Promoting Sexual Health in Colorectal Cancer Patients and Survivors: Results from a Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
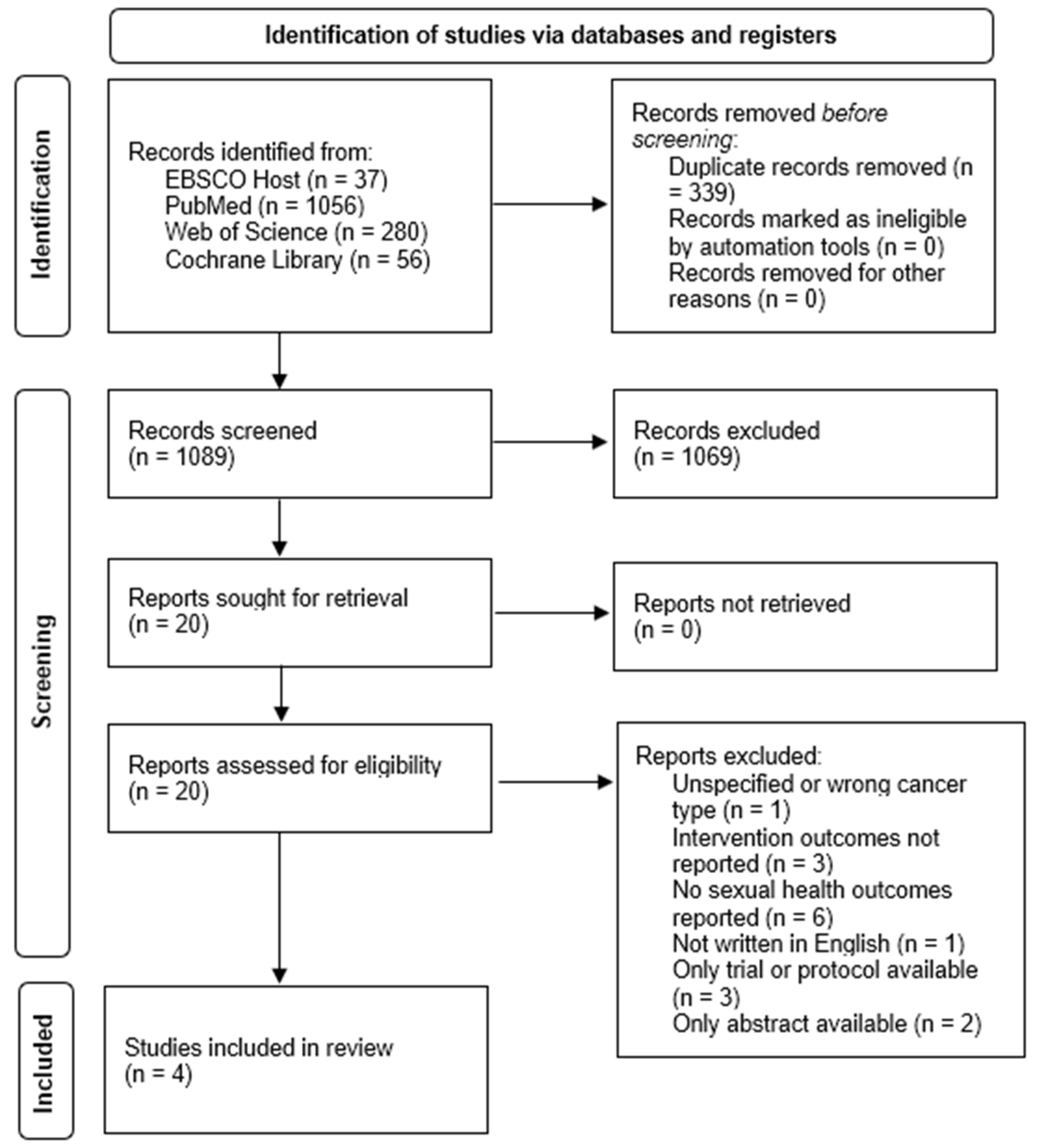
2.2. Literature Search Strategy and Study Selection
2.3. Eligibility Criteria and Data Extraction
3. Results
| Authors (Year), Country | Aims | Study Design | Participants | Intervention | Duration | Measures |
|---|---|---|---|---|---|---|
| Reese et al. (2012) [34], USA | To collect preliminary data on the feasibility and efficacy of a telephone-based couples intimacy enhancement (IE) intervention protocol. | Pilot feasibility study | N = 9 couples (CRC patients and partners) Age: M = 61.6 (SD = 14.5) | Intimacy Enhancement Intervention | Four weekly 50 min telephone-based sessions | Utilization of skills Program evaluation ISS FSFI DSCS MSIS DAS-4 |
| Outcomes | Program evaluation Considered “quite a bit” easy to participate in, overall helpful, and important for people with CRC for at least 83% of participants; 78% liked the telephone-based format; 72% reported it was “quite a bit” helpful in enhancing intimacy. Preliminary effect sizes CCR Patients: ≥0.80 for sexual distress, female sexual function, and sexual communication; between 0.30 and 0.60 for dyadic adjustment; between 0.20 and 0.30 for intimacy and male sexual function. Spouses: >0.80 for female sexual function; between 0.30 and 0.60 for remaining outcomes. Key Findings IE Intervention may be feasible and effective for CCR survivors and their spouses. | |||||
| Reese et al. (2014) [36], USA | To assess the feasibility, acceptability, and preliminary efficacy of a telephone-based couples IE intervention protocol. | Randomized pilot trial | N = 23 couples (CRC patients and partners; IE group n = 10, control group n = 8) Age: M = 52.6 (SD = 10.6) | Intimacy Enhancement Intervention | Four weekly 50 min telephone-based sessions | ISS DSCS MSIS FSFI IIEF Medical impact subscale of SFQ Self-Efficacy |
| Outcomes | Feasibility and acceptability Participation: 10 couples completed the full program. Program evaluation and skill utilization: overall favourable program evaluation; skills utilized by most participants during the past 2 weeks. Preliminary efficacy Effect sizes for CRC patients: large for female sexual function; medium to large for the reduction of medical impact on sexual function, self-efficacy, and male sexual function; no effect on sexual distress nor intimacy; negative for sexual communication and two self-efficacy items. Effect sizes for partners: large for sexual communication, male sexual function, and two self-efficacy items; medium to large for sexual distress; medium for medical impact on sexual function, intimacy, and one self-efficacy item. Key findings IE intervention may be feasible for improving CRC patients and partners’ physical and emotional intimacy. | |||||
| DuHamel et al. (2016) [38], USA | To evaluate the efficacy of pilot, telephone-based Cancer Survivorship Intervention–Sexual Health (CSI-SH) | Randomized controlled trial | N = 70 female rectal or anal cancer survivors (n = 33 intervention; n = 37 usual care) RC = 69.6% | Cancer Survivorship Intervention–Sexual Health (CSI-SH) | Four individual, 1-h, in-person or telephone sessions. | FSFI IES-R BSI EORTC-QLQ-C30 |
| Outcomes | Sexual Functioning and Psychological Distress Follow-up 1: improvement in all scores compared to baseline. Follow-up 2: equivalent results to follow-up 1. Intervention’s effect sizes Follow-up 1: medium range. Follow-up 2: QLQ-C30 emotional functioning and FSFI lubrication presented larger effect sizes at follow-up 2; remaining measures had smaller effect sizes than at follow-up 1. Linear regression Follow-up 1: significant treatment effects for IES total cancer-specific stress and QLQ-C30 emotional functioning, both improved. Follow-up 2: significant treatment effect for QLQ-C30 emotional functioning; higher IES total cancer-specific distress found for married participants. Key findings CSI-SH does not lead to significant improvements in sexual functioning. CSI-SH may lead to improvements in quality-of-life dimensions. CSI-SH is more beneficial for sexually active women and rectal and anal cancer survivors. | |||||
| Brotto et al. (2017) [31], Canada | To assess the efficacy of an online adaptation of a face-to-face psychoeducational and mindfulness-based programme for sexual difficulties. | Quantitative: baseline, follow-up 1, and follow-up 2. No control group. Qualitative: Interviews. | Total N = 61 CCR N = 8 women, 15 men (the remaining sample has other types of cancer) | Psychoeducational Intervention for Sexual Health in Cancer Survivors (OPES) | 12 weekly topics, 60 min per topic | DAS BDI Qualitative interviews. |
| Outcomes | Program Acceptability Duration: M = 29.9 weeks (SD = 19.4), range 8–111 weeks Informativeness: M = 3.62 (SD = 0.74), i.e., “moderately” and “very much”. Difficulty understanding information: M = 1.58 (SD = 0.79), i.e., “not at all” and “a little”. Sex-related distress Women: more destressed at baseline; significant decrease; further reduction at 6-month follow up. Men: no significant decrease. Sexual Functioning Women: significant improvement in all measured aspects. Men: significant improvement in intercourse satisfaction. Dyadic Adjustment Women: no significant change in consensus, satisfaction, nor cohesion. Men: significant decrease in consensus, no significant change in satisfaction nor cohesion. Mood Women: more depressive symptoms at baseline; significant decrease. Men: no significant decrease in depressive symptoms. Qualitative Interviews Opportunities for self-reflection, newfound sense of intimacy with partners, enjoyment of the online format, enjoyment of homework, and step-by-step instructions. Key findings Feasibility was found for an online mindfulness-based intervention for sexual concerns. Female and male cancer survivors may have different intervention needs. | |||||
3.1. Intimacy Enhancement (IE) Intervention
3.2. Psychoeducational Intervention for Sexual Health in Cancer Survivors (OPES)
3.3. Cancer Survivorship Intervention–Sexual Health (CSI-SH)
3.4. Risk of Bias
4. Discussion
4.1. Study Limitations
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Prz. Gastroenterol. 2019, 14, 89–103. [Google Scholar] [CrossRef]
- Wiltink, L.M.; White, K.; King, M.T.; Rutherford, C. Systematic review of clinical practice guidelines for colorectal and anal cancer: The extent of recommendations for managing long-term symptoms and functional impairments. Support Care Cancer 2020, 28, 2523–2532. [Google Scholar] [CrossRef] [PubMed]
- Johdi, N.A.; Sukor, N.F. Colorectal cancer immunotherapy: Options and strategies. Front. Immunol. 2020, 11, 1624. [Google Scholar] [CrossRef] [PubMed]
- Averyt, J.C.; Nishimoto, P.W. Psychosocial issues in colorectal cancer survivorship: The top ten questions patients may not be asking. J. Gastrointest. Oncol. 2014, 5, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Cotrim, H.; Pereira, G. Impact of colorectal cancer on patient and family: Implications for care. Eur. J. Oncol. Nurs. 2008, 12, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Denlinger, C.S.; Barsevick, A.M. The challenges of colorectal cancer survivorship. J. Natl. Compr. Cancer Netw. 2009, 7, 883–894. [Google Scholar] [CrossRef]
- El-Shami, K.; Oeffinger, K.C.; Erb, N.L.; Willis, A.; Bretsch, J.K.; Pratt-Chapman, M.L.; Cannady, R.S.; Wong, S.L.; Rose, J.; Barbour, A.L.; et al. American cancer society colorectal cancer survivorship care guidelines: American cancer society colorectal cancer survivorship care guidelines. CA Cancer J. Clin. 2015, 65, 428–455. [Google Scholar] [CrossRef] [PubMed]
- Han, C.J.; Yang, G.S.; Syrjala, K. Symptom experiences in colorectal cancer survivors after cancer treatments: A systematic review and meta-analysis. Cancer Nurs. 2020, 43, E132–E158. [Google Scholar] [CrossRef] [PubMed]
- Chokshi, A.; Belekar, D.M.; Chokshi, S. Sexual health of colorectal cancer patients—A systematic review. Indian J. Surg. 2022, 8, 5–15. [Google Scholar] [CrossRef]
- Den Oudsten, B.L.; Traa, M.J.; Thong, M.S.Y.; Martijn, H.; De Hingh, I.H.J.T.; Bosscha, K.; van de Poll-Franse, L.V. Higher prevalence of sexual dysfunction in colon and rectal cancer survivors compared with the normative population: A population-based study. Eur. J. Cancer 2012, 48, 3161–3170. [Google Scholar] [CrossRef]
- Stulz, A.; Lamore, K.; Montalescot, L.; Favez, N.; Flahault, C. Sexual health in colon cancer patients: A systematic review. Psychooncology 2020, 29, 1095–1104. [Google Scholar] [CrossRef]
- Traa, M.J.; De Vries, J.; Roukema, J.A.; Den Oudsten, B.L. Sexual (dys)function and the quality of sexual life in patients with colorectal cancer: A systematic review. Ann. Oncol. 2012, 23, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Acquati, C.; Hendren, S.; Wittmann, D.; Reese, J.B.; Karam, E.; Duby, A.; Dunn, K.B.; Kayser, K. Psychological and sexual distress in rectal cancer patients and partners. Oncol. Nurs. Forum. 2022, 31, 920–928. [Google Scholar] [CrossRef]
- Sutsunbuloglu, E.; Vural, F. Evaluation of sexual satisfaction and function in patients following stoma surgery: A descriptive study. Sex. Disabil. 2018, 36, 349–361. [Google Scholar] [CrossRef]
- Flynn, K.E.; Reese, J.B.; Jeffery, D.D.; Abernethy, A.P.; Lin, L.; Shelby, R.A.; Porter, L.S.; Dombeck, C.B.; Weinfurt, K.P. Patient experiences with communication about sex during and after treatment for cancer: Patient-provider communication about sex. Psychooncology 2012, 21, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Donovan, K.A.; Thompson, L.M.A.; Hoffe, S.E. Sexual function in colorectal cancer survivors. Cancer Control 2010, 17, 44–51. [Google Scholar] [CrossRef]
- Traa, M.J.; De Vries, J.; Roukema, J.A.; Rutten, H.J.T.; Den Oudsten, B.L. The sexual health care needs after colorectal cancer: The view of patients, partners, and health care professionals. Support Care Cancer 2014, 22, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, B.C. Sexual Health Needs and Concerns after Colorectal Cancer. 2022. Available online: https://repositorio-aberto.up.pt/handle/10216/145580 (accessed on 14 December 2022).
- Mohamed, N.E.; Shah, Q.N.; Kata, H.E.; Sfakianos, J.; Given, B. Dealing with the unthinkable: Bladder and colorectal cancer patients’ and informal caregivers’ unmet needs and challenges in life after ostomies. Semin. Oncol. Nurs. 2021, 37, 151111. [Google Scholar] [CrossRef]
- Traa, M.J.; Braeken, J.; De Vries, J.; Roukema, J.A.; Slooter, G.D.; Crolla, R.M.P.H.; Borremans, M.P.M.; Den Oudsten, B.L. Sexual, marital, and general life functioning in couples coping with colorectal cancer: A dyadic study across time: Dyadic functioning. Psychooncology 2015, 24, 1181–1188. [Google Scholar] [CrossRef] [PubMed]
- Dau, H.; Safari, A.; Saad El Din, K.; McTaggart-Cowan, H.; Loree, J.M.; Gill, S.; Gill, M.A. Assessing how health information needs of individuals with colorectal cancer are met across the care continuum: An international cross-sectional survey. BMC Cancer 2020, 20, 1031. [Google Scholar] [CrossRef]
- Santin, O.; Murray, L.; Prue, G.; Gavin, A.; Gormley, G.; Donnelly, M. Self-reported psychosocial needs and health-related quality of life of colorectal cancer survivors. Eur. J. Oncol. Nurs. 2015, 19, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Breukink, S.O.; Donovan, K.A. Physical and psychological effects of treatment on sexual functioning in colorectal cancer survivors. J. Sex. Med. 2013, 10 (Suppl. 1), 74–83. [Google Scholar] [CrossRef]
- Reese, J.B.; Haythornthwaite, J.A. Importance of sexuality in colorectal cancer: Predictors, changes, and response to an intimacy enhancement intervention. Support Care Cancer 2016, 24, 4309–4317. [Google Scholar] [CrossRef]
- Arthur, E.K.; Wills, C.E.; Menon, U. A systematic review of interventions for sexual well-being in women with gynecologic, anal, or rectal cancer. Oncol. Nurs. Forum. 2018, 45, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.S.; Kim, H.-K.; Park, S.M.; Kim, J.-H. Online-based interventions for sexual health among individuals with cancer: A systematic review. BMC Health Serv. Res. 2018, 18, 167. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Quality Assessment Tool for Quantitative Studies. Effective Public Healthcare Panacea Project. 2019. Available online: https://www.ephpp.ca/quality-assessment-tool-for-quantitative-studies/ (accessed on 14 December 2022).
- Beck, A.T.; Beamesderfer, A. Assessment of depression: The depression inventory. Mod. Probl. Pharmacopsychiatry 1974, 7, 151–169. [Google Scholar] [CrossRef]
- Brotto, L.A.; Dunkley, C.R.; Breckon, E.; Carter, J.; Brown, C.; Daniluk, J.; Miller, D. Integrating quantitative and qualitative methods to evaluate an online psychoeducational program for sexual difficulties in colorectal and gynecologic cancer survivors. J. Sex. Marital. Ther. 2017, 43, 645–662. [Google Scholar] [CrossRef] [PubMed]
- Spanier, G.B. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J. Marriage Fam. 1976, 38, 15. [Google Scholar] [CrossRef]
- Sabourin, S.; Valois, P.; Lussier, Y. Development and validation of a brief version of the dyadic adjustment scale with a nonparametric item analysis model. Psychol. Assess 2005, 17, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Reese, J.B.; Porter, L.S.; Somers, T.J.; Keefe, F.J. Pilot feasibility study of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. J. Sex. Marital. Ther. 2012, 38, 402–417. [Google Scholar] [CrossRef]
- Catania, J. Help-Seeking: An Avenue for Adult Sexual Development. Doctoral Dissertation, University of California, San Francisco, CA, USA, 1986. [Google Scholar]
- Reese, J.B.; Porter, L.S.; Regan, K.R.; Keefe, F.J.; Azad, N.S.; Diaz, L.A., Jr.; Herman, J.M.; Haythornthwaite, J.A. A randomized pilot trial of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer: Telephone-based couples intervention. Psychooncology 2014, 23, 1005–1013. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.J.M.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- DuHamel, K.; Schuler, T.; Nelson, C.; Philip, E.; Temple, L.; Schover, L.; Baser, R.E.; Starr, T.D.; Cannon, K.; Jennings, S.; et al. The sexual health of female rectal and anal cancer survivors: Results of a pilot randomized psycho-educational intervention trial. J. Cancer Surviv. 2016, 10, 553–563. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Clayton, A.H.; Lewis-D’Agostino, D.; Wunderlich, G.; Fu, Y. Validation of the Female Sexual Distress Scale-Revised for Assessing Distress in Women with Hypoactive Sexual Desire Disorder. J. Sex. Med. 2008, 5, 357–364. [Google Scholar] [CrossRef]
- Rosen, R.; Brown, C.; Heiman, J.; Leiblum, S.; Meston, C.; Shabsigh, R.; Ferguson, D.; D’Agostino, R. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J. Sex. Marital. Ther. 2000, 26, 191–208. [Google Scholar] [CrossRef]
- Weiss, D.S. The Impact of Event Scale: Revised. In Cross-Cultural Assessment of Psychological Trauma and PTSD; Springer: Boston, MA, USA, 2007; pp. 219–238. [Google Scholar]
- Hudson, W.W.; Harrison, D.F.; Crosscup, P.C. A short-form scale to measure sexual discord in dyadic relationships. J. Sex. Res. 1981, 17, 157–174. [Google Scholar] [CrossRef]
- Rosen, R.C.; Riley, A.; Wagner, G.; Osterloh, I.H.; Kirkpatrick, J.; Mishra, A. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology 1997, 49, 822–830. [Google Scholar] [CrossRef]
- Miller, R.S.; Lefcourt, H.M. The assessment of social intimacy. J. Pers. Assess 1982, 46, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Syrjala, K.L.; Schroeder, T.C.; Abrams, J.R.; Atkins, T.Z.; Brown, W.S.; Sanders, J.E.; Schubert, M.A.; Heiman, J.R. Sexual function measurement and outcomes in cancer survivors and matched controls. J. Sex. Res. 2000, 37, 213–225. [Google Scholar] [CrossRef]
- Adams, S.G.; Dubbert, P.M.; Chupurdia, K.M.; Jones, A.; Lofland, K.R.; Leermakers, E.A. Assessment of sexual beliefs and information in aging couples with sexual dysfunction. Arch. Sex. Behav. 1996, 25, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Ussher, J.M.; Perz, J.; Gilbert, E.; Wong, W.K.; Hobbs, K. Renegotiating sex and intimacy after cancer. Cancer Nurs. 2013, 36, 454–462. [Google Scholar] [CrossRef]
- Badr, H.; Bakhshaie, J.; Chhabria, K. Dyadic interventions for cancer survivors and caregivers: State of the science and new directions. Semin. Oncol. Nurs. 2019, 35, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Badr, H.; Krebs, P. A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer: Couples meta-analysis. Psychooncology 2013, 22, 1688–1704. [Google Scholar] [CrossRef] [PubMed]
- Perz, J.; Ussher, J.M.; Australian Cancer and Sexuality Study Team. A randomized trial of a minimal intervention for sexual concerns after cancer: A comparison of self-help and professionally delivered modalities. BMC Cancer 2015, 15, 629. [Google Scholar] [CrossRef] [PubMed]
- Reese, J.B.; Smith, K.C.; Handorf, E.; Sorice, K.; Bober, S.L.; Bantug, E.T.; Schwartz, S.; Porter, L.S. A randomized pilot trial of a couple-based intervention addressing sexual concerns for breast cancer survivors. J. Psychosoc. Oncol. 2019, 37, 242–263. [Google Scholar] [CrossRef]
- Schover, L.R.; Canada, A.L.; Yuan, Y.; Sui, D.; Neese, L.; Jenkins, R.; Rhodes, M.M. A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment: CAREss Counseling Program. Cancer 2012, 118, 500–509. [Google Scholar] [CrossRef]
- Scott, J.L.; Halford, W.K.; Ward, B.G. United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J. Consult. Clin. Psychol. 2004, 72, 1122–1135. [Google Scholar] [CrossRef]
- Riper, H.; Andersson, G.; Christensen, H.; Cuijpers, P.; Lange, A.; Eysenbach, G. Theme Issue on E-Mental Health: A Growing Field in Internet Research. J. Med. Internet Res. 2010, 12, e74. [Google Scholar] [CrossRef]
- Wang, K.; Ariello, K.; Choi, M.; Turner, A.; Wan, B.A.; Yee, C.; Rowbottom, L.; Macdonald, R.; Lam, H.; Drost, L.; et al. Sexual healthcare for cancer patients receiving palliative care: A narrative review. Ann. Palliat. Med. 2017, 7, 256–264. [Google Scholar] [CrossRef]
| Selection Bias | Study Design | Confounders | Blinding | Data Collection Method | Withdrawals and Dropouts | Global Rating | |
|---|---|---|---|---|---|---|---|
| Reese et al. (2012) [34] | Weak | Weak | Weak | Weak | Strong | Strong | Weak |
| Reese et al. (2014) [36] | Weak | Strong | Strong | Weak | Strong | Weak | Weak |
| DuHamel et al. (2016) [38] | Weak | Strong | Strong | Weak | Strong | Weak | Weak |
| Brotto et al. (2017) [31] | Weak | Weak | Weak | Weak | Strong | Weak | Weak |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rocha, H.B.; Carneiro, B.C.; Vasconcelos, P.A.; Pereira, R.; Quinta-Gomes, A.L.; Nobre, P.J. Promoting Sexual Health in Colorectal Cancer Patients and Survivors: Results from a Systematic Review. Healthcare 2024, 12, 253. https://doi.org/10.3390/healthcare12020253
Rocha HB, Carneiro BC, Vasconcelos PA, Pereira R, Quinta-Gomes AL, Nobre PJ. Promoting Sexual Health in Colorectal Cancer Patients and Survivors: Results from a Systematic Review. Healthcare. 2024; 12(2):253. https://doi.org/10.3390/healthcare12020253
Chicago/Turabian StyleRocha, Hélia B., Bruna C. Carneiro, Priscila A. Vasconcelos, Raquel Pereira, Ana Luísa Quinta-Gomes, and Pedro J. Nobre. 2024. "Promoting Sexual Health in Colorectal Cancer Patients and Survivors: Results from a Systematic Review" Healthcare 12, no. 2: 253. https://doi.org/10.3390/healthcare12020253
APA StyleRocha, H. B., Carneiro, B. C., Vasconcelos, P. A., Pereira, R., Quinta-Gomes, A. L., & Nobre, P. J. (2024). Promoting Sexual Health in Colorectal Cancer Patients and Survivors: Results from a Systematic Review. Healthcare, 12(2), 253. https://doi.org/10.3390/healthcare12020253





