daily Life Activities: A Descriptive Study. Healthcare, 12(24), 2575. https://doi.org/10.3390/healthcare12242575


_MD__MPH_PhD.png)



