Abstract
To evaluate associations between depression and/or anxiety disorders during pregnancy (DAP), delivery-related outcomes, and healthcare utilization among individuals with Michigan Medicaid-funded deliveries. We conducted a retrospective delivery-level analysis comparing delivery-related outcomes and healthcare utilization among individuals with and without DAP between January 2012 and September 2021. We used generalized estimating equation models assessing cesarean and preterm delivery; 30-day readmission after delivery; severe maternal morbidity within 42 days of delivery; and ambulatory, inpatient, emergency department or observation (ED), psychotherapy, or substance use disorders (SUD) visits during pregnancy. We adjusted models for age, race/ethnicity, urbanicity, federal poverty level, and obstetric comorbidities. Among 170,002 Michigan Medicaid enrollees with 218,890 deliveries, 29,665 (13.6%) had diagnoses of DAP. Compared to those without DAP, individuals with DAP were more often White, rural dwelling, had lower income, and had more comorbidities. In adjusted models, deliveries with DAP had higher odds of cesarean and preterm delivery OR = 1.02, 95% CI: [1.00, 1.05] and OR = 1.15, 95% CI: [1.11, 1.19] respectively), readmission within 30 days postpartum (OR = 1.14, 95% CI: [1.07, 1.22]), SMM within 42 days (OR = 1.27, 95% CI: [1.18, 1.38]), and utilization compared to those without DAP diagnoses (ambulatory: OR = 7.75, 95% CI: [6.75, 8.88], inpatient: OR = 1.13, 95% CI: [1.11, 1.15], ED: OR = 1.86, 95% CI: [1.80, 1.92], psychotherapy: OR = 172.8, 95% CI: [160.10, 186.58], and SUD: OR = 5.6, 95% CI: [5.37, 5.85]). Among delivering individuals in Michigan Medicaid, DAP had significant associations with adverse delivery-related outcomes and greater healthcare use. Early detection and intervention to address mental illness during pregnancy may help mitigate burdens of these complex yet treatable disorders.
Keywords:
pregnancy; depression; anxiety; maternal health; infant health; maternal health services; medicaid 1. Introduction
Pregnant individuals with mental health conditions deliver more than 800,000 infants each year [1]. Up to or exceeding 20% of individuals have depression and/or anxiety during pregnancy (DAP) [2,3,4,5,6], the most underdiagnosed obstetric complication in the United States (US) [7]. Individuals with lower incomes suffer at a higher rate (40–60%) and experience more severe episodes of DAP [7]. The estimated societal financial toll of not treating DAP exceeds $14 billion annually in the US, with healthcare expenditures and cesarean deliveries driving the overall economic burden [8].
The US experiences the worst maternal morbidity and mortality rates of any peer nation [9]. The global maternal mortality rate decreased 43% since 1990, while the US maternal mortality rate increased 16% from 12 to 14 deaths per 100,000 live births [2]. The US maternal mortality rate remains 75% higher than the average maternal mortality rate for high income nations [3]. High cesarean and preterm delivery rates drive severe maternal morbidity (SMM) and maternal death [4], often along socioeconomic and racial lines [10,11]. Disparities further influence utilization patterns as high-risk individuals seek emergency services to supplement inadequate or inaccessible perinatal health care [5].
Literature indicates that maternal depression and anxiety may increase odds of preterm birth, low birthweight, and other poor birth outcomes [6,7]; however, some systematic reviews maintain that the association is inconclusive [8] or reflects complex causal pathways [7]. A recent study using nationally representative survey data found that individuals with depressive symptoms during pregnancy had higher odds of going without routine medical care and using urgent care more frequently compared to delivering individuals without these symptoms [9]. This study will complement and extend that work by comparing associations between individuals with and without diagnosed DAP and the amounts and types of health care utilization in a high-need population of delivering individuals, namely, those with Medicaid health insurance coverage, which funds nearly half of all births [10,11].
We aimed to determine if delivering individuals with DAP had higher rates of suboptimal delivery-related outcomes and greater utilization of health services compared to delivering individuals without diagnosed DAP.
2. Materials and Methods
We conducted a retrospective cohort study to evaluate health care utilization for Michigan Medicaid enrollees aged 15 to 49 who delivered live births between 1 January 2012 and 30 September 2021 [12]. We used de-identified administrative claims from the Michigan Department of Health and Human Services (MDHHS) data warehouse. During the study period, Medicaid served as the primary payer for 40–44% of births in Michigan [13].
Our inclusion criteria required continuous enrollment in Michigan Medicaid for nine months prior to delivery and three months afterward. Although we recognize that not all pregnancies last exactly nine months, we aimed to increase the likelihood that we could observe all health services utilization during pregnancy. Similarly, Medicaid is available to an eligible woman while she is pregnant, including the month her pregnancy ends and during the two calendar months following the month her pregnancy ends (i.e., 2–3 months). Individuals could appear in our dataset more than once if they had more than one delivery during the study period.
An honest broker extracted and created a de-identified study dataset of Michigan Medicaid enrollment and administrative claims data. The eligible population included all deliveries with at least one live birth. For eligible enrollees, the dataset included all paid claims for nine months prior to and up to three months after the delivery date, including visit dates, hospital admission, and discharge dates; International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM and ICD-10) codes (diagnostic and procedure codes); Diagnosis Related Group (DRG) codes; Current Procedural Terminology, 4th edition, codes (procedure codes); Healthcare Common Procedure Coding System codes (supplies and services codes); Revenue codes, Type of Bill codes, HIC3 Specific Therapeutic Codes; and prescription dispense date. Demographic data at the time of delivery included year of birth, race/ethnicity, Medicaid benefit plan, zip codes, and income level (% Federal Poverty Level [FPL]). We did not exclude individuals with third party liability, which comprised less than 3% of the study sample. Appendix A provides cohort and all variable definitions.
The University of Michigan and Michigan Department of Health and Human Services Institutional Review Boards approved this study. We followed Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines [14].
2.1. Dependent Variables
This study included four delivery-related outcomes and five utilization outcomes during the pregnancy. Delivery-related health outcomes included cesarean delivery, preterm delivery (by diagnosis of gestational age ≤37 weeks), 30-day readmission after delivery, and severe maternal morbidity (SMM) within 42 days as defined by the Centers for Disease Control and Prevention (CDC) [15]. Utilization outcomes included (1) ambulatory care visits (i.e., all outpatient visits including prenatal care); (2) inpatient visits (excluding delivery hospitalization); (3) emergency (ED) and/or observation visits; (4) psychotherapy visits; and (5) substance use disorder (SUD) treatment visits. Utilization variables include visits in the nine months before delivery.
2.2. Independent Variables
For this study, we considered DAP to include any diagnosis of depression or anxiety disorder during pregnancy as the primary independent variable. We included maternal sociodemographic characteristics available in the Medicaid data for time of delivery with plausible associations with outcomes of interest, including age (range 15–49); race/ethnicity (American Indian/Alaskan Native, Asian, Black, Hispanic, Native Hawaiian/Pacific Islander, White, other/unspecified); urbanicity (urban, non-urban/unknown based on zip codes of residence) [16]; and percentage of FPL (0, >0 to ≤50, >50, unknown).
We also included clinical characteristics commonly associated with outcomes of interest using any diagnosis code (not just primary diagnosis), including Bateman Obstetric Comorbidity Index (OBCMI; categorized as 0–1, 2+) [17]; behavioral health diagnoses other than depression and anxiety (serious mental illness, SUD, other behavioral health diagnoses, any of the four preceding diagnosis groups); and psychotropic medication use (antidepressants, anxiolytics, antipsychotics, mood stabilizers, opioid analgesics, medication for opioid use disorder, stimulants, any of the seven psychotropic medication classes).
2.3. Statistical Methods
First, we compared sociodemographic and clinical characteristics among deliveries to childbearing individuals with and without DAP at any time during the study period. Next, we used unadjusted and adjusted odds ratios from generalized estimating equation (GEE) regression in GENMOD models to assess delivery-related and utilization outcomes with delivery as the unit of analysis. We treated deliveries as a repeated measure to account for mothers who had more than one delivery during the study period. We used a compound symmetry assumption (type = cs) for the covariance matrix. We conducted all analyses using SAS 9.4 and used the PROC GENMOD module.
3. Results
The sample included 218,890 deliveries among 170,002 Michigan Medicaid enrollees meeting study criteria during the study period. This included 129,903 (76.4%) with one delivery, 32,629 (19.2%) with two deliveries, 6329 (3.7%) with three deliveries, and 1141 (0.7%) with four or more deliveries. Of those delivering individuals, 15.7% of deliveries had diagnosed DAP during pregnancy. Figure 1 presents the study cohort selection and attrition.
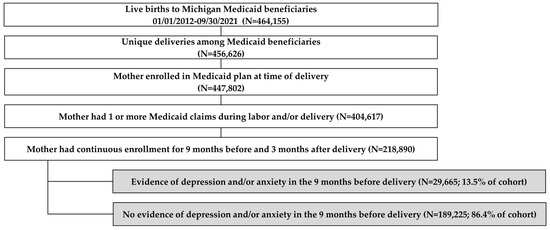
Figure 1.
Cohort selection and attrition (unit of analysis: delivery).
Table 1 compares sociodemographic characteristics and clinical characteristics of childbearing individuals with and without DAP (all p < 0.001). Deliveries with DAP had a higher proportion of White (69.6% versus 50.57%) enrollees than deliveries without DAP, as is consistent with other literature [18]. Deliveries with DAP also had a higher proportion of non-urban (20.3% versus 13.5%) and lower income (60.6% versus 55.8% with income at 0% FPL) enrollees than deliveries without DAP. Individuals with DAP had more obstetric comorbidities than those without DAP (2.07 vs. 1.27). Findings indicated substantially higher rates of other behavioral health diagnoses and psychotropic medication use among those with diagnosed DAP versus those without. Among deliveries with DAP, 49.6% had another behavioral health diagnosis, and 71.7% had any psychotropic medication use. Among those without diagnosed DAP, 8.8% had another behavioral health diagnosis, and 12.5% had any psychotropic medication use during pregnancy and/or postpartum.

Table 1.
Demographic and clinical characteristics of deliveries with and without DAP diagnoses in Michigan Medicaid, 2012–2021.
Table 2 presents findings on delivery-related outcomes and utilization of health services from adjusted and unadjusted GEE regression models displaying odds ratios. In adjusted analyses, deliveries with DAP during pregnancy versus without DAP had 2% greater odds of cesarean delivery (OR = 1.02, [95% CI: 1.00, 1.05]) and 15% greater odds of preterm delivery (OR = 1.15, [95% CI: 1.11, 1.19]). Women with DAP had 14% greater odds of being readmitted to the hospital within 30 days of delivery (OR = 1.14, [95% CI: 1.07, 1.22]) and 27% greater odds of experiencing SMM within 42 days of delivery (OR = 1.27, [95% CI: 1.18, 1.38]).

Table 2.
Unadjusted and adjusted odds ratios of delivery-related outcomes and utilization of health services among deliveries with and without DAP in Michigan Medicaid, 2012–2021.
Compared with delivering individuals without diagnosed DAP, those with pregnancy-related diagnosed DAP had a higher probability of all five types of utilization assessed during pregnancy, including an almost eight-fold increase in odds of attending an ambulatory visit (OR = 7.75, [95% CI: 6.75, 8.88]), a 13% increase in odds of attending inpatient visits (OR = 1.13, [95% CI: 1.11, 1.15]), and an 86% increase in odds of being admitted for ED/observation (OR = 1.86, [95% CI: 1.80, 1.92]). Unsurprisingly, DAP was associated with 172.8 times greater odds of attending psychotherapy visits (OR = 172.83, [95% CI: 160.10, 186.58]) and 5.61 times greater odds of attending an SUD visit (OR = 5.61, [95% CI: 5.37, 5.85]).
4. Discussion
This study demonstrates the magnitude of the excess healthcare use associated with DAP among delivering individuals with Medicaid. Delivering individuals with diagnosed DAP had higher rates of comorbid mental health and substance use diagnoses, higher use of psychotropic medication, higher rates of adverse delivery-related outcomes, and higher utilization than their counterparts without diagnosed DAP. Although higher rates of adverse delivery-related outcomes may be driven by associations with other characteristics besides DAP status, healthcare utilization rates remained higher for those with DAP in adjusted models, even for non-behavioral health-related services.
Although this study indicated that those with DAP had higher healthcare utilization, some of that excess utilization may represent appropriate and beneficial care, whereas other utilization may have included inappropriate or low value treatment. Individuals with DAP may need more services; however, we cannot determine from this analysis whether the care received represented the right amount and mix or type of services. Ideally, individuals with DAP would receive necessary and high value care as appropriate to their conditions; their utilization patterns would not necessarily match those for individuals without DAP.
These findings are consistent with existing literature, which consistently identifies an association between depression and/or anxiety and preterm birth [6,7,8]. However, the literature on cesarean delivery is decidedly more mixed. One systematic review found an overall null association between antenatal anxiety and cesarean delivery [6]. These null results may reflect heterogeneity within patients with DAP, as untreated DAP increased risk of cesarean delivery, while treated DAP decreased risk of cesarean delivery. Our study did not control for treatment status, but Medicaid recipients are less likely to receive postpartum mental health treatment than privately insured individuals [19], which may also occur in the antenatal population. We did not identify literature associating DAP with SMM or 30-day rehospitalization. The prevalence of both SMM and DAP has increased over the past decade [20,21], and our findings may indicate that these increases are linked.
These findings correspond with other literature on the higher healthcare utilization among those with behavioral health conditions compared to those without these conditions in delivering and non-delivering populations [9,22,23,24,25]. A five-year retrospective cohort study of Medicaid-insured individuals in South Carolina found that eligible individuals who received group visits had a reduced risk of premature birth, low birthweight, and neonatal intensive care unit stays [26]. Another study suggests establishing routine care and decreasing acute care in this population [9]. Future interventions, including repeated screening throughout pregnancy and postpartum, could also assist in the early detection and management of DAP.
This study documents high rates of comorbidity within and across behavioral health conditions, including SUD, and higher use of SUD treatment among those with DAP. Given the overlap of these conditions in this and in other studies [27,28], this finding also reiterates the importance of both early detection and appropriately tailored treatment that addresses needs of those with multiple behavioral health comorbidities.
Limitations
Diagnoses represent detected illness, yet DAP frequently goes undiagnosed, especially in non-White individuals; furthermore, race/ethnicity groups may approach treatment for DAP differently [29,30]. Systemic racism can also yield barriers for non-White individuals to accessing perinatal physical and mental health care [31,32]. This creates heterogeneity in under-diagnosis, which may skew our results. Residual bias may have also occurred such that we could not account for all possible confounding influences on the relationship between DAP and outcomes. Imperfect timing of diagnoses in claims data during healthcare visits relative to onset of illness may also have influenced study findings. Claims data can only indicate current diagnoses and may not accurately reflect symptom onset, severity of symptoms, or remission.
This study used a retrospective, observational design, which cannot establish causality. This study included individuals with continuous enrollment, yet Medicaid churn for postpartum individuals remains pervasive [33,34]. More than half of the individuals originally identified in our study population did not meet criteria for continuous enrollment. Therefore, the true extent of the impact of their DAP on healthcare utilization remains unknown and hard to accurately quantify. Individuals enrolled in Medicaid may have higher and more severe rates of DAP; findings may not necessarily generalize to non-Medicaid populations; however, individuals without continuous coverage may have higher rates of DAP than those with continuous coverage. Further, findings may not generalize to Medicaid populations in other states, as each state may handle access to care and coverage differently. For all these reasons, we anticipate that these findings represent an underestimate of the impact of DAP. We focused this study on DAP; individuals experiencing mental health conditions during pregnancy have an increased risk of maintaining or developing those conditions postpartum compared to people without DAP.
5. Conclusions
Accounting for sociodemographic and clinical characteristics, we found that childbearing individuals with DAP with Medicaid insurance coverage in Michigan had higher rates of adverse birth outcomes and healthcare utilization compared to those without DAP. Given the well-established negative intergenerational effects of inadequate care for childbearing individuals on outcomes for their infants, early detection and tailored, appropriate treatment of DAP may help mitigate the health burdens associated with these complex yet treatable disorders.
Author Contributions
Conceptualization, K.Z., X.Z., A.T., S.J.C. and S.V.H.; methodology, K.Z., X.Z. and A.T.; validation, X.Z. and A.T.; formal analysis, X.Z. and A.T.; data curation, X.Z. and A.T.; writing—original draft preparation, K.Z. and X.Z.; writing—review and editing, K.Z., S.J.C. and S.V.H.; funding acquisition, K.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This project received funding support from the Center of Medicare and Medicaid Services through the Michigan Department of Health and Human Services (MDHHS).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the University of Michigan Institutional Review Board (IRB) under HUM00148854 and by the MDHHS IRB Log #: 201811-10-EA-(R1).
Informed Consent Statement
Patient consent was waived by both the University of Michigan IRB and MDHHS IRB as permitted under 45 CR 46.116(d).
Data Availability Statement
The data that support the findings of this study are available from the MDHHS Data Warehouse. Restrictions apply to the availability of these data, which were used under license for this study and thus are not publicly available. Data from the MDHHS Data Warehouse for this study was made available through a Data Use Agreement with MDHHS by program sponsors Michigan Pregnancy Risk Assessment Monitoring System, Medical Services Administration, Behavioral Health and Developmental Disabilities Administration, and Vital Records.
Acknowledgments
We would like to acknowledge Rebecca Brownlee, Acham Gebremariam, Amy Schroeder, and Erin Miller in the technical support of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript’ or in the decision to publish the results.
Appendix A. Cohort and Variable Definitions
Delivery Codes
| Variable | ICD Diagnosis Code | ICD Procedure Code | DRG | CPT/HCPCS |
| Cesarean | - | 740, 741, 742, 744, 7499; 10D00Z0, 10D00Z1, 10D00Z2 | 370, 371, 765, 766, 540, 5401, 5402, 5403, 5404 | 59510, 59514, 59515, 59618, 59620, 59622 |
| Vaginal | 10D07Z3, 10D07Z4, 10D07Z5, 10D07Z6, 10D07Z7, 10D07Z8, 10E0XZZ | 372, 373, 374, 375, 767 768, 774, 775, 541, 542, 560, 5411, 5412, 5413, 5414, 5421, 5422, 5423, 5424, 5601, 5602, 5603 | 59400, 59409, 59410, 59610, 59612, 59614 | |
| Preterm Birth | O601, O6010, O6010X0, O6010X1, O6010X2, O6010X3, O6010X4, O6010X5, O6010X9, O6012, O6012X0, O6012X1, O6012X2, O6012X3, O6012X4, O6012X5, O6012X9, O6013, O6013X0, O6013X1, O6013X2, O6013X3, O6013X4, O6013X5, O6013X9, O6014, O6014X0, O6014X1, O6014X2, O6014X3, O6014X4, O6014X5, O6014X9 |
Mental Health Disorder Codes
| Variable | ICD Diagnosis Code | |
| Depression and/or Anxiety (DAP) | Anxiety | 300.xx, 308.xx, 313.xx, 293.xx, F06.xx, F40.xx, F41.xx, F42.xx, F43.xx, F48.xx, R45.xx |
| Depression | 311.xx, 296.xx, 300.xx, F32.xx, F33.xx | |
| Other Behavioral Health Conditions | Mental Health Disorders, excluding DAP | 312.xx, 314.xx, 313.xx, F90.xx, F91.xx, R46.xx, R46.xx, R46.xx, R46.xx, 309.xx, 309.xx, F43.xx |
Psychotropic Medication Classification Codes
| Medication class | HIC 3 Specific Therapeutic Code |
| Antidepressant | H24, H2H, H2J, H2K, H2N, H2S, H2U, H2Y, H7B, H7C, H7D, H7E, H7I, H7J, H7K, H7L, H8P, H8S, H8T, H8Z |
| Antidepressant/antipsychotic | H2W, H7A |
| Antidepressant/anxiolytic | H2X, H7M |
| Antipsychotic | H2G, H2I, H2L, H2O, H7O, H7P, H7Q, H7R, H7S, H7T, H7U, H7V, H7X, H7Z, H8N, H8W |
| Anxiolytic | H20, H2F, H2P, H8A, H8K |
| Mood stabilizer | H2M |
| Opioid/narcotic analgesic | H30, H3A, H3B, H3H, H3J, H3M, H3N, H3Q, H3R, H3U, H3X, H3Z, S7G |
| Opioid/narcotic antagonist | H3T, H3W, H3Y, H33 |
| Opioid/narcotic antitussive | B4F, B4N, B6C, B6I, B6U |
| Stimulant | H2V, H7Y, H8M, H8Q, J5B |
Visit Codes
| Visit Type | ICD Diagnosis Code | ICD Procedure Code | CPT/HCPCS | Revenue | Bill Type |
| Ambulatory Care | Z00.00, Z00.01, Z00.121, Z00.129, Z00.3, Z00.5, Z00.8, Z02.0, Z02.1, Z02.2, Z02.3, Z02.4, Z02.5, Z02.6, Z02.71, Z02.79, Z02.81, Z02.82, Z02.83, Z02.89, Z02.9, Z76.1, Z76.2, V20.2, V70.0, V70.3, V70.5, V70.6, V70.8, V70.9 | 92002, 92004, 92012, 92014, 99201, 99202, 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215, 99241, 99242, 99243, 99244, 99245, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99315, 99316, 99318, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, 99381, 99382, 99383, 99384, 99385, 99386, 99387, 99391, 99392, 99393, 99394, 99395, 99396, 99397, 99401, 99402, 99403, 99404, 99411, 99412, 99429, 99461, 99483, G0463, T1015, G0402, G0438, G0439, S0620, S0621, 98966, 98967, 98968, 99441, 99442, 99443 | 510, 511, 512, 513, 514, 515, 516, 517, 519, 520, 521, 522, 523, 524, 525, 526, 527, 528, 529, 982, 983 | ||
| Inpatient | 100, 1000, 1001, 1002, 1003, 1004, 1005, 101, 110, 111, 112, 113, 114, 116, 117, 118, 119, 120, 121, 122, 123, 124, 126, 127, 128, 129, 130, 131, 132, 133, 134, 136, 137, 138, 139, 140, 141, 142, 143, 144, 146, 147, 148, 149, 150, 151, 152, 153, 154, 156, 157, 158, 159, 160, 164, 167, 169, 170, 171, 172, 173, 174, 179, 190, 191, 192, 193, 194, 199, 200, 201, 202, 203, 204, 206, 207, 208, 209, 210, 211, 212, 213, 214, 219, 22, 24, 524, 525, 550, 551, 552, 559, 660, 661, 662, 663, 669, 720, 721, 722, 723, 724, 729, 987 | 180, 181, 182, 183, 184, 185, 187, 188, 210, 211, 212, 213, 214, 215, 217, 218, 220, 221, 222, 223, 224, 225, 227, 228, 280, 281, 282, 283, 284, 285, 287, 288, 289, 650, 652, 653, 654, 655, 657, 658, 660, 662, 663, 664, 665, 667, 668, 860, 862, 863, 864, 865, 867, 868, 018F, 018G,018H, 018I, 018J, 018K, 018M, 018O, 018X, 018Y, 018Z, 021F, 021G, 021H, 021I, 021J, 021K, 021M, 021O, 021X, 021Y, 021Z, 022F, 022G, 022H, 022I, 022J, 022K, 022M, 022O, 022X, 022Y, 022Z, 028F, 028G, 028H, 028I, 028J, 028K, 028M, 028O, 028X, 028Y, 028Z, 065F, 065G, 065H, 065I, 065J, 065K, 065M, 065O, 065X, 065Y, 065Z, 066F, 066G, 066H, 066I, 066J, 066K, 066M, 066O, 066X, 066Y, 066Z, 086F, 086G, 086H, 086I, 086J, 086K, 086M, 086O, 086X, 086Y, 086Z | |||
| Emergency Department and/or observation | 99281, 99282, 99283, 99284, 99285, G0380, G0381, G0382, G0383, G0384 EDsurgprocPOS23 if place of service = 23 AND CPT between 10050–69979 ObsProc if CPT codes: 99217, 99218, 99219, 99220, G0378, G0379 ObsRev if revenue code 0762 | 045, 0981 | |||
| Psychotherapy | 90804, 90805, 90806, 90807, 90808, 90809, 90810, 90811, 90812, 90813, 90814, 90815, 90816, 90817, 90818, 90819, 90820, 90821, 90822, 90823, 90824, 90826, 90827, 90828, 90829, 90832, 90833, 90834, 90836, 90837, 90838, 90839, 90840, 90841, 90842, 90843, 90844, 90846, 90847, 90849, 90853, 90855 | ||||
| Substance Use Disorder Related | 291.xx, 357.xx, 425.xx, 535.xx, 571.xx, 980.xx, 303.xx, 305.xx, 760.xx, F10.xx, G62.xx, I42.xx, K29.xx, K70.xx, O99.xx, 304.xx, F12.xx, F14.xx, 292.xx, 779.xx, 648.xx, 655.xx, 965.xx, F55.xx, O35.xx, F16.xx, F18.xxP04.xx, P96.xx, Q86.xx, F11.xx, F15.xx, F19.xx, F13.xx, T36.xx, T37.xx, T38.xx, T39.xx, T40.xx, T41.xx, T42.xx, T43.xx, T44.xx, T45.xx, T46.xx, T47.xx, T48.xx, T49.xx, T50.xx, T51.xx, T52.xx, T53.xx, T54xx, T55.xx, T56.xx, T57.xx, T58.xx, T59.xx, T60.xx, T61.xx, T62.xx, T63.xx, T64.xx, T65.xx, T71.xx, V65.xx, F17.xx | 9462, 9461, 9463, 946, 9446, 9469, 9468, 9467, 9465, 9464, 9466 | G0397, G0396, H0048, H2034, H0014, H0027, H0029, H0007, H0016, H0026, H0028, H0003, H0009, H0005, H0015, H001, H0012, H0011, H0013, H0020, H0008, T1006, H0050, H0022, H0006, H0021, H0047, H2036, H2035, H0001, H0049, T102, T1007, T1011, S9475, G0442, H0039, H0040, H0004, H2012, H0030, H0023, H0025, H0017, H0024, H0002, H0019, H018, G0443, T1009, H2015, H2016, H2011, T1008, T1010, H2025, H2026, H0033, H2001, H0038, H2014, H2019, H2020, H2ZZZZ, HZ63ZZZ, HZ33ZZZ, GZ3ZZZZ, HZ82ZZZ, HZ83ZZZ, HZ87ZZZ, HZ86ZZZ, HZ81ZZZ, HZ85ZZZ, HZ84ZZZ, HZ80ZZZ, HZ89ZZZ, HZ88ZZZ, HZ93ZZZ, HZ97ZZZ, HZ96ZZZ, HZ92ZZZ, HZ95ZZZ, HZ94ZZZ, HZ98ZZZ, HZ91ZZZ, HZ90ZZZ, HZ99ZZ |
Severe Maternal Morbidity Codes
| Variable | ICD Diagnosis Code | ICD Procedure Code |
| Acute Myocardial Infarction | 410.xx, I21.01, I21.02, I21.09, I21.11, I21.19, I21.21, I21.29, I21.3, I21.4, I21.9, I21.A1 and I21.A9, I22.0, I22.1, I22.2, I22.8, I22.9 | |
| Aneurysm | 441.xx, I71.00–I71.03, I71.1, I71.2, I71.3, I71.4, I71.5, I71.6, I71.8, I71.9, I79.0 | |
| Acute Renal Failure | 584.5, 584.6, 584.7, 584.8, 584.9, 669.3x, N17.0, N17.1, N17.2, N17.8, N17.9, O90.4 | |
| Adult Respiratory Distress Syndrome | 518.5x, 518.81 518.82 518.84, 799.1, J80, J95.1, J95.2, J95.3, J95.821, J95.822, J96.00, J96.01, J96.02, J96.20, J96.21, J96.22, R09.2 | |
| Amniotic Fluid Embolism | 673.1x, O88.11x *, O88.12, O88.13 * x = 1st, 2nd, and 3rd trimester | |
| Cardiac Arrest/Ventricular Fibrillation | 427.41, 427.42, 427.5, I46.2, I46.8, I46.9, I49.01, I49.02 | |
| Conversion of Cardiac Rhythm | 99.6x, 5A2204Z, 5A12012 | |
| Disseminated Intravascular Coagulation | 286.6, 286.9, 666.3x, D65, D68.8, D68.9, O72.3 | |
| Eclampsia | 642.6x, O15.00, O15.02, O15.03, O15.1, O15.2, O15.9, O14.22, O14 | |
| Heart Failure/Arrest during Surgery or Procedure | 997.1, I97.120, I97.121, I97.130, I97.131, I97.710, I97.711 | |
| Puerperal Cerebrovascular Disorders | 430.xx, 431.xx, 432.xx, 433.xx, 434.xx, 436xx, 437.xx, 671.5x, 674.0x, 997.02, I60.0x, I60.1x, I60.2, I60.3x, I60.4, I60.5x, I60.6, I60.7, I60.8, I60.9; I61.1, I61.2, I61.3, I61.4, I61.5, I61.6, I61.8, I61.9; I62.0x, I62.1, I62.9; I63.0xx, I63.1xx, I63.2xx, I63.3xx, I63.4xx, I63.5xx, I63.6, I63.8, I63.9; I65.0x, I65.1, I65.2x, I65.8, I65.9; I66.0x, I66.1x, I66.2x, I66.3, I66.8, I66.9; I67.0, I67.1, I67.2, I67.3, I67.4, I67.5, I67.6, I67.7, I67.8xx, I67.9; I68.0, I68.2, I68.8; O22.51, O22.52, O22.53, I97.810, I97.811, I97.820, I97.821, O87.3, 674.0x | |
| Pulmonary edema/Acute Heart Failure | 518.4, 428.1, 428.0, 428.21, 428.23, 428.31, 428.33, 428.41, 428.43, J81.0, I50.1, I50.20, I50.21, I50.23, I50.30, I50.31, I50.33, I50.40, I50.41, I50.43, I50.9 | |
| Severe Anesthesia Complications | 668.0x, 668.1x, 668.2x, O74.0, O74.1, O74.2, O74.3, O89.01, O89.09, O89.1, O89.2 | |
| Sepsis | 038.xx, 995.91, 995.92, 670.2x (after October 1, 2009); O85, O86.04, T80.211A, T81.4XXA, T81.44, T81.44XA, T81.44XD, T81.44XS, R65.20 or A40.0, A40.1, A40.3, A40.8, A40.9, A41.01, A41.02, A41.1, A41.2, A41.3, A41.4, A41.50, A41.51, A41.52, A41.53, A41.59, A41.81, A41.89, A41.9, A32.7 | |
| Shock | 669.1x, 785.5x, 995.0, 995.4, 998.0x, O75.1, R57.0, R57.1, R57.8, R57.9, R65.21, T78.2XXA, T88.2XXA, T88.6XXA, T81.10XA, T81.11XA, T81.19XA | |
| Sickle Cell Disease with Crisis | 282.42, 282.62, 282.64, 282.69, D57.00, D57.01, D57.02, D57.211, D57.212, D57.219, D57.411, D57.412, D57.419, D57.811, D57.812, D57.819 (5th digit: unspecified, acute chest syndrome or splenic sequestration) | |
| Air and Thrombotic Embolism | 415.1x, 673.0x, 673.2x 673.3x, 673.8x, I26.01, I26.02, I26.09, I26.90, I26.92, I26.99, O88.011-O88.019, 088.02, O88.03, O88.211-O88.219, O88.22, O88.23, O88.311-O88.319, O88.32, O88.33, O88.81, O88.82, O88.83 | |
| Blood Products Transfusion | 99.0x, 30233H1, 30233L1, 30233K1, 30233M1, 30233N1, 30233P1, 30233R1, 30233T1, 30233H0, 30233L0, 30233K0, 30233M0, 0233N0, 30233P0, 30233R0, 30233T0, 30230H1, 30230L1, 30230K1, 30230M1, 30230N1, 30230P1, 30230R1, 30230T1, 30230H0, 30230L0, 30230K0, 30230M0, 30230N0, 30230P0, 30230R0, 30230T0, 30240H1, 30240L1, 30240K1, 30240M1, 30240N1, 30240P1, 30240R1, 30240T1, 30240H0, 30240L0, 30240K0, 30240M0, 30240N0, 30240P0, 30240R0, 30240T0, 30243H1, 30243L1, 30243K1, 30243M1, 30243N1, 30243P1, 30243R1, 30243T1, 30243H0, 30243L0, 30243K0, 30243M0, 30243N0, 30243P0, 30243R0, 30243T0, 30250H1, 30250L1, 30250K1, 30250M1, 30250N1, 30250P1, 30250R1, 30250T1, 30250H0, 30250L0, 30250K0, 30250M0, 30250N0, 30250P0, 30250R0, 30250T0, 30253H1, 30253L1, 30253K1, 30253M1, 30253N1, 30253P1, 30253R1, 30253T1, 30253H0, 30253L0, 30253K0, 30253M0, 30253N0, 30253P0, 30253R0, 30253T0, 30260H1, 30260L1, 30260K1, 30260M1, 30260N1, 30260P1, 30260R1, 30260T1, 30260H0, 30260L0, 30260K0, 30260M0, 30260N0, 30260P0, 30260R0, 30260T0, 30263H1, 30263L1, 30263K1, 30263M1, 30263N1, 30263P1, 30263R1, 30263T1, 30263H0, 30263L0, 30263K0, 30263M0, 30263N0, 30263P0, 30263R0, 30263T0 | |
| Hysterectomy | 68.3x-68.9x, 0UT90ZZ, 0UT94ZZ, 0UT97ZZ, 0UT98ZZ, 0UT9FZZ | |
| Temporary Tracheostomy | 31.1, 0B110Z4, 0B110F4, 0B113Z4, 0B113F4, 0B114Z4, 0B114F4 | |
| Ventilation | 93.90, 96.01, 96.02, 96.03, 96.05, 5A1935Z, 5A1945Z, 5A1955Z |
Bateman Obstetric Comorbidity Index
| Variable | ICD Diagnosis Code |
| Bateman Obstetric Comorbidity Index | 291, 303, 3050, 493, 394, 395, 396, 397, 424, 42822, 42823, 42832, 42833, 42842, 42843, 412, 413, 414, 581, 582, 583, 585, 587, 588, 6462, 7450, 7451, 7452, 7453, 7454, 7455, 7456, 7457, 7458, 7459, 7460, 7461, 7462, 7463, 7464, 7465, 7466, 7467, 7468, 7469, 7470, 7471, 7472, 7473, 7474, 6485, 304, 3052, 3053, 3054, 3055, 3056, 3057, 3058, 3059, 6483, 6423, 042, V08, 6424, 6427, 651, V272, V273, V274, V275, V276, V277, V278, 6410, 6411, 250, 6480, 401, 402, 403, 404, 405, 6420, 6421, 6422, 6427, 6542, 4160, 4168, 4169, 6425, 6466, 2824, 2826, 7100, F10, J44, J45, I05, I06, I07, I08, I09, I34, I35, I36, I37, I38, I39, I500, I20, I25, N022, N03, N04, N05, N08, N171, N172, N18, N25, O268, Q20, Q21, Q22, Q23, Q24, Q25, Q26, O994, F11, F12, F13, F14, F15, F16, F18, F19, O13, O16, B20, B24, O987, Z21, O11, O14, O30, O31, Z372, Z373, Z374, Z375, Z376, Z377, Z3790, O44, E10, E11, O245, O246, O247, I10, I11, I12, I13, I15, O10, O11, O3420, I270, I272, I278, I279, O14, O15, D56, D57, M32 |
References
- Maternal Mental Health Leadership Alliance. Fact Sheet: Maternal Mental Health; Maternal Mental Health Leadership Alliance: Arlington, VA, USA, 2020. [Google Scholar]
- Wilson Center. What Explains the United States’ Dismal Maternal Mortality Rates? Wilson Center: Washington, DC, USA, 2015. [Google Scholar]
- World Bank. Maternal Mortality Ratio (Modeled Estimate per 100,000 Live Births)—High Income; World Bank: Washington, DC, USA, 2023. [Google Scholar]
- Centers for Disease Control and Prevention. How Does CDC Identify Severe Maternal Morbidity; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2023. [Google Scholar]
- Malik, S.; Kothari, C.; MacCallum, C.; Liepman, M.; Tareen, S.; Rhodes, K.V. Emergency Department Use in the Perinatal Period: An Opportunity for Early Intervention. Ann. Emerg. Med. 2017, 70, 835–839. [Google Scholar] [CrossRef] [PubMed]
- Grigoriadis, S.; Graves, L.; Peer, M.; Mamisashvili, L.; Tomlinson, G.; Vigod, S.N.; Dennis, C.L.; Steiner, M.; Brown, C.; Cheung, A.; et al. Maternal Anxiety During Pregnancy and the Association with Adverse Perinatal Outcomes: Systematic Review and Meta-Analysis. J. Clin. Psychiatry 2018, 79, e1–e22. [Google Scholar] [CrossRef] [PubMed]
- Staneva, A.; Bogossian, F.; Pritchard, M.; Wittkowski, A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 2015, 28, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Accortt, E.E.; Cheadle, A.C.D.; Dunkel Schetter, C. Prenatal Depression and Adverse Birth Outcomes: An Updated Systematic Review. Matern. Child Health J. 2015, 19, 1306–1337. [Google Scholar] [CrossRef] [PubMed]
- Masters, G.A.; Li, N.; Lapane, K.L.; Liu, S.-H.; Person, S.D.; Byatt, N. Utilization of Health Care among Perinatal Women in the United States: The Role of Depression. J. Women’s Health 2020, 29, 944–951. [Google Scholar] [CrossRef]
- Meltzer, R.; Markus, A.R. An Analysis of Payment Mix Patterns of Preterm Births in a Post-Affordable Care Act Insurance Market: Implications for the Medicaid Program. Women’s Health Issues 2020, 30, 248–259. [Google Scholar] [CrossRef]
- Medicaid and CHIP Payment and Access Commission. Fact Sheet: Medicaid’s Role in Financing Maternity Care; MACPAC: Washington, DC, USA, 2020. [Google Scholar]
- Kuklina, E.V.; Whiteman, M.K.; Hillis, S.D.; Jamieson, D.J.; Meikle, S.F.; Posner, S.F.; Marchbanks, P.A. An enhanced method for identifying obstetric deliveries: Implications for estimating maternal morbidity. Matern. Child Health J. 2008, 12, 469–477. [Google Scholar] [CrossRef]
- Annie, E. Casey Foundation. Medicaid Paid Births—Single Year in Michigan. 2019. Available online: https://datacenter.kidscount.org/data/tables/1716-medicaid-paid-births--single-year#detailed/2/any/false/37,871,870,573,869,36,868,867,133,38/any/3639,13078 (accessed on 1 January 2023).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.F.; Vandenbroucke, J.P.; Initiative, S. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Severe Maternal Morbidity Indicators and Corresponding ICD Codes during Delivery Hospitalizations; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018. [Google Scholar]
- United States Department of Agriculture Economic Research Service. 2010 Rural-Urban Commuting Area (RUCA) Codes; United States Department of Agriculture Economic Research Service: Washington, DC, USA, 2020.
- Bateman, B.T.; Mhyre, J.M.; Hernandez-Diaz, S.; Huybrechts, K.F.; Fischer, M.A.; Creanga, A.A.; Callaghan, W.M.; Gagne, J.J. Development of a comorbidity index for use in obstetric patients. Obstet. Gynecol. 2013, 122, 957–965. [Google Scholar] [CrossRef]
- Pollack, L.M.; Chen, J.; Cox, S.; Luo, F.; Robbins, C.L.; Tevendale, H.D.; Li, R.; Ko, J.Y. Healthcare Utilization and Costs Associated with Perinatal Depression Among Medicaid Enrollees. Am. J. Prev. Med. 2022, 62, e333–e341. [Google Scholar] [CrossRef]
- Sherman, L.J.; Ali, M.M. Diagnosis of Postpartum Depression and Timing and Types of Treatment Received Differ for Women with Private and Medicaid Coverage. Women’s Health Issues 2018, 28, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Tabb, K.M.; Dalton, V.K.; Tilea, A.; Kolenic, G.E.; Admon, L.K.; Hall, S.V.; Zhang, X.; Ryckman, K.K.; Zivin, K. Trends in antenatal depression and suicidal ideation diagnoses among commercially insured childbearing individuals in the United States, 2008–2018. J. Affect. Disord. 2023, 320, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Fink, D.A.; Kilday, D.; Cao, Z.; Larson, K.; Smith, A.; Lipkin, C.; Perigard, R.; Marshall, R.; Deirmenjian, T.; Finke, A.; et al. Trends in Maternal Mortality and Severe Maternal Morbidity During Delivery-Related Hospitalizations in the United States, 2008 to 2021. JAMA Netw. Open 2023, 6, e2317641. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, J.F.; Phelan, J.; Orav, E.J.; Patel, V.; Jha, A.K. Association of Mental Health Disorders with Health Care Spending in the Medicare Population. JAMA Netw. Open 2020, 3, e201210. [Google Scholar] [CrossRef]
- Sporinova, B.; Manns, B.; Tonelli, M.; Hemmelgarn, B.; MacMaster, F.; Mitchell, N.; Au, F.; Ma, Z.; Weaver, R.; Quinn, A. Association of Mental Health Disorders with Health Care Utilization and Costs Among Adults with Chronic Disease. JAMA Netw. Open 2019, 2, e199910. [Google Scholar] [CrossRef]
- Peahl, A.F.; Gourevitch, R.A.; Luo, E.M.; Fryer, K.E.; Moniz, M.H.; Dalton, V.K.; Fendrick, A.M.; Shah, N. Right-Sizing Prenatal Care to Meet Patients’ Needs and Improve Maternity Care Value. Obstet. Gynecol. 2020, 135, 1027–1037. [Google Scholar] [CrossRef]
- Woo, V.G.; Lundeen, T.; Matula, S.; Milstein, A. Achieving higher-value obstetrical care. Am. J. Obstet. Gynecol. 2017, 216, 250–255. [Google Scholar] [CrossRef]
- Gareau, S.; Lopez-De Fede, A.; Loudermilk, B.L.; Cummings, T.H.; Hardin, J.W.; Picklesimer, A.H.; Crouch, E.; Covington-Kolb, S. Group Prenatal Care Results in Medicaid Savings with Better Outcomes: A Propensity Score Analysis of CenteringPregnancy Participation in South Carolina. Matern. Child Health J. 2016, 20, 1384–1393. [Google Scholar] [CrossRef]
- Shen, Y.; Lo-Ciganic, W.H.; Segal, R.; Goodin, A.J. Prevalence of substance use disorder and psychiatric comorbidity burden among pregnant women with opioid use disorder in a large administrative database, 2009–2014. J. Psychosom. Obstet. Gynecol. 2020, 1–7. [Google Scholar] [CrossRef]
- Short, V.L.; Hand, D.J.; MacAfee, L.; Abatemarco, D.J.; Terplan, M. Trends and disparities in receipt of pharmacotherapy among pregnant women in publically funded treatment programs for opioid use disorder in the United States. J. Subst. Abuse Treat. 2018, 89, 67–74. [Google Scholar] [CrossRef]
- Cox, E.Q.; Sowa, N.A.; Meltzer-Brody, S.E.; Gaynes, B.N. The Perinatal Depression Treatment Cascade: Baby Steps Toward Improving Outcomes. J. Clin. Psychiatry 2016, 77, 1189–1200. [Google Scholar] [CrossRef]
- Kozhimannil, K.B.; Trinacty, C.M.; Busch, A.B.; Huskamp, H.A.; Adams, A.S. Racial and Ethnic Disparities in Postpartum Depression Care Among Low-Income Women. Psychiatric Serv. 2011, 62, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Howell, E.A. Reducing Disparities in Severe Maternal Morbidity and Mortality. Clin. Obstet. Gynecol. 2018, 61, 387–399. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S. Advancing Racial Equity in Maternal Mental Health Policy; The Center for Law and Social Policy: Washington, DC, USA, 2021. [Google Scholar]
- Daw, J.R.; Hatfield, L.A.; Swartz, K.; Sommers, B.D. Women in The United States Experience High Rates of Coverage ‘Churn’ in Months before and after Childbirth. Health Aff. 2017, 36, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Daw, J.R.; Kozhimannil, K.; Admon, L.K. High Rates of Perinatal Insurance Churn Persist after the ACA. Health Aff. Blog 2019. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).