Cross-Cultural Adaptation and Validation of the Arabic Version of the Physical Activity Scale for Individuals with Physical Disabilities in Saudi Arabia (PASIPD-AR)
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants in the Main Study
2.2. Physical Activity Scale for Individuals with Physical Disabilities (PASIPD)
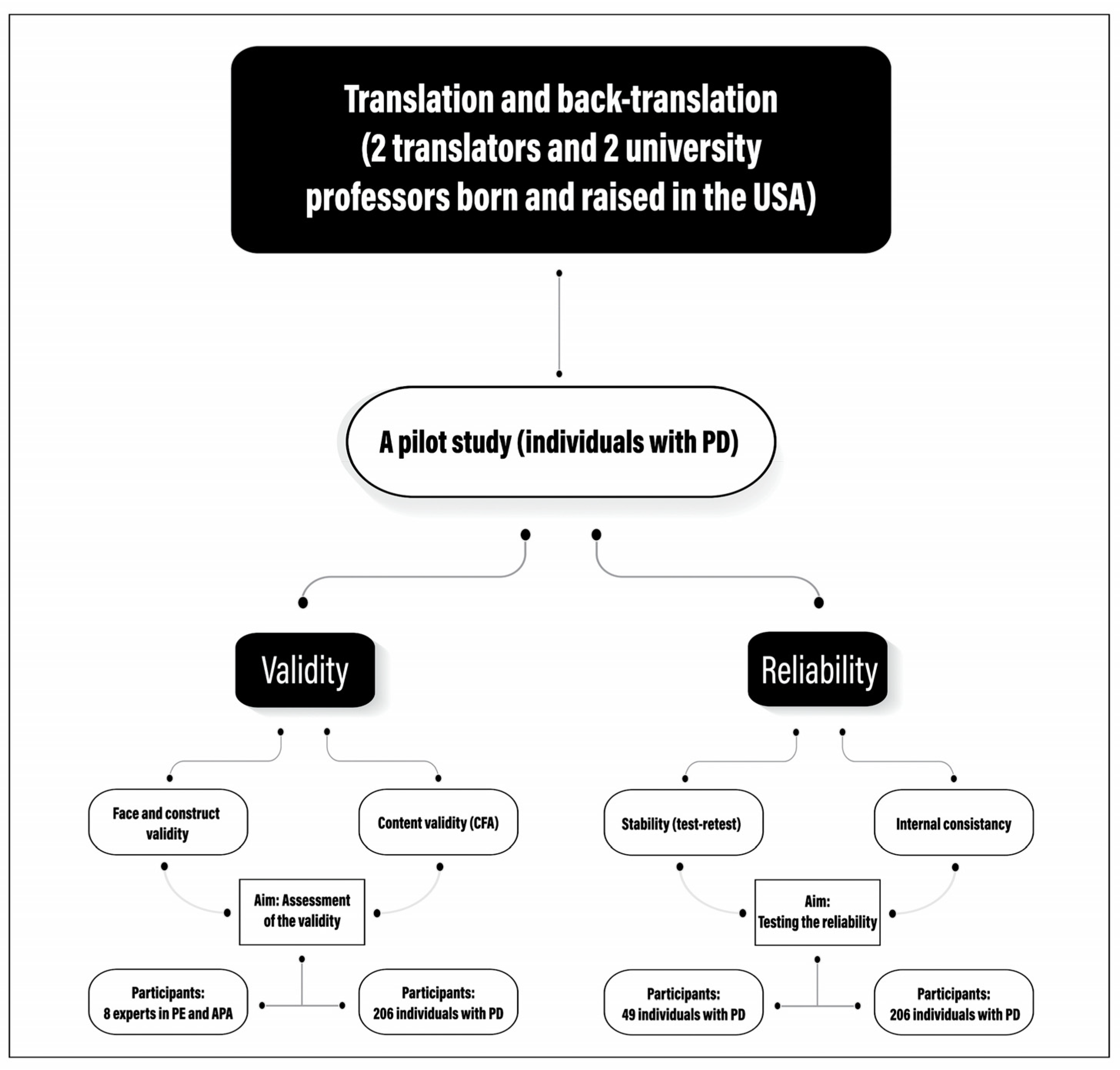
2.3. Translation and Cross-Cultural Adaptation of the PASIPD Scale
Pilot Test
2.4. Validity
2.5. Face Validity and Content Validity
2.6. Construct Validity
2.7. Reliability
3. Results
3.1. Participants Characteristics
3.2. Validation
Face Validity and Content Validity
3.3. Construct Validity
3.4. Reliability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Global Report on Health Equity for Persons with Disabilities (Geneva, 2022). 2022. Available online: https://www.who.int/publications/i/item/9789240063600 (accessed on 28 December 2023).
- World Health Organization (WHO). WHO Reveals Leading Causes of Death and Disability Worldwide: 2000–2019? 2020. Available online: https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000–2019 (accessed on 16 October 2023).
- Zahra, A.; Hassan, M.S.; Park, J.-H.; Hassan, S.-U.; Parveen, N. Role of Environmental Quality of Life in Physical Activity Status of Individuals with and without Physical Disabilities in Saudi Arabia. Int. J. Environ. Res. Public Health 2022, 19, 4228. [Google Scholar] [CrossRef] [PubMed]
- Okoro, C.A.; Hollis, N.D.; Cyrus, A.C.; Griffin-Blake, S. Prevalence of Disabilities and Health Care Access by Disability Status and Type Among Adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 882–887. [Google Scholar] [CrossRef] [PubMed]
- ADA National Network Information, Guidance, and Training on the Americans with Disabilities Act. Available online: https://adata.org/faq/what-definition-disability-under-ada (accessed on 15 October 2023).
- World Health Organization (WHO). Guidelines on Physical Activity and Sedentary Behaviour. 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 10 October 2023).
- US Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd ed.; US Department of Health and Human Services: Washington, DC, USA, 2018.
- Arbour-Nicitopoulos, K.P.; Grassmann, V.; Orr, K.; McPherson, A.C.; Faulkner, G.E.; Wright, F.V. A Scoping Review of Inclusive Out-of-School Time Physical Activity Programs for Children and Youth with Physical Disabilities. Adapt. Phys. Act. Q. 2018, 35, 111–138. [Google Scholar] [CrossRef] [PubMed]
- Orr, K.; Wright, F.V.; Grassmann, V.; McPherson, A.C.; Faulkner, G.E.; Arbour-Nicitopoulos, K.P. Children and youth with impairments in social skills and cognition in out-of-school time inclusive physical activity programs: A scoping review. Int. J. Dev. Disabil. 2019, 67, 79–93. [Google Scholar] [CrossRef]
- Anderson, L.; Heyne, L. Structuring recreation and youth programs to facilitate social inclusion. Impact 2011, 24, 34–35. [Google Scholar]
- Centers for Disease Control and Prevention. Physical Activity for People with Disability. 2022. Available online: https://www.cdc.gov/ncbddd/disabilityandhealth/features/physical-activity-for-all.html (accessed on 20 October 2023).
- Hollis, N.D.; Zhang, Q.C.; Cyrus, A.C.; Courtney-Long, E.; Watson, K.; Carroll, D.D. Physical activity types among US adults with mobility disability, Behavioral Risk Factor Surveillance System, 2017. Disabil. Health J. 2020, 13, 100888. [Google Scholar] [CrossRef] [PubMed]
- Healey, E.L.; Allen, K.D.; Bennell, K.; Bowden, J.L.; Quicke, J.G.; Smith, R. Self-Report Measures of Physical Activity. Arthritis Care Res. 2020, 72, 717–730. [Google Scholar] [CrossRef] [PubMed]
- Harvey, S.A. Observe Before You Leap: Why Observation Provides Critical Insights for Formative Research and Intervention Design That You’ll Never Get from Focus Groups, Interviews, or KAP Surveys. Glob. Health Sci. Pract. 2018, 6, 299–316. [Google Scholar] [CrossRef]
- Melanson, E.L.; Freedson, P.S.; Blair, S. Physical activity assessment: A review of methods. Crit. Rev. Food Sci. Nutr. 1996, 36, 385–396. [Google Scholar] [CrossRef]
- Jenn, N.C. Designing A Questionnaire. Malays. Fam. Physician Off. J. Acad. Fam. Physicians Malays. 2006, 1, 32–35. [Google Scholar]
- Doma, K.; Speyer, R.; Parsons, L.A.; Cordier, R. Comparison of psychometric properties between recall methods of interview-based physical activity questionnaires: A systematic review. BMC Med. Res. Methodol. 2019, 19, 43. [Google Scholar] [CrossRef] [PubMed]
- Washburn, R.A.; Zhu, W.; McAuley, E.; Frogley, M.; Figoni, S.F. The physical activity scale for individuals with physical disabilities: Development and evaluation. Arch. Phys. Med. Rehabil. 2002, 83, 193–200. [Google Scholar] [CrossRef]
- Van der Ploeg, H.P.; Streppel, K.R.; van der Beek, A.J.; van der Woude, L.H.; Vollenbroek-Hutten, M.; van Mechelen, W. The Physical Activity Scale for Individuals with Physical Disabilities: Test-Retest Reliability and Comparison with an Accelerometer. J. Phys. Act. Health 2007, 4, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Tanhoffer, R.A.; Tanhoffer, A.I.P.; Raymond, J.; Hills, A.P.; Davis, G.M. Comparison of methods to assess energy expenditure and physical activity in people with spinal cord injury. J. Spinal Cord Med. 2012, 35, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Lankhorst, K.; Oerbekke, M.; Berg-Emons, R.v.D.; Takken, T.; de Groot, J. Instruments Measuring Physical Activity in Individuals Who Use a Wheelchair: A Systematic Review of Measurement Properties. Arch. Phys. Med. Rehabil. 2020, 101, 535–552. [Google Scholar] [CrossRef] [PubMed]
- Al-Jadid, M.S. Disability in Saudi Arabia. Saudi Med. J. 2013, 34, 453–460. [Google Scholar] [PubMed]
- Safipour, J.; Tessma, M.K.; Higginbottom, G.; Emami, A. Measuring social alienation in adolescence: Translation and validation of the Jessor and Jessor Social Alienation Scale. Scand. J. Psychol. 2010, 51, 517–524. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef]
- Bell, M.L.; Kenward, M.G.; Fairclough, D.L.; Horton, N.J. Differential dropout and bias in randomised controlled trials: When it matters and when it may not. BMJ 2013, 346, e8668. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Jordan, C.; Hoefer, R.A. Reliability and validity in quantitative measurement. In Social Work Research Methods; Thyer, B.A., Ed.; SAGE: Thousand Oaks, CA, USA, 2001; pp. 53–68. [Google Scholar]
- Li, N.; Huang, J.; Feng, Y. Construction and confirmatory factor analysis of the core cognitive ability index system of ship C2 system operators. PLoS ONE 2020, 15, e0237339. [Google Scholar] [CrossRef] [PubMed]
- Garson, D. Neural Networks: An Introductory Guide for Social Scientists (New Technologies for Social Research Series); SAGE Publications Ltd.: London, UK, 1998. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 2nd ed.; The Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Marsh, H.W.; Hocevar, D. Application of confirmatory factor analysis to the study of self-concept: First- and higher order factor models and their invariance across groups. Psychol. Bull. 1985, 97, 562–582. [Google Scholar] [CrossRef]
- Chen, F.F. Sensitivity of Goodness of Fit Indexes to Lack of Measurement Invariance. Struct. Equ. Model. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- MacCallum, R.C.; Browne, M.W.; Sugawara, H.M. Power Analysis and Determination of Sample Size for Co-variance Structure Modeling. Psychol. Methods 1996, 1, 130–149. [Google Scholar] [CrossRef]
- Uedufy How to Interpret Model Fit Results in AMOS. 30 August 2023. Available online: https://uedufy.com/how-to-interpret-model-fit-results-in-amos/ (accessed on 18 October 2023).
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- West, R.F.; Meserve, R.J.; Stanovich, K.E. Cognitive sophistication does not attenuate the bias blind spot. J. Pers. Soc. Psychol. 2012, 103, 506–519. [Google Scholar] [CrossRef]
- Warrens, M.J. On Cronbach’s Alpha as the Mean of All Split-Half Reliabilities. In Quantitative Psychology Research; Millsap, R., Bolt, D., van der Ark, L.A., Wang, W.C., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2015; pp. 293–300. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [CrossRef]
- Blasco-Abadía, J.; Bellosta-López, P.; Palsson, T.; González, S.M.; García-Campayo, J.; Doménech-García, V. Spanish version of the pain beliefs questionnaire: Translation, cross-cultural adaptation, validation, and psychometric properties in a working population. Musculoskelet. Sci. Pract. 2023, 66, 102827. [Google Scholar] [CrossRef]
- Hajjar, S.E. Statistical Analysis: Internal-Consistency Reliability and Construct Validity. Int. J. Quant. Qual. Res. Methods 2018, 6, 46–57. [Google Scholar]
- Phelan, C.; Wren, J. Reliability Is the Degree to Which an Assessment Tool Produces Stable and Consistent Results. 2005. Available online: https://chfasoa.uni.edu/reliabilityandvalidity.htm (accessed on 20 October 2023).
- Faremi, Y.A. Reliability Coefficient of Multiple–Choice and Short Answer Objective Test Items in Basic Technology: Comparative Approach. J. Educ. Policy Entrep. Res. 2016, 3, 59–69. [Google Scholar]
- Guttman, L. A basis for analyzing test-retest reliability. Psychometrika 1945, 10, 255–282. [Google Scholar] [CrossRef]
- Revelle, W.; Zinbarg, R.E. Coefficients Alpha, Beta, Omega, and the glb: Comments on Sijtsma. Psychometrika 2009, 74, 145–154. [Google Scholar] [CrossRef]
- Jakson, P.H. A note on the relation between coefficient alpha and Guttman’s “split-half” lower bounds. Psychometrika 1979, 44, 251–252. [Google Scholar] [CrossRef]
- Yusoff, M.S.B. ABC of Content Validation and Content Validity Index Calculation. Educ. Med. J. 2019, 11, 49–54. [Google Scholar] [CrossRef]
- Lynn, M.R. Determination and Quantification of Content Validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef]
- Chen, F.; Bollen, K.A.; Paxton, P.; Curran, P.J.; Kirby, J.B. Improper Solutions in Structural Equation Models: Causes, consequences, and strategies. Sociol. Methods Res. 2001, 29, 468–508. [Google Scholar] [CrossRef]
- Rode, N. Translation of measurement instruments and their reliability: An example of job-related affective well-being scale. Metod. Zv. 2005, 2, 15–26. [Google Scholar] [CrossRef]
- Spector, P.E. Summated Rating Scale Construction: Quantitative Applications in the Social Sciences Series; SAGE: Thousand Oaks, CA, USA, 1992. [Google Scholar]
- Chau, P.Y. On the use of construct reliability in MIS research: A meta-analysis. Inf. Manag. 1999, 35, 217–227. [Google Scholar] [CrossRef]
- Courten, M.P. Developing a simple global physical activity questionnaire for population studies. Australas. Epidemiol. 2002, 9, 6–9. [Google Scholar]
- Booth, M. Assessment of Physical Activity: An International Perspective. Res. Q. Exerc. Sport 2000, 71, 114–120. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Ginis, K.A.M.; Latimer, A.E.; Hicks, A.L.; Craven, B.C. Development and Evaluation of an Activity Measure for People with Spinal Cord Injury. Med. Sci. Sports Exerc. 2005, 37, 1099–1111. [Google Scholar] [CrossRef] [PubMed]
- Latimer, A.E.; Ginis, K.A.; Craven, B.C.; Hicks, A.L. The physical activity recall assessment for people with spinal cord injury: Validity. Med. Sci. Sports Exerc. 2006, 38, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.A.; Miller, T.; O’Connell, S.; Jelinek, C.; Collins, E.G. Physical Activity Inventory for Patients with Spinal Cord Injury. SCI Nurs. 2008, 25, 20–28. [Google Scholar] [PubMed]
- Rimmer, J.H.; Riley, B.B.; Rubin, S.S. A new measure for assessing the physical activity behaviors of persons with disabilities and chronic health conditions: The Physical Activity and Disability Survey. Am. J. Health Promot. 2001, 16, 34–45. [Google Scholar] [CrossRef]
- Burhaein, E.; Tarigan, B.; Budiana, D.; Hendrayana, Y.; Phytanza DT, P.; Lourenço, C.; Festiawan, R. Dimen-sions in the learning implementation and strategies of adapted physical education for children with special needs during the covid-19 pandemic: A literature review & grounded theory. Sport Sci. 2021, 15, 189–201. [Google Scholar]
- Ulaş, K.; Topuz, S.; Horasan, G. The validity and reliability of the Turkish version of the Physical Activity Scale for Individuals with Physical Disabilities (PASIPD). Turk. J. Med. Sci. 2019, 49, 1620–1625. [Google Scholar] [CrossRef]
- Rezaee, F.; Jafari, M. Dynamic capability in an under-researched cultural environment. Manag. Sci. Lett. 2016, 6, 177–192. [Google Scholar] [CrossRef]
- Martínez-Costa, M.; Jiménez-Jiménez, D. The Effectiveness of TQM the key role of organizational learning in small businesses. Int. Small Bus. J. 2009, 27, 98–125. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Yi, Y. On the evaluation of structural equation models. J. Acad. Mark. Sci. 1988, 16, 74–94. [Google Scholar] [CrossRef]
- Browne, M.W.; Cudeck, R. Alternative ways of assessing model fit. Sociol. Methods Res. 1992, 21, 230–258. [Google Scholar] [CrossRef]
- Cooperman, A.W.; Waller, N.G. Heywood you go away! Examining causes, effects, and treatments for Heywood cases in exploratory factor analysis. Psychol. Methods 2022, 27, 156–176. [Google Scholar] [CrossRef]
| N (%) | Age | Weight (kg) | Height (cm) | BMI (kg/m2) | PASIPD-AR | |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 134 (65.0%) | 39.66 ± 12.22 | 73.11 ± 24.00 | 159.49 ± 23.66 | 33.90 ± 35.38 | 8.48 ± 9.42 |
| Female | 72 (35.0%) | 39.38 ± 12.15 | 70.32 ± 24.93 | 150.11 ± 22.13 | 36.00 ± 34.76 | 8.87 ± 9.25 |
| Marital status | ||||||
| Single | 80 (38.8%) | 30.21 ± 9.71 | 59.90 ± 17.41 | 155.45 ± 21.25 | 27.07 ± 20.18 | 7.24 ± 7.82 |
| Married | 101(49%) | 45.05 ± 9.19 | 78.54 ± 22.63 | 157.98 ± 23.50 | 38.00 ± 41.77 | 9.17 ± 10.18 |
| Divorced | 16 (7.8%) | 46.00 ± 10.88 | 82.25 ± 36.71 | 146.75 ± 36.61 | 50.72 ± 48.56 | 12.31 ± 10.90 |
| Widowed | 4 (1.9%) | 56.75 ± 8.96 | 76.25 ± 9.46 | 157.50 ± 10.21 | 31.07 ± 5.71 | 14.52 ± 7.17 |
| Do not want to respond | 5 (2.4%) | 44.00 ± 10.51 | 102.80 ± 27.10 | 162.00 ± 3.81 | 39.08 ± 9.49 | 2.98 ± 4.23 |
| Education level | ||||||
| Primary school degree | 44 (21.4%) | 44.89 ± 12.89 | 68.27 ± 22.29 | 150.89 ± 26.88 | 35.23 ± 29.99 | 8.27 ± 9.04 |
| Middle school degree | 23 (11.2%) | 44.87 ± 11.53 | 81.57 ± 31.83 | 153.17 ± 33.72 | 51.48 ± 70.25 | 6.89 ± 7.38 |
| High school degree | 76 (36.9%) | 36.71 ± 11.68 | 71.12 ± 23.49 | 159.80 ± 18.27 | 30.60 ± 27.74 | 9.08 ± 9.39 |
| University degree | 57 (27.7%) | 37.67 ± 11.16 | 72.68 ± 24.17 | 157.82 ± 18.45 | 30.46 ± 13.87 | 9.06 ± 10.06 |
| Postgraduate degree | 6 (2.9%) | 34.33 ± 6.09 | 72.00 ± 10.75 | 146.17 ± 44.67 | 56.37 ± 70.92 | 7.69 ± 12.65 |
| Self-rated health | ||||||
| Poor | 26 (12.6%) | 44.65 ± 12.88 | 75.73 ± 29.38 | 156.23 ± 25.28 | 33.65 ± 21.26 | 6.57 ± 7.42 |
| Good | 139 (67.5%) | 39.50 ± 11.93 | 71.14 ± 22.90 | 156.23 ± 23.97 | 34.91 ± 38.60 | 8.68 ± 9.55 |
| Excellent | 41 (19.9%) | 36.56 ± 11.71 | 73.22 ± 25.79 | 156.15 ± 21.24 | 34.33 ± 29.82 | 9.69 ± 9.72 |
| Self-rated physical activity | ||||||
| Not active at all | 61 (29.6%) | 42.38 ± 13.22 | 77.33 ± 31.97 | 154.79 ± 25.41 | 37.63 ± 40.65 | 8.87 ± 8.96 |
| Moderately active | 128 (62.1%) | 38.54 ± 11.50 | 70.67 ± 20.45 | 157.13 ± 21.45 | 32.89 ± 30.91 | 8.45 ± 9.51 |
| Active/extremely active | 17 (8.3%) | 37.18 ± 12.08 | 64.53 ± 15.37 | 154.41 ± 31.51 | 36.97 ± 43.98 | 8.95 ± 9.95 |
| Use of mobility assistive device | ||||||
| Independent | 42 (20.4%) | 36.88 ± 11.25 | 71.10 ± 21.98 | 155.52 ± 24.91 | 35.19 ± 33.02 | 10.31 ± 9.53 |
| Wheelchair | 120 (58.3%) | 39.96 ± 12.84 | 71.86 ± 26.20 | 155.12 ± 24.62 | 34.51 ± 32.00 | 8.63 ± 9.67 |
| Crutches | 24 (11.7%) | 41.38 ± 12.58 | 70.17 ± 19.54 | 154.83 ± 23.66 | 39.39 ± 60.21 | 4.82 ± 4.24 |
| Walking sticks | 20 (9.7%) | 40.65 ± 8.77 | 78.35 ± 22.82 | 165.90 ± 6.60 | 28.50 ± 8.22 | 9.54 ± 10.63 |
| Correlation with Total Score | Factor Loading | ||||
|---|---|---|---|---|---|
| Factor 1: Home Repair Lawn and Garden Work | Factor 2: Housework | Factor 3: Sports and Recreation | Factor 4: Occupation | ||
| Walk and wheel push outside home (not for exercise) | 0.646 ** | - | - | - | 0.750 |
| Light sport and recreation | 0.582 ** | - | - | 0.603 | - |
| Moderate sport and recreation | 0.541 ** | - | - | 0.628 | - |
| Strenuous sport and recreation | 0.418 ** | - | - | 0.720 | - |
| Exercise to increase muscular strength | 0.468 ** | - | - | 0.618 | - |
| Light housework | 0.544 ** | - | 0.889 | - | - |
| Heavy housework | 0.614 ** | - | 0.649 | - | - |
| Home repair | 0.451 ** | 0.600 | - | - | - |
| Lawn work and yard care | 0.482 ** | 0.822 | - | - | - |
| Moderate sports and recreational activities | 0.401 ** | 0.778 | - | - | - |
| Outdoor garden work | 0.481 ** | - | 0.583 | - | - |
| Paid employment/volunteering | 0.612 ** | - | - | - | 0.617 |
| Eigenvalues | - | 2.442 | 1.711 | 1.956 | 1.285 |
| % Variance | - | 20.353 | 14.261 | 16.301 | 10.705 |
| Cumulative % variance | - | 20.353 | 34.614 | 50.915 | 61.621 |
| PASIPD-AR Items, Subscales, and Total | Four-Factors Model | ||||
|---|---|---|---|---|---|
| Mean ± SD (MET h/d) | Cronbach’s Alpha | Beta Weights | VIF | ||
| Item-Factor | Factor- PASIPD-AR | ||||
| Factor 1: Home repair, lawn, and garden work | 1.362 ± 4.86 | 0.580 | 0.728 | ||
| Home repairs | 0.484 ± 1.634 | 0.73 | 1.365 | ||
| Lawn work or yard care | 0.472 ± 1.965 | 0.62 | 2.272 | ||
| Outdoor gardening | 0.406 ± 1.820 | 0.70 | 2.282 | ||
| Factor 2: Housework | 2.612 ± 4.918 | 0.581 | 0.611 | ||
| Light housework | 0.640 ± 1.343 | 0.73 | 1.910 | ||
| Heavy housework or chores | 0.906 ± 2.639 | 1.81 | 2.269 | ||
| Caring for another person | 1.065 ± 1.966 | 0.53 | 1.236 | ||
| Factor 3: Light to vigorous sport and recreational activity | 3.99 ± 9.7 | 0.619 | 0.883 | ||
| Strenuous sports and recreational activities | 1.111 ± 3.757 | 0.73 | 1.409 | ||
| Exercise to increase muscle strength and endurance | 1.405 ± 3.671 | 0.67 | 1.539 | ||
| Light sports or recreational activities | 0.617 ± 1.634 | 0.70 | 1.485 | ||
| Moderate sports and recreational activities | 0.859 ± 2.537 | 0.49 | 1.310 | ||
| Factor 4: Occupational and transportation activity | 5.03 ± 7.227 | 0.42 | 0.730 | ||
| Walk, wheel, push outside home. | 2.754 ± 3.502 | 0.73 | 1.272 | ||
| Paid employment/volunteering | 2.277 ± 5.257 | 1.93 | 1.371 | ||
| PASIPD-AR | 12.996 ± 20.424 | 0.694 | |||
| Reliability | ||||||
|---|---|---|---|---|---|---|
| Test–Retest Correlation | Internal Consistency Cronbach’s Alpha | Split-Half | ||||
| Walk and wheel push outside home (not for exercise) | 0.969 ** | 0.726 | Cronbach’s Alpha | Part 1 | Value | 0.684 |
| N of Items | 6 a | |||||
| Light sport and recreation | 0.956 ** | 0.657 | Part 2 | Value | 0.444 | |
| Moderate sport and recreation | 0.981 ** | 0.664 | N of Items | 6 b | ||
| Strenuous sport and recreation | 0.944 ** | 0.681 | Total N of Items | 12 | ||
| Exercise to increase muscular strength | 0.977 ** | 0.674 | Correlation Between Forms | 0.55 | ||
| Light housework | 0.902 ** | 0.667 | Spearman–Brown Coefficient | Equal Length | 0.709 | |
| Heavy house work | 0.701 ** | 0.653 | Unequal Length | 0.709 | ||
| Home repair | 0.920 ** | 0.676 | Guttman Split-Half Coefficient | 0.693 | ||
| Lawn work and yard care | 0.968 ** | 0.681 | Lambda | 1 | 0.636 | |
| 2 | 0.713 | |||||
| Outdoor garden work | 0.835 ** | 0.689 | 3 | 0.694 | ||
| 4 | 0.693 | |||||
| Caring for another person | 0.740 ** | 0.683 | 5 | 0.711 | ||
| 6 | 0.731 | |||||
| Paid employment/volunteering | 0.969 ** | 0.659 | a. items 3–8. b. items 2, 9–13. | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhumaid, M.M.; Said, M.A.; Adnan, Y.; Khoo, S. Cross-Cultural Adaptation and Validation of the Arabic Version of the Physical Activity Scale for Individuals with Physical Disabilities in Saudi Arabia (PASIPD-AR). Healthcare 2024, 12, 179. https://doi.org/10.3390/healthcare12020179
Alhumaid MM, Said MA, Adnan Y, Khoo S. Cross-Cultural Adaptation and Validation of the Arabic Version of the Physical Activity Scale for Individuals with Physical Disabilities in Saudi Arabia (PASIPD-AR). Healthcare. 2024; 12(2):179. https://doi.org/10.3390/healthcare12020179
Chicago/Turabian StyleAlhumaid, Majed M., Mohamed A. Said, Yuhanis Adnan, and Selina Khoo. 2024. "Cross-Cultural Adaptation and Validation of the Arabic Version of the Physical Activity Scale for Individuals with Physical Disabilities in Saudi Arabia (PASIPD-AR)" Healthcare 12, no. 2: 179. https://doi.org/10.3390/healthcare12020179
APA StyleAlhumaid, M. M., Said, M. A., Adnan, Y., & Khoo, S. (2024). Cross-Cultural Adaptation and Validation of the Arabic Version of the Physical Activity Scale for Individuals with Physical Disabilities in Saudi Arabia (PASIPD-AR). Healthcare, 12(2), 179. https://doi.org/10.3390/healthcare12020179







