Abstract
Background/Objectives: Perineal injuries, including episiotomies and spontaneous tears, are common complications during childbirth, often leading to significant discomfort and prolonged recovery for women. This retrospective observational cohort study aimed to explore the relationship between antenatal anovaginal distance (AVD) and the incidence of perineal injuries in a cohort of pregnant women evaluated for pelvic floor health at 28 to 32 weeks of gestation. Methods: Conducted at the University Hospital of Padua over 18 months, the study included 416 women who underwent vaginal delivery at term. Based on AVD, the study participants were divided into two groups: AVD-N group, which included 252 patients with AVD ≥ 2 cm, and the AVD-R group, which included 164 with AVD < 2 cm. The results of the pelvic floor assessment and those related to childbirth were then examined in relation to AVD (reduced vs. normal). Results: The study found that women with reduced AVD were more likely to experience perineal injuries. Specifically, the incidence of episiotomy and severe perineal tears (3rd and 4th degree) was significantly higher in the reduced AVD group (p < 0.05). Furthermore, a lower AVD was associated with increased perineal muscle hypertonicity and a higher likelihood of operative delivery with episiotomy. Logistic regression analysis confirmed that reduced AVD was an independent risk factor for perineal injuries, regardless of other maternal or neonatal characteristics. Conclusions: These results suggest that AVD measurement during pregnancy may help identify women at higher risk of perineal trauma, enabling more personalized obstetric care to mitigate these outcomes.
1. Introduction
Childbirth-related perineal trauma is a common complication during vaginal delivery, often leading to short-term and long-term maternal morbidity [1]. Perineal trauma refers to damage to the skin, muscles of the perineum, and the anal sphincter complex, including the anal epithelium, and typically results from either spontaneous laceration or an incision made during vaginal delivery [2]. These injuries are common outcomes after vaginal birth, affecting nearly 90% of women. Second-degree perineal tears are particularly prevalent, occurring twice as often in first-time births, with an incidence rate of around 40%. Obstetric anal sphincter injuries occur in approximately 3% of vaginal deliveries, with a significantly higher occurrence in first-time mothers compared to those who have previously given birth (6% vs. 2%) [3].
Several risk factors contribute to the occurrence of perineal trauma during childbirth. These include first-time vaginal births, maternal ethnicity (particularly Southeast Asian background), maternal age over 35 years, large birth weight or head circumference, fetal malposition, prolonged second stage of labor, and instrumental deliveries [4,5].
Perineal trauma can lead to a range of health issues with varying impacts on a woman’s quality of life. These issues include perineal pain, wound dehiscence, infections, dyspareunia, sexual dysfunction, and urinary or fecal incontinence [6,7,8,9]. Consequently, it is crucial for clinicians and midwives to provide evidence-based care to mitigate these physical and psychological symptoms.
The perineum, a soft tissue area extending from the anus to the posterior border of the vulvar vestibule, plays a critical role in childbirth. During pregnancy, increased blood flow occurs in this region, and the overstretching that can happen during vaginal delivery may result in trauma [10]. Perineal size and other anatomical parameters, including anovaginal distance (AVD) have recently emerged as potential anatomical predictors of perineal injury during childbirth. AVD is influenced by several factors, including maternal age, body mass index (BMI), and hormonal changes during pregnancy [11,12]. The perineum’s ability to accommodate the descending fetal head is essential in preventing tears, and a shorter perineum might predispose women to higher tension and thus, a higher injury risk [13]. Several studies have suggested that women with a shorter perineal length are more likely to undergo episiotomy and have a significantly higher risk of third- and fourth-degree perineal tears during vaginal delivery [14,15].
Despite these associations, there is limited data on how AVD measurements in the prenatal period correlate with perineal outcomes post-delivery. Previous studies have highlighted the importance of perineal body length and other anatomical parameters in predicting the likelihood of perineal tears during vaginal delivery [3,15,16,17]. However, most of these studies have focused on evaluating these parameters immediately before, during, or after childbirth—when intervention is no longer possible, and the opportunity to influence these outcomes has passed. Investigating the relationship between anovaginal distance (AVD) assessed during the gestational age of 28 to 32 weeks offers a valuable and underexplored window of opportunity. This period is early enough to identify women at higher risk of perineal trauma, allowing for the implementation of targeted prevention strategies before delivery. Such interventions could focus on improving muscle elasticity and promoting perineal stretching, thereby reducing the risk of tearing or the need for episiotomy during childbirth [7,18]. Moreover, understanding this relationship could enhance individualized risk assessment, enabling clinicians to tailor their management approaches more effectively. This study, therefore, seeks to fill a gap in the literature by evaluating the association between AVD and perineal outcomes, with the aim of contributing to improved strategies for preventing perineal trauma during childbirth.
2. Materials and Methods
2.1. Design and Patients
This observational retrospective cohort study was conducted at the Breastfeeding and Pelvic Floor Clinic of the University Hospital of Padua, a tertiary university hospital in Padua, Italy. This clinic specializes in the assessment and management of pelvic floor health and supports breastfeeding among new mothers. The study spanned 18 months, from 1 January 2023 to 31 June 2024, and included consecutive women who underwent perineal assessment at the University Hospital of Padua between 28 and 32 weeks of gestation and subsequently gave birth in the same facility between 37 + 0 and 41 + 6 weeks of gestation. Included in the analysis were all women with vaginal delivery at term. Both spontaneous vaginal deliveries and vacuum-assisted deliveries were included. Exclusion criteria were maternal age under 18 years, obesity (BMI > 30 kg/m2), diabetes, hypertension, preterm or post-term delivery, twin or multiple pregnancies, parity greater than 2, emergency or scheduled cesarean deliveries, macrosomia, and newborn head circumference >35 cm.
2.2. Data Collection
The study utilized data from a preexisting, prospectively maintained electronic database containing records of all deliveries at the hospital during the study period. The database included comprehensive information on patient history, labor and delivery parameters, and maternal and neonatal outcomes (Table 1).

Table 1.
Maternal characteristics, delivery, and neonatal outcomes considered for the study.
2.3. Study Protocol
The data of 472 patients who consecutively visited the clinic for pelvic floor evaluation and gave birth in the same clinic were checked for inclusion in the study. After applying the inclusion/exclusion criteria, 416 women were included in the final analysis. Based on the results obtained from AVD measurements in our study (from 0.5 cm to 4.0 cm) and data from the literature [15], we defined reduced AVD for values <2 cm and normal AVD for values ≥2 cm. According to AVD, the research subjects were split up into two groups: the AVD-N group, which included 252 patients with AVD ≥2 cm, and the AVD-R group, which included 164 with AVD <2 cm. The results of the pelvic floor assessment and those related to childbirth were then examined in relation to AVD (reduced vs. normal).
2.4. Statistical Analysis
Nominal variables are presented as frequencies and percentages, whereas continuous variables are reported as mean values with their corresponding standard deviations.
Data for nominal variables were presented as frequencies and percentages, whereas continuous variables were reported as mean values with their corresponding standard deviations. Associations between categorical variables related to maternal, pelvic, and obstetric characteristics were analyzed using the χ2 test. Quantitative variables were compared using either the two-sample t-test or the Mann-Whitney U test, depending on the Shapiro-Wilk test for normality. ANOVA (the Kruskal-Wallis non-parametric test) was used for analyzing the association between characteristics of the study population and AVD. Post hoc analyses were conducted using the Bonferroni test. A multivariate logistic regression model was developed to account for potential confounders in the association between AVD and perineal injuries. A p-value of ≤0.05 was regarded as the threshold for statistical significance. All analyses were conducted using JASP software (version 19).
3. Results
A total of 416 women, mean age 34.24 ± 3.93 (range 19–46), were included in this retrospective observational cohort study. The average gestational week at AVD assessment was 30.60 ± 1.58 (range 28–32) weeks, and the average AVD was 2.287 cm ± 0.809 (range 0.5–4 cm). The incidence of episiotomy in the entire group was 19.71%, and 242 (58.17%) suffered perineal tears of different degrees. Of the 416 women, 252 (60.58%) had normal AVD (≥2 cm) and 164 (39.42%) had reduced AVD (<2 cm).
Results of the comparative analysis of the two groups, AVD-N (N = 252) and AVD-R (N = 164), across maternal and neonatal evaluated characteristics indicated that both groups had similar means of age and BMI, similar distributions of parity, and were evaluated around the same gestational week (p < 0.05). A significantly higher percentage of women in the AVD-N group had normal perineal tonicity (52.362%) compared to the AVD-R group (31.902%), while hypertonicity was significantly more common in the AVD-R group (63.42%) compared to the AVD-N group (38.89%) (p < 0.001).
Both groups had similar gestational ages at delivery, with no significant difference (p = 0.407). A higher percentage of women in the AVD-N group (57.29%) had a spontaneous vaginal delivery compared to the AVD-R group (43.29%), while OD with episiotomy was more common in the AVD-R group (20.12%) compared to the AVD-N group (6.34%) (p < 0.001).
The mean newborn weight and head circumference were very similar between the two groups, with no significant difference (p < 0.05).
The AVD-R group had a higher rate of episiotomy (35.97%) compared to the AVD-N group (8.66%) (p < 0.001). A significant difference was also observed in the degree of tears at delivery. The AVD-N group had a higher percentage of no tears (49.20%) compared to the AVD-R group (30.49%), whereas 3rd and 4th-degree tears occurred only in the AVD-R group (p < 0.001) (Table 2).

Table 2.
Associations of demographic and clinical characteristics with reduced AVD.
Descriptive analysis of the AVD based on different perineal characteristics, types of delivery, and perineal injuries showed that AVD is generally higher in spontaneous (SD) and induced (ID) deliveries compared to operative deliveries (OD); the presence of an episiotomy in spontaneous deliveries appears to lower the AVD (mean = 1.748) compared to when no episiotomy is performed (mean = 2.404); and AVD decreases with increasing severity of perineal laceration, from grade 0 to grade 4. The most severe lacerations (grade 3 and 4) are associated with the lowest AVD values, indicating a significant impact of AVD on severe perineal injuries. All results are presented in Table 3 and Figure 1.

Table 3.
Descriptive analysis of AVD based on perineal tonicity, type of delivery and perineal injuries.
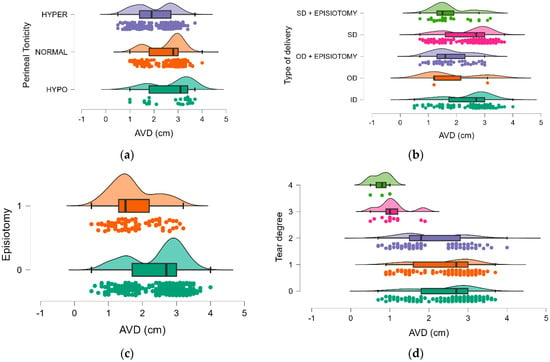
Figure 1.
The distribution of AVD: (a)—by perineal tonicity, (b)—by type of delivery, (c)—by tear degree, (d)—by episiotomy.
Data were further examined using the Kruskal-Wallis test, with Bonferroni post hoc comparison, to determine whether AVD and parameters with a significant difference between the two groups were associated. To achieve this, AVD was used as a continuous variable. There were statistically significant AVD-related differences for all tested parameters (p < 0.05). At the level of perineal tonicity, significant differences in AVD were observed between the hypo and hyper groups, (0.738 cm, p < 0.001) and between the normal and hyper groups (0.531 cm, p < 0.001), suggesting that individuals with hypertonic perineal muscles have a significantly smaller AVD compared to those with hypotonic or normal tonicity. There is no significant difference between the hypo and normal groups (0.208 cm, p = 0.358), indicating that the AVDs are more similar between these two groups.
Regarding the type of delivery, the significant differences were primarily between deliveries with and without episiotomy. ID has a significantly higher AVD compared to OD + episiotomy and SD + episiotomy, suggesting that episiotomy is associated with a reduction in AVD. SD also shows a higher AVD compared to SD with episiotomy, further reinforcing that a lower AVD leads to episiotomy. There are no significant differences between ID and OD, ID and SD, OD and OD + episiotomy, OD and SD, and OD + episiotomy and SD + episiotomy.
The mean AVD was higher in the group without episiotomy (2.427 cm) compared to the group with episiotomy (1.718 cm). This indicates that the anovaginal distance is generally shorter when an episiotomy is performed. The results indicate that there are significant differences in AVD as the degree of perineal tear increases from 0 to 4 (p < 0.05). Particularly, larger differences in AVD were registered as the tear degree increases, with tear degrees 3 and 4 associated with much lower AVD compared to lower degrees. The non-significant results between tear degrees 0 and 1 Mean Difference = 0.035, p-value = 1.000), as well as between 3 and 4 Mean Difference = 0.310, p-value = 1.000) suggest that AVD does not change as much between these adjacent degrees (Table 4).

Table 4.
Post hoc comparisons for association between AVD, perineal tonicity, type of delivery, episiotomy, and tear degree.
Two logistic regression analyses were conducted, incorporating all relevant factors as independent variables and perineal injury (episiotomy and perineal tears) as dependent variables. Continuous variables included age, BMI, newborn weight (g), and newborn head circumference (cm). The categorical variables were assigned specific numerical values for analysis: episiotomy: 0 = no episiotomy, 1 = episiotomy, tear degree 0 = no (laceration grades 0 and 1), 1 = yes (laceration grades 2, 3 and 4), AVD: <2 = reduced, AVD ≥2 cm = normal.
After adjusting for confounding factors, the odds ratio (OR) remained statistically significant at 3.588 (95% CI 0.972–1.120) for predicting perineal tears and 6.346 (95% CI 3.560–11.311) for episiotomy (Table 5). The analysis highlights that reduced AVD is a significant risk factor for both perineal tears and episiotomy. It has a strong effect on increasing the likelihood of these injuries, independent of other factors such as age, BMI, and newborn characteristics.

Table 5.
Associations of AVD category with perineal tears and episiotomy.
4. Discussion
Despite extensive research, the effectiveness of interventions to reduce the risk of perineal trauma remains controversial. Understanding the factors that contribute to these injuries is crucial for improving maternal outcomes and guiding clinical practice. Factors such as fetal weight, maternal age, episiotomy, and labor duration have traditionally been studied as predictors of perineal injury [16]. Recently, attention has turned to anatomical measurements, including the AVD [15].
This study aimed to investigate the anovaginal distance (AVD) measured between 28–32 weeks of gestation as a potential determinant of perineal injuries during childbirth.
Our results indicate significant differences between women with normal AVD (AVD-N) and those with reduced AVD (AVD-R) across several key outcomes, particularly regarding perineal tonicity, mode of delivery, and the severity of perineal injuries, suggesting that measuring the anogenital distance at 28–32 weeks of gestation may offer a non-invasive method to predict perineal injury risk during childbirth, potentially guiding interventions to improve maternal outcomes. The gestational age between 28 and 32 weeks was recommended for measuring the AVD because in this period the tissues are still responsive to physiological changes but are not yet under the full stress related to late pregnancy. This gestational age allows a time window that is early enough for prevention strategies to be implemented if high-risk findings are detected.
The study involving 416 women provides insightful data on the relationship between AVD and perineal outcomes during childbirth. The average AVD in the cohort was 2.287 cm, and 60.58% of the women had a normal AVD (≥2 cm), while 39.42% had a reduced AVD (<2 cm).
Comparative analysis showed that women with a reduced AVD were more likely to experience perineal hypertonicity, operative deliveries with episiotomy, and severe perineal tears compared to those with a normal AVD.
In this study, individuals with hypertonic perineal muscles have significantly smaller AVD compared to those with hypotonic or normal tonicity. Pelvic floor hypertonicity occurs when the muscles of the pelvic floor are excessively tense and cannot fully relax. This condition can lead to various pelvic health issues, including constipation, painful intercourse (dyspareunia), urinary urgency, and chronic pelvic pain, and can have a significant impact on a woman’s overall pelvic health and quality of life [20]. According to previous studies, women with higher degrees of dyspareunia are more likely to have third-degree tears during childbirth. This has been linked to the inability of some patients to relax their pelvic floor muscles, suggesting that proper pelvic floor relaxation plays an important role in childbirth [20,21]. These findings highlight the importance of pelvic floor assessment and targeted interventions, such as physical therapy, to help women with hypertonic pelvic floors achieve better muscle relaxation, ultimately supporting safer and less traumatic childbirth experiences.
The AVD-R group has been reregistered a lower rate of spontaneous vaginal deliveries and a higher rate of operative deliveries with episiotomy, showing that a shorter AVD is associated with higher rates of episiotomy and instrumental delivery. Also, subjects with reduced AVD had a significantly higher rate of episiotomy (35.97%) and severe lacerations, including third- and fourth-degree tears, than the AVD-N group. Previous studies have highlighted the importance of perineal body length and other anatomical parameters in predicting the likelihood of perineal tears during vaginal delivery and identified the length of the perineal body as a significant predictor of obstetric anal sphincter injuries (OASIS) [22,23,24,25].
The logistic regression analysis further reinforces this relationship, showing that a reduced AVD is a potential predictor of perineal injuries, including both perineal tears and episiotomy, independent of other factors like age, BMI, and newborn characteristics.
The long-term consequences of these injuries can include pelvic floor dysfunction, leading to urinary or fecal incontinence and pelvic organ prolapse. Women may also experience chronic perineal pain and dyspareunia, negatively affecting their sexual health and overall quality of life [26]. These physical symptoms can contribute to emotional distress, anxiety, and depression, further complicating postpartum recovery and reducing long-term well-being [27,28].
Clinically, assessing AVD during pregnancy, particularly between 28 and 32 weeks, allows for early identification of women at higher risk of perineal trauma. This enables the implementation of targeted prevention strategies, such as pelvic floor training to improve muscle elasticity, antenatal perineal massage to enhance flexibility, and, in some cases, considering alternative delivery methods to minimize trauma. Evidence suggests that starting perineal massage in the third trimester can improve muscle elasticity and aid in perineal stretching during childbirth, potentially reducing the likelihood of tearing or the need for an episiotomy [3,7]. Also, perineal support techniques or alternative birthing positions could be considered to mitigate the risk of injury [3]. Additionally, the use of episiotomy for women with reduced AVD should be based on individualized clinical judgment rather than routine practice. Early episiotomy based solely on reduced AVD presents ethical considerations, as it is an invasive procedure with associated risks such as increased pain, infection, and extended recovery time [29,30]. For women who do sustain perineal injuries, focused postpartum rehabilitation can aid in restoring function and alleviating long-term complications [26].
By incorporating AVD measurement into prenatal care, clinicians can improve maternal outcomes and enhance personalized obstetric management. However, our study serves as a preliminary step in understanding the relationship between AVD and perineal injury, and future research should aim to refine this understanding to establish standardized protocols that integrate AVD into clinical decision-making.
This study offers an innovative approach by exploring anovaginal distance (AVD) as a non-invasive predictor of perineal trauma during childbirth. Measuring AVD between 28 and 32 weeks of gestation provides an early opportunity to identify women at high risk of perineal injuries, allowing for timely implementation of preventive strategies. The use of robust statistical analysis strengthens the findings, demonstrating that reduced AVD is associated with a higher risk of episiotomy and severe perineal tears, independent of other factors. Clinically, the study highlights the potential to incorporate AVD measurement into prenatal care, supporting more personalized obstetric management.
Despite the promising findings, the retrospective nature of the study limits its capacity to establish definitive causal relationships and introduces potential biases, such as selection bias and recall bias, and important confounding factors like childbirth position, maternal nutrition, and pelvic floor exercises were not controlled for, which could have influenced the outcomes. Although we employed a standardized protocol for AVD, potential variability in these measurements exists, and further steps to ensure measurement reliability should be taken in future studies. Additionally, the exclusion of women with a BMI greater than 30 restricts the applicability of the results, as obesity is a known risk factor for perineal trauma. Also, the study’s geographic limitation to a single hospital may restrict the generalizability of the findings, requiring broader validation in diverse settings. The lack of standardized protocols for integrating AVD measurement into clinical practice highlights the need for further research to establish its role in routine obstetric care. Lastly, while the study touches on long-term consequences of perineal trauma, future longitudinal studies are necessary to assess these impacts more comprehensively.
This study aims to raise awareness about the prevention of perineal trauma, an issue that remains largely overlooked in obstetrics. Currently, there are no specific guidelines addressing this issue, but we hope that our findings will inspire larger studies that incorporate a more diverse population, control for additional confounders, ensure measurement consistency, and explore long-term outcomes and tailored clinical strategies.
5. Conclusions
This study suggested that early assessment of AVD could serve as a valuable clinical tool for identifying women at risk of severe perineal trauma, allowing for the implementation of personalized preventive strategies or targeted interventions to improve pelvic floor elasticity. The significant number of women with perineal tears and the varying AVD measurements emphasize the need for further research into how AVD can be used to optimize childbirth outcomes, possibly leading to more individualized care plans that reduce the risk of perineal injury.
Author Contributions
Conceptualization, F.V. and C.F.; Data curation, B.M.; Formal analysis, M.M.T. and R.F.; Investigation, F.V., Z.L., M.G., C.P. and B.M.; Methodology, E.C., A.C., M.M.T. and C.F.; Project administration, C.F.; Resources, F.V., E.C., Z.L., M.G. and C.P.; Supervision, E.C. and C.F.; Validation, R.F.; Visualization, E.C. and A.C.; Writing—original draft, F.V., C.P. and A.C.; Writing—review & editing, Z.L., M.G., B.M., M.M.T. and R.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Scientific Research Ethics Commission of the Western University “Vasile Goldiș”, Arad (18/26 March 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Aguiar, M.; Farley, A.; Hope, L.; Amin, A.; Shah, P.; Manaseki-Holland, S. Birth-Related Perineal Trauma in Low- and Middle-Income Countries: A Systematic Review and Meta-analysis. Matern. Child Health J. 2019, 23, 1048–1070. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Webb, S.; Manresa, M.; Hodgetts-Morton, V.; Morris, R.K. The Incidence of Wound Infection and Dehiscence Following Childbirth-Related Perineal Trauma: A Systematic Review of the Evidence. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Okeahialam, N.A.; Sultan, A.H.; Thakar, R. The Prevention of Perineal Trauma during Vaginal Birth. Am. J. Obstet. Gynecol. 2024, 230, S991–S1004. [Google Scholar] [CrossRef] [PubMed]
- Marschalek, M.L.; Worda, C.; Kuessel, L.; Koelbl, H.; Oberaigner, W.; Leitner, H.; Marschalek, J.; Husslein, H. Risk and Protective Factors for Obstetric Anal Sphincter Injuries: A Retrospective Nationwide Study. Birth 2018, 45, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.N.; Homer, C.S.E. Third- and Fourth-Degree Tears: A Review of the Current Evidence for Prevention and Management. Aust. N. Z. J. Obstet. Gynaecol. 2020, 60, 175–182. [Google Scholar] [CrossRef]
- Smith, V.; Guilliland, K.; Dixon, L.; Reilly, M.; Keegan, C.; McCann, C.; Begley, C. Irish and New Zealand Midwives’ Expertise at Preserving the Perineum Intact (the MEPPI Study): Perspectives on Preparations for Birth. Midwifery 2017, 55, 83–89. [Google Scholar] [CrossRef]
- Villani, F.; Furau, C.; Mazzucato, B.; Cavalieri, A.; Todut, O.C.; Ciobanu, V.; Dodi, G.; Petre, I. Antenatal Perineal Training for Injuries Prevention: Follow Up after Puerperium. Medicina 2024, 60, 1264. [Google Scholar] [CrossRef]
- Bączek, G.; Rzońca, E.; Sys, D.; Rychlewicz, S.; Durka, A.; Rzońca, P.; Bień, A. Spontaneous Perineal Trauma during Non-Operative Childbirth—Retrospective Analysis of Perineal Laceration Risk Factors. Int. J. Environ. Res. Public Health 2022, 19, 7653. [Google Scholar] [CrossRef]
- Sun, R.; Huang, J.; Zhu, X.; Hou, R.; Zang, Y.; Li, Y.; Pan, J.; Lu, H. Effects of Perineal Warm Compresses During the Second Stage of Labor on Reducing Perineal Trauma and Relieving Postpartum Perineal Pain in Primiparous Women: A Systematic Review and Meta-Analyses. Healthcare 2024, 12, 702. [Google Scholar] [CrossRef]
- O’Kelly, S.M.; Moore, Z.E. Antenatal Maternal Education for Improving Postnatal Perineal Healing for Women Who Have Birthed in a Hospital Setting. Cochrane Database Syst. Rev. 2017, 12, CD012258. [Google Scholar] [CrossRef]
- Hjertberg, L.; Uustal, E.; Pihl, S.; Blomberg, M. Maternal Body Mass Index and Anovaginal Distance in Active Phase of Term Labor. BioMed Res. Int. 2018, 2018, 1532949. [Google Scholar] [CrossRef] [PubMed]
- Jain, V.G.; Goyal, V.; Chowdhary, V.; Swarup, N.; Singh, R.J.; Singal, A.; Shekhawat, P. Anogenital distance is determined during early gestation in humans. Hum. Reprod. 2018, 33, 1619–1627. [Google Scholar] [CrossRef] [PubMed]
- Djusad, S.; Purwosunu, Y.; Hidayat, F. Relationship between perineal body length and degree of perineal tears in primigravidas undergoing vaginal delivery with episiotomy. Obstet. Gynecol. Int. 2021, 2021, 2621872. [Google Scholar] [CrossRef]
- Moya-Jiménez, L.C.; Sánchez-Ferrer, M.L.; Adoamnei, E.; Mendiola, J. New approach to the evaluation of perineal measurements to predict the likelihood of the need for an episiotomy. Int. Urogynecol. J. 2019, 30, 815–821. [Google Scholar] [CrossRef]
- Pihl, S.; Uustal, E.; Blomberg, M. Anovaginal distance and obstetric anal sphincter injury: A prospective observational study. Int. Urogynecol. J. 2019, 30, 939–944. [Google Scholar] [CrossRef]
- Jansson, M.H.; Franzén, K.; Hiyoshi, A.; Tegerstedt, G.; Dahlgren, H.; Nilsson, K. Risk factors for perineal and vaginal tears in primiparous women—The prospective POPRACT-cohort study. BMC Pregnancy Childbirth 2020, 20, 749. [Google Scholar] [CrossRef] [PubMed]
- Aytan, H.; Tapisiz, O.L.; Tuncay, G.; Avsar, F.A. Severe Perineal Lacerations in Nulliparous Women and Episiotomy Type. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005, 121, 46–50. [Google Scholar] [CrossRef]
- Beckmann, M.M.; Stock, O.M. Antenatal Perineal Massage for Reducing Perineal Trauma. Cochrane Database Syst. Rev. 2013, 4, CD005123. [Google Scholar] [CrossRef]
- SIGO Guidelines Recommendations on Prevention, Recognition and Treatment of Obstetric Perineal Trauma (April 2024). Available online: https://www.sigo.it/linee-guida/nazionali/ (accessed on 8 October 2024).
- Rosenbaum, T.Y.; Padoa, A. Managing pregnancy and delivery in women with sexual pain disorders. J. Sex. Med. 2012, 9, 1726–1735. [Google Scholar] [CrossRef]
- Alon, R.; Shimonovitz, T.; Brecher, S.; Shick-Nave, L.; Lev-Sagie, A. Delivery in patients with dyspareunia—A prospective study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 237, 131–136. [Google Scholar] [CrossRef]
- Mboua Batoum, V.; Ngo Um Meka, E.; Essiben, F.; Robinson, M.E. Perineal body length and prevention of perineal lacerations during delivery in Cameroonian primigravid patients. Int. J. Gynaecol. Obstet. 2021, 154, 481–484. [Google Scholar] [CrossRef]
- Geller, E.J.; Robinson, B.L.; Matthews, C.A.; Celauro, K.P.; Dunivan, G.C.; Crane, A.K.; Ivins, A.R.; Woodham, P.C.; Fielding, J.R. Perineal body length as a risk factor for ultrasound-diagnosed anal sphincter tear at first delivery. Int. Urogynecol. J. 2013, 25, 631–636. [Google Scholar] [CrossRef]
- Packet, B.; Page, A.S.; Cattani, L.; Bosteels, J.; Deprest, J.; Richter, J. Predictive factors for obstetric anal sphincter injury in primiparous women: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2023, 62, 486–496. [Google Scholar] [CrossRef]
- Lane, T.L.; Chung, C.P.; Yandell, P.M.; Kuehl, T.J.; Larsen, W.I. Perineal body length and perineal lacerations during delivery in primigravid patients. Baylor Univ. Med. Cent. Proc. 2017, 30, 151–153. [Google Scholar] [CrossRef][Green Version]
- Villani, F.; Minopoli, B.; Rigano, D.; Furau, C.; Todut, O.C.; Ciobanu, V.; Vornic, I.; Onel, C.; Petre, I. Perineal Rehabilitation in Pelvic Floor Dysfunction: The Benefits of Vaginal Cone Training. Balneo PRM Res. J. 2024, 15, 729. [Google Scholar]
- Peinado Molina, R.A.; Hernández Martínez, A.; Martínez Vázquez, S.; Martínez Galiano, J.M. Influence of Pelvic Floor Disorders on Quality of Life in Women. Front. Public Health 2023, 11, 1180907. [Google Scholar] [CrossRef]
- Rodríguez-Almagro, J.; Hernández Martínez, A.; Martínez-Vázquez, S.; Peinado Molina, R.A.; Bermejo-Cantarero, A.; Martínez-Galiano, J.M. A Qualitative Exploration of the Perceptions of Women Living with Pelvic Floor Disorders and Factors Related to Quality of Life. J. Clin. Med. 2024, 13, 1896. [Google Scholar] [CrossRef]
- van der Pijl, M.; Verhoeven, C.; Hollander, M.; de Jonge, A.; Kingma, E. The Ethics of Consent during Labour and Birth: Episiotomies. J. Med. Ethics 2023, 49, 611–617. [Google Scholar] [CrossRef]
- Bączek, G.; Rychlewicz, S.; Sys, D.; Rzońca, P.; Teliga-Czajkowska, J. Episiotomy for Medical Indications during Vaginal Birth—Retrospective Analysis of Risk Factors Determining the Performance of This Procedure. J. Clin. Med. 2022, 11, 4334. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).