The Mediating Effects of Symptom Experiences on the Relationship between Body Image and Quality of Life among Hemodialysis Patients in a Single Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Instrument
2.2.1. Body Image
2.2.2. Symptom Experiences
2.2.3. Quality of Life
2.3. Data Collection
2.4. Ethical Consideration
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics and Differences in Quality of Life
3.2. Degrees of Body Image, Symptom Experiences and Quality of Life
3.3. Correlations among Body Image, Symptom Experiences, and Quality of Life
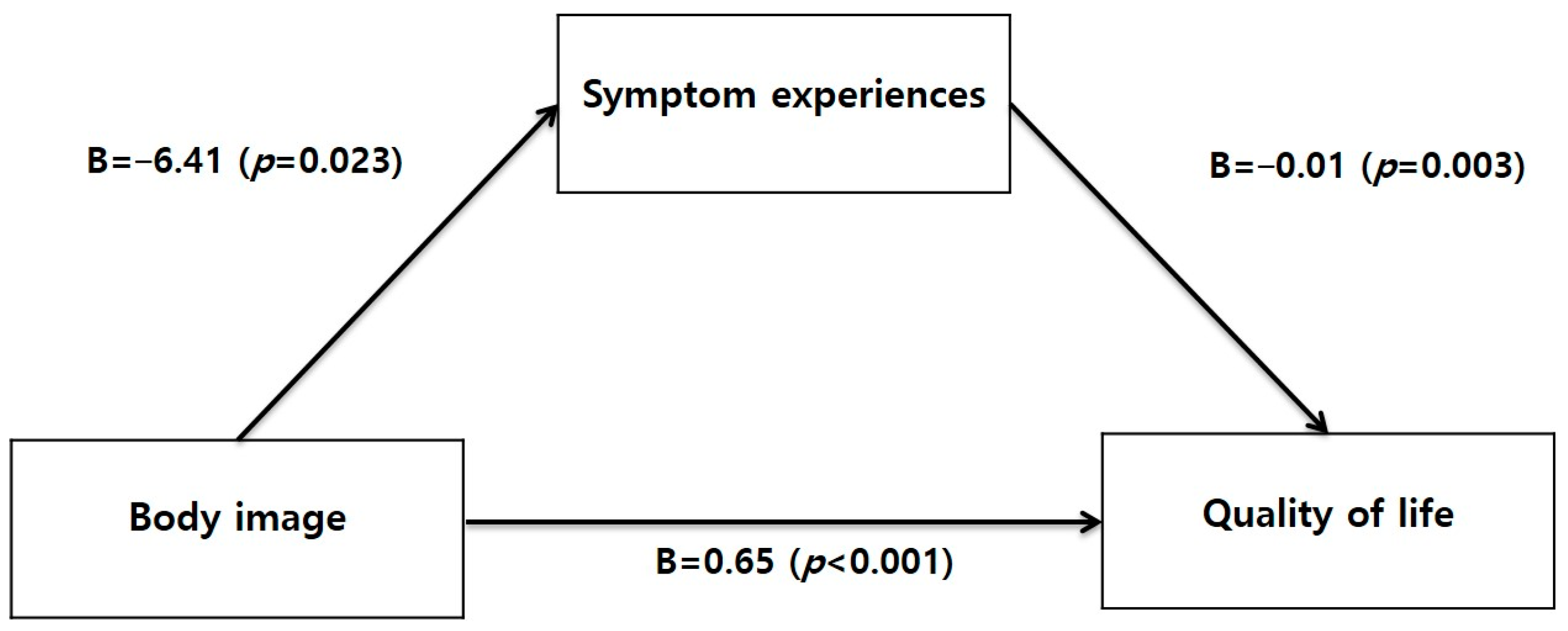
3.4. Mediating Effect of Symptom Experiences between Body Image and Quality of Life
4. Discussion
5. Conclusions
6. Limitations
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ESRD Registry Committee. Current Renal Replacement Therapy in Korea; The Korean Society of Nephrology: Seoul, Republic of Korea, 2023; Available online: https://ksn.or.kr/bbs/index.php?code=report (accessed on 15 July 2024).
- Musavi Ghahfarokhi, M.; Mohammadian, S.; Mohammadi Nezhad, B.; Kiarsi, M. Relationship between spiritual health and hope by dietary adherence in hemodialysis patients in 2018. Nurs. Open 2019, 7, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Li, C.Y.; Hsieh, C.J.; Shih, Y.L.; Lin, Y.T. Spiritual well-being of patients with chronic renal failure: A cross-sectional study. Nurs. Open 2021, 8, 2461–2469. [Google Scholar] [CrossRef]
- Shaheen, F.A.M.; Al-Attar, B.; Ahmad, M.K.; Follero, P.M. Burden of disease: Prevalence and incidence of end stage renal disease in Middle Eastern countries. Clin. Nephrol. 2020, 93, 120–123. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States. 2023. Available online: https://www.cdc.gov/kidney-disease/php/data-research/index.html (accessed on 15 July 2024).
- Kallenbach, J. Review of Hemodialysis for Nurses and Dialysis Personnel; Elsevier: Maryland Heights, MO, USA, 2020. [Google Scholar]
- Di Corrado, D.; Coco, M.; Guarnera, M.; Maldonato, N.M.; Quartiroli, A.; Magnano, P. The influence of self-efficacy and locus of control on body image: A path-analysis in aspiring fashion models, athletes and students. Int. J. Environ. Res. Public Health 2021, 18, 6128. [Google Scholar] [CrossRef]
- Kim, E.K.; Hwang, S.K.; Lee, Y.J. Dialysis adequacy, symptom experience, mood states, and hope among patients receiving hemodialysis. Glob. Health Nurs. 2018, 8, 90–100. [Google Scholar] [CrossRef]
- Horigan, A.E. Fatigue in hemodialysis patients: A review of current knowledge. J. Pain Symptom Manag. 2012, 44, 715–724. [Google Scholar] [CrossRef]
- Broers, N.J.; Martens, R.J.; Canaud, B.; Cornelis, T.; Dejagere, T.; Diederen, N.M.; Hermans, M.M.; Konings, C.J.; Stifft, F.; Wirtz, J.J.; et al. Health-related quality of life in end-stage renal disease patients: The effects of starting dialysis in the first year after the transition period. Int. Urol. Nephrol. 2018, 50, 1131–1142. [Google Scholar] [CrossRef]
- Jung, H.Y.; Park, Y.K.; Suh, S.R. Factors affecting quality of life of hemodialysis patients: With focus on resilience, symptom experience and self-management. J. Health Inform. Stat. 2021, 46, 429–434. [Google Scholar] [CrossRef]
- Hur, J. Treatment related-stressors and stress coping methods of hemodialysis noncompliant patients. J. Korean Acad. Nurs. Adm. 2005, 11, 439–448. [Google Scholar]
- Lee, H.N.; Sim, J.H. The impact of symptom experience and self-care agency on quality of life in patients with hemodialysis. J. Korean Clin. Nurs. Res. 2023, 29, 135–145. [Google Scholar] [CrossRef]
- Yom, Y.H.; Lee, K.E. Factors affecting body image of undergraduate students. J. Korean Acad. Fundam. Nurs. 2011, 18, 452–462. [Google Scholar]
- Gerogianni, S.; Babatsikou, F.; Gerogianni, G.; Grapsa, E.; Vasilopoulos, G.; Zyga, S.; Koutis, C. Concerns of patients on dialysis: A Research Study. Health Sci. J. 2014, 8, 423–437. [Google Scholar]
- Güçer, B.K.; Kantarcı, G. Body image perception of chronic kidney disease patients and its impact on their personal relationships. Turk. J. Nephrol. 2020, 29, 122–128. [Google Scholar] [CrossRef]
- Partridge, K.A.; Robertson, N. Body-image disturbance in adult dialysis patients. Disabil. Rehabil. 2011, 33, 504–510. [Google Scholar] [CrossRef]
- Sadeghian, J.; Roudsari, D.; Seyedfatemi, N.; Rafiei, H. Body-image disturbance: A comparative study among haemodialysis and kidney transplant patients. J. Clin. Diagn. Res. 2016, 10, 14–16. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, M.Y. The experience of fluid management in hemodialysis patients. J. Korean Acad. Nurs. 2015, 45, 773–782. [Google Scholar] [CrossRef]
- Tanyi, R.A. Sexual unattractiveness: A patient’s story. Medsurg Nurs. 2002, 11, 95–99. [Google Scholar]
- Seo, N.S.; Sim, E.K. Influence of social support and health literacy on treatment adherence in hemodialysis patients. J. Korea Acad.-Ind. Coop. Soc. 2020, 21, 656–666. [Google Scholar] [CrossRef]
- Jesus, N.M.; Souza, G.F.; Mendes-Rodrigues, C.; Almeida Neto, O.P.; Rodrigues, D.M.; Cunha, C.M. Quality of life of individuals with chronic kidney disease on dialysis. J. Bras. Nephrol. 2019, 41, 364–374. [Google Scholar] [CrossRef]
- Cha, J.E.; Yi, M.S. Symptom clusters and quality of life in patients on hemodialysis. J. Korean Clin. Nurs. Res. 2014, 20, 123–133. [Google Scholar]
- Kim, G.D. Effects of symptom clusters, spiritual well-being on the quality of life in patients undergoing hemodialysis. J. Kyungpook Nurs. Sci. 2020, 24, 59–70. [Google Scholar] [CrossRef]
- Cho, Y.H.; Lee, Y.M. Resilience as a moderator and mediator of the relationship between symptom experience and quality of life in hemodialysis patients. Korean J. Adult Nurs. 2019, 31, 68–77. [Google Scholar] [CrossRef]
- Lee, M.H.; Song, M.S.; Yoo, K.M. Relationship among powerlessness, self-efficacy and quality of life in hemodialysis patients. Korean J. Rehabil. Nurs. 2002, 5, 166–179. [Google Scholar]
- Morsch, C.M.; Goncalves, L.F.; Barros, E. Health-related quality of life among hemodialysis patients-relationship with clinical indicators, morbidity and mortality. J. Clin. Nurs. 2006, 15, 498–504. [Google Scholar] [CrossRef]
- Choi, H.S.; Kang, S.G.; Boo, C.S.; Lee, H.J.; Cho, W.Y.; Kim, H.K.; Kim, L. Restless legs syndrome and quality of life in hemodialysis patients. Sleep Med. Psychophysiol. 2007, 14, 99–106. [Google Scholar]
- Kraus, M.A.; Fluck, R.J.; Weinhandl, E.D.; Kansal, S.; Copland, M.; Komenda, P.; Finkelstein, F.O. Intensive hemodialysis and health-related quality of life. Am. J. Kidney Dis. 2016, 68, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Seo, N.S.; Kang, S.J.; Kim, J.H.; Kim, S.J. Relationships between fatigue, sleep disturbance, stress, self-efficacy and depression in hemodialysis patients. J. Korean Clin. Nurs. Res. 2013, 19, 285–297. [Google Scholar]
- Lee, Y.H.; Kim, H.S. The effect of family support, self-efficacy, and fatigue on the quality of life in hemodialysis patients. J. East-West Nurs. Res. 2015, 21, 1–9. [Google Scholar] [CrossRef]
- Moon, S.M.; Cha, C.Y. Relationship of symptom clusters, compliance with the patient’s role behavior, and dialysis adequacy with quality of life in hemodialysis patients. J. Korean Acad. Fundam. Nurs. 2022, 29, 295–304. [Google Scholar] [CrossRef]
- Alemayehu, Y.H.; Seylania, K.; Bahramnezhad, F. The relationship between health literacy and quality of life among hemodialysis patients: An integrative review. Hum. Antibodies 2020, 18, 75–81. [Google Scholar] [CrossRef]
- Kim, S.S.; Choi, Y.S. Effects of a repeated hemodialysis diet education program for older adults. Korean J. Adult Nurs. 2020, 32, 515–525. [Google Scholar] [CrossRef]
- Ki, E.J.; So, H.S. Development and effects of smartphone app-based exercise program for hemodialysis patients. J. Korean Acad. Nurs. 2020, 50, 52–65. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Cash, T.F. The situational inventory of body-image dysphoria: Psychometric evidence and development of a short form. Int. J. Eat. Disord. 2002, 32, 362–366. [Google Scholar] [CrossRef]
- Kang, S.Y. Appearance Complex and Body-Image. Master’s Thesis, Catholic University, Seoul, Republic of Korea, 2003. [Google Scholar]
- Weisbord, S.D.; Fried, L.F.; Arnold, R.M.; Rotondi, A.J.; Fine, M.J.; Levenson, D.J.; Switzer, G.E. Development of a symptom assessment instrument for chronic hemodialysis patients: The dialysis symptom index. J. Pain Symptom Manag. 2004, 27, 226–240. [Google Scholar] [CrossRef]
- Lim, E.J. Symptom Clusters, Depression and Quality of Life in Patients on Hemodialysis. Master’s Thesis, Kyung Hee University, Seoul, Republic of Korea, 2016. [Google Scholar]
- Min, S.K.; Lee, C.I.; Kim, K.I.; Suh, S.Y.; Kim, D.K. Development of Korean version of WHO quality of life scale abbreviated version (WHOQOL-BREF). J. Korean Neuropsychiatr. Assoc. 2000, 39, 571–579. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 28.0; Armonk: New York, NY, USA, 2021. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Sohn, S.K.; Lee, M.H.; Song, M.S. Relationship between body image and self-esteem in patients with chronic renal failure. J. Korean Acad. Fundam. Nurs. 2001, 8, 160–171. [Google Scholar]
- Lee, Y.J.; Lee, E.O. An exploratory study on clothing benefits sought by breast cancer survivors. Res. J. Costume Cult. 2014, 22, 823–833. [Google Scholar]
- Cha, J.E.; Han, D.L. Factors related to hope and relationships between hope, physical symptoms, depressive mood and quality of life in young adult and prime-aged patients with hemodialysis. J. Korean Acad. Psychiatr. Ment. Health Nurs. 2014, 23, 250–258. [Google Scholar] [CrossRef]
- Park, S.M.; Kim, C.H.; Hur, H.K.; Kim, G.Y. A descriptive study on development of an ALARM sexual counseling program for patients with ostomy. J. Korean Pubilc Health Nurs. 2007, 21, 46–56. [Google Scholar]
- Smith, D.H.; Pillemer, K. Self-help groups as social movement organizations: Social structure and social change. Res. Soc. Mov. Confl. Chang. 1983, 5, 203–233. [Google Scholar]
- Kim, B.K.; Oh, P.J. The effects of spiritual well-being on self-care practices in people undergoing hemodialysis: The mediating effect of hope. Korean J. Adult Nurs. 2022, 34, 592–601. [Google Scholar] [CrossRef]
- Lee, Y.J.; Oh, E.G. Body image, self esteem, and health related quality of life in patients with crohn’s disease. Korean J. Adult Nurs. 2014, 26, 383–392. [Google Scholar] [CrossRef]
| Variables | Categories | n (%) | Mean ± SD | t or F (p-Value) | Scheffé |
|---|---|---|---|---|---|
| Sex | Male | 80 (52.3) | 2.94 ± 0.46 | −0.98 (0.331) | |
| Female | 73 (47.7) | 3.02 ± 0.52 | |||
| Age (yr) | ≤39 | 9 (5.8) | 3.05 ± 0.63 | 0.53 (0.711) | |
| 40~49 | 11 ( 7.2) | 2.85 ± 0.41 | |||
| 50~59 | 31 (20.3) | 2.93 ± 0.43 | |||
| 60~69 | 57 (37.3) | 2.98 ± 0.49 | |||
| ≥70 | 45 (29.4) | 3.05 ± 0.52 | |||
| Marital status | Unmarried | 30 (19.6) | 2.82 ± 0.41 | 2.61 (0.077) | |
| Married | 102 (66.7) | 3.04 ± 0.51 | |||
| Others | 21 (13.7) | 2.91 ± 0.45 | |||
| Religion | Yes | 72 (47.1) | 3.07 ± 0.51 | 2.17 (0.031) | |
| No | 81 (52.9) | 2.90 ± 0.46 | |||
| Education | ≤Elementary school | 37 (24.2) | 2.85 ± 0.46 | 2.43 (0.068) | |
| Middle school | 30 (19.6) | 2.95 ± 0.55 | |||
| High school | 54 (35.3) | 2.99 ± 0.44 | |||
| ≥College | 32 (20.9) | 3.16 ± 0.52 | |||
| Occupation | Yes | 24 (15.7) | 3.29 ± 0.51 | 3.40 (0.001) | |
| No | 129 (84.3) | 2.93 ± 0.47 | |||
| Monthly family income (KRW 10,000) | <100 a | 63 (41.2) | 2.78 ± 0.45 | 10.62 (<0.001) | d,c > a |
| 100~199 b | 35 (22.9) | 2.95 ± 042 | |||
| 200~299 c | 19 (12.4) | 3.11 ± 0.51 | |||
| ≥300 d | 36 (23.5) | 3.30 ± 0.45 | |||
| The person who helps the most | Spouse | 69 (45.1) | 3.05 ± 0.49 | 1.22 (0.305) | |
| Parents | 18 (11.8) | 2.86 ± 0.40 | |||
| Children | 36 (23.5) | 3.01 ± 0.52 | |||
| Others | 21 (13.7) | 2.95 ± 0.52 | |||
| None | 9 ( 5.9) | 2.73 ± 0.49 | |||
| Regular exercise | Yes | 78 (51.0) | 3.03 ± 0.48 | 1.35 (0.180) | |
| No | 75 (49.0) | 2.93 ± 0.50 | |||
| Etiology CKD | Diabetes mellitus | 89 (58.2) | 2.85 ± 0.41 | 0.54 (0.613) | |
| Hypertension | 47 (30.6) | 3.01 ± 0.61 | |||
| Kidney stone | 7 (4.8) | 2.93 ± 0.43 | |||
| Glomerulonephritis | 6 (4.0) | 2.91 ± 0.47 | |||
| malignancy | 4 (2.4) | 2.95 ± 0.51 | |||
| Comorbidity * | Yes | 94 (61.4) | 2.87 ± 0.47 | −3.71 (<0.001) | |
| No | 59 (38.6) | 3.16 ± 0.48 | |||
| Frequency of hemodialysis (week) | Twice | 37 (24.2) | 3.06 ± 0.43 | 1.17 (0.244) | |
| Three times | 116 (75.8) | 2.96 ± 0.51 | |||
| Hemodialysis periods(yr) | <2 | 40 (26.1) | 3.07 ± 0.46 | 1.12 (0.344) | |
| 2~4 | 46 (30.1) | 2.98 ± 0.51 | |||
| 4~9 | 44 (28.8) | 2.98 ± 0.53 | |||
| ≥10 | 23 (15.0) | 2.83 ± 0.44 | |||
| Moisture removal amount (kg) | <1 | 13 ( 8.5) | 2.94 ± 0.30 | 1.15 (0.331) | |
| 1~1.9 | 26 (17.0) | 3.09 ± 0.61 | |||
| 2~2.9 | 75 (49.0) | 2.92 ± 0.47 | |||
| ≥3 | 39 (25.5) | 3.05 ± 0.50 | |||
| Hospitalization experience in the past year | Yes | 61 (39.9) | 2.94 ± 0.49 | −0.96 (0.336) | |
| No | 92 (60.1) | 3.01 ± 0.49 |
| Variables | Mean ± SD | Min | Max | Possible Range |
|---|---|---|---|---|
| Body image | 2.88 ± 0.36 | 1.91 | 4.13 | 1–5 |
| Emotional dimension | 2.67 ± 0.50 | 1.63 | 4.33 | 1–5 |
| Cognitive–behavioral dimension | 3.02 ± 0.35 | 2.05 | 4.00 | 1–5 |
| Symptom experiences | 0.96 ± 0.79 | 0.00 | 4.47 | 0–5 |
| Physical symptoms | 0.94 ± 0.79 | 0.00 | 4.48 | 0–5 |
| Emotional symptoms | 1.03 ± 0.98 | 0.00 | 4.44 | 0–5 |
| Quality of life | 2.93 ± 0.46 | 2.04 | 4.31 | 1–5 |
| Overall quality of life and general health | 2.55 ± 0.86 | 1.00 | 5.00 | 1–5 |
| Physical health domain | 2.94 ± 0.46 | 1.71 | 4.00 | 1–5 |
| Psychological domain | 2.85 ± 0.52 | 1.67 | 4.33 | 1–5 |
| Social relationships domain | 2.66 ± 0.78 | 1.00 | 4.67 | 1–5 |
| Environmental domain | 3.19 ± 0.59 | 1.50 | 5.00 | 1–5 |
| Variables | Body Image | Symptom Experiences | Quality of Life |
|---|---|---|---|
| r (p) | r (p) | r (p) | |
| Body image | 1 | ||
| Symptom experiences | −0.18 (0.023) | 1 | |
| Quality of life | 0.61 (<0.001) | −0.31 (<0.001) | 11 |
| Step 1 | Step 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Symptom Experiences | Quality of Life | |||||||
| B | SE | t | p | B | SE | t | p | |
| (Constant) | 60.66 | 12.28 | 4.94 | <0.001 | 1.25 | 0.28 | 4.39 | <0.001 |
| Religion * (yes) | 1.40 | 2.79 | 0.50 | 0.617 | 0.08 | 0.06 | 1.33 | 0.185 |
| Occupation * (yes) | 5.48 | 4.03 | 1.36 | 0.176 | 0.16 | 0.09 | 1.84 | 0.067 |
| Monthly family income (KRW 100~199) | 0.57 | 3.62 | 0.156 | 0.876 | 0.10 | 0.08 | 1.29 | 0.200 |
| Monthly family income (KRW 200~299) | 0.80 | 4.52 | 0.18 | 0.861 | 0.19 | 0.10 | 1.98 | 0.049 |
| Monthly family income (≥KRW 300) | −0.47 | 3.87 | −0.12 | 0.903 | 0.26 | 0.08 | 3.12 | 0.002 |
| Comorbidities (yes) | 8.40 | 2.96 | 2.84 | 0.005 | −0.06 | 0.07 | −0.91 | 0.367 |
| Body image | −6.41 | 4.13 | −1.55 | 0.023 | 0.65 | 0.09 | 7.26 | <0.001 |
| Symptom experiences | −0.01 | 0.01 | −3.00 | 0.003 | ||||
| F(p) R2 (adj R2) d (du) | 2.01 (0.057) 0.090 (0.045) 1.96 (1.80) | 17.21 (<0.001) 0.49 (0.460) 2.05 (1.82) | ||||||
| B | Boot SE | Boot 95%CI | ||
|---|---|---|---|---|
| LLCI | ULCI | |||
| Body image → Symptom experiences → Quality of life | 0.044 | 0.024 | 0.006 | 0.100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y. The Mediating Effects of Symptom Experiences on the Relationship between Body Image and Quality of Life among Hemodialysis Patients in a Single Center. Healthcare 2024, 12, 1779. https://doi.org/10.3390/healthcare12171779
Yang Y. The Mediating Effects of Symptom Experiences on the Relationship between Body Image and Quality of Life among Hemodialysis Patients in a Single Center. Healthcare. 2024; 12(17):1779. https://doi.org/10.3390/healthcare12171779
Chicago/Turabian StyleYang, Yaki. 2024. "The Mediating Effects of Symptom Experiences on the Relationship between Body Image and Quality of Life among Hemodialysis Patients in a Single Center" Healthcare 12, no. 17: 1779. https://doi.org/10.3390/healthcare12171779
APA StyleYang, Y. (2024). The Mediating Effects of Symptom Experiences on the Relationship between Body Image and Quality of Life among Hemodialysis Patients in a Single Center. Healthcare, 12(17), 1779. https://doi.org/10.3390/healthcare12171779






