Practice Site Heterogeneity within and between Medicaid Accountable Care Organizations
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Contract Participation Measures
2.3. Process Measures
2.4. Outcome Measure
2.5. Practice Site Characteristics
2.6. ACO Characteristics
2.7. Analyses
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abodunde, B.; Slater, C.; Coustasse, A. MACRA and Accountable Care Organizations: Is It Working? J. Ambul. Care Manag. 2020, 44, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Whitman, E. Lured by MACRA bonuses, more Medicare ACOs venture into risk. Mod. Healthc. 2017, 47, 22–24. [Google Scholar] [PubMed]
- Muhlestein, D.B.; Bleser, W.K.; Saunders, R.S.; Richards, R.; Singletary, E.; McClellan, M. Spread of ACOs and Value-Based Payment Models in 2019: Gauging the Impact of Pathways to Success|Health Affairs. Health Affairs Blog. 2019. Available online: https://www.healthaffairs.org/do/10.1377/hblog20191020.962600/full/ (accessed on 31 May 2020).
- Medicaid State ACO Activities. National Association of ACOs. 2021. Available online: https://www.naacos.com/medicaid-acos (accessed on 24 August 2021).
- Winfield, L.; Zollinger, B.; Richards, R.; Gary, C.; Muhlestein, D.B. Medicaid ACO Landscape; Leavitt Partners: Salt Lake City, UT, USA, 2019. [Google Scholar]
- Center for Health Care Strategies, Inc. Medicaid Accountable Care Organizations: State Update; Center for Health Care Strategies, Inc.: Hamilton, NJ, USA, 2018; Available online: https://www.chcs.org/media/ACO-Fact-Sheet-02-27-2018-1.pdf (accessed on 24 August 2021).
- Colla, C.H.; Fisher, E.S. Moving Forward with Accountable Care Organizations: Some Answers, More Questions. JAMA Intern. Med. 2017, 177, 527–528. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McConnell, K.J.; Renfro, S.; Chan, B.K.S.; Meath, T.H.A.; Mendelson, A.; Cohen, D.; Waxmonsky, J.; McCarty, D.; Wallace, N.; Lindrooth, R.C. Early Performance in Medicaid Accountable Care Organizations: A Comparison of Oregon and Colorado. JAMA Intern. Med. 2017, 177, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Medicare Spending after 3 Years of the Medicare Shared Savings Program|NEJM. Available online: https://www.nejm.org/doi/full/10.1056/NEJMsa1803388 (accessed on 16 September 2020).
- McWilliams, J.M.; Chernew, M.E.; Landon, B.E. Medicare ACO Program Savings Not Tied to Preventable Hospitalizations or Concentrated Among High-Risk Patients. Health Aff. 2017, 36, 2085–2093. [Google Scholar] [CrossRef] [PubMed]
- 2019 Medicare Shared Savings Program ACO Performance: Lower Costs and Promising Results Under ‘Pathways To Success’|Health Affairs Blog. Available online: http://www.healthaffairs.org/do/10.1377/hblog20200914.598838/full/ (accessed on 2 March 2021).
- Henke, R.M.; Karaca, Z.; Gibson, T.B.; Cutler, E.; White, C.; Head, M.; Wong, H.S. Medicaid Accountable Care Organizations and Childbirth Outcomes. Med. Care Res. Rev. 2020, 77, 559–573. [Google Scholar] [CrossRef] [PubMed]
- Firth, S. CMS Report: ACOs Save Billions for Medicare; MedPage Today: New York, NY, USA, 2019; Available online: https://www.medpagetoday.com/publichealthpolicy/medicare/82544 (accessed on 27 May 2020).
- McWilliams, J.M.; Hatfield, L.A.; Landon, B.E.; Chernew, M.E. Savings or Selection? Initial Spending Reductions in the Medicare Shared Savings Program and Considerations for Reform. Milbank Q. 2020, 98, 847–907. [Google Scholar] [CrossRef]
- Kaufman, B.G.; Spivack, B.S.; Stearns, S.C.; Song, P.H.; O’Brien, E.C. Impact of Accountable Care Organizations on Utilization, Care, and Outcomes: A Systematic Review. Med. Care Res. Rev. MCRR 2019, 76, 255–290. [Google Scholar] [CrossRef]
- Rutledge, R.I.; Romaire, M.A.; Hersey, C.L.; Parish, W.J.; Kissam, S.M.; Lloyd, J.T. Medicaid Accountable Care Organizations in Four States: Implementation and Early Impacts. Milbank Q. 2019, 97, 583–619. [Google Scholar] [CrossRef]
- Bleser, W.K.; Saunders, R.S.; Muhlestein, D.B.; McClellan, M. Why Do Accountable Care Organizations Leave the Medicare Shared Savings Program? Health Aff. 2019, 38, 794–803. [Google Scholar] [CrossRef]
- Shortell, S.M.; Colla, C.H.; Lewis, V.A.; Fisher, E.; Kessell, E.; Ramsay, P. Accountable Care Organizations: The National Landscape. J. Health Polit. Policy Law 2015, 40, 647–668. [Google Scholar] [CrossRef] [PubMed]
- Comfort, L.N.; Shortell, S.M.; Rodriguez, H.P.; Colla, C.H. Medicare Accountable Care Organizations of Diverse Structures Achieve Comparable Quality and Cost Performance. Health Serv. Res. 2018, 53, 2303–2323. [Google Scholar] [CrossRef] [PubMed]
- Ouayogodé, M.H.; Colla, C.H.; Lewis, V.A. Determinants of success in Shared Savings Programs: An analysis of ACO and market characteristics. Healthcare 2017, 5, 53–61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Barnes, A.J.; Unruh, L.; Chukmaitov, A.; van Ginneken, E. Accountable care organizations in the USA: Types, developments and challenges. Health Policy 2014, 118, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ouayogodé, M.H.; Mainor, A.J.; Meara, E.; Bynum, J.P.W.; Colla, C.H. Association Between Care Management and Outcomes Among Patients with Complex Needs in Medicare Accountable Care Organizations. JAMA Netw. Open 2019, 2, e196939. [Google Scholar] [CrossRef]
- McWilliams, J.M.; Chernew, M.E.; Zaslavsky, A.M.; Hamed, P.; Landon, B.E. Delivery System Integration and Health Care Spending and Quality for Medicare Beneficiaries. JAMA Intern. Med. 2013, 173, 1447–1456. [Google Scholar] [CrossRef]
- Peiris, D.; Phipps-Taylor, M.C.; Stachowski, C.A.; Kao, L.-S.; Shortell, S.M.; Lewis, V.A.; Rosenthal, M.B.; Colla, C.H. ACOs Holding Commercial Contracts Are Larger and More Efficient Than Noncommercial ACOs. Health Aff. 2016, 35, 1849–1856. [Google Scholar] [CrossRef][Green Version]
- Maeng, D.D.; Graf, T.R.; Davis, D.E.; Tomcavage, J.; Bloom, F.J. Can a patient-centered medical home lead to better patient outcomes? The quality implications of Geisinger’s ProvenHealth Navigator. Am. J. Med. Qual. Off. J. Am. Coll. Med. Qual. 2012, 27, 210–216. [Google Scholar] [CrossRef]
- Liao, J.M.; Sommers, B.D.; Navathe, A.S. Medicaid’s Path to Value-Based Reform. N. Engl. J. Med. 2018, 379, 105–108. [Google Scholar] [CrossRef]
- Song, Z.; Ji, Y.; Safran, D.G.; Chernew, M.E. Health Care Spending, Utilization, and Quality 8 Years into Global Payment. N. Engl. J. Med. 2019, 381, 252–263. [Google Scholar] [CrossRef]
- Van Vleet, A.; Paradise, J. The State Innovation Models (SIM) Program: An Overview. KFF. 2014. Available online: https://www.kff.org/medicaid/fact-sheet/the-state-innovation-models-sim-program-an-overview/ (accessed on 2 March 2021).
- Centers for Medicaid & Medicare Services. Where Innovation is Happening|CMS Innovation Center—Massachusetts; Centers for Medicaid & Medicare Services: Baltimore, MD, USA, 2021. Available online: https://innovation.cms.gov/innovation-models#views=models&stt=MA (accessed on 2 March 2021).
- Mechanic, R.E.; Altman, S.H.; McDonough, J.E. The new era of payment reform, spending targets, and cost containment in Massachusetts: Early lessons for the nation. Health Aff. 2012, 31, 2334–2342. [Google Scholar] [CrossRef] [PubMed]
- Mass. gov. Massachusetts Delivery System Reform Incentive Payment (DSRIP) Program Protocol; Mass. gov.: Burlington, MA, USA, 2020. [Google Scholar]
- Massachusetts Health Policy Commission ACO Certification Program. Accountable Care Organizations in Massachusetts: Profiles of the 2017 and 2018 HPC-certified ACOs; Massachusetts Health Policy Commission ACO Certification Program: Boston, MA, USA, 2019. Available online: https://www.mass.gov/files/documents/2019/04/26/ACO%20profiles%20packet_0.pdf (accessed on 15 September 2020).
- Merlo, J.; Chaix, B.; Ohlsson, H.; Beckman, A.; Johnell, K.; Hjerpe, P.; Råstam, L.; Larsen, K. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J. Epidemiol. Community Health 2006, 60, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Dieleman, J.L.; Templin, T. Random-Effects, Fixed-Effects and the within-between Specification for Clustered Data in Observational Health Studies: A Simulation Study. PLoS ONE 2014, 9, e110257. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4208783/ (accessed on 17 June 2020). [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services. Driving Health System Transformation—A Strategy for the CMS Innovation Center’s Second Decade; Centers for Medicare & Medicaid Services: Baltimore, MD, USA, 2021; p. 32. Available online: https://innovation.cms.gov/strategic-direction-whitepaper (accessed on 11 January 2022).
- Frieden, J. Medicaid will Be a Bigger Target for Alternative Payment Models, CMS Official Says; MedPage Today: New York, NY, USA, 2021; Available online: https://www.medpagetoday.com/meetingcoverage/phc/95029 (accessed on 11 January 2022).
- Chernew, M.E. Do Commercial ACOs Save Money? Interpreting Diverse Evidence. Med. Care 2019, 57, 843–844. [Google Scholar] [CrossRef]
- The Commonwealth Fund. International Profiles of Health Care Systems; The Commonwealth Fund: New York, NY, USA, 2020; Available online: https://www.commonwealthfund.org/sites/default/files/2020-12/International_Profiles_of_Health_Care_Systems_Dec2020.pdf (accessed on 5 January 2024).
- Alcusky, M.; Ferrari, L.; Rossi, G.; Liu, M.; Hojat, M.; Maio, V. Attitudes Toward Collaboration Among Practitioners in Newly Established Medical Homes: A Survey of Nurses, General Practitioners, and Specialists. Am. J. Med. Qual. 2016, 31, 526–535. [Google Scholar] [CrossRef]
- Keith, S.W.; Waters, D.; Alcusky, M.; Hegarty, S.; Jafari, N.; Lombardi, M.; Pini, M.; Maio, V. The Medical Home Initiative in Italy: An Analysis of Changes in Healthcare Utilization. J. Gen. Intern. Med. 2022, 37, 1380–1387. [Google Scholar] [CrossRef]
- McWilliams, J.M.; Chen, A.J. Understanding the Latest ACO “Savings”: Curb Your Enthusiasm and Sharpen Your Pencils—Part 2. Health Affairs Forefront. 2020. Available online: https://www.healthaffairs.org/do/10.1377/forefront.20201106.1578/full/ (accessed on 11 January 2022).
- McWilliams, J.M.; Chen, A.J. Understanding the Latest ACO “Savings”: Curb Your Enthusiasm and Sharpen Your Pencils—Part 1. Health Affairs Forefront. 2020. Available online: https://www.healthaffairs.org/do/10.1377/forefront.20201106.719550/full/ (accessed on 11 January 2022).
- Bleser, W.K.; Saunders, R.S.; Muhlestein, D.B.; Olson, A.; Richards, R.; Taylor, D.; McClellan, M.B. Following Medicare’s ACO Program Overhaul, Most ACOs Stay—But Physician-Led ACOs Leave at A Higher Rate. Health Affairs Forefront. 2019. Available online: https://www.healthaffairs.org/do/10.1377/hblog20190311.776139/full/ (accessed on 16 September 2020).
- Sullivan, G.; Feore, J. Physician-Led Accountable Care Organizations Outperform Hospital-Led Counterparts; Avalere Health: Washington, DC, USA, 2019; Available online: https://avalere.com/press-releases/physician-led-accountable-care-organizations-outperform-hospital-led-counterparts (accessed on 16 September 2020).
| Respondents (n = 225) | Sample (n = 353) | Sample Frame (n = 672) | |
|---|---|---|---|
| Practice type | |||
| Group practice | 175 (78%) | 278 (79%) | 576 (86%) |
| Health center | 50 (22%) | 74 (21%) | 95 (14%) |
| Practice size | |||
| <100 members | 13 (6%) | 28 (8%) | 69 (10%) |
| 100–999 members | 137 (61%) | 214 (61%) | 415 (61%) |
| 1000–9999 members | 68 (30%) | 101 (29%) | 176 (26%) |
| ≥10,000 members | 6 (3%) | 9 (3%) | 11 (2%) |
| Patient population | |||
| Adult patients only | 71 (33%) | ||
| Pediatric patients only | 41 (19%) | ||
| Both adult and pediatric patients | 106 (49%) | ||
| Experience with ACO contracts | 55% | ||
| ≥50% patients covered by cost accountability contracts | 55% | ||
| Contract experience with same clinical partners | 39% | ||
| ACO anchoring organization | |||
| Physician-organization-anchored | 38 (17%) | 66 (19%) | 66 (10%) |
| Community-hospital-anchored | 49 (22%) | 74 (21%) | 75 (11%) |
| Teaching-hospital-anchored | 138 (61%) | 213 (60%) | 531 (79%) |
| ACO size | |||
| <19,000 members | 62 (28%) | 98 (28%) | 118 (18%) |
| 19,000–28,999 members | 87 (39%) | 144 (41%) | 397 (59%) |
| ≥29,000 members | 76 (34%) | 111 (31%) | 157 (23%) |
| ACOs represented | 17 | 17 | 17 |
| Range of practice sites per ACO | 7–25 | 7–30 | 7–161 |
| Members attributed to practice sites (in thousands) | 345 | 511 | 824 |
| 1. Process change In the past year, to what extent has your practice changed its processes and approaches to caring for MassHealth members? | ||||
| Minimum | Q1 | Median | Q3 | Maximum |
| 2.00 | 2.47 | 2.80 | 3.19 | 3.55 |
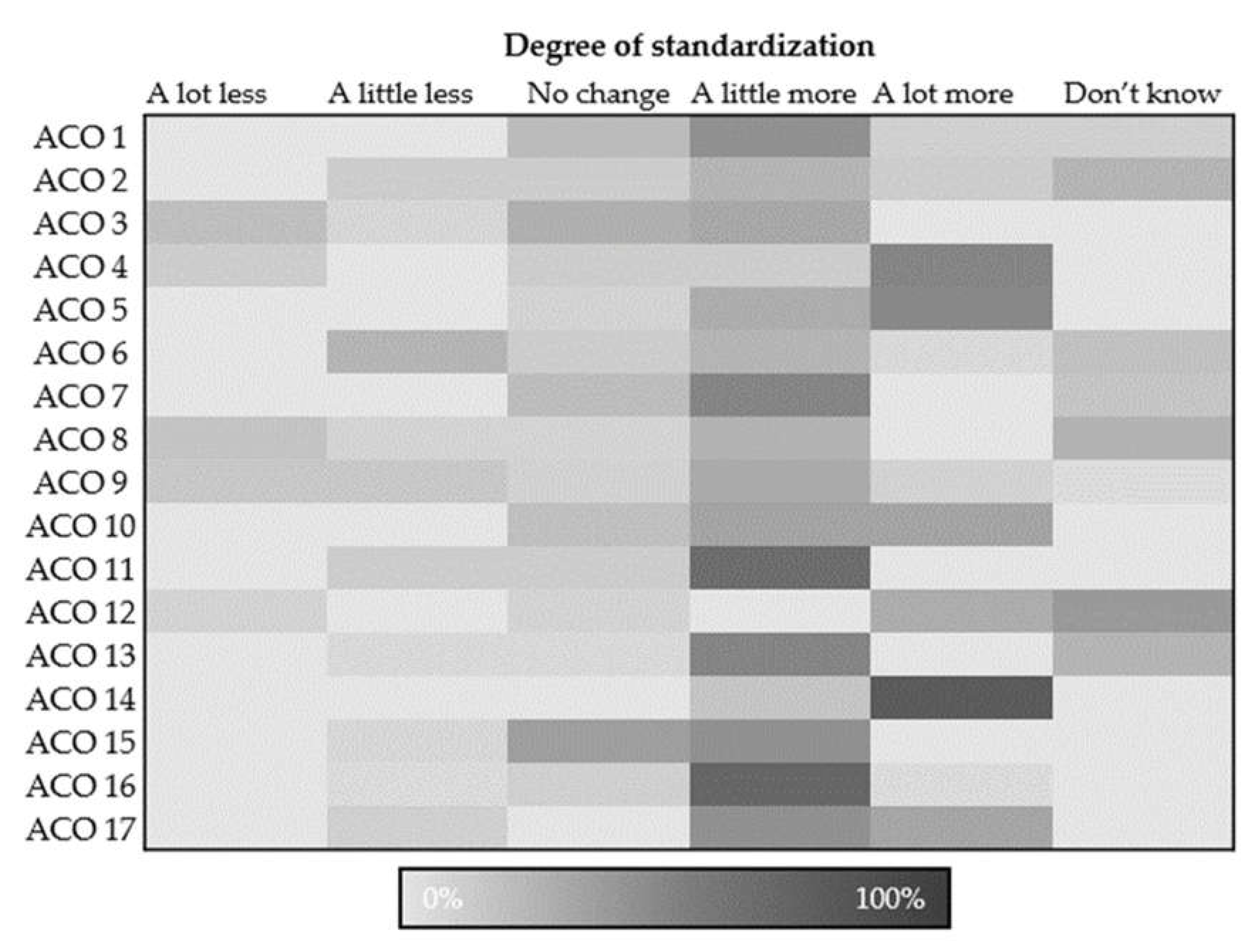
| 2. Standardized practices In the past year, to what degree have care practices and team structure in your clinic become more standardized, less standardized or not changed? | ||||
| Minimum | Q1 | Median | Q3 | Maximum |
| 3.63 | 3.81 | 4.18 | 4.37 | 4.83 |
| 3. Social service referrals How often are MassHealth members referred from your practice to social service organizations to address health-related social needs (e.g., housing, food security)? | ||||
| Minimum | Q1 | Median | Q3 | Maximum |
| 2.80 | 3.14 | 3.58 | 3.91 | 4.60 |
| 4. Ability to care for vulnerable populations In the past year, how has your practice site’s ability to tailor delivery of care to meet the needs of patients affected by health inequities changed? | ||||
| Minimum | Q1 | Median | Q3 | Maximum |
| 2.30 | 3.00 | 3.28 | 3.50 | 4.14 |
| 5. Ability to provide high-quality care In the past year, to what extent has your practice’s ability to deliver high quality care to MassHealth members gotten better, gotten worse, or stayed the same? | ||||
| Minimum | Q1 | Median | Q3 | Maximum |
| 2.63 | 3.15 | 3.32 | 3.44 | 4.00 |
| ACO-Level Variance (SE) | ICC | MOR (95% CrI) | ||
|---|---|---|---|---|
| Contract participation measures | ||||
| Experience with ACO contracts | 1.13 (0.61) | 0.26 | 2.76 (2.42–6.53) | |
| Patients covered by cost accountability contracts | 0.04 (0.15) | 0.01 | 1.22 (1.11–2.96) | |
| Contract experience with the same clinical partners | 0.22 (0.21) | 0.06 | 1.56 (1.41–3.15) | |
| Process measures | ||||
| Process change | 0.63 (0.36) | 0.16 | 2.13 (1.82–4.06) | |
| Standardized practices | 0.48 (0.32) | 0.13 | 1.94 (1.64–3.92) | |
| Social service referrals | 0.71 (0.38) | 0.18 | 2.23 (1.99–4.33) | |
| Ability to care for vulnerable populations | 1.17 (0.55) | 0.26 | 2.80 (2.36–5.21) | |
| Outcome measure | ||||
| Ability to provide high-quality care | 0.37 (0.27) | 0.10 | 1.78 (1.57–3.69) | |
| Unadjusted | Practice Site Level | Practice Site and ACO Levels | |
|---|---|---|---|
| Measures of clustering and variation | |||
| Accountable care organization (ACO)-level variance | 0.37 | 0.40 | 0.04 |
| Intraclass correlation coefficients (ICCs) | 0.10 | 0.11 | 0.01 |
| Median odds ratios (95% credible intervals) | 1.78 (1.57–3.69) | 1.83 (1.56–5.00) | 1.20 (1.00–4.21) |
| Practice-site-level measures, odds ratios | |||
| Group practice vs. health Center | 2.23 (0.84–6.48) | 1.52 (0.51–4.57) | |
| Experience with ACO contracts vs. no experience | 1.56 (0.79–3.08) | 1.96 (0.95–4.03) | |
| Less than half of patients part of risk contracts vs. half or more | 1.16 (0.61–2.20) | 1.20 (0.64–2.26) | |
| No experience with the same clinical partners vs. some experience | 1.24 (0.66–2.32) | 1.24 (0.67–2.29) | |
| Both pediatric and adult patients at the site vs. adults only | 5.11 (2.13–12.3) | 5.24 (2.17–12.7) | |
| Pediatric-only vs. adult-only | 1.68 (0.61–4.65) | 1.67 (0.60–4.64) | |
| Fewer than 500 Medicaid patients vs. more than 500 | 1.77 (0.90–3.47) | 1.67 (0.86–3.24) | |
| ACO-level measures, odds ratios | |||
| Teaching-hospital- vs. physician-organization-anchored | 1.72 (0.71–4.16) | ||
| Community-hospital- vs. physician-organization-anchored | 3.42 (1.07–11.0) | ||
| Medium vs. small organization | 2.32 (0.88–6.11) | ||
| Large vs. small organization | 1.07 (0.30–3.81) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dyer, Z.; Alcusky, M.; Himmelstein, J.; Ash, A.; Kerrissey, M. Practice Site Heterogeneity within and between Medicaid Accountable Care Organizations. Healthcare 2024, 12, 266. https://doi.org/10.3390/healthcare12020266
Dyer Z, Alcusky M, Himmelstein J, Ash A, Kerrissey M. Practice Site Heterogeneity within and between Medicaid Accountable Care Organizations. Healthcare. 2024; 12(2):266. https://doi.org/10.3390/healthcare12020266
Chicago/Turabian StyleDyer, Zachary, Matthew Alcusky, Jay Himmelstein, Arlene Ash, and Michaela Kerrissey. 2024. "Practice Site Heterogeneity within and between Medicaid Accountable Care Organizations" Healthcare 12, no. 2: 266. https://doi.org/10.3390/healthcare12020266
APA StyleDyer, Z., Alcusky, M., Himmelstein, J., Ash, A., & Kerrissey, M. (2024). Practice Site Heterogeneity within and between Medicaid Accountable Care Organizations. Healthcare, 12(2), 266. https://doi.org/10.3390/healthcare12020266


_MD__MPH_PhD.png)



