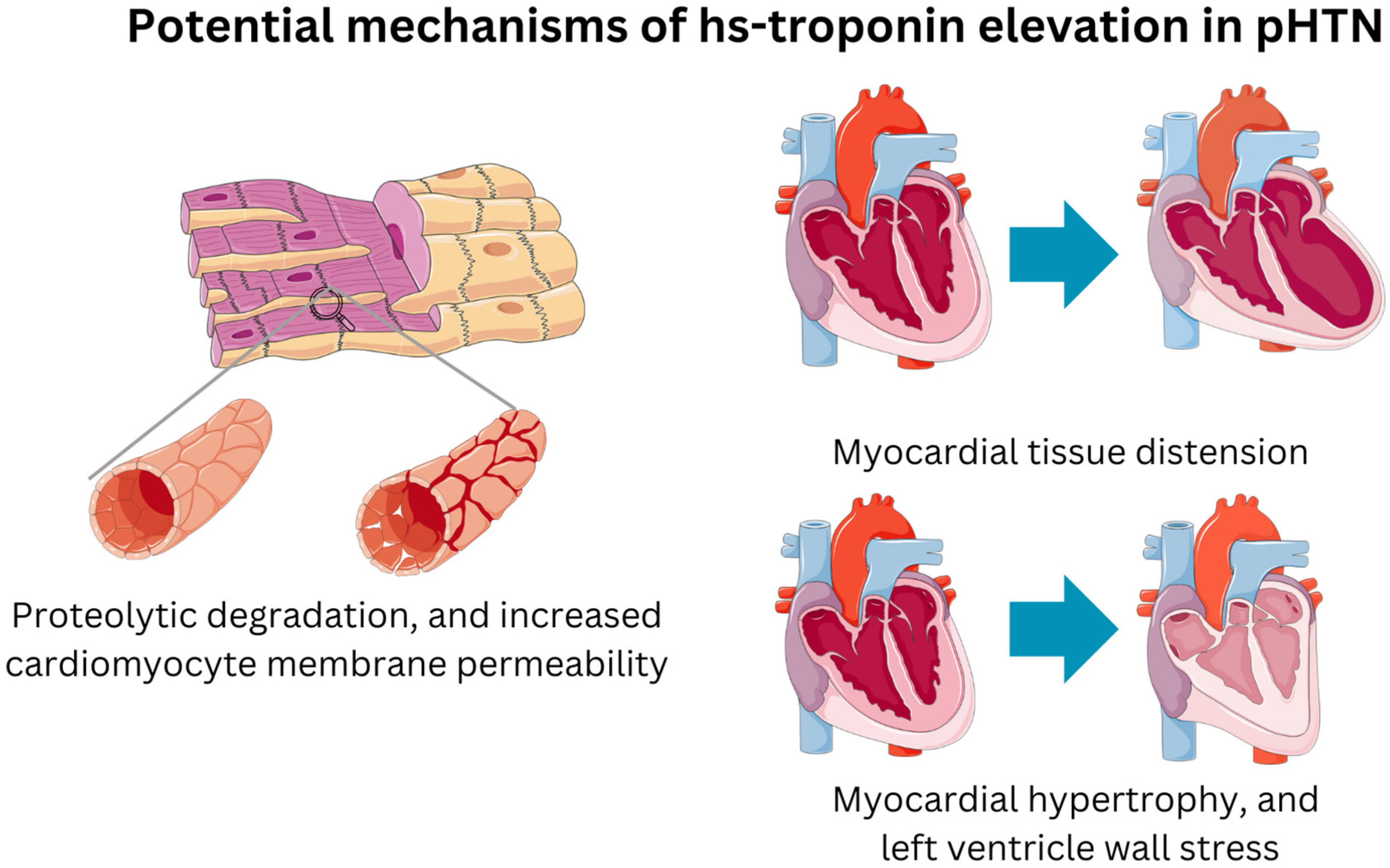
High-Sensitivity Cardiac Troponin [hs-cTn] as a Valuable Biomarker for Pulmonary Hypertension Risk Stratification: A Contemporary Review of the Literature
Abstract
1. Introduction
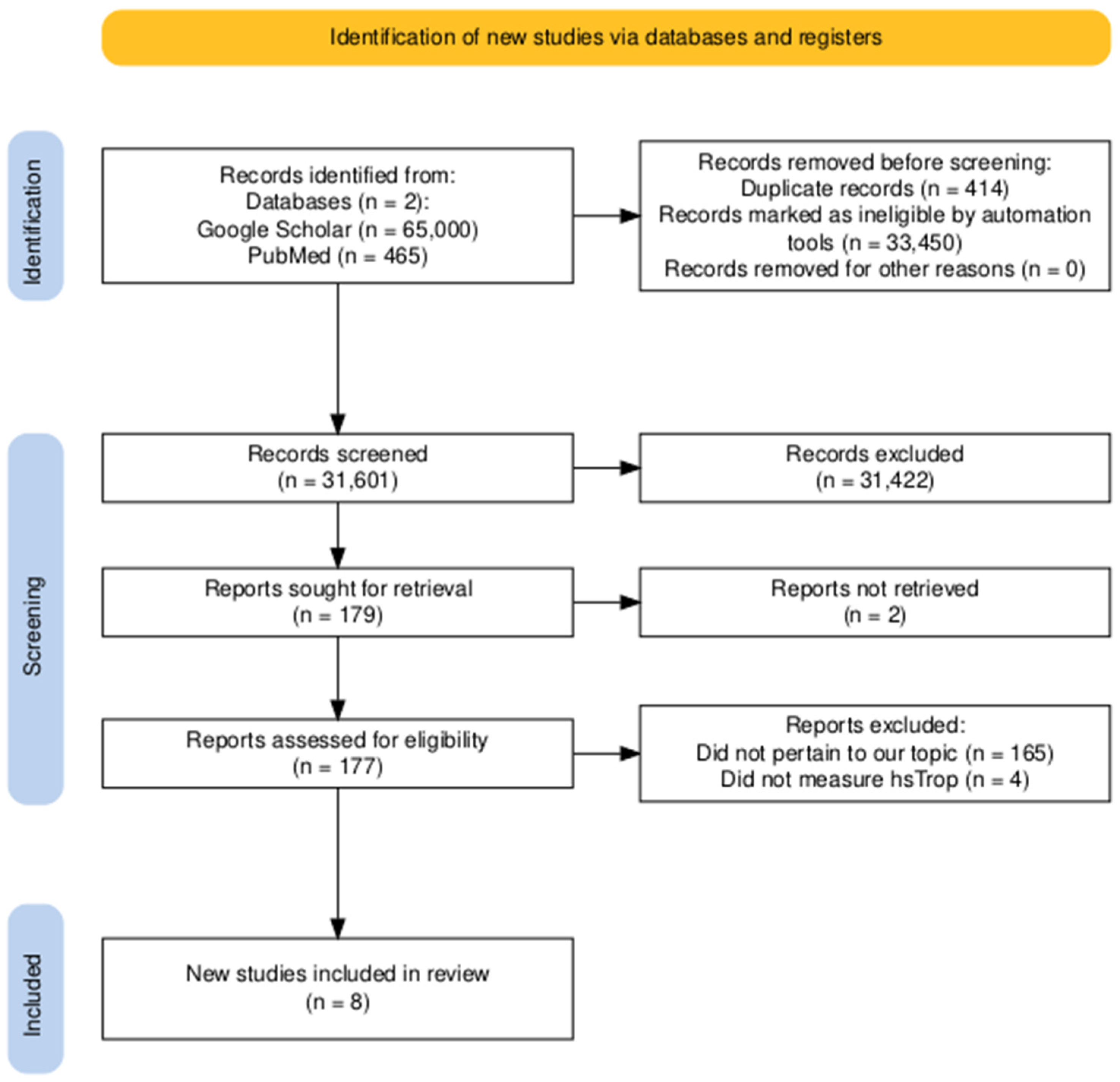
2. Materials and Methods
3. Results
Review of Literature/Evidence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tonelli, A.R.; Arelli, V.; Minai, O.A.; Newman, J.; Bair, N.; Heresi, G.A.; Dweik, R.A. Causes and Circumstances of Death in Pulmonary Arterial Hypertension. Am. J. Respir. Crit. Care Med. 2013, 188, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.-C.; Potoka, K.C.; Champion, H.C.; Mora, A.L.; Gladwin, M.T. Pulmonary Arterial Hypertension: The Clinical Syndrome. Circ. Res. 2014, 115, 115–130. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Kovacs, G.; Hoeper, M.M.; Badagliacca, R.; Berger, R.M.; Brida, M.; Carlsen, J.; Coats, A.J.; Escribano-Subias, P.; Ferrari, P.; et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Respir. J. 2022, 61, 2200879. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.K.; McCullagh, B.N.; Segurado, R.; McGorrian, C.; Keane, E.; Keaney, J.; Fitzgibbon, M.N.; Mahon, N.G.; Murray, P.T.; Gaine, S.P. Detection of high-sensitivity troponin in outpatients with stable pulmonary hypertension identifies a subgroup at higher risk of adverse outcomes. J. Card. Fail. 2014, 20, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Santens, B.; Van De Bruaene, A.; De Meester, P.; D’alto, M.; Reddy, S.; Bernstein, D.; Koestenberger, M.; Hansmann, G.; Budts, W. Diagnosis and treatment of right ventricular dysfunction in congenital heart disease. Cardiovasc. Diagn. Ther. 2020, 10, 1625–1645. [Google Scholar] [CrossRef] [PubMed]
- Raber, I.; McCarthy, C.P.; Januzzi, J.L. A Test in Context: Interpretation of High-Sensitivity Cardiac Troponin Assays in Different Clinical Settings. J. Am. Coll. Cardiol. 2021, 77, 1357–1367. [Google Scholar] [CrossRef]
- Park, K.C.; Gaze, D.C.; O Collinson, P.; Marber, M.S. Cardiac troponins: From myocardial infarction to chronic disease. Cardiovasc. Res. 2017, 113, 1708–1718. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Lockwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. (Eds.) JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2024; Available online: https://synthesismanual.jbi.global (accessed on 25 August 2024).
- Schuuring, M.J.; van Riel, A.C.; Vis, J.C.; Duffels, M.G.; van Straalen, J.P.; Boekholdt, S.M.; Tijssen, J.G.; Mulder, B.J.; Bouma, B.J. High-sensitivity Troponin T Is Associated with Poor Outcome in Adults with Pulmonary Arterial Hypertension due to Congenital Heart Disease. Congenit. Heart Dis. 2012, 8, 520–526. [Google Scholar] [CrossRef]
- Kvisvik, B.; Skjørten, I.; Hilde, J.M.; Strand, H.; Omland, T.; Steine, K. Abstract 17161: High-sensitivity Troponin T Predicts Mortality Independently of Ventricular Dysfunction and Pulmonary Hypertension in Stable Chronic Obstructive Pulmonary Disease. Circulation 2019, 140 (Suppl. S1), A17161. Available online: https://www.ahajournals.org/doi/10.1161/circ.140.suppl_1.17161 (accessed on 25 August 2024).
- Kimura, M.; Kohno, T.; Kawakami, T.; Inohara, T.; Takei, M.; Tsugu, T.; Kataoka, M.; Murata, M.; Maekawa, Y.; Fukuda, K. Abstract 13252: High-sensitivity Troponin T is a Useful Biomarker of Hemodynamics Response After Balloon Pulmonary Angioplasty in Patients With Chronic Thromboembolic Pulmonary Hypertension. Circulation 2015, 132 (Suppl. S3), A13252. [Google Scholar] [CrossRef]
- Heresi, G.; Tang, W.; Aytekin, M.; Hammel, J.; Hazen, S.; Dweik, R. Sensitive cardiac troponin I predicts poor outcomes in pulmonary arterial hypertension. Eur. Respir. J. 2012, 39, 939–944. [Google Scholar] [CrossRef]
- Filusch, A.; Giannitsis, E.; Katus, H.A.; Meyer, F.J. High-sensitive troponin T: A novel biomarker for prognosis and disease severity in patients with pulmonary arterial hypertension. Clin. Sci. 2010, 119, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Kriechbaum, S.D.; Wiedenroth, C.B.; Keller, T.; Wolter, J.S.; Ajnwojner, R.; Peters, K.; Haas, M.A.; Roller, F.C.; Breithecker, A.; Rieth, A.J.; et al. Dynamics of high-sensitivity cardiac troponin T during therapy with balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. PLoS ONE 2018, 13, e0204683. [Google Scholar] [CrossRef] [PubMed]
- Vélez-Martínez, M.; Ayers, C.; Mishkin, J.D.; Bartolome, S.B.; García, C.K.; Torres, F.; Drazner, M.H.; de Lemos, J.A.; Turer, A.T.; Chin, K.M. Association of Cardiac Troponin I with Disease Severity and Outcomes in Patients with Pulmonary Hypertension. Am. J. Cardiol. 2013, 111, 1812–1817. [Google Scholar] [CrossRef] [PubMed]
- Chaulin, A. Cardiac Troponins: Contemporary Biological Data and New Methods of Determination. Vasc. Health Risk Manag. 2021, 17, 299–316. [Google Scholar] [CrossRef]
- Long, B.; Long, D.A.; Tannenbaum, L.; Koyfman, A. An emergency medicine approach to troponin elevation due to causes other than occlusion myocardial infarction. Am. J. Emerg. Med. 2019, 38, 998–1006. [Google Scholar] [CrossRef]
- Chaudary, N.; Geraci, S.A. Prognostic value of cardiac-specific troponins in chronic obstructive pulmonary disease exacerbations: A systematic review. J. Miss. State Med. Assoc. 2014, 55, 40–44. [Google Scholar]
- Wang, T.K.M.; Dugo, C.; Whalley, G.; Wynne, Y.; Semple, H.; Smith, K.; Cleave, P.; Christiansen, J.; To, A.; Amir, N.; et al. Diagnostic Utility of High Sensitivity Troponins for Echocardiographic Markers of Structural Heart Disease. Med. Sci. 2018, 6, 17. [Google Scholar] [CrossRef]
- Masri, W.; Le Guillou, E.; Hamdi, E.; Ghazal, K.; Lebigot, E.; Cosson, C.; Cynober, F.B.; Therond, P. Troponin elevation in other conditions than acute coronary syndromes. Ann. Biol. Clin. 2017, 75, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Chaulin, A. Clinical and Diagnostic Value of Highly Sensitive Cardiac Troponins in Arterial Hypertension. Vasc. Health Risk Manag. 2021, 17, 431–443. [Google Scholar] [CrossRef] [PubMed]
- Sigurdardottir, F.D.; Lyngbakken, M.N.; Holmen, O.L.; Dalen, H.; Hveem, K.; Røsjø, H.; Omland, T. Relative Prognostic Value of Cardiac Troponin I and C-Reactive Protein in the General Population (from the Nord-Trøndelag Health [HUNT] Study). Am. J. Cardiol. 2018, 121, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhang, C.; Xu, S.; Zhao, F.; Liu, L.; Xie, C.; Xing, X.; Zhu, Y. Serum cardiac troponin elevation predicts mortality in patients with pulmonary hypertension: A meta-analysis of eight cohort studies. Clin. Respir. J. 2019, 13, 82–91. [Google Scholar]
| Study ID | Type of Study | Study Population | Methodology | Study Findings |
|---|---|---|---|---|
| Roy et al. [4] | Prospective investigation | 108 subjects attending the National Pulmonary Hypertension Unit in Dublin, Ireland (2007–2009). Connective tissue disease-associated pulmonary hypertension was the most common etiology, present in 33 patients. | Primary outcomes were all-cause mortality and combined clinical endpoint of rehospitalization due to pulmonary hypertension. | hsTnT, BNP, and decrementing 6MWT were independent prognosticators of mortality; hsTnT can discern a PH subgroup with poorer prognosis and might be employed in a risk prediction model. |
| Schuuring et al. [11] | Prospective investigation | 31 subjects with CHD-PAH referred for advanced medical therapy at the Academic Medical Center in Amsterdam. All patients were started on bosentan monotherapy. | The primary outcome was all-cause mortality. Patients with severe renal impairment (eGFR < 30 mL/min) were excluded. | Elevated hsTnT concentrations were observed in 26% of patients; elevated hsTnT concentrations were a predictor of mortality. |
| Kvisvik et al. [12] | Prospective investigation | 112 patients with GOLD stage I–IV COPD were selected for this study. | Hs-cTnT was measured in 98 patients and associations with all-cause mortality were assessed by Cox regression and Kaplan–Meier analysis. | Elevated hs-cTnT levels were associated with the severity of pulmonary hypertension and cardiac dysfunction in patients with stable COPD and were an independent predictor of all-cause mortality. |
| Kimura et al. [13] | Prospective investigation | 63 consecutive chronic thromboembolic pulmonary hypertension (CTEPH) patients who underwent BPA procedures. | Measured hsTnT levels before and after BPA. | Significant improvements in mean pulmonary artery pressure and pulmonary vascular resistance, and significant decrease in hsTnT after BPA; hsTnT-decrease group showed better outcomes compared to hsTnT-increase or stable group. |
| Heresi et al. [14] | Prospective investigation | 68 patients with PAH diagnostic category 1. | cTnI was measured using a sensitive immunoassay with a lower limit of detection of 0.008 ng/mL. Acute coronary syndromes and advanced renal disease, defined as a serum creatinine > 2 mg/dL−1, were excluded. | Detectable cTnI in 25% of PAH patients; patients with detectable cTnI had more advanced functional class symptoms, shorter six-minute walk distance, and higher mortality risk; cTnI was associated with a 4.7-fold increased risk of death related to right ventricular failure or transplant. |
| Filusch et al. [15] | Prospective investigation | 55 PAH patients with a mean pulmonary artery pressure of 45 ± 18 mmHg. | cTnT levels assessed using both a conventional fourth-generation assay and the novel hsTnT assay with a lower limit of detection at 2 pg/mL. | hsTnT assay was more effective in detecting cTnT levels than the fourth-generation assay; patients with higher hsTnT levels had a poorer prognosis; hsTnT was as effective as established biomarkers (hFABP or NT-proBNP) in predicting death and demonstrated a better predictive ability for WHO functional classes > II; hsTnT assay may be valuable in evaluating prognosis and disease severity in PAH patients. |
| Kriechbaum et al. [16] | Post hoc analysis | 51 patients with chronic thromboembolic pulmonary hypertension (CTEPH). | hs-cTnT and NT-proBNP levels before each balloon pulmonary angioplasty (BPA) and at a 6-month follow-up. | Steady decrease in hs-cTnT and NT-proBNP levels, with significant reductions in mean pulmonary arterial pressure (meanPAP) and pulmonary vascular resistance (PVR). |
| Vélez-Martínez et al. [17] | Prognostic observational study | 255 patients diagnosed with pulmonary hypertension. | hsTroponin levels, along with demographic data, hemodynamic assessments, cardiac MRI, and B-type natriuretic peptide levels, with survival analyzed using Kaplan–Meier and Cox regression methods. | With a median follow-up of 3.5 years, higher cTnI levels were associated with worse hemodynamics, structural cardiac abnormalities, and increased mortality, providing prognostic information for patients with PH. |
| Studies/Quality Metrics | Roy et al. [4] | Schuuring et al. [11] | Kvisvik et al. [12] | Kimura et al. [13] | Heresi et al. [14] | Filusch et al. [15] | Kriechbaum et al. [16] | Vélez-Martínez et al. [17] |
|---|---|---|---|---|---|---|---|---|
| Comparability | Yes | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes |
| Matching | Yes | No | No | No | Yes | No | Yes | Yes |
| Standard criteria for identification | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Reliable and standard tools of measurement | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Unclear |
| Consistency in measurement | Yes | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes |
| Confounding Identified | No | Unclear | Unclear | Unclear | No | Unclear | No | Unclear |
| Strategies to address confounding | Yes | Unclear | No | No | Yes | Yes | Yes | Yes |
| Standard assessment method | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Appropriate duration | No | Yes | Yes | Yes | Unclear | Yes | Unclear | Yes |
| Appropriate analysis | Yes | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganipineni, V.D.P.; Jitta, S.R.; Gudiwada, M.C.V.B.; Jasti, J.R.; Janga, C.; Merugu, B.; Bandaru, R.R.; Puli, S.; Venkata, V.S.; Vasavada, A.; et al. High-Sensitivity Cardiac Troponin [hs-cTn] as a Valuable Biomarker for Pulmonary Hypertension Risk Stratification: A Contemporary Review of the Literature. Healthcare 2024, 12, 2037. https://doi.org/10.3390/healthcare12202037
Ganipineni VDP, Jitta SR, Gudiwada MCVB, Jasti JR, Janga C, Merugu B, Bandaru RR, Puli S, Venkata VS, Vasavada A, et al. High-Sensitivity Cardiac Troponin [hs-cTn] as a Valuable Biomarker for Pulmonary Hypertension Risk Stratification: A Contemporary Review of the Literature. Healthcare. 2024; 12(20):2037. https://doi.org/10.3390/healthcare12202037
Chicago/Turabian StyleGanipineni, Vijay Durga Pradeep, Sahas Reddy Jitta, Mohan Chandra Vinay Bharadwaj Gudiwada, Jaswanth Rao Jasti, Chaitra Janga, Bhavyasri Merugu, Revanth Reddy Bandaru, Srikanth Puli, Vikramaditya Samala Venkata, Advait Vasavada, and et al. 2024. "High-Sensitivity Cardiac Troponin [hs-cTn] as a Valuable Biomarker for Pulmonary Hypertension Risk Stratification: A Contemporary Review of the Literature" Healthcare 12, no. 20: 2037. https://doi.org/10.3390/healthcare12202037
APA StyleGanipineni, V. D. P., Jitta, S. R., Gudiwada, M. C. V. B., Jasti, J. R., Janga, C., Merugu, B., Bandaru, R. R., Puli, S., Venkata, V. S., Vasavada, A., & Desai, R. (2024). High-Sensitivity Cardiac Troponin [hs-cTn] as a Valuable Biomarker for Pulmonary Hypertension Risk Stratification: A Contemporary Review of the Literature. Healthcare, 12(20), 2037. https://doi.org/10.3390/healthcare12202037






