COVID-19 Recovery Time and Its Predictors among Hospitalized Patients in Designated Hospitals in the Madhesh Province of Nepal: A Multicentric Study
Abstract
1. Introduction
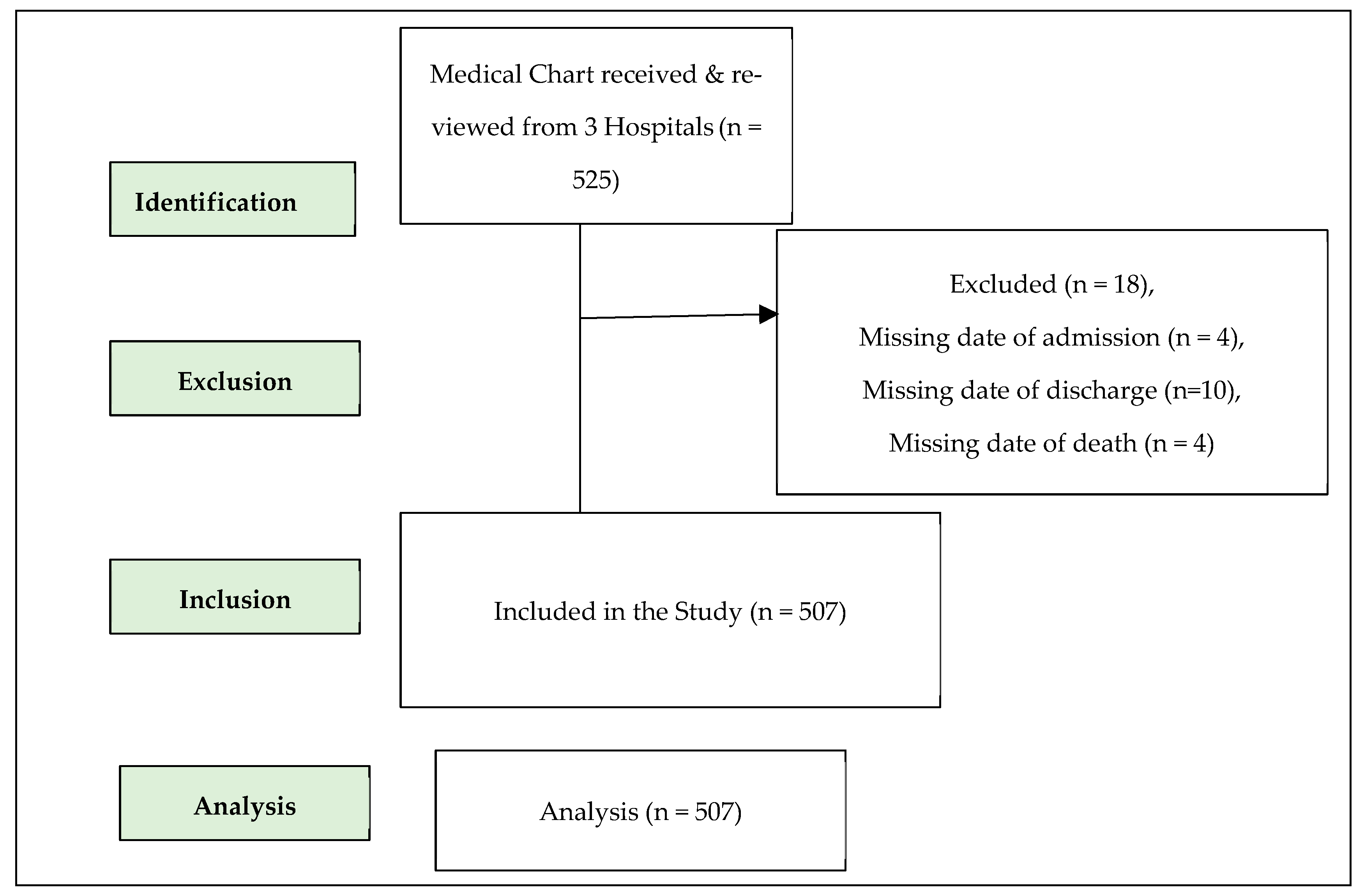
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Sample Size and Sampling Technique
2.4. Data Extraction and Analysis
2.5. Data Quality Assurance
2.6. Study Variables and Their Measurement
2.7. Statistical Methods
2.8. Ethics Statement
3. Results
3.1. Treatment Outcomes
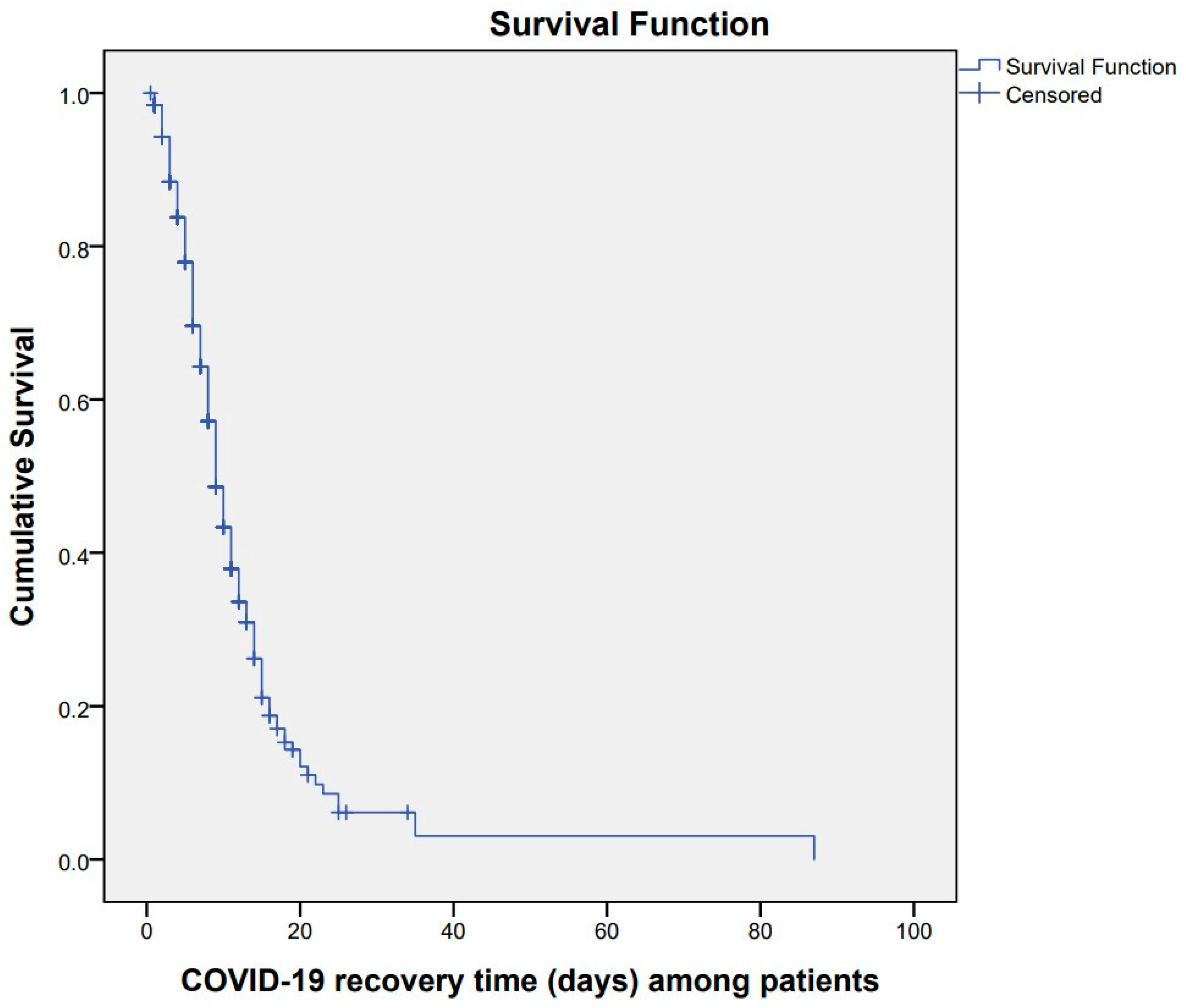
3.2. COVID-19 Recovery Time of Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Biancolella, M.; Colona, V.L.; Luzzatto, L.; Watt, J.L.; Mattiuz, G.; Conticello, S.G.; Kaminski, N.; Mehrian-Shai, R.; Ko, A.I.; Gonsalves, G.S.; et al. COVID-19 annual update: A narrative review. Hum. Genom. 2023, 17, 68. [Google Scholar] [CrossRef] [PubMed]
- Tamura, T.; Ito, J.; Uriu, K.; Zahradnik, J.; Kida, I.; Anraku, Y.; Nasser, H.; Shofa, M.; Oda, Y.; Lytras, S.; et al. Virological characteristics of the SARS-CoV-2 XBB variant derived from recombination of two Omicron subvariants. Nat. Commun. 2023, 14, 2800. [Google Scholar] [CrossRef] [PubMed]
- Marrone, M.; Buongiorno, L.; Stellacci, A.; Cazzato, G.; Stefanizzi, P.; Tafuri, S. COVID-19 Vaccination Policies: Ethical Issues and Responsibility. Vaccines 2022, 10, 1602. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19). Available online: https://www.who.int/news-room/fact-sheets/detail/coronavirus-disease-(covid-19) (accessed on 12 November 2023).
- Rothan, H.A.; Byrareddy, S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020, 109, 102433. [Google Scholar] [CrossRef]
- COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines; 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK570371/ (accessed on 24 February 2023).
- Bezzio, C.; Saibeni, S.; Variola, A.; Allocca, M.; Massari, A.; Gerardi, V.; Casini, V.; Ricci, C.; Zingone, F.; Amato, A.; et al. Outcomes of COVID-19 in 79 patients with IBD in Italy: An IG-IBD study. Gut 2020, 69, 1213–1217. [Google Scholar] [CrossRef]
- Desai, A.D.; Lavelle, M.; Boursiquot, B.C.; Wan, E.Y. Long-term complications of COVID-19. Am. J. Physiol.-Cell Physiol. 2022, 322, C1–C11. [Google Scholar] [CrossRef]
- Pei, G.; Zhang, Z.; Peng, J.; Liu, L.; Zhang, C.; Yu, C.; Ma, Z.; Huang, Y.; Liu, W.; Yao, Y.; et al. Renal Involvement and Early Prognosis in Patients with COVID-19 Pneumonia. J. Am. Soc. Nephrol. 2020, 31, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Arab-Zozani, M.; Hashemi, F.; Safari, H.; Yousefi, M.; Ameri, H. Health-Related Quality of Life and its Associated Factors in COVID-19 Patients. Osong Public Health Res. Perspect. 2020, 11, 296–302. [Google Scholar] [CrossRef]
- Di Fusco, M.; Shea, K.M.; Lin, J.; Nguyen, J.L.; Angulo, F.J.; Benigno, M.; Malhotra, D.; Emir, B.; Sung, A.H.; Hammond, J.L.; et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J. Med. Econ. 2021, 24, 308–317. [Google Scholar] [CrossRef]
- Kaye, A.D.; Okeagu, C.N.; Pham, A.D.; Silva, R.A.; Hurley, J.J.; Arron, B.L.; Sarfraz, N.; Lee, H.N.; Ghali, G.E.; Gamble, J.W.; et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best. Pract. Res. Clin. Anaesthesiol. 2021, 35, 293–306. [Google Scholar] [CrossRef]
- Nizigiyimana, A.; Acharya, D.; Poder, T.G. Impact of COVID-19 pandemic on the health-related quality of life of frontline workers: The case of seven low-income Eastern African countries. Health Qual. Life Outcomes 2023, 21, 97. [Google Scholar] [CrossRef]
- Ismaila, H.; Asamani, J.A.; Lokossou, V.K.; Oduro-Mensah, E.; Nabyonga-Orem, J.; Akoriyea, S.K. The cost of clinical management of SARS-COV-2 (COVID-19) infection by level of disease severity in Ghana: A protocol-based cost of illness analysis. BMC Health Serv. Res. 2021, 21, 1115. [Google Scholar] [CrossRef] [PubMed]
- Rees, E.M.; Nightingale, E.S.; Jafari, Y.; Waterlow, N.R.; Clifford, S.; Pearson, C.A.B.; CMMID Working Group; Jombart, T.; Procter, S.R.; Knight, G.M. COVID-19 length of hospital stay: A systematic review and data synthesis. BMC Med. 2020, 18, 270. [Google Scholar] [CrossRef] [PubMed]
- Baker, M.A.; Sands, K.E.; Huang, S.S.; Kleinman, K.; Septimus, E.J.; Varma, N.; Blanchard, J.; Poland, R.E.; Coady, M.H.; Yokoe, D.S.; et al. The Impact of Coronavirus Disease 2019 (COVID-19) on Healthcare-Associated Infections. Clin. Infect. Dis. 2021, 74, 1748–1754. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Scaravilli, V.; Mangioni, D.; Scudeller, L.; Alagna, L.; Bartoletti, M.; Bellani, G.; Biagioni, E.; Bonfanti, P.; Bottino, N.; et al. Hospital-Acquired Infections in Critically Ill Patients with COVID-19. Chest 2021, 160, 454–465. [Google Scholar] [CrossRef] [PubMed]
- Lemma Tirore, L.; Abose Nadamo, S.; Tamrat Derilo, H.; Erkalo, D.; Sedore, T.; Tadesse, T.; Ermias, D.; Yaekob, T. Time to Recovery from COVID-19 and Its Predictors Among Patients Admitted to Treatment Centers of Southern Nations Nationalities and Peoples Region (SNNPR), ETHIOPIA: Multi-Center Retrospective Cohort Study. Infect. Drug Resist. 2022, 15, 3047–3062. [Google Scholar] [CrossRef]
- Abrahim, S.A.; Tessema, M.; Defar, A.; Hussen, A.; Ejeta, E.; Demoz, G.; Tereda, A.B.; Dillnessa, E.; Feleke, A.; Amare, M.; et al. Time to recovery and its predictors among adults hospitalized with COVID-19: A prospective cohort study in Ethiopia. PLoS ONE 2020, 15, e0244269. [Google Scholar] [CrossRef] [PubMed]
- Tolossa, T.; Wakuma, B.; Seyoum Gebre, D.; Merdassa Atomssa, E.; Getachew, M.; Fetensa, G.; Ayala, D.; Turi, E. Time to recovery from COVID-19 and its predictors among patients admitted to treatment center of Wollega University Referral Hospital (WURH), Western Ethiopia: Survival analysis of retrospective cohort study. PLoS ONE 2021, 16, e0252389. [Google Scholar] [CrossRef] [PubMed]
- Meng, Y.; Wu, P.; Lu, W.; Liu, K.; Ma, K.; Huang, L.; Cai, J.; Zhang, H.; Qin, Y.; Sun, H.; et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: A retrospective study of 168 severe patients. PLoS Pathog. 2020, 16, e1008520. [Google Scholar] [CrossRef]
- Ministry of Health and Population. Health Sector Response to COVID-19; Ministry of Health and Population: Kathmandu, Nepal, 2021.
- COVID-19 CORONAVIRUS Pandemic. Available online: https://www.worldometers.info/coronavirus/ (accessed on 10 November 2023).
- Mininstry of Health and Population Nepal. Coronavirus Disease (COVID-19) Outbreak Updates & Resource Materials—Health Emergency Operation Center; Mininstry of Health and Population Nepal: Kathmandu, Nepal, 2020.
- Diagnostic Detection of 2019-nCoV by Real-Time RT-PCR. Available online: https://www.who.int/docs/default-source/coronaviruse/protocol-v2-1.pdf (accessed on 20 March 2021).
- Feng, Y.; Ling, Y.; Bai, T.; Xie, Y.; Huang, J.; Li, J.; Xiong, W.; Yang, D.; Chen, R.; Lu, F.; et al. COVID-19 with Different Severities: A Multicenter Study of Clinical Features. Am. J. Respir. Crit. Care Med. 2020, 201, 1380–1388. [Google Scholar] [CrossRef]
- Barman, M.P.; Rahman, T.; Bora, K.; Borgohain, C. COVID-19 pandemic and its recovery time of patients in India: A pilot study. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- Benoni, R.; Campagna, I.; Panunzi, S.; Varalta, M.S.; Salandini, G.; De Mattia, G.; Turrina, G.; Moretti, F.; Lo Cascio, G.; Spiteri, G.; et al. Estimating COVID-19 recovery time in a cohort of Italian healthcare workers who underwent surveillance swab testing. Public Health 2021, 196, 52–58. [Google Scholar] [CrossRef] [PubMed]
- George, N.; Tyagi, N.K.; Prasad, J.B. COVID-19 pandemic and its average recovery time in Indian states. Clin. Epidemiol. Glob. Health 2021, 11, 100740. [Google Scholar] [CrossRef]
- Daniels, L.B.; Sitapati, A.M.; Zhang, J.; Zou, J.; Bui, Q.M.; Ren, J.; Longhurst, C.A.; Criqui, M.H.; Messer, K. Relation of Statin Use Prior to Admission to Severity and Recovery Among COVID-19 Inpatients. Am. J. Cardiol. 2020, 136, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Faes, C.; Abrams, S.; Van Beckhoven, D.; Meyfroidt, G.; Vlieghe, E.; Hens, N.; Belgian Collaborative Group on COVID-19 Hospital Surveillance. Time between Symptom Onset, Hospitalisation and Recovery or Death: Statistical Analysis of Belgian COVID-19 Patients. Int. J. Environ. Res. Public Health 2020, 17, 7560. [Google Scholar] [CrossRef]
- Gao, Y.-d.; Ding, M.; Dong, X.; Zhang, J.-j.; Kursat Azkur, A.; Azkur, D.; Gan, H.; Sun, Y.-l.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef] [PubMed]
- Hull, J.H.; Wootten, M.; Moghal, M.; Heron, N.; Martin, R.; Walsted, E.S.; Biswas, A.; Loosemore, M.; Elliott, N.; Ranson, C. Clinical patterns, recovery time and prolonged impact of COVID-19 illness in international athletes: The UK experience. Br. J. Sports Med. 2022, 56, 4–11. [Google Scholar] [CrossRef] [PubMed]
- SeyedAlinaghi, S.; Abbasian, L.; Solduzian, M.; Ayoobi Yazdi, N.; Jafari, F.; Adibimehr, A.; Farahani, A.; Salami Khaneshan, A.; Ebrahimi Alavijeh, P.; Jahani, Z.; et al. Predictors of the prolonged recovery period in COVID-19 patients: A cross-sectional study. Eur. J. Med. Res. 2021, 26, 41. [Google Scholar] [CrossRef]
- Callender, L.A.; Curran, M.; Bates, S.M.; Mairesse, M.; Weigandt, J.; Betts, C.J. The Impact of Pre-existing Comorbidities and Therapeutic Interventions on COVID-19. Front. Immunol. 2020, 11, 1991. [Google Scholar] [CrossRef]
- Meng, L.; Qiu, H.; Wan, L.; Ai, Y.; Xue, Z.; Guo, Q.; Deshpande, R.; Zhang, L.; Meng, J.; Tong, C.; et al. Intubation and Ventilation amid the COVID-19 Outbreak: Wuhan’s Experience. Anesthesiology 2020, 132, 1317–1332. [Google Scholar] [CrossRef]
- Murthy, S.; Gomersall, C.D.; Fowler, R.A. Care for Critically Ill Patients with COVID-19. JAMA 2020, 323, 1499–1500. [Google Scholar] [CrossRef] [PubMed]
- Chivukula, R.R.; Maley, J.H.; Dudzinski, D.M.; Hibbert, K.; Hardin, C.C. Evidence-Based Management of the Critically Ill Adult with SARS-CoV-2 Infection. J. Intensive Care Med. 2021, 36, 18–41. [Google Scholar] [CrossRef]
- Palladino, M. Complete blood count alterations in COVID-19 patients: A narrative review. Biochem. Medica 2021, 31, 030501. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.J.; Qi, G.Q.; Gu, X.; Zhang, X.Y.; Fang, Y.F.; Jiang, H.; Zhao, Y.J. Lymphocyte blood levels that remain low can predict the death of patients with COVID-19. Medicine 2021, 100, e26503. [Google Scholar] [CrossRef] [PubMed]
- Huang, I.; Pranata, R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): Systematic review and meta-analysis. J. Intensive Care 2020, 8, 36. [Google Scholar] [CrossRef]
- Shenoy, N.; Luchtel, R.; Gulani, P. Considerations for target oxygen saturation in COVID-19 patients: Are we under-shooting? BMC Med. 2020, 18, 260. [Google Scholar] [CrossRef] [PubMed]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospitalization and critical illness among 4103 patients with COVID-19 disease in New York City. medRxiv 2020. [Google Scholar] [CrossRef]
- Rodríguez-Molinero, A.; Gálvez-Barrón, C.; Miñarro, A.; Macho, O.; López, G.F.; Robles, M.T.; Dapena, M.D.; Martínez, S.; Milà Ràfols, N.; Monaco, E.E.; et al. Association between COVID-19 prognosis and disease presentation, comorbidities and chronic treatment of hospitalized patients. PLoS ONE 2020, 15, e0239571. [Google Scholar] [CrossRef] [PubMed]
- Ospina-Tascón, G.A.; Calderón-Tapia, L.E.; García, A.F.; Zarama, V.; Gómez-Álvarez, F.; Álvarez-Saa, T.; Pardo-Otálvaro, S.; Bautista-Rincón, D.F.; Vargas, M.P.; Aldana-Díaz, J.L.; et al. Effect of High-Flow Oxygen Therapy vs Conventional Oxygen Therapy on Invasive Mechanical Ventilation and Clinical Recovery in Patients with Severe COVID-19: A Randomized Clinical Trial. JAMA 2021, 326, 2161–2171. [Google Scholar] [CrossRef]
- Eltzschig, H.K.; Carmeliet, P. Hypoxia and Inflammation. N. Engl. J. Med. 2011, 364, 656–665. [Google Scholar] [CrossRef]
- Huang, L.; Li, X.; Gu, X.; Zhang, H.; Ren, L.; Guo, L.; Liu, M.; Wang, Y.; Cui, D.; Wang, Y.; et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: A longitudinal cohort study. Lancet Respir. Med. 2022, 10, 863–876. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ashcroft, T.; Chung, A.; Dighero, I.; Dozier, M.; Horne, M.; McSwiggan, E.; Shamsuddin, A.; Nair, H. Risk factors for poor outcomes in hospitalised COVID-19 patients: A systematic review and meta-analysis. J. Glob. Health 2021, 11, 10001. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Jayasundara, D.; Pye, V.; Dobbins, T.; Dore, G.J.; Matthews, G.; Kaldor, J.; Spokes, P. Whole of population-based cohort study of recovery time from COVID-19 in New South Wales Australia. Lancet Reg. Health-West. Pac. 2021, 12, 100193. [Google Scholar] [CrossRef] [PubMed]



| Variables | All Patients (n = 507) | Patients Who Recovered (n = 251) | Patients Who Died/Referred * (n = 256) | p-Value |
|---|---|---|---|---|
| Age, years | ||||
| Mean (SD) | 51.09 (14.92) | 48.61 (14.99) | 53.52 (14.48) | <0.001 |
| Gender | ||||
| Male | 345 (68.0) | 173 (50.1) | 172 (49.9) | 0.675 |
| Female | 162 (32.0) | 78 (48.1) | 84 (51.9) | |
| Origin of Residence * | ||||
| Dhanusha | 255 (67.1) | 126 (49.4) | 129 (50.6) | 0.713 |
| Mahottari | 76 (20.0) | 36 (47.4) | 40 (52.6) | |
| Sarlahi | 26 (6.8) | 13 (50.0) | 13 (50.0) | |
| Siraha | 17 (4.5) | 6 (35.3) | 11 (64.7) | |
| Bara/Parsa/Rautahat/Saptari | 6 (1.6) | 4 (66.7) | 2 (33.3) | |
| Area of Residence ** | ||||
| Urban | 299 (80.4) | 147 (49.2) | 152 (50.8) | 0.692 |
| Rural | 73 (19.6) | 34 (46.6) | 39 (53.4) | |
| Types of Hospital | ||||
| Public | 285 (56.2) | 149 (52.3) | 136 (47.7) | 0.157 |
| Private | 222 (43.8) | 102 (45.9) | 120 (54.1) | |
| Severity at admission *** | ||||
| Mild | 103 (22.3) | 62 (60.2) | 41 (39.8) | <0.0001 |
| Moderate | 157 (34.0) | 101 (64.3) | 56 (35.7) | |
| Severe | 135 (29.2) | 51 (37.8) | 84 (62.2) | |
| Critical | 67 (14.5) | 13 (19.4) | 54 (80.6) | |
| Respiratory support **** | ||||
| None | 80 (20.0) | 62 (77.5) | 18 (22.5) | <0.0001 |
| Oxygen mask | 260 (64.8) | 136 (52.3) | 124 (47.7) | |
| Mechanical Ventilation | 61 (15.2) | 8 (13.1) | 53 (86.9) |
| Variables | All Patients (n = 507) | Patients Who Recovered (n = 251) | Patients Who Died or Referred * (n = 256) | p-Value |
|---|---|---|---|---|
| Symptoms reported at admission | ||||
| Shortness of breath | 332 (65.5) | 156 (47.0) | 176 (53.0) | 0.233 |
| Fever | 310 (61.1) | 157 (50.6) | 153 (49.4) | 0.680 |
| Cough | 305 (60.2) | 154 (50.5) | 151 (49.5) | 0.603 |
| Fatigue | 56 (11.0) | 27 (48.2) | 29 (51.8) | 0.495 |
| Respiratory distress | 16 (3.2) | 6 (37.5) | 10 (62.5) | 0.221 |
| Headache | 29 (5.7) | 16 (55.2) | 13 (44.8) | 0.888 |
| Pre-existing conditions | ||||
| Diabetes mellitus | 95 (18.7) | 41 (43.2) | 54 (56.8) | 0.256 |
| Hypertension | 54 (10.7) | 27 (50.0) | 27 (50.0) | 0.686 |
| Chronic obstructive pulmonary disease | 14 (2.8) | 7 (50.0) | 7 (50.0) | 0.785 |
| Asthma | 4 (0.8) | 1 (25.0) | 3 (75.0) | 0.343 |
| Chronic cardiac disease ‡ (Excluding hypertension) | 6 (1.2) | 3 (50.0) | 3 (50.0) | 0.839 |
| TB | 4 (0.8) | 2 (50.0) | 2 (50.0) | 0.908 |
| HIV/AIDS | 1 (0.2) | 0 (0.0) | 1 (100.0) | - |
| Thyroid | 16 (3.2) | 9 (56.3) | 7 (43.7) | 0.738 |
| Chronic kidney disease of any stage * | 8 (1.6) | 2 (25.0) | 6 (75.0) | 0.250 |
| Vital signs at hospital presentation | ||||
| Temperature (°F) [n = 328] | 98 (97–99) | 98 (97–99) | 98 (97–99) | 0.017 |
| Oxygen saturation (%) [n = 475] | 94 (88–97) | 95 (92–97) | 90 (80–95) | <0.0001 |
| Heart rate (beats per min) [n = 335] | 88 (80–100) | 86 (80–97) | 89 (80–105) | 0.039 |
| Respiratory rate (breaths per min) [n = 173] | 22 (20–28) | 22 (20–24) | 24 (20–32) | 0.018 |
| Systolic blood pressure (mm Hg) [n = 303] | 110 (110–120) | 110 (110–120) | 110 (100–120) | 0.066 |
| Diastolic blood pressure (mm Hg) [n = 303] | 70 (70–80) | 70 (70–80) | 70 (70–80) | 0.026 |
| Variables | Number | Median Recovery Time | Log Rank χ2-Value | p-Value |
|---|---|---|---|---|
| Point Estimate (95% CI) | ||||
| Age group, years | ||||
| <20 | 10 (2.0) | 9 (6.63–11.36) | 7.11 | 0.212 |
| 20–29 | 30 (5.9) | 9 (6.31–11.68) | ||
| 30–39 | 66 (13.0) | 9 (7.25–10.74) | ||
| 40–49 | 104 (20.5) | 8 (6.88–9.11) | ||
| 50–59 | 127 (25.0) | 9 (7.68–10.31) | ||
| 60–69 | 170 (33.5) | 12 (10.16–13.83) | ||
| Sex | ||||
| Male | 345 (68.0) | 9 (8.11–9.88) | 0.004 | 0.947 |
| Female | 162 (32.0) | 9 (7.07–10.92) | ||
| Origin of Residence | ||||
| Dhanusha | 255 (67.1) | 9 (7.85–10.14) | 2.60 | 0.626 |
| Mahottari | 76 (20.0) | 10 (6.74–13.25) | ||
| Sarlahi | 26 (6.8) | 10 | ||
| Siraha | 17 (4.5) | 18 (10.16–13.83) | ||
| Bara/Parsa/Rautahat/Saptari | 6 (1.6) | 9 (8.03–9.96) | ||
| Missing | 127 | |||
| Area of Residence | ||||
| Urban | 299 (80.4) | 10 (8.89–11.10) | 0.005 | 0.945 |
| Rural | 73 (19.6) | 9 (7.23–10.76) | ||
| Missing | 135 | |||
| Types of Hospital | ||||
| Public | 285 (56.2) | 9 (8.05–9.95) | 6.60 | 0.010 |
| Private | 222 (43.8) | 10 (8.78–11.21) | ||
| Severity at admission | ||||
| Mild | 103 (22.3) | 7 (5.18–8.81) | 39.42 | <0.0001 |
| Moderate | 157 (34.0) | 9 (7.78–10.22) | ||
| Severe | 135 (29.2) | 10 (8.59–11.40) | ||
| Critical | 67 (14.5) | 18 (11.96–24.03) | ||
| Missing | 45 | |||
| Respiratory support | ||||
| None | 80 (20.0) | 5 (4.08–5.91) | 90.16 | <0.0001 |
| Oxygen mask | 260 (64.8) | 10 (8.98–11.01) | ||
| Mechanical Ventilation | 61 (15.2) | 22 (9.13–34.86) | ||
| Missing | 106 |
| Variables | Number | Median Recovery Time | Log Rank χ2-Value | p-Value |
|---|---|---|---|---|
| Point Estimate (95% CI) | ||||
| Fever | ||||
| Presence | 310 | 9 (7.93–10.06) | 0.213 | 0.644 |
| Absence | 123 | 9 (7.65–10.34) | ||
| Missing | ||||
| Cough | ||||
| Presence | 305 | 9 (7.84–10.15) | 0.001 | 0.975 |
| Absence | 122 | 9 (7.66–10.33) | ||
| Missing | ||||
| Fatigue | ||||
| Presence | 56 | 10 (7.35–12.64) | 0.700 | 0.403 |
| Absence | 121 | 9 (7.95–10.05) | ||
| Missing | ||||
| Shortness of breath | ||||
| Presence | 332 | 10 (8.66–11.33) | 0.566 | 0.452 |
| Absence | 120 | 9 (7.95–10.04) | ||
| Missing | ||||
| Respiratory distress | ||||
| Presence | 16 | 10 (7.21–12.78) | 0447 | 0.504 |
| Absence | 119 | 9 (7.95–10.04) | ||
| Missing | ||||
| Headache | ||||
| Presence | 29 | 9 (7.95–10.05) | 0318 | 0.573 |
| Absence | 121 | 8 (5.08–10.91) | ||
| Missing | ||||
| Pre-existing conditions | ||||
| Diabetes mellitus | ||||
| Presence | 95 | 11 (8.07–13.92) | 5.00 | 0.025 |
| Absence | 93 | 9 (7.57–10.42) | ||
| Missing | ||||
| Hypertension | ||||
| Presence | 54 | 11 (8.13–13.86) | 0.137 | 0.712 |
| Absence | 103 | 9 (7.44–10.55) | ||
| Missing | ||||
| Chronic obstructive pulmonary disease | ||||
| Presence | 14 | 12 (10.85–13.14) | 1.81 | 0.178 |
| Absence | 117 | 9 (7.66–10.33) | ||
| Missing | ||||
| Asthma | ||||
| Presence | 4 | 9 (7.95–10.05) | 0.105 | 0.746 |
| Absence | 212 | 9 | ||
| Missing | ||||
| Chronic cardiac disease (excluding hypertension) | ||||
| Presence | 6 | 7 (0.01–15.58) | 0.429 | 0.512 |
| Absence | 118 | 9 (7.95–10.04) | ||
| Missing | ||||
| Tuberculosis | ||||
| Presence | 4 | 5 (7.69–10.30) | 0.175 | 0.676 |
| Absence | 119 | 9 | ||
| Missing | ||||
| HIV/AIDS | ||||
| Presence | 1 | - | - | - |
| Absence | 121 | - | ||
| Missing | ||||
| Thyroid | ||||
| Presence | 16 | 8 (3.69–12.31) | 1.69 | 0.193 |
| Absence | 112 | 9 (7.61–10.38) | ||
| Missing | ||||
| Chronic kidney disease of any stage | ||||
| Presence | 8 | 11 | 0.075 | 0.784 |
| Absence | 120 | 9 (7.63–10.06) |
| Variables | Univariable HR (95% CI) | Multivariable HR (95% CI) | ||||
|---|---|---|---|---|---|---|
| Model-I | Model-II | |||||
| CHR (95% CI) | p-Value | AHR (95% CI) | p-Value | AHR (95% CI) | p-Value | |
| Age (per 10-year increase) | 0.90 (0.83–0.98) | 0.023 | 0.87 (0.78–0.96) | 0.006 | 0.88 (0.75–1.04) | 0.887 |
| Types of Hospital | ||||||
| Private | Reference | - | Reference | - | Reference | - |
| Public | 1.37 (1.06–1.77) | 0.014 | 1.05 (0.77–1.44) | 0.717 | 3.01 (0.30–29.86) | 0.345 |
| Severity at admission | ||||||
| Mild | Reference | - | Reference | - | Reference | - |
| Moderate | 0.70 (0.51–0.97) | 0.032 | 0.54 (0.37–0.80) | 0.002 | 0.62 (0.23–1.67) | 0.352 |
| Severe/critical | 0.37 (0.26–0.52) | <0.0001 | 0.46 (0.29–0.71) | 0.001 | 0.34 (0.15–0.79) | 0.012 |
| Respiratory support | ||||||
| None | Reference | - | Reference | - | Reference | - |
| Oxygen mask | 0.30 (0.22–0.41) | <0.0001 | 0.34 (0.24–0.48) | <0.0001 | 0.76 (0.35–1.63) | 0.481 |
| Mechanical Ventilation | 0.10 (0.04–0.21) | <0.0001 | 0.11 (0.05–0.25) | <0.0001 | 0.26 (0.05–1.28) | 0.098 |
| Vital signs at hospital presentation | ||||||
| Oxygen saturation (%) | 1.05 (1.03–1.07) | <0.0001 | - | - | 1.09 (1.01–1.17) | 0.018 |
| Temperature (°F) | 0.90 (0.76–1.07) | 0.240 | - | - | 0.96 (0.71–1.29) | 0.810 |
| Heart rate (beats per min) | 0.98 (0.97–0.99) | 0.015 | - | - | 0.99 (0.97–1.01) | 0.547 |
| Respiratory rate (breaths per min) | 0.94 (0.90–0.99) | 0.031 | - | - | 1.02 (0.95–1.09) | 0.536 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, J.K.; Acharya, D.; Gautam, S.; Neupane, D.; Bajgain, B.B.; Mishra, R.; Yadav, B.K.; Chhetri, P.; Lee, K.; Shah, A. COVID-19 Recovery Time and Its Predictors among Hospitalized Patients in Designated Hospitals in the Madhesh Province of Nepal: A Multicentric Study. Healthcare 2024, 12, 1691. https://doi.org/10.3390/healthcare12171691
Singh JK, Acharya D, Gautam S, Neupane D, Bajgain BB, Mishra R, Yadav BK, Chhetri P, Lee K, Shah A. COVID-19 Recovery Time and Its Predictors among Hospitalized Patients in Designated Hospitals in the Madhesh Province of Nepal: A Multicentric Study. Healthcare. 2024; 12(17):1691. https://doi.org/10.3390/healthcare12171691
Chicago/Turabian StyleSingh, Jitendra Kumar, Dilaram Acharya, Salila Gautam, Dinesh Neupane, Bishnu Bahadur Bajgain, Raman Mishra, Binod Kumar Yadav, Pradip Chhetri, Kwan Lee, and Ankur Shah. 2024. "COVID-19 Recovery Time and Its Predictors among Hospitalized Patients in Designated Hospitals in the Madhesh Province of Nepal: A Multicentric Study" Healthcare 12, no. 17: 1691. https://doi.org/10.3390/healthcare12171691
APA StyleSingh, J. K., Acharya, D., Gautam, S., Neupane, D., Bajgain, B. B., Mishra, R., Yadav, B. K., Chhetri, P., Lee, K., & Shah, A. (2024). COVID-19 Recovery Time and Its Predictors among Hospitalized Patients in Designated Hospitals in the Madhesh Province of Nepal: A Multicentric Study. Healthcare, 12(17), 1691. https://doi.org/10.3390/healthcare12171691






