Abstract
Background: Compassion fatigue is a significant issue considering its consequences including negative feelings, impaired cognition, and increased risk of long-term morbidities. We aimed to assess current evidence on the effects of interventions for compassion fatigue in healthcare providers (HCP). Methods: We used the Cochrane methodology for Systematic Reviews and Meta-Analyses (PRISMA) for conducting and reporting this review. Results: Fifteen RCTs (n = 1740) were included. The sample size of individual studies was small ranging from 23 to 605. There was significant heterogeneity in participant, intervention, control, and outcome characteristics. The tools for assessing intervention effects on compassion fatigue included ProQOL, compassion fatigue scale, and nurses compassion fatigue inventory. Thirteen out of the fifteen included RCTs had overall high risk of bias (ROB). Meta-analysis could not be performed given the significant heterogeneity. Conclusions: Current evidence on interventions for reducing compassion fatigue in HCPs is inadequate. Given the benefits reported in some of the included studies, well-designed and adequately powered RCTs are urgently needed.
1. Introduction
Empathy and compassion are at the core of the medical field, the business of providing care and comfort and, if possible, cure for patients. Empathy, the driver of prosocial behaviour, is the ability to understand and truly share the feelings of others [1,2,3]. Empathy is considered as the first step to more humane care [4] and critical for effective communication and healthcare [5,6,7,8,9,10].
Driven by empathy, compassion is the deep feeling that arises after becoming distressed by another person’s suffering, accompanied by a strong desire to help and improve his/her wellbeing [11,12,13,14]. Compassion leads to acts of kindness, taking empathy a step ahead [15,16,17,18].
Carrying the emotional burden of the suffering of other people over a long period can hurt the care provider due to the acute or cumulative effects of secondary stress [19,20]. Researchers hence consider empathy as a double-edged sword or the ‘cost of caring’ and emphasise the importance of awareness of this risk in healthcare providers [21,22,23,24,25,26]. The broad definition of compassion fatigue [27] is focused on secondary traumatic stress (STS), the emotional duress experienced by people in close contact with a trauma survivor [28,29]. Aspects of burnout were later added to this definition to include energy depletion as a well-known feature of compassion fatigue [29,30,31,32,33]. The secondary stress in compassion fatigue is similar to that in STS. However, compassion fatigue is characterised by reduced empathic capacity after repeated exposure to traumatic situations experienced by others [34,35]. Researchers suggest that STS occurs first and gives rise to compassion fatigue [36]. Compassion fatigue is a form of vicarious trauma with symptoms like that of post-traumatic stress disorder (PTSD) but without the inner change in worldview [37,38].
The significance of compassion fatigue cannot be overemphasised given its high prevalence [39,40,41,42]. Moreover, it has serious consequences including negative feelings, impaired cognition, and increased risk of long-term morbidities such as cardiovascular disease, and psychiatric illness [43,44,45].
Current evidence includes only a few systematic reviews in the field of compassion fatigue [46,47,48,49,50,51,52]. These reviews have significant heterogeneity in the participant (e.g., physicians, nurses, radiographers), faculty (e.g., oncology, emergency department), and location (e.g., rural, low-middle income nations) characteristics, and the evaluated aspects of compassion fatigue (e.g., prevalence, risk factors, interventions). Furthermore, some of these reviews focus on isolated components of compassion fatigue [48,52]. Interpreting and applying evidence from such heterogenous studies is hence difficult [53]. The recent systematic review by Chen et al. [54] has focused mainly on the effects of psychological interventions on empathy (not compassion) fatigue only in nurses. Similarly, the systematic review by Xie et al. [55] has assessed the effects of psychological interventions on compassion fatigue only in nurses.
Given the significance of underlining issues, we aimed to review the current evidence on the effect of various strategies for reducing compassion fatigue in healthcare providers. Our specific objective was to conduct a comprehensive and robust systematic review focused exclusively on randomised controlled trials (RCTs) of interventions for compassion fatigue in healthcare providers. Our findings will help in guiding research and clinical practice in the field.
2. Material and Methods
We followed the Cochrane methodology [56] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [57] statement for this systematic review. The protocol was approved by the university supervisor for this project [58].
2.1. Literature Search
PubMed, EMBASE, CINAHL, Emcare, and Cochrane library were searched from inception until December 2022. Grey literature was searched through Mednar (https://mednar.com (accessed on 10 January 2023)). Reviewers DP and SP independently searched the literature. The reference lists of the relevant studies were hand-searched to identify additional articles. No language restrictions were applied. The literature search focussed separately on systematic reviews and clinical/randomised trials assessing any intervention for compassion fatigue as follows:
- (1)
- The above-mentioned databases were searched for systematic reviews on interventions for compassion fatigue. PubMed were searched using the search terms (“compassion fatigue”[MeSH Terms] OR (“compassion”[All Fields] AND “fatigue”[All Fields]) OR “compassion fatigue”[All Fields]) AND (meta-analysis [Filter] OR systematic review [Filter]). Similar terms were used for other databases.
- (2)
- All databases were searched again for individual RCTs on interventions for compassion fatigue. PubMed was searched using the following broad key words: ((compassion fatigue) OR (compassion satisfaction)) OR (empathy fatigue) Filters: Clinical Trial, Randomized Controlled Trial. That automatic mapping system of PubMed expanded it to cover all the following terms: (“compassion fatigue”[MeSH Terms] OR (“compassion”[All Fields] AND “fatigue”[All Fields]) OR “compassion fatigue”[All Fields] OR ((“empathy”[MeSH Terms] OR “empathy”[All Fields] OR “compassion”[All Fields]) AND (“personal satisfaction”[MeSH Terms] OR (“personal”[All Fields] AND “satisfaction”[All Fields]) OR “personal satisfaction”[All Fields] OR “satisfaction”[All Fields] OR “satisfactions”[All Fields] OR “satisfaction s”[All Fields])) OR ((“empathy”[MeSH Terms] OR “empathy”[All Fields]) AND (“fatiguability”[All Fields] OR “fatiguable”[All Fields] OR “fatigue”[MeSH Terms] OR “fatigue”[All Fields] OR “fatigued”[All Fields] OR “fatigues”[All Fields] OR “fatiguing”[All Fields] OR “fatigueability”[All Fields]))) AND (clinicaltrial[Filter] OR randomizedcontrolledtrial[Filter]). Similar terms were used for other databases.
2.2. Inclusion Criteria
RCTs and quasi-RCTs assessing interventions for compassion fatigue were eligible for inclusion. Studies not assessing interventions for compassion fatigue or dealing with STS, burnout, and vicarious trauma were excluded. We excluded reviews, editorials, case reports, letters and commentaries but read them to identify potential studies.
The primary outcome was the effect of the intervention on compassion fatigue (Mean pre-post difference in scores) measured by a validated tool such as the Professional Quality of Life (ProQOL) scale [59,60,61,62]. Secondary outcomes included effects of the intervention on individual components of compassion fatigue, including burnout and STS, and other outcomes reported in the individual studies.
2.3. Assessing the Risk of Bias (ROB)
The Cochrane ROB tool (RoB 2.0) was used to assess the ROB based on the following criteria [61]: 1. Was the allocation sequence adequately generated? 2. Was allocation adequately concealed? 3. Was blinding of participants, personnel, and outcome assessors adequate? 4. Were incomplete outcome data adequately addressed? 5. Are reports of the study free of selective outcome reporting? 6. Was the study apparently free of other problems? Overall, this tool assesses the randomisation process, deviations from intended interventions, missing outcomes, the method for measuring the outcomes and selective reporting [63].
2.4. Data Extraction
Two reviewers (SP and DP) independently extracted the data using a prespecified data collection form. All reviewers verified the information about study design and outcomes independently. Disagreements were resolved through joint discussions if required. If required, we planned to contact the authors of included studies for incomplete data or clarifications. Studies were excluded after two failed attempts to contact the authors.
2.5. Data Synthesis
We planned to conduct the meta-analysis using the Review manager V.5.4 (Cochrane collaboration, Nordic Cochrane Centre, Copenhagen, Denmark). We selected the random-effects model for meta-analysis given the significant heterogeneity [64]. We chose relative risk (RR) size and the mean difference (MD) to express the effects for dichotomous and continuous outcomes, respectively.
2.6. Assessment of Heterogeneity, Publication Bias and Certainty of the Evidence (CoE)
We planned to assess statistical heterogeneity with the χ2 test, I2 statistic and by visual inspection of the forest plot (overlap of CIs) [65]. As recommended, an I2 value of >50% indicates substantial heterogeneity [65]. When pooling was not possible, we planned to present the non-pooled data in tabular form. We planned to check publication bias by a funnel plot if more than 10 RCTs were available for meta-analysis. We also planned to assess publication bias objectively by Egger’s test [66,67]. We planned to report the certainty of evidence using the GRADE framework [68].
2.7. Exploring Heterogeneity
Heterogeneity was explored by considering the variations in participant, interventions, comparator, and outcomes in included studies. We planned to explore differences in the design (e.g., randomised vs. quasi-randomised) and settings (ICU vs. non-ICU, urban vs. rural-remote) of the included studies.
3. Results
The literature search retrieved 865 potentially relevant citations. After carefully reviewing the abstracts, 260 duplicate studies were excluded. A total of 570 studies were excluded after reading titles and abstracts. Twenty articles were excluded after reading 35 full texts. Finally, 15 RCTs were included in the review [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83]. The flow diagram of the study selection process is shown in Figure 1.
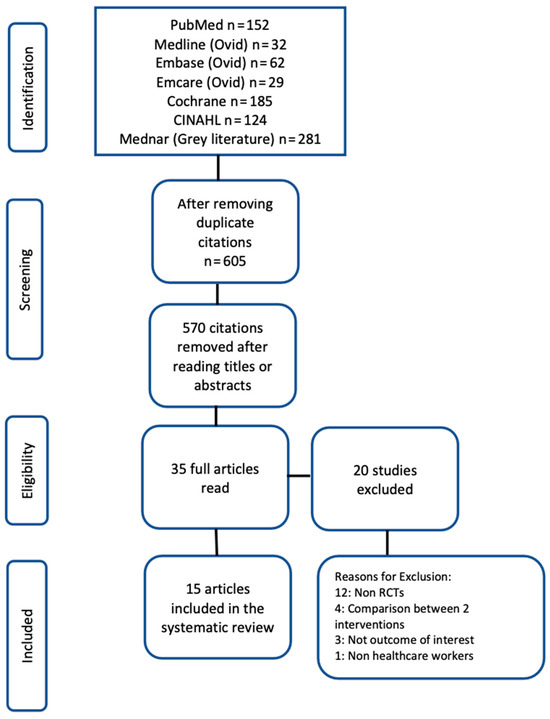
Figure 1.
PRISMA flow chart for study selection.
The characteristics of the 15 included studies are described in Table 1. There was significant heterogeneity in the participants, interventions, control, and outcome characteristics, and the settings, and timing of assessing the effect of the intervention in these studies. The sample size of individual studies was small, ranging from 23 to 605 participants [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83]. The total sample size was 1740 (mean: 116). Nine out of fifteen included studies showed reduction in either compassion fatigue or its components after intervention [70,71,73,74,75,77,79,81,83]. Six studies did not show any effect of intervention on compassion fatigue or its components [69,72,76,78,80,82]. The design of a quasi-experimental study with ‘nurses from a similar unit’ as control group was unclear [82].

Table 1.
Characteristics of included studies.
Majority of the included studies (11/15) recruited nurses working in different settings ranging from intensive care unit, and emergency department to elderly care centres, and trauma centres. Two studies recruited mental health workers, behavioural health clinicians, and another recruited a proportion (39.5% of 253) of participants as psychologists, psychotherapists, coaches, and counsellors. The studies were conducted in various nations including Iran (n = 3), Turkey (n = 3), Slovakia, Israel, Spain, Korea (n = 1 each), and USA (n = 5).
The interventions ranged from motivational messages, acupressure, and guided imagery to inhalation of patchouli oil, chromotherapy, and Emotion-Focused Training for Health Professionals (EFT-HP). The various tools for assessing intervention effects included the ProQOL, compassion fatigue scale, nurses compassion fatigue inventory, Disaster-Helper Self-Efficacy Scale (DHSES), Rosenberg self-esteem scale (RSE), Self-rated Hope Scale, Mastery scale, and the Pittsburgh Sleep Quality Index (PSQI).
Four studies had ‘wait list’ controls [71,72,79,81]. Other studies did not offer the intervention to participants in the control group.
Trial registration was reported in 9/15 included RCTs [71,73,74,75,76,80,81,82,83]. An approach to sample size and power estimation was reported in 6/15 included studies [69,70,72,77,78,80]. Some of these trials did not report the rationale for sample size estimation adequately [72,78]. The distinction between primary and secondary outcomes was unclear in majority of the included RCTs. Five studies were reported as a pilot [73,74,80,81,82]. The tools used in the included studies for assessing the effect of interventions specifically on compassion fatigue included ProQOL [84,85,86,87,88,89], compassion fatigue scale [70], and nurses compassion fatigue inventory [69,90].
Our literature search revealed two recently published systematic reviews [54,55]. Chen et al. included 7 RCTs (Total 513 nurses) and assessed the effects of psychological intervention on empathy fatigue in nurses. Four of the seven RCTs included in Chen review were identified in our literature search and remaining three were judged ineligible being non-RCTs [91,92,93]. Xie Wanging et al. that assessed the effects of psychological interventions on compassion fatigue among nursing staff was excluded as the full paper was not available despite contacting the authors [55]. The translated abstract in English was unreliable (e.g., “Thirteen RCTs involving 13 nursing staff were included”).
3.1. Approach to Synthesis
Given the significant heterogeneity in participants, interventions (type and duration), controls, and outcomes as well as the settings, tools for assessments, and timing of assessments post-intervention in the included RCTs pooling of data was considered inappropriate. Hence, a narrative approach to synthesis was undertaken. A funnel plot to assess the probability of publication bias was not considered.
3.2. Risk of Bias Assessment (Figure 2)
Thirteen out of the fifteen (87%) included studies had overall high ROB. The two domains with high ROB involved the randomization process (12/15 (80%) included studies) and in the measurement of outcomes (13/15 (87%) of the 15 included studies). The high ROB in the measurement of outcomes domain is because of the nature of intervention and reporting of outcomes by the participants themselves. Figure 2 provides the results of the ROB assessment.
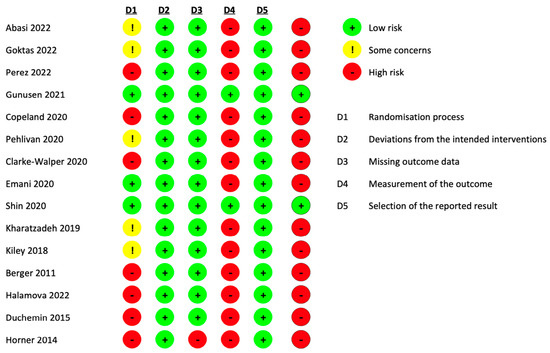
Figure 2.
Risk of bias assessment of the included studies [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83].
4. Discussion
Our systematic review revealed 15 RCTs (n = 1740) assessing various interventions for reducing compassion fatigue in healthcare providers from different sectors. Most studies used the ProQOL scale for the purpose. Significant heterogeneity in characteristics of the settings, participants, interventions, comparator groups, outcomes, and timing (and in few studies, the tool) for assessing the effects of the intervention meant conducting meta-analysis was inappropriate. All included studies had small sample size and high risk of bias. Deriving a robust conclusion from such inadequate and low-quality data was hence difficult. Our findings indicate the urgent need for well-designed and adequately powered definitive RCTs of interventions to reduce the risk of compassion fatigue in healthcare providers.
The significance of the methodology and results of two systematic reviews [46,54] need to be discussed in the context of our systematic review. Cocker et al. [46] reported a systematic review of studies assessing psychological interventions for reducing compassion fatigue in healthcare providers in various settings. The studies used validated measures such as Pro-QoL, Maslach Burnout Scale [94], or the Resilience Scale [95]. Of the total 229 studies identified, only 13 studies were included in the review (n = 671, range: 7 to 153). There was significant heterogeneity in participant, setting, and intervention characteristics, the period of follow up, and the study design including the type of control group. Participants were not truly representative of the target population as their selection was based on convenience rather than random sampling. Given the small total sample size, and the fact that 11 of the 13 included studies were non-RCTs it is difficult to derive clear and valid conclusions from this systematic review. The results of the included two small RCTs are also not helpful in this context [46]. The ideal intervention for compassion fatigue would be one that reduces burnout and STS (the negative aspect) and increases compassion satisfaction, the positive aspect of professional quality of life. One of the thirteen included studies that showed such results involved a two-step intervention amongst emergency nurses [96].
Chen et al. reported a systematic review assessing the effects of psychological interventions on empathy (not compassion) fatigue in nurses [54]. Meta-analysis of data from 7 included RCTs (n = 513 nurses) showed that empathy fatigue (SMD = −0.22, 95% CI: −0.42~−0.02, p = 0.03) and burnout (SMD = −0.37, 95% CI: −0.56~−0.19, p < 0.001) scores were significantly lower in the intervention vs. control group. The empathy satisfaction score was significantly higher in intervention vs. control group (SMD = 0.45, 95% CI: 0.27–0.63, p < 0.001). The effects of the intervention were significantly different in different settings including ICU, paediatric, and other departments (p = 0.0007). Both mindfulness (SMD = 0.50, 95% CI: 0.24–0.77, p = 0.0002) and other interventions (SMD = 0.41, 95% CI: 0.16–0.65, p = 0.001) had a significant effect on empathy satisfaction between the intervention vs. control group [54]. We believe that pooling data from heterogeneous interventions under a common label as ‘psychological’ interventions is debatable.
Overall, the data on the range of interventions from studies included in our systematic review and those by Cocker et al. [46], Chen et al. [54], and the findings of some of the studies discussed here [97,98,99] should be useful in selecting intervention for assessing in future studies.
Selecting the design of future studies in this field is a critical issue. RCTs are considered as the gold standard for clinical research to assess the effects (benefits and risks) of an intervention [100]. The strength of the RCT design lies in its ability to control for not only the known, but also the unknown confounders. No other study design can achieve this goal [101,102]. However, well-designed large adequately powered RCTs are not easy to conduct considering the difficulties related to their feasibility, acceptability, and need for resources, and expertise. A systematic review and meta-analysis of RCTs with comparable characteristics of participants, interventions, comparator, and outcomes provides a robust way to synthesise the evidence with more power and precision when the available RCTs are small and have conflicting results [103,104].
Randomisation at individual participant level will be difficult in RCTs of interventions to reduce compassion fatigue and/or improve compassion satisfaction, especially in small organisations. Contamination of the control group participants is inevitable if they work in the same section of an organisation as those assigned to the intervention group. This is particularly a possibility given the nature of psychological interventions and the fact that humans influence others consciously or subconsciously. Cluster RCT design is hence more appropriate for such studies [105,106,107]. The limitations of cluster RCTs include the need for biostatisticians with expertise (e.g., power, precision, number and size of the clusters, imbalance between clusters, intra-cluster correlation coefficient) [108,109,110,111,112,113,114,115]. Furthermore, the power and precision of results generated by a cluster-RCT are lower compared to those from a conventional RCT. The stepped wedge design is an alternative for rigorous evaluation of organisational interventions such as those for managing compassion fatigue [116,117]. This unique design provides an option where all trial participants receive the intervention but the order in which the intervention is received is randomised.
As for interventions, considering their simplicity, acceptability, ease of application, and logistics of implementation, as well as resources and socioeconomic and cultural differences is important in designing trials in this field. The ProQOL scale is perhaps the most appropriate tool for assessing effects of interventions for compassion fatigue considering it is culturally adapted and validated in several countries and has high reliability and validity [118,119]. Biological markers such as salivary amylase will optimise the validity of the results RCTs [81]. Salivary amylase is a marker of stress-induced activation of the autonomic nervous system. Its secretion is controlled by sympathetic activation through β-adrenergic receptors. It has been used as a marker to measure effects of stress reduction interventions [81]. The first responders and those in an intensive care set-up could be the priority population for future trials given they are at high risk of compassion fatigue. Equally important will be the considerations such as the settings (high- vs. low-income counties), language, and culture. Considering the ethical implications for any intervention to be assessed is an important issue in the design of future RCTs.
5. Conclusions
Our comprehensive systematic review with robust methodology including assessment of the risk of bias by a validated toll (ROB-2) indicates that current evidence on interventions for reducing compassion fatigue in healthcare providers is inadequate. Given the benefits reported in some of the included studies, there is an urgent need for well-designed and adequately powered definitive RCTs in this field. Our systematic review is helpful in the designing such trials.
Author Contributions
Conceptualization, S.P.; Methodology, S.P., D.P. and C.R.; Formal analysis, S.P. and D.P.; Data curation S.P., D.P. and C.R.; Writing—original draft preparation S.P. and D.P.; Writing—review and editing, S.P. and C.R.; Supervision, S.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Decety, J.; Bartal, I.B.-A.; Uzefovsky, F.; Knafo-Noam, A. Empathy as a driver of prosocial behaviour: Highly conserved neurobehavioural mechanisms across species. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20150077. [Google Scholar] [CrossRef]
- Irving, P.; Dickson, D. Empathy: Towards a conceptual framework for health professionals. Int. J. Health Care Qual. Assur. 2004, 17, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, D. Empathy, sympathy and compassion in healthcare: Is there a problem? Is there a difference? Does it matter? J. R. Soc. Med. 2016, 109, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, D. Clarifying empathy: The first step to more humane clinical care. Br. J. General. Pract. 2016, 66, e143–e145. [Google Scholar] [CrossRef] [PubMed]
- Moudatsou, M.; Stavropoulou, A.; Philalithis, A.; Koukouli, S. The role of empathy in health and social care professionals. Healthcare 2020, 8, 26. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Moscrop, A.; Mebius, A.; Fanshawe, T.R.; Lewith, G.; Bishop, F.L.; Mistiaen, P.; Roberts, N.W.; Dieninytė, E.; Hu, X.-Y.; et al. Effects of empathic and positive communication in healthcare consultations: A systematic review and meta-analysis. J. R. Soc. Med. 2018, 111, 240–252. [Google Scholar] [CrossRef] [PubMed]
- Dambha-Miller, H.; Feldman, A.L.; Kinmonth, A.L.; Griffin, S.J. Association between primary care practitioner empathy and risk of cardiovascular events and all-cause mortality among patients with type 2 diabetes: A population-based prospective cohort study. Ann. Fam. Med. 2019, 17, 311–318. [Google Scholar] [CrossRef]
- Sturzu, L.; Lala, A.; Bisch, M.; Guitter, M.; Dobre, D.; Schwan, R. Empathy and burnout–a cross-sectional study among mental healthcare providers in France. J. Med. Life 2019, 12, 21. [Google Scholar] [CrossRef] [PubMed]
- Doyle, C.; Lennox, L.; Bell, D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013, 3, e001570. [Google Scholar] [CrossRef]
- Wilkinson, H.; Whittington, R.; Perry, L.; Eames, C. Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burn. Res. 2017, 6, 18–29. [Google Scholar] [CrossRef]
- Babaei, S.; Taleghani, F.; Farzi, S. Components of Compassionate Care in Nurses Working in the Cardiac Wards: A Descriptive Qualitative Study. J. Caring Sci. 2022, 11, 240. [Google Scholar] [CrossRef]
- Chochinov, H.M. Dignity and the essence of medicine: The A, B, C, and D of dignity conserving care. BMJ 2007, 335, 184–187. [Google Scholar] [CrossRef]
- Goldberg, M.J. Compassionate Care: Making it a priority and the science behind it. J. Pediatr. Orthop. 2020, 40, S4–S7. [Google Scholar] [CrossRef]
- Perez-Bret, E.; Altisent, R.; Rocafort, J. Definition of compassion in healthcare: A systematic literature review. Int. J. Palliat. Nurs. 2016, 22, 599–606. [Google Scholar] [CrossRef]
- Frederick, C. Beyond empathy: The tree of compassion with malevolent ego states. Am. J. Clin. Hypn. 2016, 58, 331–346. [Google Scholar] [CrossRef]
- Sinclair, S.; Beamer, K.; Hack, T.F.; McClement, S.; Raffin Bouchal, S.; Chochinov, H.M.; Hagen, N.A. Sympathy, empathy, and compassion: A grounded theory study of palliative care patients’ understandings, experiences, and preferences. Palliat. Med. 2017, 31, 437–447. [Google Scholar] [CrossRef]
- Goetz, J.L.; Keltner, D.; Simon-Thomas, E. Compassion: An evolutionary analysis and empirical review. Psychol. Bull. 2010, 136, 351. [Google Scholar] [CrossRef]
- Hiçdurmaz, D.; İnci, F.A. Compassion fatigue: Description, causes and prevention. Curr. Approaches Psychiatry 2015, 7, 295–303. [Google Scholar] [CrossRef]
- Field, B. Can You Have too Much Empathy? 20 May 2022. Available online: https://www.verywellmind.com/can-you-have-too-much-empathy-5224139 (accessed on 12 April 2023).
- Oshberg, F. When Helping Hurts: The American Stress Institute. 2022. Available online: https://www.stress.org/military/for-practitionersleaders/compassion-fatigue (accessed on 12 April 2023).
- Haque, O.S.; Waytz, A. Why doctors should be more empathetic—But not too much more. Sci. Am. 2011, 26. Available online: https://www.scientificamerican.com/article/doctors-and-dehumanization-effect/ (accessed on 12 April 2023).
- Figley, C.R. Compassion fatigue as secondary traumatic stress disorder: An overview. In Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized; Psychosocial Stress Series; Figley, C.R., Ed.; Routledge Taylor and Francis Group: New York, NY, USA, 1995; pp. 1–20. [Google Scholar]
- Figley, C.R. Compassion fatigue: Toward a new understanding of the costs of caring. In Secondary Traumatic Stress: Self-Care Issues for Clinicians, Researchers, and Educators, 2nd ed.; Stamm, B.H., Ed.; The Sidran Press: Baltimore, MD, USA, 1999; pp. 3–28. [Google Scholar]
- Watson, J. The theory of human caring: Retrospective and prospective. Nurs. Sci. Q. 1997, 10, 49–52. [Google Scholar] [CrossRef]
- Watson, J. Nursing: The Philosophy and Science of Caring, Rev. ed.; University Press of Colorado: Boulder, CO, USA, 2008. [Google Scholar]
- Joinson, C. Coping with compassion fatigue. Nursing 1992, 22, 116, 118–120. [Google Scholar]
- Figley, C.R.; Kleber, R.J. Beyond the “victim”: Secondary traumatic stress. In Beyond Trauma: Cultural and Societal Dynamics; Kleber, R.J., Figley, C.R., Gersons, B.P.R., Eds.; Plenum Press: New York, NY, USA, 1995; pp. 75–98. [Google Scholar]
- Essary, J.N.; Barza, L.; Thurston, R.J. Secondary traumatic stress among educators. Kappa Delta Pi Rec. 2020, 56, 116–121. [Google Scholar] [CrossRef]
- Saggar, I. Compassion Satisfaction, Compassion Fatigue and Mental-Well Being among Health Care Workers during COVID-19 outbreak. Int. J. Indian Psychȯl. 2021, 9, 888–895. [Google Scholar] [CrossRef]
- Stamm, B. The Concise ProQOL Manual, 2nd ed.; ProQOL.org: Pocatello, ID, USA, 2010. [Google Scholar]
- Bhutani, J.; Bhutani, S.; Balhara, Y.P.S.; Kalra, S. Compassion fatigue and burnout amongst clinicians: A medical exploratory study. Indian. J. Psychol. Med. 2012, 34, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C. Job burnout: New directions in research and intervention. Curr. Dir. Psychol. Sci. 2003, 12, 189–192. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Buunk, B.P. Burnout: An overview of 25 years of research and theorizing. Handb. Work. Health Psychol. 2003, 2, 282–424. [Google Scholar]
- Ormiston, H.E.; Nygaard, M.A.; Apgar, S. A Systematic Review of Secondary Traumatic Stress and Compassion Fatigue in Teachers. Sch. Ment. Health 2022, 14, 802–817. [Google Scholar] [CrossRef] [PubMed]
- Robertson, S.; Olanloye, E.; Hon, Y.; England, A.; McNair, H.; Cruickshank, S. Are radiographers suffering from symptoms of compassion fatigue due to occupational stress: A systematic review. Radiography 2022, 28, 857–864. [Google Scholar] [CrossRef]
- Cieslak, R.; Shoji, K.; Douglas, A.; Melville, E.; Luszczynska, A.; Benight, C.C. A meta-analysis of the relationship between job burnout and secondary traumatic stress among workers with indirect exposure to trauma. Psychol. Serv. 2014, 11, 75. [Google Scholar] [CrossRef]
- McCann, I.L.; Pearlman, L.A. Vicarious traumatization: A framework for understanding the psychological effects of working with victims. J. Trauma. Stress. 1990, 3, 131–149. [Google Scholar] [CrossRef]
- Laurie Anne pearlman KWS. Treating therapists with vicarious traumatization and secondary traumatic stress disorders. In Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized; Figley, C.R., Ed.; Routledge Taylor and Francis Group: New York, NY, USA, 1995; pp. 150–177. [Google Scholar]
- Marshman, C.; Hansen, A.; Munro, I. Compassion fatigue in mental health nurses: A systematic review. J. Psychiatr. Ment. Health Nurs. 2022, 29, 529–543. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Campos, E.; Vargas-Román, K.; Velando-Soriano, A.; Suleiman-Martos, N.; Cañadas-de la Fuente, G.A.; Albendín-García, L.; Gómez-Urquiza, J.L. Compassion fatigue, compassion satisfaction, and burnout in oncology nurses: A systematic review and meta-analysis. Sustainability 2019, 12, 72. [Google Scholar] [CrossRef]
- Sousa, L.; Ferreira, B.; Silva, P.; Tomás, M.; José, H.; Garcia-Navarro, E.B.; Ortega-Galán, Á. Bibliometric Analysis of the Scientific Production on Compassion Fatigue. J. Pers. Med. 2022, 12, 1574. [Google Scholar] [CrossRef]
- Van Mol, M.M.; Kompanje, E.J.; Benoit, D.D.; Bakker, J.; Nijkamp, M.D. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: A systematic review. PLoS ONE 2015, 10, e0136955. [Google Scholar] [CrossRef]
- Stoewen, D.L. Moving from compassion fatigue to compassion resilience Part 4: Signs and consequences of compassion fatigue. Can. Vet. J. 2020, 61, 1207. [Google Scholar]
- Hooper, C.; Craig, J.; Janvrin, D.R.; Wetsel, M.A.; Reimels, E. Compassion satisfaction, burnout, and compassion fatigue among emergency nurses compared with nurses in other selected inpatient specialties. J. Emerg. Nurs. 2010, 36, 420–427. [Google Scholar] [CrossRef]
- Mathieu, F. The Compassion Fatigue Workbook: Creative Tools for Transforming Compassion Fatigue and Vicarious Traumatization; Routledge: New York, NY, USA, 2012. [Google Scholar]
- Cocker, F.; Joss, N. Compassion fatigue among healthcare, emergency and community service workers: A systematic review. Int. J. Environ. Res. Public Health 2016, 13, 618. [Google Scholar] [CrossRef]
- Aluttis, C.; Bishaw, T.; Frank, M.W. The workforce for health in a globalized context–global shortages and international migration. Glob. Health Action 2014, 7, 23611. [Google Scholar] [CrossRef]
- Conversano, C.; Ciacchini, R.; Orrù, G.; Di Giuseppe, M.; Gemignani, A.; Poli, A. Mindfulness, compassion, and self-compassion among health care professionals: What’s new? A systematic review. Front. Psychol. 2020, 11, 1683. [Google Scholar] [CrossRef]
- Xie, W.; Chen, L.; Feng, F.; Okoli, C.T.; Tang, P.; Zeng, L.; Jin, M.; Zhang, Y.; Wang, J. The prevalence of compassion satisfaction and compassion fatigue among nurses: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021, 120, 103973. [Google Scholar] [CrossRef] [PubMed]
- Crego, A.; Yela, J.R.; Riesco-Matías, P.; Gómez-Martínez, M.; Vicente-Arruebarrena, A. The Benefits of Self-Compassion in Mental Health Professionals: A Systematic Review of Empirical Research. Psychol. Res. Behav. Manag. 2022, 15, 2599–2620. [Google Scholar] [CrossRef]
- Gillman, L.; Adams, J.; Kovac, R.; Kilcullen, A.; House, A.; Doyle, C. Strategies to promote coping and resilience in oncology and palliative care nurses caring for adult patients with malignancy: A comprehensive systematic review. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 131–204. [Google Scholar] [CrossRef]
- Greinacher, A.; Derezza-Greeven, C.; Herzog, W.; Nikendei, C. Secondary traumatization in first responders: A systematic review. Eur. J. Psychotraumatol. 2019, 10, 1562840. [Google Scholar] [CrossRef]
- Hasanpoor, E.; Hajebrahimi, S.; Janati, A.; Abedini, Z.; Haghgoshayie, E. Barriers, facilitators, process and sources of evidence for evidence-based management among health care managers: A qualitative systematic review. Ethiop. J. Health Sci. 2018, 28. [Google Scholar] [CrossRef]
- Chen, X.; Chen, M.; Zheng, H.; Wang, C.; Chen, H.; Wu, Q.; Liao, H.; Zhu, J.; Lin, J.; Ou, X.; et al. Effects of psychological intervention on empathy fatigue in nurses: A meta-analysis. Front. Public. Health 2022, 10, 952932. [Google Scholar] [CrossRef]
- Xie, W.; Wang, J.; Luo, X.; Tang, P.; Zeng, L.; Jin, M. Meta-analysis of the effect of psychological intervention on compassion fatigue of nursing staff. Chin. J. Labor Health Occup. Dis. 2022, 40, 39–45. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: New York, NY, USA, 2019. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 105906. [Google Scholar] [CrossRef]
- Deakin University, Master of Leadership, Unit MPP 703. Available online: https://www.deakin.edu.au/course/master-leadership (accessed on 12 April 2023).
- Bride, B.E.; Radey, M.; Figley, C.R. Measuring compassion fatigue. Clin. Social. Work. J. 2007, 35, 155–163. [Google Scholar] [CrossRef]
- Heritage, B.; Rees, C.S.; Hegney, D.G. The ProQOL-21: A revised version of the Professional Quality of Life (ProQOL) scale based on Rasch analysis. PLoS ONE 2018, 13, e0193478. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of burnout among physicians: A systematic review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef]
- Yıldırım, S.; Cavcav, F. The Compassion Fatigue-Short Scale for healthcare professionals: A Turkish study of validity and reliability. Perspect. Psychiatr. Care 2021, 57, 1459–1465. [Google Scholar] [CrossRef]
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Santesso, N.; Helfand, M.; Vist, G.; Kunz, R.; Brozek, J.; Norris, S.; Meerpohl, J.; Djulbegovic, B.; et al. GRADE guidelines: 12. Preparing summary of findings tables—Binary outcomes. J. Clin. Epidemiol. 2013, 66, 158–172. [Google Scholar] [CrossRef]
- Abasi, S.; Akbari, H.; Sabery, M. The effects of acupressure on sleep quality and compassion fatigue among emergency and critical care nurses during the coronavirus disease 2019 epidemic: A clinical trial. Nurs. Midwifery Stud. 2022, 11, 79–84. [Google Scholar]
- Goktas, S.; Gezginci, E.; Kartal, H. The effects of motivational messages sent to emergency nurses during the COVID-19 pandemic on job satisfaction, compassion fatigue, and communication skills: A randomized controlled trial. J. Emerg. Nurs. 2023, 48, 547–558, Erratum in: J. Emerg. Nurs. 2023, 49, 149. [Google Scholar] [CrossRef]
- Pérez, V.; Menéndez-Crispín, E.J.; Sarabia-Cobo, C.; de Lorena, P.; Fernández-Rodríguez, A.; González-Vaca, J. Mindfulness-based intervention for the reduction of compassion fatigue and burnout in nurse caregivers of institutionalized older persons with dementia: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 11441. [Google Scholar] [CrossRef]
- Partlak Günüşen, N.; Şengün İnan, F.; Üstün, B.; Serttaş, M.; Sayin, S.; Yaşaroğlu Toksoy, S. The effect of a nurse-led intervention program on compassion fatigue, burnout, compassion satisfaction, and psychological distress in nurses: A randomized controlled trial. Perspect. Psychiatr. Care 2022, 58, 1576–1586. [Google Scholar] [CrossRef]
- Halamová, J.; Ondrejková, N.; Kováč, K. Randomized controlled trial of emotion-focused training for helping professionals. Front. Psychol. 2022, 13, 1024451. [Google Scholar] [CrossRef]
- Copeland, D. Brief workplace interventions addressing burnout, compassion fatigue, and teamwork: A pilot study. West. J. Nurs. Res. 2021, 43, 130–137. [Google Scholar] [CrossRef]
- Pehlivan, T.; Güner, P. Effect of a compassion fatigue resiliency program on nurses’ professional quality of life, perceived stress, resilience: A randomized controlled trial. J. Adv. Nurs. 2020, 76, 3584–3596. [Google Scholar] [CrossRef] [PubMed]
- Clarke-Walper, K.; Penix, E.A.; Trachtenberg, F.; Simon, E.; Coleman, J.; Magnavita, A.; Ortigo, K.; Regala, S.; Marceau, L.; Ruzek, J.I.; et al. Efficacy of a web-based tool in reducing burnout among behavioral health clinicians: Results from the PTSD Clinicians Exchange. Psychiatr. Res. Clin. Pract. 2020, 2, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Emani, R.; Ghavami, H.; Radfar, M.; Khalkhali, H.R. Impact of chromotherapy on professional quality of life in intensive care unit nurses: A randomized controlled trial. Fatigue Biomed. Health Behav. 2020, 8, 121–129. [Google Scholar] [CrossRef]
- Shin, Y.K.; Lee, S.Y.; Lee, J.M.; Kang, P.; Seol, G.H. Effects of short-term inhalation of Patchouli oil on professional quality of life and stress levels in emergency nurses: A randomized controlled trial. J. Altern. Complement. Med. 2020, 26, 1032–1038. [Google Scholar] [CrossRef]
- Kharatzadeh, H.; Alavi, M.; Mohammadi, A.; Visentin, D.; Cleary, M. Emotional regulation training for intensive and critical care nurses. Nurs. Health Sci. 2020, 22, 445–453. [Google Scholar] [CrossRef]
- Kiley, K.A.; Sehgal, A.R.; Neth, S.; Dolata, J.; Pike, E.; Spilsbury, J.C.; Albert, J.M. The effectiveness of guided imagery in treating compassion fatigue and anxiety of mental health workers. Social. Work. Res. 2018, 42, 33–43. [Google Scholar] [CrossRef]
- Duchemin, A.M.; Steinberg, B.A.; Marks, D.R.; Vanover, K.; Klatt, M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: Effects on salivary α-amylase levels. J. Occup. Environ. Med. 2015, 57, 393. [Google Scholar] [CrossRef]
- Horner, J.K.; Piercy, B.S.; Eure, L.; Woodard, E.K. A pilot study to evaluate mindfulness as a strategy to improve inpatient nurse and patient experiences. Appl. Nurs. Res. 2014, 27, 198–201. [Google Scholar] [CrossRef]
- Berger, R.; Gelkopf, M. An intervention for reducing secondary traumatization and improving professional self-efficacy in well baby clinic nurses following war and terror: A random control group trial. Int. J. Nurs. Stud. 2011, 48, 601–610. [Google Scholar] [CrossRef]
- Stamm, B.H. Professional Quality of Life: Compassion Satisfaction and Fatigue Version 5 (ProQOL); ProQOL.org: Pocatello, ID, USA, 2009. [Google Scholar]
- Stamm, B.H. The ProQOL Manual: The Professional Quality of Life Scale: Compassion Satisfaction, Burnout & Compassion Fatigue/Secondary Trauma Scales; Sidran Press: Baltimore, MD, USA, 2005; pp. S1–S13. [Google Scholar]
- Hotchkiss, J.T.; Wong, M.Y.C. Factorial Structure of the ProQOL—Systematic Meta-analysis and Integration of 27 International Factor Analysis Studies. Trends Psychol. 2022, 1–32. [Google Scholar] [CrossRef]
- Taber, K.S. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Cho, E. A comprehensive review of so-called Cronbach’s alpha. J. Product. Res. 2020, 38, 9–20. [Google Scholar]
- Sabery, M.; Tafreshi, M.Z.; Hosseini, M.; Mohtashami, J.; Ebadi, A. Development and psychometric evaluation of the nurses’ compassion fatigue inventory. J. Nurs. Meas. 2017, 25, 185–201. [Google Scholar] [CrossRef]
- Kang, H.; Bang, K. Development and evaluation of a self-reflection program for intensive care unit nurses who have experienced the death of pediatric patients. J. Korean Acad. Nurs. 2017, 47, 392. [Google Scholar] [CrossRef]
- Wylde, C.M.; Mahrer, N.E.; Meyer, R.M.; Gold, J.I. Mindfulness for novice pediatric nurses: Smartphone application versus traditional intervention. J. Pediatr. Nurs. 2017, 36, 205–212. [Google Scholar] [CrossRef]
- Slatyer, S.; Craigie, M.; Heritage, B.; Davis, S.; Rees, C. Evaluating the effectiveness of a brief mindful self-care and resiliency (MSCR) intervention for nurses: A controlled trial. Mindfulness 2018, 9, 534–546. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Evaluating Stress: A Book of Resources; Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1997; Volume 3, pp. 191–218. [Google Scholar]
- Wagnild, G.M.; Guinn, P.E.; Center, R. The Resilience Scale User’s Guide: For the Us English Version of the Resilience Scale and the 14-Item Resilience Scale (rs-14); Resilience Center: Billings, MT, USA, 2011. [Google Scholar]
- Flarity, K.; Gentry, J.E.; Mesnikoff, N. The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Adv. Emerg. Nurs. J. 2013, 35, 247–258. [Google Scholar] [CrossRef]
- Hansen, E.M.; Eklund, J.H.; Hallén, A.; Bjurhager, C.S.; Norrström, E.; Viman, A.; Stocks, E.L. Does feeling empathy lead to compassion fatigue or compassion satisfaction? The role of time perspective. J. Psychol. 2018, 152, 630–645. [Google Scholar] [CrossRef] [PubMed]
- Wagaman, M.A.; Geiger, J.M.; Shockley, C.; Segal, E.A. The role of empathy in burnout, compassion satisfaction, and secondary traumatic stress among social workers. Soc. Work. 2015, 60, 201–209. [Google Scholar] [CrossRef]
- Cummings, C.; Singer, J.; Hisaka, R.; Benuto, L.T. Compassion satisfaction to combat work-related burnout, vicarious trauma, and secondary traumatic stress. J. Interpers. Violence 2021, 36, NP5304–NP5319. [Google Scholar] [CrossRef]
- Hariton, E.; Locascio, J.J. Randomised controlled trials—The gold standard for effectiveness research: Study design: Randomised controlled trials. BJOG 2018, 125, 1716. [Google Scholar] [CrossRef] [PubMed]
- Hannan, E.L. Randomized clinical trials and observational studies: Guidelines for assessing respective strengths and limitations. JACC Cardiovasc. Interv. 2008, 1, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Thadani, R. Formal trials versus observational studies. Chapter 14. In Fabry Disease: Perspectives from 5 Years of FOS.; Mehta, A., Beck, M., Sunder-Plassmann, G., Eds.; Oxford Pharma Genesis: Oxford, UK, 2006. Available online: https://www.ncbi.nlm.nih.gov/books/NBK11597/ (accessed on 12 April 2023).
- Hackshaw, A. Small studies: Strengths and limitations. Eur. Respir. J. 2008, 32, 1141–1143. [Google Scholar] [CrossRef]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef]
- Centre for Evaluation. London School of Hygiene and Tropical Medicine. Available online: https://www.lshtm.ac.uk/research/centres/centre-evaluation/cluster-randomised-trials#:~:text=In%20some%20circumstances%2C%20cluster%20randomisation,rather%20than%20at%20individual%20level (accessed on 18 April 2023).
- Taljaard, M.; Grimshaw, J.M. Concept, characteristics and implications of cluster randomization. Clin. Investig. 2014, 4, 1–4. [Google Scholar] [CrossRef]
- Elley, C.R.; Chondros, P.; Kerse, N.M. Randomised trials—Cluster versus individual randomisation Primary Care Alliance for Clinical Trials (PACT) network. Aust. Fam. Physician Sept. 2004, 33, 759–763. [Google Scholar]
- Hemming, K.; Eldridge, S.; Forbes, G.; Weijer, C.; Taljaard, M. How to design efficient cluster randomised trials. BMJ 2017, 358, j3064. [Google Scholar] [CrossRef] [PubMed]
- Hemming, K.; Girling, A.J.; Sitch, A.J.; Marsh, J.; Lilford, R.J. Sample size calculations for cluster randomised controlled trials with a fixed number of clusters. BMC Med. Res. Methodol. 2011, 11, 102, Erratum in: BMC Med. Res. Methodol. 2017, 17, 8.. [Google Scholar] [CrossRef]
- Campbell, M.K.; Grimshaw, J.M.; Elbourne, D.R. Intracluster correlation coefficients in cluster randomized trials: Empirical insights into how should they be reported. BMC Med. Res. Methodol. 2004, 4, 9. [Google Scholar] [CrossRef] [PubMed]
- Tishkovskaya, S.V.; Sutton, C.J.; Thomas, L.H.; Watkins, C.L. Determining the sample size for a cluster-randomised trial using knowledge elicitation: Bayesian hierarchical modelling of the intracluster correlation coefficient. Clin. Trials 2023, 10, 17407745231164569. [Google Scholar] [CrossRef]
- Tong, J.; Li, F.; Harhay, M.O.; Tong, G. Accounting for expected attrition in the planning of cluster randomized trials for assessing treatment effect heterogeneity. BMC Med. Res. Methodol. 2023, 23, 85. [Google Scholar] [CrossRef]
- Harrison, L.J.; Wang, R. Sample size calculation for randomized trials via inverse probability of response weighting when outcome data are missing at random. Stat. Med. 2023, 42, 1802–1821. [Google Scholar] [CrossRef]
- Davis-Plourde, K.; Taljaard, M.; Li, F. Power analyses for stepped wedge designs with multivariate continuous outcomes. Stat. Med. 2023, 42, 559–578. [Google Scholar] [CrossRef]
- Bolland, M.J.; Avenell, A.; Grey, A. Analysis of cluster randomised trials as if they were individually randomised. Lancet Diabetes Endocrinol. 2023, 11, 75. [Google Scholar] [CrossRef]
- Hemming, K.; Haines, T.P.; Chilton, P.J.; Girling, A.J.; Lilford, R.J. The stepped wedge cluster randomised trial: Rationale, design, analysis, and reporting. BMJ 2015, 350, h391. [Google Scholar] [CrossRef]
- Dreischulte, T.; Grant, A.; Donnan, P.; Guthrie, B. Pro’s and con’s of the stepped wedge design in cluster randomised trials of quality improvement interventions: Two current examples. Trials 2013, 14 (Suppl. S1), O87. [Google Scholar] [CrossRef][Green Version]
- Lee, H.J.; Lee, M.; Jang, S.J. Compassion satisfaction, secondary traumatic stress, and burnout among nurses working in trauma centers: A cross-sectional study. Int. J. Env. Res. Public. Health 2021, 18, 7228. [Google Scholar] [CrossRef] [PubMed]
- Misouridou, E.; Pavlou, V.; Kasidi, K.; Apostolara, P.; Parissopoulos, S.; Mangoulia, P.; Fradelos, E. Translation and cultural adaptation of the Professional Quality of Life Scale (ProQOL V) for Greece. Mater. Sociomed. 2020, 32, 187–190. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).