Abstract
Background: Primary care physicians play a key role in initiating opioid therapy. However, knowledge gaps in opioid use and pain management are significant barriers to providing optimal care. This research study aims to investigate the educational needs of primary care physicians regarding opioid therapy and opioid use in pain management. Methods: A computer-assisted web interview (CAWI) protocol was used to collect data from primary care physicians. Drug selection criteria, knowledge of opioid substitutes and dosage, and practical use of opioid therapy were evaluated. Results: While 84% of participating physicians (724 respondents) reported initiating opioid treatment, only a minority demonstrated accurate opioid dosage calculations. Significant discrepancies between physicians’ self-perceived knowledge and their clinical skills in opioid prescribing and pain management were observed. In total, 41% of physicians incorrectly indicated dose conversion rates for tramadol (the most frequently used drug according to 65% of responders). Conclusions: Targeted educational programs are essential to bridge the knowledge gap and increase physicians’ competence in pain management. The proper self-assessment of one’s own skills may be the key to improvement. Further research should focus on developing specialized educational courses and decision-support tools for primary care physicians and examining the impact of interprofessional pain management teams on patient outcomes.
1. Introduction
The perception of pain is a major public health problem [1]. The basic premise of its treatment is to provide comprehensive support to patients experiencing pain so that they can re-engage in daily life and their previously performed duties [2]. Most often, the responsibility for the treatment of pain and the initiation of therapy with opioid drugs lies with primary care physicians. Patients’ easy access to general practitioners positions them as a key link in pain management. This can lead to many challenges and potential problems due to a lack of education and experience [3]. Deficiencies in physician education are observed both during medical school education and during internships in hospitals and apply to the rules governing opioid use, mastering the management of side effects, and knowledge of opioid abuse and misuse [4,5,6,7]. These deficiencies, when not supplemented with adequate training, become significant knowledge gaps.
Reviewing the existing literature, we noted the multifaceted nature of physicians’ educational needs regarding the proper use of opioid medications [7,8]. Opioids are a class of potent pain-relieving drugs. Opioids are highly effective and safe analgesics, and their appropriate use by competent clinicians is an important element of modern pain management. Critical side effects include respiratory depression, drowsiness, constipation, and nausea. Long-term use can lead to physical dependence and withdrawal symptoms [3]. Patients undergoing opioid treatment should remain under the close supervision of well-educated medical professionals, who may be well-trained family medicine physicians. If the treatment used is not successful, the strategy should be thoroughly reviewed and adjusted [9]. The correct dose of a given opioid is the lowest possible dose that provides the desired effect. When it is necessary to use the highest doses of an opioid, if the pain is still too intense or side effects are maximized, it is advisable to try to implement an alternative opioid drug [3,9,10]. The conversion of opioid doses is not based only on a calculation but should also take into account many other factors (health condition, age, treatment tolerance, and undesirable effects) [11].
In Poland, recommendations in accordance with the World Health Organization’s analgesic ladder are followed. They specify treatment according to the severity of pain, ranging from the use of OTC painkillers (for mild pain) to opioid drugs (for moderate-to-severe pain) [12,13,14,15,16]. However, the international literature repeatedly indicates that most often, opioids are not prescribed because of concerns about a patient’s addiction or abuse of the drug [3,17,18]. Moreover, doctors’ decisions are also influenced by other issues, such as previous professional experience in opioid prescribing [17,18], concerns about professional competence and level of education in pain management and opioid drug use [18,19,20], patients’ reluctance to take opioid drugs [21], concerns about the impact of opioid drugs on patient behavior [3,22,23], the degree of faith in opioids as an effective pain management option [18,20,22], concerns about comorbidities and potential adverse events that could result in suboptimal pain management [6,18,24], complicated procedures for prescribing opioid drugs [22,23], a lack of knowledge of standardized guidelines for opioid use in Europe [3,25] and insufficient time and available resources [26].
Studies indicate that physicians’ greater belief in the use of opioid drugs for cancer pain compared to non-cancer pain is a common phenomenon [6,27]. The majority of family physicians (83%) consider opioids to be an effective treatment for non-cancer pain. At the same time, they worry about the long-term use of these drugs and the management of their doses, which seems to be a very significant inconvenience for them in their daily clinical practice [22]. It was found that the most “liberal” approach to the topic of pain management with opioids is correlated with young physician age and having experience working in specialized oncology/palliative care units [28,29]. Many physicians find the care of patients requiring opioid medications stressful [30]. Analyses conducted in this field have shown that a doctor with extensive experience and a significant number of patients taking opioids under their care has greater confidence and a higher sense of comfort [18,31]. In contrast, a negative belief based on the finding that many patients quickly become addicted to opioids was correlated with the much less frequent prescription of such drugs [18,31]. Due to the human right to live without pain, it is necessary to understand the educational needs of primary care physicians and implement appropriate interventions to improve their knowledge. Therefore, this research study aims to investigate the educational needs of primary care physicians regarding opioid therapy and pain management in the Polish health system setting.
2. Materials and Methods
2.1. Study Design and Settings
An anonymous computer-assisted web interview (CAWI) survey was prepared as an online questionnaire directed toward doctors working in primary health care (PHC). The study was voluntary, and informed consent was collected from participants. The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) was used [32]. The survey was divided into a section collecting demographic data (5 questions) and employment information and a content section (9 questions).
The survey was developed after performing an intensive literature review on the paper’s topic and a series of interviews between the authors and key individuals related to the scope of the study. The interview answers were collected in the form of a questionnaire, using questions with open-answer options as well as Likert-scale questions. There was also a “non-response” option.
The consent of the Bioethical Committee of the Medical University of Wrocław, decision number KB 472/2020, was obtained.
For the survey, the following combination of tools was used: an online data collection platform, typeform.com, a Google Analytics web analytics system and an .xls file data collection system, that is, Google Docs. This verified that each user filled out the survey only once (IP) and also examined the level of survey abandonment during completion. These tools were launched and set. A pilot study was then performed on a group of 10 doctors, checking the clarity of the questions and how they were answered. Minor modifications were made to better clarify the issues the survey investigated.
The methodology for measuring opioid use and knowledge was based on answering 9 single-choice questions related to these issues. Key from the perspective of the problem at hand were questions addressing the following:
- Criteria for deciding which painkillers to use;
- Knowledge related to morphine substitutes and their proper doses;
- Knowledge related to the management of specific patients;
- Opioids with the highest prescription rate.
Statistical significance for the studied population of physicians was achieved.
2.2. Data Assembly (Study Period and How It Was Performed) and Collection
The questionnaire was made available to respondents in the following time frame: from 10 June 2020 to 10 September 2021. The timing of the research data collection coincided with the SARS-CoV-2 virus pandemic. The authors decided to carry out the survey in the only manner that provided full security to the respondents, i.e., through an online questionnaire. Information about the survey was communicated through classical channels (oral and written invitations; information disseminated at medical events) and close online channels (a newsletter, a website and a forum for primary care physicians in a group on facebook.com) which aimed to invite all doctors to the survey, regardless of their daily use of electronic media. The survey was available on the websites of the Polish Society of Family Medicine and the Polish Society of Palliative Medicine. The survey was open; it was not mandatory for any visitor who wanted to visit the website to complete it, and no incentive was offered in exchange for completing the survey. The criterion for inclusion in the study was working in primary health care. Participants declaring that they did not work in primary care and those who did not provide consent to participate were excluded from this study. The studied population is indicated in Figure 1.
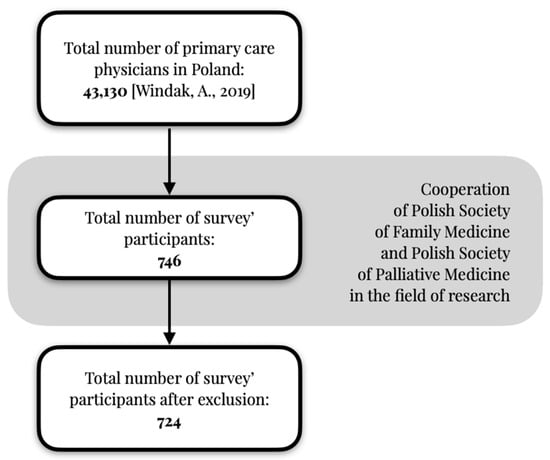
Figure 1.
Studied population of primary care physicians [32].
The research data were made available on the Polish Society of Family Medicine website (a trusted third-party site).
2.3. Statistical Approach
For the studied group of doctors working in primary care, the minimum number of respondents at the confidence level α = 0.95, at a fraction size of 0.5 and with a maximum error of 5% was 382 respondents. At the same time, it should be stated that for the subgroup of doctors specializing in family medicine, the number of respondents should have exceeded 372, and for doctors with work experience longer than 1 year, the number of respondents should have exceeded 380.
Statistica 13.1 was used for a statistical analysis. In the statistical analysis, the Shapiro–Wilk test was used to test normality. Furthermore, medians and quartile values (Q25, Q75) were used. Utilizing the chi-square test with a significance threshold of p < 0.05, this study assessed the occurrence of statistically significant differences within subpopulations of the examined physicians. This assessment included physicians with and without specializations in family medicine. Further, the assessment compared those working up to 40 h per week versus those working over 40 h. Finally, all participants were categorized into subgroups based on the duration of their professional experience. The findings are detailed in tables that are included in the Supplementary Materials of this publication.
3. Results
3.1. General Characteristics of Participants
Of all respondents, more than 85% had a professional length of service as a primary care physician of at least one year, with more than half of the doctors working in PHC for at least six years. The vast majority of respondents mentioned PHC as their main place of work (87.6%), and only a minority of them (3.3%) worked in palliative care at the same time. Over 77% (Q75) of the respondents to the questionnaire were family medicine specialists or in training for this specialization. The occupational characteristics of the respondents are presented in Table 1.

Table 1.
Participant characteristics.
3.2. The Choice of Pain Medication and Opioid Prescription
The first question of the survey concerned the main criterion that determined the choice of pain medication (Table 2). Family physicians in Poland claim that they choose analgesics in accordance with current medical knowledge, based on a clear clinical rationale, such as pain intensity, as measured using a pain rating scale (53% of respondents), the nature of pain (27%) and the rate of pain changes (12%) (Table 2). Another important issue that respondents were asked about was the writing of prescriptions for opioid drugs. Nearly 54% of general practitioners said they initiate pain treatment with weak or strong opioids as needed. There was no statistical significance of the observations in the subgroup of examined physicians [Supplementary Tables S1–S3].

Table 2.
Criteria for the choice of pain medication and opioid prescription statements.
3.3. Primary Care Physician Knowledge on the Topic of Opioid Usage
The respondents were then asked two separate questions about morphine and its substitutes, that is, to indicate what doses of morphine correspond to 400 mg of tramadol and 35 μg of buprenorphine (Table 3). The question was formulated based on the knowledge requirements from the specialization examination for family doctors in Poland. The purpose of this question was to objectify doctors’ declarations regarding the use of painkillers. As many as 42% and 48% of general practitioners, respectively, declared no knowledge or skills to convert the correct dose of morphine. Moreover, a further 39% (for tramadol conversion) and 33% (buprenorphine) incorrectly converted doses. In the case of a patient with NRS 6/10 pain, only every fourth respondent indicated the need to use drugs from the third step of the analgesic ladder.

Table 3.
Practical questions testing the ability to calculate the dose of an opioid drug and case studies checking the ability of primary care physicians to properly manage pain treatment.
Subsequently, the study participants were presented with two clinical cases for which they were asked to suggest a course of action to reduce patients’ pain. Table 3 shows the numerical values corresponding to the number of specific responses. Almost 73% of doctors do not attempt to adjust the dose of morphine despite the presence of obvious clinical indications.
Another question in the survey asked about the opioid medications most commonly used in daily medical practice (Table 4). The analysis shows that only 3.7% of respondents use an orally administered morphine treatment. Statistical significance was not achieved for the observation of declarations of preferable opioid drugs chosen by physicians.

Table 4.
Most chosen opioids (declarations), coanalgesic drug introduction and the most difficult part of pain treatment in daily primary care practice.
Further analysis showed that nearly 72% of respondents choose to implement coanalgesic drugs when pain of significant severity is diagnosed (Table 4). One of the most important questions for the problem at hand, also concerned the identification of the most difficult element of pain treatment in the daily practice of primary care physicians (Table 4). No statistical significance was demonstrated between study subgroups [Supplementary Tables S1–S3].
3.4. Comparison of the Right Clinical Decision with the Percentage of Doctors Declaring Opioid Use
In the surveyed group of physicians, a declarative 84% include treatment with drugs from levels II and/or III of the analgesic ladder (Figure 2). Furthermore, as little as 25% of physicians initiating opioid therapy and less than 10% of physicians using tramadol or buprenorphine in their practice correctly recalculate opioid doses, while when asked about the practical use of opioid drugs, 64% and 27%, respectively, incorrectly select clinical management. The group of examined doctors with specialties other than family medicine in the entire study group did not have a statistically significant impact on the overall result, which was calculated.
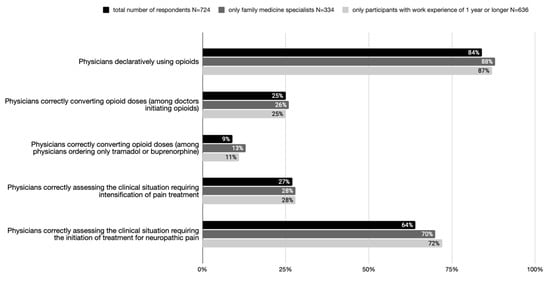
Figure 2.
Percentage of doctors making the right clinical decision compared to percentage of doctors declaring opioid use.
4. Discussion
4.1. Main Findings
The main findings of this study show the disproportion between the declarative use of opioids in pain therapy (84% of respondents) and actual knowledge regarding their administration (the correct conversion of opioid doses in the case of 9% of physicians ordering only tramadol or buprenorphine and 25% of physicians initiating opioids).
Previous studies were conducted mainly on groups other than primary care physicians (pre-graduation), as in the study by Pieters et al. [4]. In the systematic review of Hooten et al., physicians reported a high level of awareness of the potential for opioid misuse and were concerned about inadequate prior training in pain management [6]. In the opinion of the authors, based on the collected results, this fact can be questioned. Doctors overestimate their skills and incorrectly define their state of knowledge.
In a 2014 study by Jamison et al. examining primary care physicians, respondents expressed concern about medication misuse (89%) and felt that managing patients with chronic pain was stressful (84%). Most were worried about addiction (82%). At the same time, only less than half felt that they were sufficiently trained in prescribing opioids (46%) [33]. An analysis of the scientific literature indicates that physicians have a limited ability to reliably self-assess their skills and competencies [34,35,36,37]. Significant discrepancies between the belief in one’s own knowledge about the use of opioid analgesics and one’s actual skills in this area carry significant risks for patients suffering from pain [34]. A primary care physician convinced of their own skills is at risk of making more mistakes, mistaking a drug or its dosage and finally, may have difficulty meeting the basic tenets of effective pain therapy (adequacy, avoiding side effects) [34].
The authors agree with the general conclusions of the systematic review by Carey et al., which indicated available comprehensive training for primary care practitioners is likely needed to address issues of low confidence [37]. In our opinion, it is important not to base the development of training solely on the subjective needs reported by primary care physicians. There should not only be dedicated training at the pre-graduation stage. They must (not only “ideally” [37] but actually) take into account the needs of primary care physicians, including the inadequate assessment of skills in relation to their actual usage in clinical practice. In their work, Green at al. draw attention to the five key roles of the primary care physician in palliative care from the points of view of patients and their caregivers. They include knowledge and competence. The perspective of the patient, who is predominantly unable to assess the correctness of the doctor’s work, is important in our opinion [38]. Difficulty arises when, as we have shown, the doctor does not correctly assess their skills.
4.2. What This Study Provides
The factor in the form of a subjective belief in one’s own skills that stands in contrast to actual skills should, in our opinion, be added to the deficiencies in education, accessibility difficulties, prejudice and legislation identified in the literature as another factor that significantly limits the proper management of pain treatment. An important element to consider, therefore, when designing educational and clinical decision support solutions and targeting primary care physicians should be the proper determination of actual, rather than declarative, knowledge [33].
Juxtaposing data obtained from questions about actual clinical situations with data on the use of specific drug groups helps identify issues that need to be addressed in educational programs for primary care physicians. Properly conducted research can also help create an educational program for training doctors. Doctors claim difficulties in titrating morphine, for example. However, they mention it as the least frequently used opioid drug. The declaration (in terms of the frequency of morphine use) juxtaposed with the description of the difficulties (lack of titration skills) indicates the most important issues that need to be addressed when creating educational programs for doctors.
The authors of this paper carried out a process of creating an educational course and a decision support solution for opioid medication rotation [9] based on the results of the presented study.
One of the important elements for improving the effectiveness of the implemented pain treatment strategies and improving the safety of the applied therapy in the primary care setting is the provision of access to pain management teams [37,39] through the presence of interdisciplinary teams giving the family doctor the opportunity to consult or by referring the patient to readily available pain management teams (clinics).
4.3. Strengths and Limitations
The survey covered a significant number of primary care physicians working in Poland, ensuring a broad representation of this group and increasing the generalizability of the results, while the use of an online survey for data collection allowed for easy access, reduced the data collection time and acquired responses from physicians across the country. The response rate is consistent with that expected from the literature [40] and from similar studies conducted in Poland using the CAWI method. The study focused on determining the educational needs of primary care physicians in terms of not only declarative knowledge or skills possessed but both.
The results of the survey are based on self-reported assessments of physicians regarding their knowledge and skills, which may not fully reflect their actual behavior in clinical practice, though it does allow for an assessment of the discrepancy between self-assessments of their competence and their actual skills. The research design did not include any interventions, which limits the ability to establish causal relationships between educational programs and improved pain management. Although the authors made efforts to obtain representativeness in the group, statistical significance was obtained, and a group of over 1% of all primary care physicians was examined; it should be noted that in this study, no selection was made of the surveyed participants in terms of representation (gender, age, or place). It should be noted that for doctors specializing in family medicine for p < 0.05, the required number of study participants was not achieved. Subsequent research should focus on this group to determine whether the observed differences are statistically significant.
The aim of this study was not to determine the circumstances of introducing opioid drugs in primary health care. Further research should focus on identifying whether primary care physicians effectively implement and modify treatment depending on the nature of the pain (acute pain; chronic pain). Future research studies can focus on types of problems that doctors encounter in patients treated chronically with opioids and their correlation with treatment errors. This may provide an answer as to whether the side effects that patients complain about are correlated with the properties of a drug or its improper use.
This study showed a significant number of incorrect answers and a lack of self-awareness of doctors when providing them. Further research is required to determine the causes of these errors, the correlation between knowledge and treatment management and how to address this via education programs or other solutions.
5. Conclusions
The proper self-assessment of one’s own skills may be the key to improving pain management in primary care. Targeted educational programs are essential to bridging the knowledge gap and increasing physicians’ competence in opioid therapy and pain management. Solutions that objectify pain treatment should be implemented in everyday medical practice (both the use of appropriate tools and scales and support for clinical decision making). Further research should focus on developing specialized educational courses and decision-support tools for primary care physicians and examining the impact of interprofessional pain management teams on patient outcomes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare12020217/s1, Tables of data (Tables S1–S3): Pearson’s chi-square test used to determine a statistically significant differences between the subgroups of respondents.
Author Contributions
Conceptualization, methodology, formal analysis, and investigation: A.M.B., A.M.-M. and A.C.-R.; writing—original draft preparation: A.M.B.; writing—review and editing: A.M.B., A.M.-M. and A.C.-R.; validation: A.M.B., A.M.-M. and A.C.-R.; visualization: A.M.B.; supervision: A.M.-M. and A.C.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Wroclaw Medical University, SUBZ.C290.24.054.
Institutional Review Board Statement
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and relevant local and national regulations and guidelines. The consent of the Bioethical Committee of the Medical University of Wrocław was obtained (decision number KB 472/2020, approval date 9 July 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data and materials generated during this study are available freely upon request from the Polish Society of Family Medicine web page.
Acknowledgments
All individuals listed as authors have contributed significantly to the conception, design, execution, or interpretation of the research study.
Conflicts of Interest
Author Aleksander Biesiada was employed by the company Family Physician Office S&M Ltd. The authors declare that this study received funding from the Wrocław Medical University. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef]
- Zimmermann, A.; Mędrzycka-Dąbrowska, W.; Zagłoba, M. Patient’s right to pain treatment. Palliat. Med. Pract. 2018, 12, 11–19. [Google Scholar]
- O’Brien, T.; Christrup, L.; Drewes, A.; Fallon, M.; Kress, H.; McQuay, H.; Mikus, G.; Morlion, B.; Perez-Cajaraville, J.; Pogatzki-Zahn, E.; et al. European Pain Federation position paper on appropriate opioid use in chronic pain management. Eur. J. Pain 2017, 21, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Pieters, J.; Dolmans, D.H.J.M.; Verstegen, D.M.L.; Warmenhoven, F.C.; Courtens, A.M.; van den Beuken-van Everdingen, M.H.J. Palliative care education in the undergraduate medical curricula: Students’ views on the importance of, their confidence in, and knowledge of palliative care. BMC Palliat. Care 2019, 18, 72. [Google Scholar] [CrossRef]
- The European Pain Federation (EFIC) 2013. APPEAL (Advancing Provision of Pain Education and Learning) Study. Available online: http://hepmp.med.bg.ac.rs/wp-content/uploads/2018/01/Pain_APPEAL-Study_Backgrounder-dok.pdf (accessed on 27 July 2023).
- Hooten, W.M.; Dvorkin, J.; Warner, N.S.; Pearson, A.C.; Murad, M.H.; Warner, D.O. Characteristics of physicians who prescribe opioids for chronic pain: A meta-narrative systematic review. J. Pain Res. 2019, 12, 2261–2289. [Google Scholar] [CrossRef] [PubMed]
- Alford, D.P. Opioid Prescribing for Chronic Pain—Achieving the Right Balance through Education. N. Engl. J. Med. 2016, 374, 301–303. [Google Scholar] [CrossRef] [PubMed]
- Polacek, C.; Christopher, R.; Mann, M.; Udall, M.; Craig, T.; Deminski, M.; Sathe, N.A. Healthcare professionals’ perceptions of challenges to chronic pain management. Am. J. Manag. Care 2020, 26, e135–e139. [Google Scholar] [CrossRef]
- Polish Society of Family Medicine. Online Calculator to Convert Opioid Doses. Available online: https://kalkulatoropioidow.pl/ (accessed on 25 July 2023).
- Häuser, W.; Morlion, B.; Vowles, K.E.; Bannister, K.; Buchser, E.; Casale, R.; Chenot, J.; Chumbley, G.; Drewes, A.M.; Dom, G.; et al. European* clinical practice recommendations on opioids for chronic noncancer pain—Part 1: Role of opioids in the management of chronic noncancer pain. Eur. J. Pain 2021, 25, 949–968. [Google Scholar] [CrossRef]
- Yang, J.; A Bauer, B.; Wahner-Roedler, D.L.; Chon, T.Y.; Xiao, L. The Modified WHO Analgesic Ladder: Is It Appropriate for Chronic Non-Cancer Pain? J. Pain Res. 2020, 13, 411–417. [Google Scholar] [CrossRef]
- EAPC Atlas of Palliative Care in Europe 2019. Available online: https://mariabouri.eu/sitecake-content/1d2d3ae4-7d60-11e9-9993-000000000000-1.pdf (accessed on 25 July 2023).
- Caraceni, A.; Hanks, G.; Kaasa, S.; Bennett, M.I.; Brunelli, C.; Cherny, N.; Dale, O.; De Conno, F.; Fallon, M.; Hanna, M.; et al. Use of opioid analgesics in the treatment of cancer pain: Evidence-based recommendations from the EAPC. Lancet Oncol. 2012, 13, e58–e68. [Google Scholar] [CrossRef]
- Ciałkowska-Rysz, A.; Dzierżanowski, T. Podstawowe zasady farmakoterapii bólu u chorych na nowotwory i inne przewlekłe, postępujące, zagrażające życiu choroby [Basic principles of pharmacotherapy of pain in patients with cancer and other chronic, progressive, life-threatening diseases]. Med. Paliatywna/Palliat. Med. 2014, 6, 1–6. [Google Scholar]
- Wordliczek, J.; Kotlińska-Lemieszek, A.; Leppert, W.; Woroń, J.; Dobrogowski, J.; Krajnik, M.; Przeklasa-Muszyńska, A.; Jassem, J.; Drobnik, J. Pharmacotherapy of pain in cancer patients—Recommendations of the Polish Association for the Study of Pain, Polish Society of Palliative Medicine, Polish Society of Oncology, Polish Society of Family Medicine, Polish Society of Anaesthesiology and Intensive Therapy and Association of Polish Surgeons. Ann. Surg. 2018, 90, 51–80. [Google Scholar] [CrossRef]
- Mills, S.E.; Nicolson, K.P.; Smith, B.H. Chronic pain: A review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 2019, 123, e273–e283. [Google Scholar] [CrossRef]
- Punwasi, R.; de Kleijn, L.; Rijkels-Otters, J.B.M.; Veen, M.; Chiarotto, A.; Koes, B. General practitioners’ attitudes towards opioids for non-cancer pain: A qualitative systematic review. BMJ Open 2022, 12, e054945. [Google Scholar] [CrossRef]
- Green, C.R.; Wheeler, J.R.; Marchant, B.; LaPorte, F.; Guerrero, E. Analysis of the physician variable in pain management. Pain Med. 2001, 2, 317–327. [Google Scholar] [CrossRef]
- Desveaux, L.; Saragosa, M.; Kithulegoda, N.; Ivers, N.M. Understanding the behavioural determinants of opioid prescribing among family physicians: A qualitative study. BMC Fam. Pract. 2019, 20, 59. [Google Scholar] [CrossRef]
- Tyson, D.M.; Chavez, M.N.; Lake, P.; Gutierrez, A.; Sherry, P.; Rigg, K.K.; Marshall, V.K.; Henderson, H.; di Ciccone, B.L.; Rajasekhara, S.; et al. Perceptions of prescription opioid medication within the context of cancer survivorship and the opioid epidemic. J. Cancer Surviv. 2021, 15, 585–596. [Google Scholar] [CrossRef]
- Paul, A.K.; Smith, C.M.; Rahmatullah, M.; Nissapatorn, V.; Wilairatana, P.; Spetea, M.; Gueven, N.; Dietis, N. Opioid Analgesia and Opioid-Induced Adverse Effects: A Review. Pharmaceuticals 2021, 14, 1091. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.-C.; Pallotti, P.; Dickinson, R.; Harley, C. ‘If you can’t see a dilemma in this situation you should probably regard it as a warning’: A metasynthesis and theoretical modelling of general practitioners’ opioid prescription experiences in primary care. Br. J. Pain 2019, 13, 159–176. [Google Scholar] [CrossRef] [PubMed]
- Makhlouf, S.M.; Pini, S.; Ahmed, S.; Bennett, M.I. Managing Pain in People with Cancer—A Systematic Review of the Attitudes and Knowledge of Professionals, Patients, Caregivers and Public. J. Cancer Educ. 2020, 35, 214–240. [Google Scholar] [CrossRef] [PubMed]
- Dzierżanowski, T.; Ciałkowska-Rysz, A. Accessibility of opioid analgesics and barriers to optimal chronic pain treatment in Poland in 2000–2015. Support. Care Cancer 2017, 25, 775–781. [Google Scholar] [CrossRef]
- Krebs, E.E.; Bergman, A.A.; Coffing, J.M.; Campbell, S.R.; Frankel, R.M.; Matthias, M.S. Barriers to guideline-concordant opioid management in primary care—A qualitative study. J. Pain 2014, 15, 1148–1155. [Google Scholar] [CrossRef]
- Grata-Borkowska, U.; Drobnik, J.; Bujnowska-Fedak, M.M.; Pokorna-Kałwak, D.; Odonicz-Czarnecki, G. Leczenie bólu w praktyce lekarza rodzinnego—Doniesienie wstępne [Pain management in family physician practice—Preliminary report]. Forum Med. Rodz. 2015, 9, 456–459. [Google Scholar]
- Hannes, K.; Leys, M.; Vermeire, E.; Aertgeerts, B.; Buntinx, F.; Depoorter, A.-M. Implementing evidence-based medicine in general practice: A focus group based study. BMC Fam. Pract. 2005, 6, 37. [Google Scholar] [CrossRef]
- Dzierżanowski, T.; Kozłowski, M. Opioid prescribing attitudes of palliative care physicians versus other specialists: A questionnaire-based survey. Postgrad. Med. J. 2022, 98, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Jamison, R.N.; Sheehan, B.K.A.; Scanlan, N.E.; Matthews, M.; Ross, E.L. Beliefs and attitudes about opioid prescribing and chronic pain management: Survey of primary care providers. J. Opioid Manag. 2014, 10, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Richards, G.C.; Mahtani, K.R.; Muthee, T.B.; DeVito, N.J.; Koshiaris, C.; Aronson, J.K.; Goldacre, B.; Heneghan, C.J. Factors associated with the prescribing of high-dose opioids in primary care: A systematic review and meta-analysis. BMC Med. 2020, 18, 68. [Google Scholar] [CrossRef]
- Klepstad, P.; Kaasa, S.; Borchgrevink, P.C. Starting Step III opioids for moderate to severe pain in cancer patients: Dose titration: A systematic review. Palliat. Med. 2011, 25, 424–430. [Google Scholar] [CrossRef]
- Windak, A. Primary Health Care in Poland—Diagnosis and Draft Changes; Report, Instytut Medycyny Wsi im; Witold Chodźka in Lublin: Lublin, Poland, 2019. [Google Scholar]
- Eysenbach, G. Improving the quality of web surveys: The checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Meyer, A.N.D.; Payne, V.L.; Meeks, D.W.; Rao, R.; Singh, H. Physicians’ Diagnostic Accuracy, Confidence, and Resource Requests: A Vignette Study. JAMA Intern. Med. 2013, 173, 1952–1958. [Google Scholar] [CrossRef]
- Kuhn, J.; van den Berg, P.; Mamede, S.; Zwaan, L.; Bindels, P.; van Gog, T. Improving medical residents’ self-assessment of their diagnostic accuracy: Does feedback help? Adv. Health Sci. Educ. 2022, 27, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Glowacki, D. Effective pain management and improvements in patients’ outcomes and satisfaction. Crit. Care Nurse 2015, 35, 33–41. [Google Scholar] [CrossRef]
- Carey, M.L.; Zucca, A.C.; Freund, M.A.; Bryant, J.; Herrmann, A.; Roberts, B.J. Systematic review of barriers and enablers to the delivery of palliative care by primary care practitioners. Palliat. Med. 2019, 33, 1131–1145. [Google Scholar] [CrossRef]
- Green, E.; Knight, S.; Gott, M.; Barclay, S.; White, P. Patients’ and carers’ perspectives of palliative care in general practice: A systematic review with narrative synthesis. Palliat. Med. 2018, 32, 838–850. [Google Scholar] [CrossRef]
- Thelen, M.; Brearley, S.G.; Walshe, C. A grounded theory of interdependence between specialist and generalist palliative care teams across healthcare settings. Palliat. Med. 2023, 37, 1474–1483. [Google Scholar] [CrossRef]
- Fan, W.; Yan, Z. Factors affecting response rates of the web survey: A systematic review. Comput. Hum. Behav. 2010, 26, 132–139. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).