Group-Based Trajectory Modeling of N-Terminal Pro-Brain Natriuretic Peptide Levels in Pulmonary Artery Hypertension Associated with Connective Tissue Disease
Abstract
1. Introduction
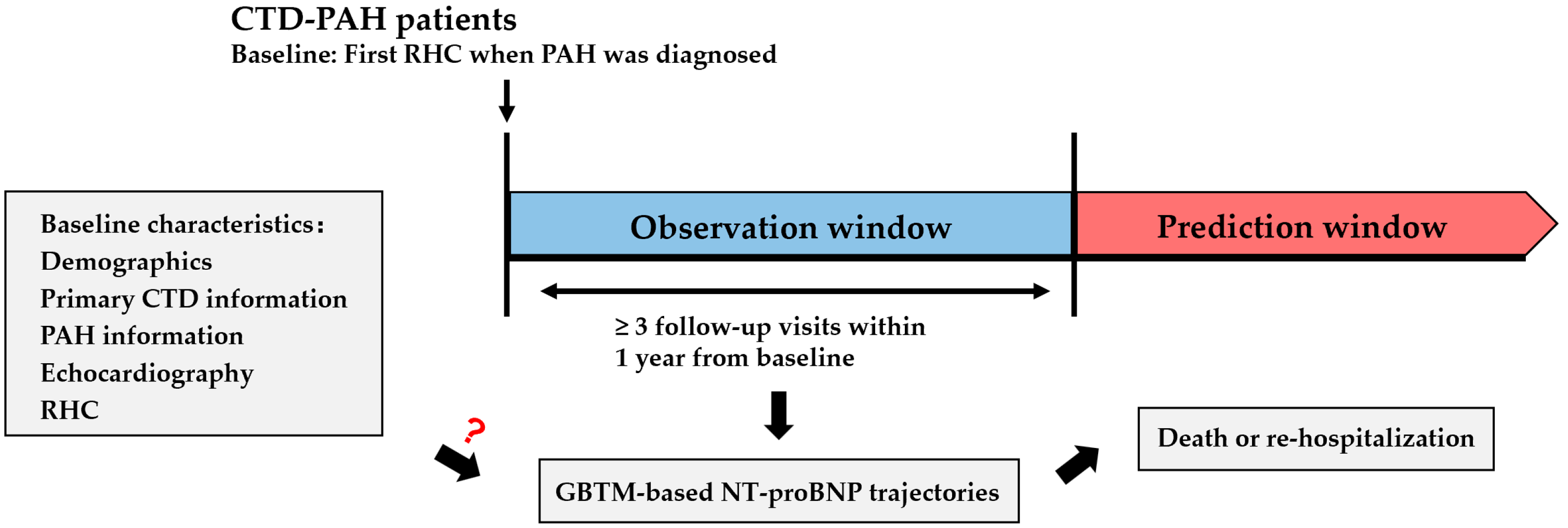
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Latent Trajectory Modeling
2.4. Statistics
3. Results
3.1. Patient Characteristics
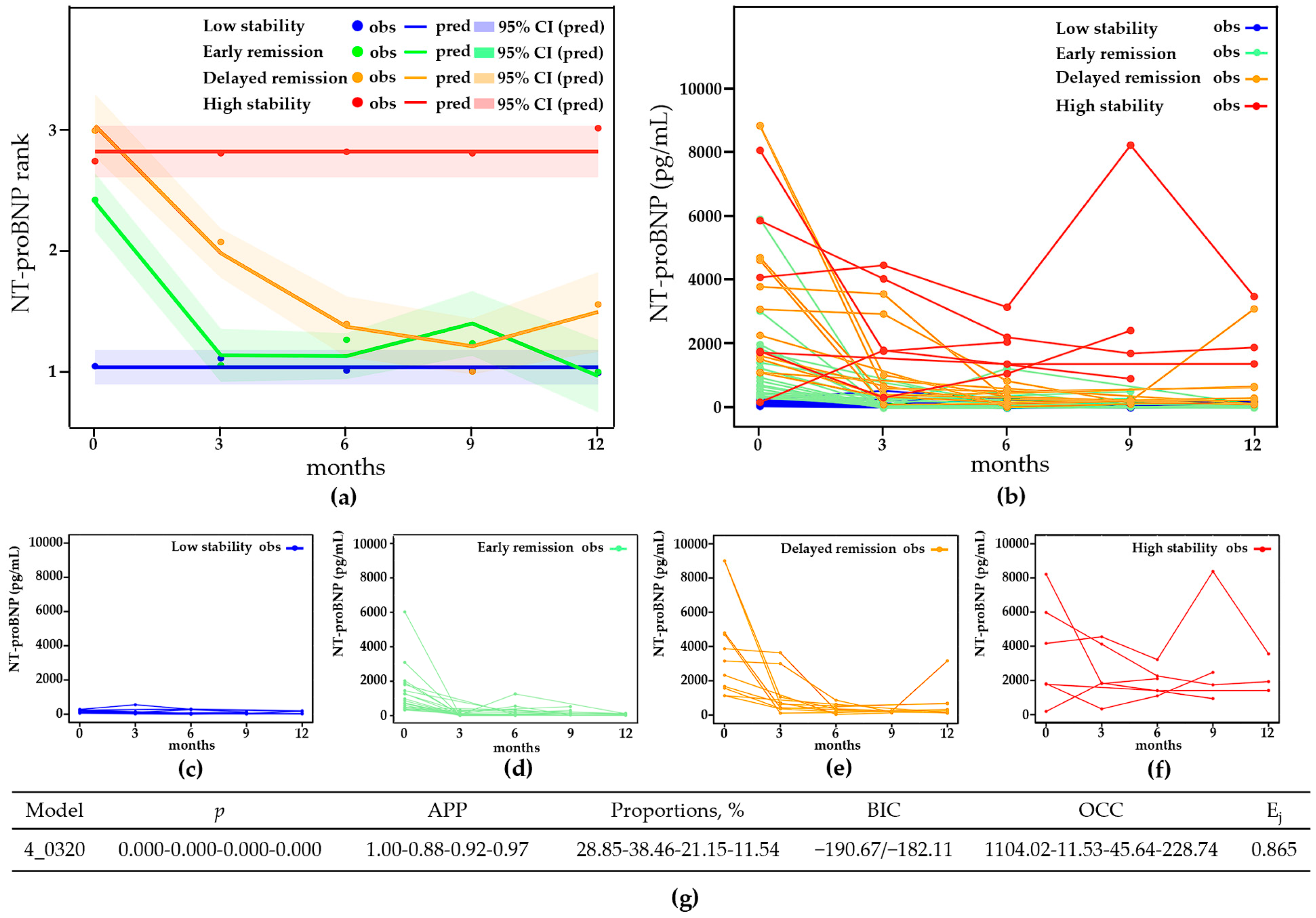
3.2. NT-proBNP Trajectories
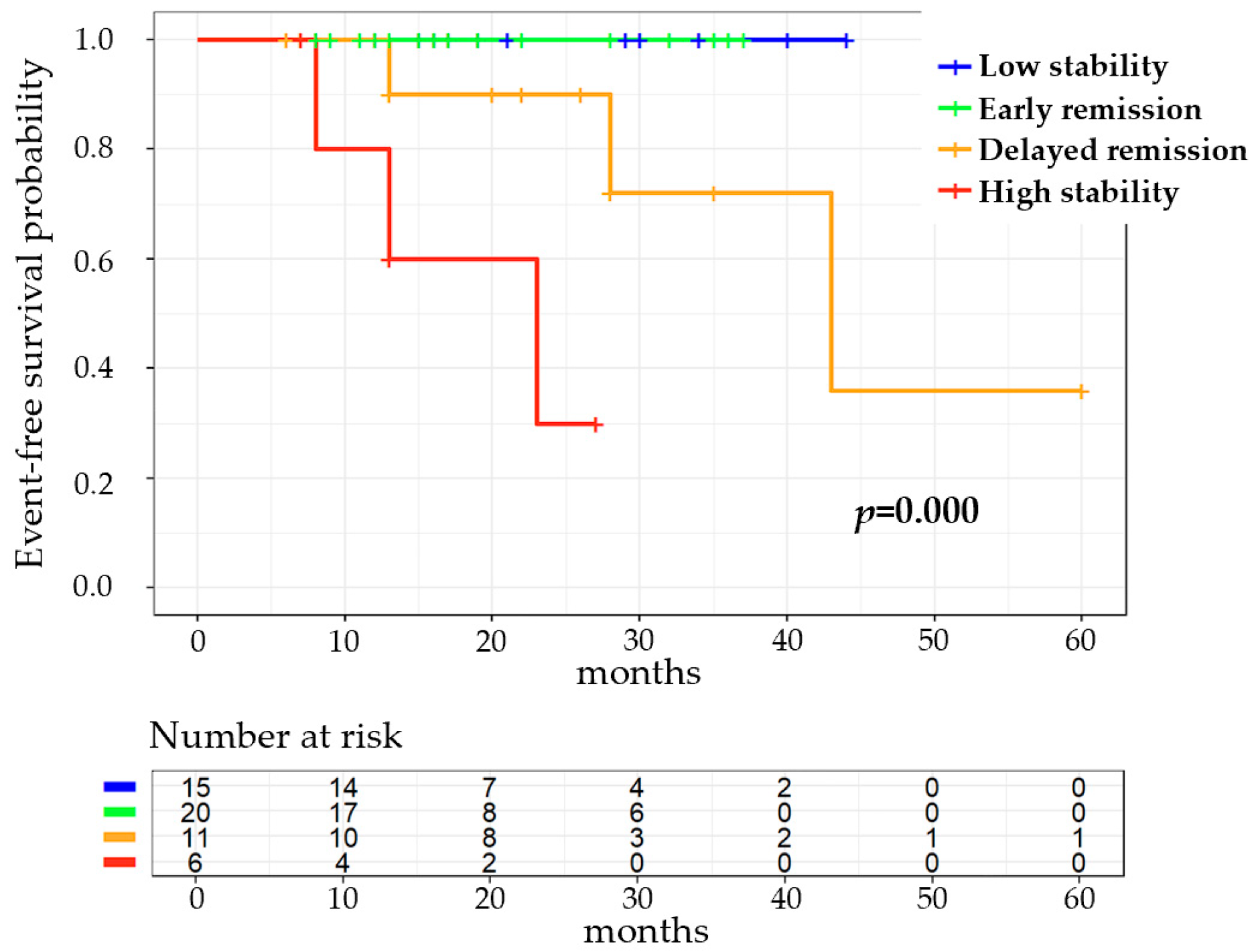
3.3. Association between NT-proBNP Trajectories and Prognosis
3.4. Effects of Baseline Clinical Characteristics on NT-proBNP Trajectories
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kovacs, G.; Berghold, A.; Scheidl, S.; Olschewski, H. Pulmonary arterial pressure during rest and exercise in healthy subjects: A systematic review. Eur. Respir. J. 2009, 34, 888–894. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Kovacs, G.; Hoeper, M.M.; Badagliacca, R.; Berger, R.M.F.; Brida, M.; Carlsen, J.; Coats, A.J.S.; Escribano-Subias, P.; Ferrari, P.; et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur. Respir. J. 2023, 61, 3618–3731. [Google Scholar] [CrossRef] [PubMed]
- Thoreau, B.; Mouthon, L. Pulmonary arterial hypertension associated with connective tissue diseases (CTD-PAH): Recent and advanced data. Autoimmun. Rev. 2023, 23, 103506. [Google Scholar] [CrossRef]
- Lau, E.M.T.; Giannoulatou, E.; Celermajer, D.S.; Humbert, M. Epidemiology and treatment of pulmonary arterial hypertension. Nat. Rev. Cardiol. 2017, 14, 603–614. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Channick, R.N.; Frantz, R.P.; Grünig, E.; Jing, Z.C.; Moiseeva, O.; Preston, I.R.; Pulido, T.; Safdar, Z.; Tamura, Y.; et al. Risk stratification and medical therapy of pulmonary arterial hypertension. Eur. Respir. J. 2019, 53, 1801889. [Google Scholar] [CrossRef]
- Benza, R.L.; Gomberg-Maitland, M.; Elliott, C.G.; Farber, H.W.; Foreman, A.J.; Frost, A.E.; McGoon, M.D.; Pasta, D.J.; Selej, M.; Burger, C.D.; et al. Predicting Survival in Patients with Pulmonary Arterial Hypertension: The REVEAL Risk Score Calculator 2.0 and Comparison With ESC/ERS-Based Risk Assessment Strategies. Chest 2019, 156, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Benza, R.L.; Kanwar, M.K.; Raina, A.; Scott, J.V.; Zhao, C.L.; Selej, M.; Elliott, C.G.; Farber, H.W. Development and Validation of an Abridged Version of the REVEAL 2.0 Risk Score Calculator, REVEAL Lite 2, for Use in Patients with Pulmonary Arterial Hypertension. Chest 2021, 159, 337–346. [Google Scholar] [CrossRef]
- Nagin, D.S.; Jones, B.L.; Elmer, J. Recent Advances in Group-Based Trajectory Modeling for Clinical Research. Annu. Rev. Clin. Psychol. 2024, 20, 285–305. [Google Scholar] [CrossRef]
- Nagin, D.S.; Odgers, C.L. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 2010, 6, 109–138. [Google Scholar] [CrossRef]
- Aringer, M.; Costenbader, K.; Daikh, D.; Brinks, R.; Mosca, M.; Ramsey-Goldman, R.; Smolen, J.S.; Wofsy, D.; Boumpas, D.T.; Kamen, D.L.; et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann. Rheum. Dis. 2019, 78, 1151–1159. [Google Scholar] [CrossRef]
- Vitali, C.; Bombardieri, S.; Jonsson, R.; Moutsopoulos, H.M.; Alexander, E.L.; Carsons, S.E.; Daniels, T.E.; Fox, P.C.; Fox, R.I.; Kassan, S.S.; et al. Classification criteria for Sjögren’s syndrome: A revised version of the European criteria proposed by the American-European Consensus Group. Ann. Rheum. Dis. 2002, 61, 554–558. [Google Scholar] [CrossRef] [PubMed]
- van den Hoogen, F.; Khanna, D.; Fransen, J.; Johnson, S.R.; Baron, M.; Tyndall, A.; Matucci-Cerinic, M.; Naden, R.P.; Medsger, T.A., Jr.; Carreira, P.E.; et al. 2013 classification criteria for systemic sclerosis: An American college of rheumatology/European league against rheumatism collaborative initiative. Ann. Rheum. Dis. 2013, 72, 1747–1755. [Google Scholar] [CrossRef]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann. Rheum. Dis. 2010, 69, 1580–1588. [Google Scholar] [CrossRef] [PubMed]
- Sharp, G.C.; Irvin, W.S.; Tan, E.M.; Gould, R.G.; Holman, H.R. Mixed connective tissue disease—An apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am. J. Med. 1972, 52, 148–159. [Google Scholar] [CrossRef]
- Bombardier, C.; Gladman, D.D.; Urowitz, M.B.; Caron, D.; Chang, C.H. Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum. 1992, 35, 630–640. [Google Scholar] [CrossRef] [PubMed]
- Seror, R.; Bootsma, H.; Saraux, A.; Bowman, S.J.; Theander, E.; Brun, J.G.; Baron, G.; Le Guern, V.; Devauchelle-Pensec, V.; Ramos-Casals, M.; et al. Defining disease activity states and clinically meaningful improvement in primary Sjögren’s syndrome with EULAR primary Sjögren’s syndrome disease activity (ESSDAI) and patient-reported indexes (ESSPRI). Ann. Rheum. Dis. 2016, 75, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Medsger, T.A., Jr.; Silman, A.J.; Steen, V.D.; Black, C.M.; Akesson, A.; Bacon, P.A.; Harris, C.A.; Jablonska, S.; Jayson, M.I.; Jimenez, S.A.; et al. A disease severity scale for systemic sclerosis: Development and testing. J. Rheumatol. 1999, 26, 2159–2167. [Google Scholar] [PubMed]
- Anderson, J.; Caplan, L.; Yazdany, J.; Robbins, M.L.; Neogi, T.; Michaud, K.; Saag, K.G.; O’Dell, J.R.; Kazi, S. Rheumatoid arthritis disease activity measures: American College of Rheumatology recommendations for use in clinical practice. Arthritis Care Res. 2012, 64, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. Ser. B 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Kylhammar, D.; Kjellström, B.; Hjalmarsson, C.; Jansson, K.; Nisell, M.; Söderberg, S.; Wikström, G.; Rådegran, G. A comprehensive risk stratification at early follow-up determines prognosis in pulmonary arterial hypertension. Eur. Heart J. 2018, 39, 4175–4181. [Google Scholar] [CrossRef]
- Qian, J.; Li, M.; Zhang, X.; Wang, Q.; Zhao, J.; Tian, Z.; Wei, W.; Zuo, X.; Zhang, M.; Zhu, P.; et al. Long-term prognosis of patients with systemic lupus erythematosus-associated pulmonary arterial hypertension: CSTAR-PAH cohort study. Eur. Respir. J. 2019, 53, 1800081. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Qian, J.; Zhang, S.; Xu, D.; Leng, X.; Zhao, J.; Wang, Q.; Zhang, W.; Tian, X.; Li, M.; et al. Immunosuppressive therapy in patients with connective tissue disease-associated pulmonary arterial hypertension: A systematic review. Int. J. Rheum. Dis. 2022, 25, 982–990. [Google Scholar] [CrossRef] [PubMed]
| Baseline Clinical Characteristics | NT-proBNP Trajectories | p | |
|---|---|---|---|
| Early Remission (n = 20) | Delayed Remission and High Stability (n = 17) | ||
| Age, years | 34.00 (25.00, 45.00) | 48.00 (36.50, 57.50) | 0.006 |
| Primary CTD | 0.120 | ||
| SLE, n (%) | 8 (40.00) | 6 (35.30) | |
| pSS, n (%) | 5 (25.00) | 4 (23.53) | |
| SSc, n (%) | 0 (0.00) | 5 (29.41) | |
| RA, n (%) | 1 (5.00) | 0 (0.00) | |
| MCTD, n (%) | 2 (10.00) | 1 (5.88) | |
| UCTD, n (%) | 4 (20.00) | 1 (5.88) | |
| CTD duration, years | 0.00 (0.00, 0.00) | 2.00 (0.00, 7.50) | 0.024 |
| Active CTD, n (%) | 11 (55.00) | 6 (35.29) | 0.231 |
| Intensive CTD immunotherapy, n (%) | 19 (95.00) | 9 (52.94) | 0.005 |
| PAH duration, years | 0.00 (0.00, 1.00) | 1.00 (0.00, 2.00) | 0.242 |
| WSPH groups | 0.033 | ||
| Low risk, n (%) | 5 (25.00) | 1 (5.88) | |
| Intermediate risk, n (%) | 13 (65.00) | 8 (47.06) | |
| High risk, n (%) | 2 (10.00) | 8 (47.06) | |
| 6MWD, m | 458.50 (392.75, 538.75) | 368.00 (227.00, 443.50) | 0.004 |
| WHO-FC | 0.023 | ||
| I, n (%) | 1 (5.00) | 0 (0.00) | |
| II, n (%) | 10 (50.00) | 3 (17.65) | |
| III, n (%) | 9 (45.00) | 11 (64.71) | |
| IV, n (%) | 0 (0.00) | 3 (17.65) | |
| RAD, mm | 40.00 (38.25, 44.75) | 46.00 (41.50, 51.00) | 0.010 |
| RVDd, mm | 41.80 ± 4.07 | 46.12 ± 5.78 | 0.012 |
| TRV, cm/s | 401.00 ± 72.25 | 424.29 ± 62.73 | 0.307 |
| TAPSE/PASP ratio | 0.27 ± 0.12 | 0.20 ± 0.09 | 0.061 |
| Pericardial effusion, n (%) | 7 (35.00) | 13 (76.47) | 0.012 |
| mPAP, mmHg | 41.00 (34.25, 57.75) | 49.00 (39.50, 62.00) | 0.131 |
| SVO2, % | 63.50 (59.25, 67.75) | 57.00 (46.00, 70.50) | 0.293 |
| mRAP, mmHg | 5.50 (3.00, 9.00) | 7.00 (4.50, 9.00) | 0.340 |
| PAWP, mmHg | 8.20 ± 3.02 | 9.12 ± 3.08 | 0.368 |
| mRVP, mmHg | 22.50 (19.50, 34.75) | 28.00 (24.50, 37.00) | 0.184 |
| PVR, Wood | 8.20 (5.55, 13.13) | 10.63 (6.63, 21.88) | 0.170 |
| Cardiac index, L/min/m2 | 2.72 ± 0.75 | 2.51 ± 0.89 | 0.424 |
| PAH-targeted drug therapy | 0.439 | ||
| ERA, n (%) | 0 (0.00) | 0 (0.00) | |
| PDE5i, n (%) | 0 (0.00) | 1 (5.88) | |
| ERA + PDE5i, n (%) | 12 (60.00) | 10 (58.82) | |
| ERA + PRA, n (%) | 0 (0.00) | 1 (5.88) | |
| PDE5i + PRA, n (%) | 0 (0.00) | 0 (0.00) | |
| ERA + PDE5i + PRA, n (%) | 8 (40.00) | 5 (29.41) | |
| Baseline Clinical Characteristics | LASSO Regression Coefficient | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|---|
| p | OR (95% CI) | p | OR (95% CI) | ||
| Age | 0.014 | 0.015 | 1.080 (1.015–1.149) | 0.061 | 1.106 (0.995–1.229) |
| Primary CTD | >0.05 | ||||
| CTD duration | 0.259 | 1.062 (0.957–1.179) | |||
| Active CTD | 0.234 | 0.446 (0.118–1.685) | |||
| Intensive CTD immunotherapy | −0.718 | 0.013 | 0.059 (0.006–0.548) | 0.048 | 0.027 (0.001–0.963) |
| PAH duration | 0.893 | 0.985 (0.787–1.232) | |||
| 6MWD rank | 0.024 | 2.679 (1.136–6.319) | |||
| WHO-FC | 0.307 | 0.013 | 5.689 (1.448–22.348) | 0.077 | 7.710 (0.799–74.377) |
| RAD | 0.023 | 1.176 (1.022–1.353) | |||
| RVDd | 0.029 | 0.020 | 1.203 (1.029–1.406) | 0.205 | 1.171 (0.918–1.494) |
| TRV | 0.299 | 1.005 (0.995–1.015) | |||
| TAPSE/PASP ratio rank | 0.056 | 2.402 (0.976–5.908) | |||
| Pericardial effusion | 0.319 | 0.015 | 6.036 (1.417–25.710) | 0.054 | 15.887 (0.955–264.229) |
| mPAP | 0.139 | 1.035 (0.989–1.084) | |||
| SVO2 | 0.110 | 0.946 (0.885–1.013) | |||
| mRAP | 0.489 | 1.069 (0.884–1.294) | |||
| PAWP | 0.358 | 1.109 (0.889–1.383) | |||
| mRVP | 0.573 | 1.019 (0.954–1.088) | |||
| PVR | 0.119 | 1.074 (0.982–1.176) | |||
| Cardiac index | 0.413 | 0.709 (0.311–1.616) | |||
| PAH-targeted drug therapy | >0.05 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, H.; Lu, F.; Huang, Y.; Wang, Q.; Sun, X.; Zhang, M.; Zhou, L. Group-Based Trajectory Modeling of N-Terminal Pro-Brain Natriuretic Peptide Levels in Pulmonary Artery Hypertension Associated with Connective Tissue Disease. Healthcare 2024, 12, 1633. https://doi.org/10.3390/healthcare12161633
Tang H, Lu F, Huang Y, Wang Q, Sun X, Zhang M, Zhou L. Group-Based Trajectory Modeling of N-Terminal Pro-Brain Natriuretic Peptide Levels in Pulmonary Artery Hypertension Associated with Connective Tissue Disease. Healthcare. 2024; 12(16):1633. https://doi.org/10.3390/healthcare12161633
Chicago/Turabian StyleTang, Heng, Fengyun Lu, Yingheng Huang, Qiang Wang, Xiaoxuan Sun, Miaojia Zhang, and Lei Zhou. 2024. "Group-Based Trajectory Modeling of N-Terminal Pro-Brain Natriuretic Peptide Levels in Pulmonary Artery Hypertension Associated with Connective Tissue Disease" Healthcare 12, no. 16: 1633. https://doi.org/10.3390/healthcare12161633
APA StyleTang, H., Lu, F., Huang, Y., Wang, Q., Sun, X., Zhang, M., & Zhou, L. (2024). Group-Based Trajectory Modeling of N-Terminal Pro-Brain Natriuretic Peptide Levels in Pulmonary Artery Hypertension Associated with Connective Tissue Disease. Healthcare, 12(16), 1633. https://doi.org/10.3390/healthcare12161633






