Motivational Barriers and Facilitators for Older Adults’ Engagement in Exercise during Depressive Episodes: A Network Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Database Search and Identification
2.2. Inclusion and Exclusion Criteria
2.3. Model Construction for Network Meta-Analysis
2.4. Risk of Bias Assessment
2.5. Primary Outcome: Improvement of Depression in the Older Adults
2.6. Secondary Outcome: Differences in Dropout Rates
2.7. Data Extraction, Handling, and Transformation
2.8. Statistical Analysis
2.9. Sensitivity Analysis Methods
2.10. Publication Bias
3. Results
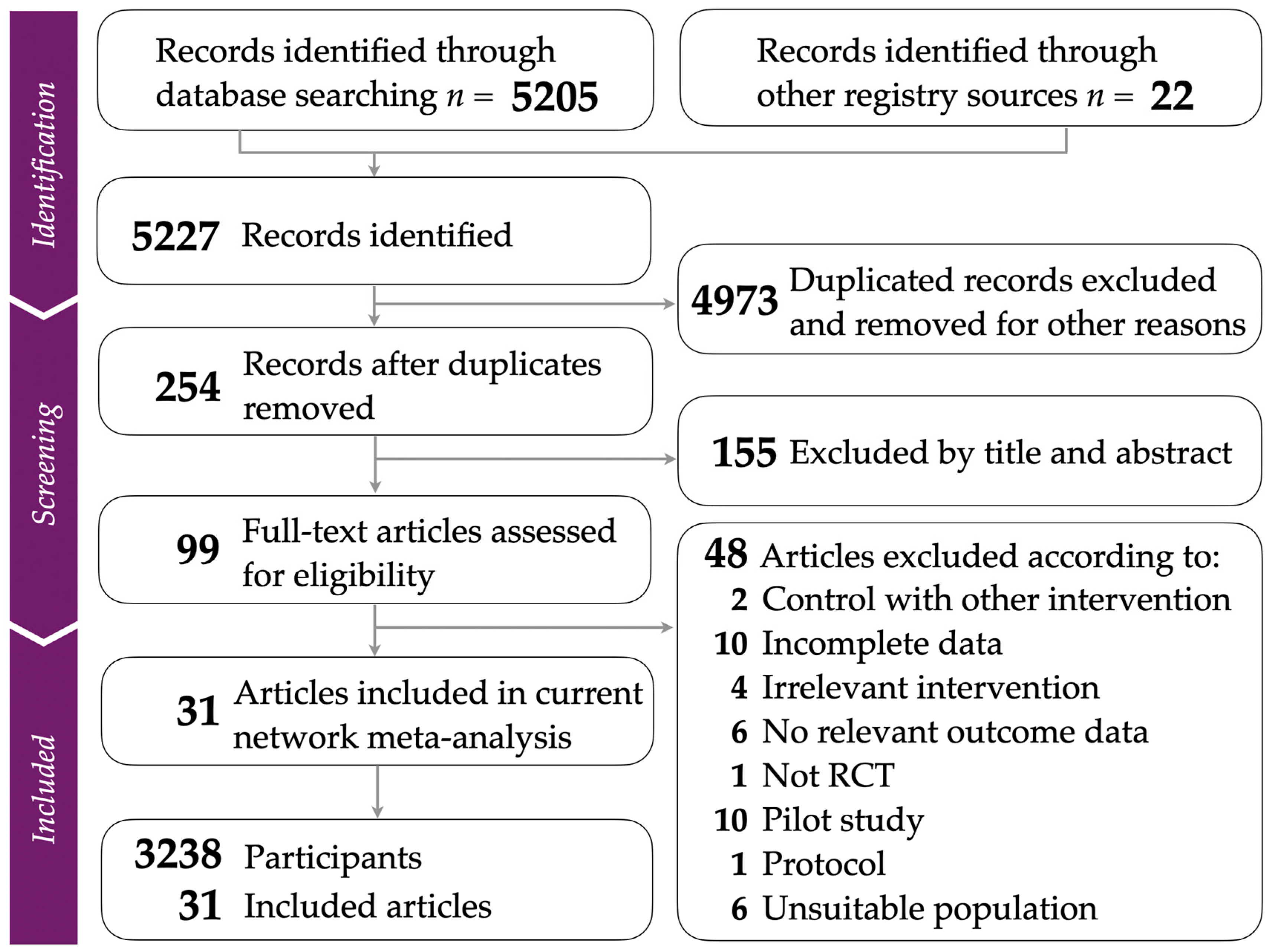
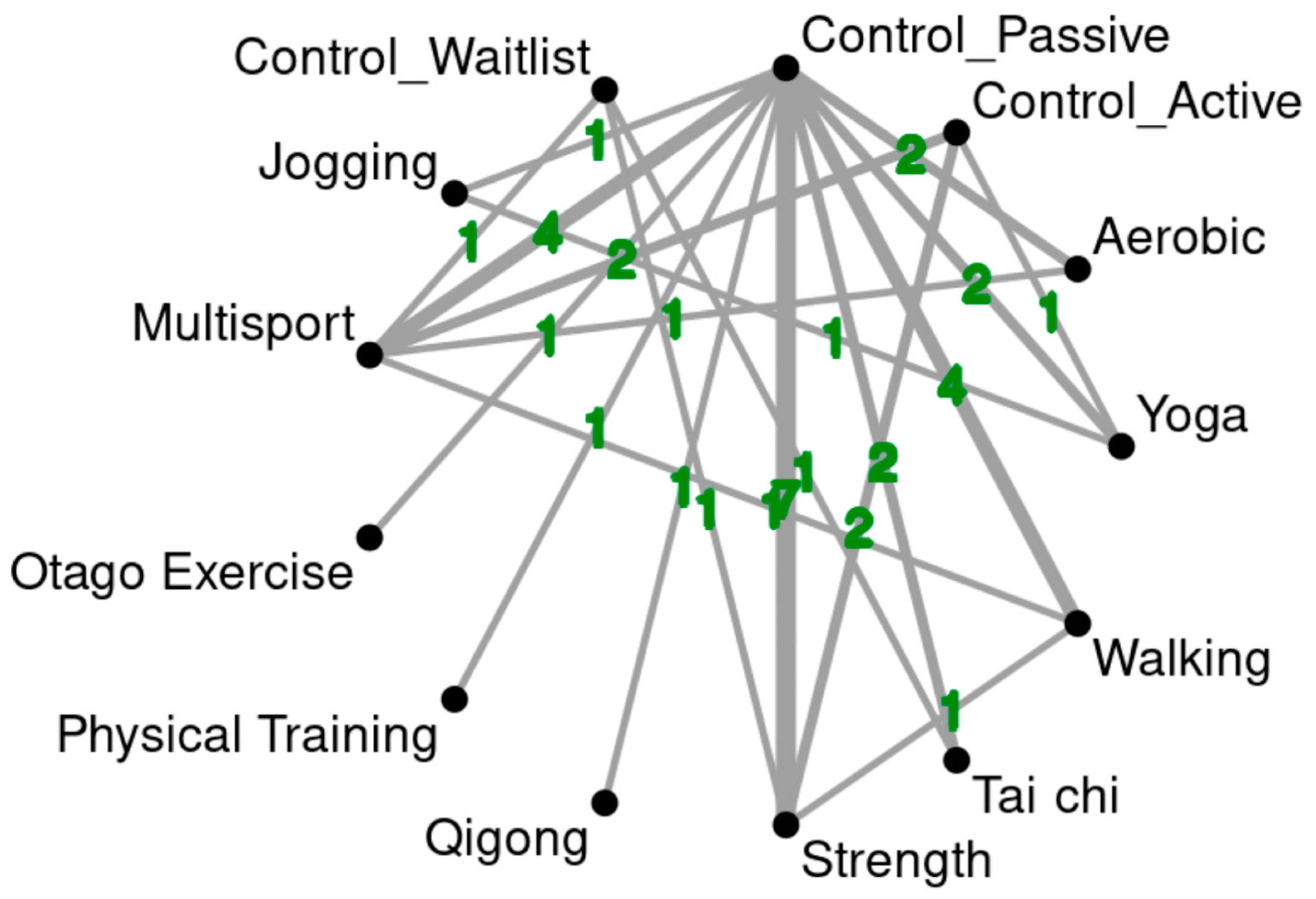
3.1. Study Identification and Network Model Construction
3.2. Studies’ Quality and Risk of Bias Assessment
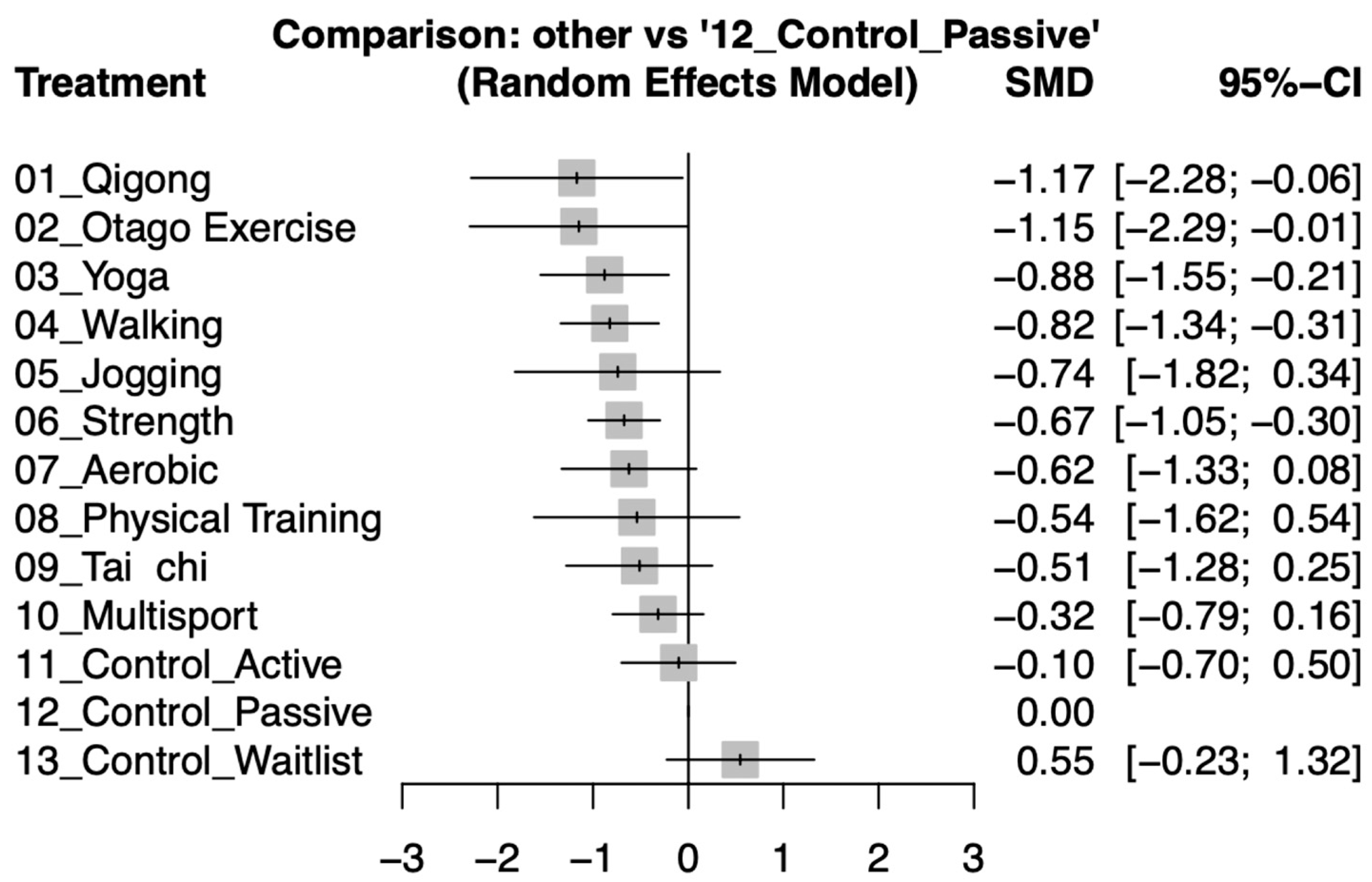
3.3. Main Outcome: Effective Exercise Interventions for Alleviating Depression in Older Adults
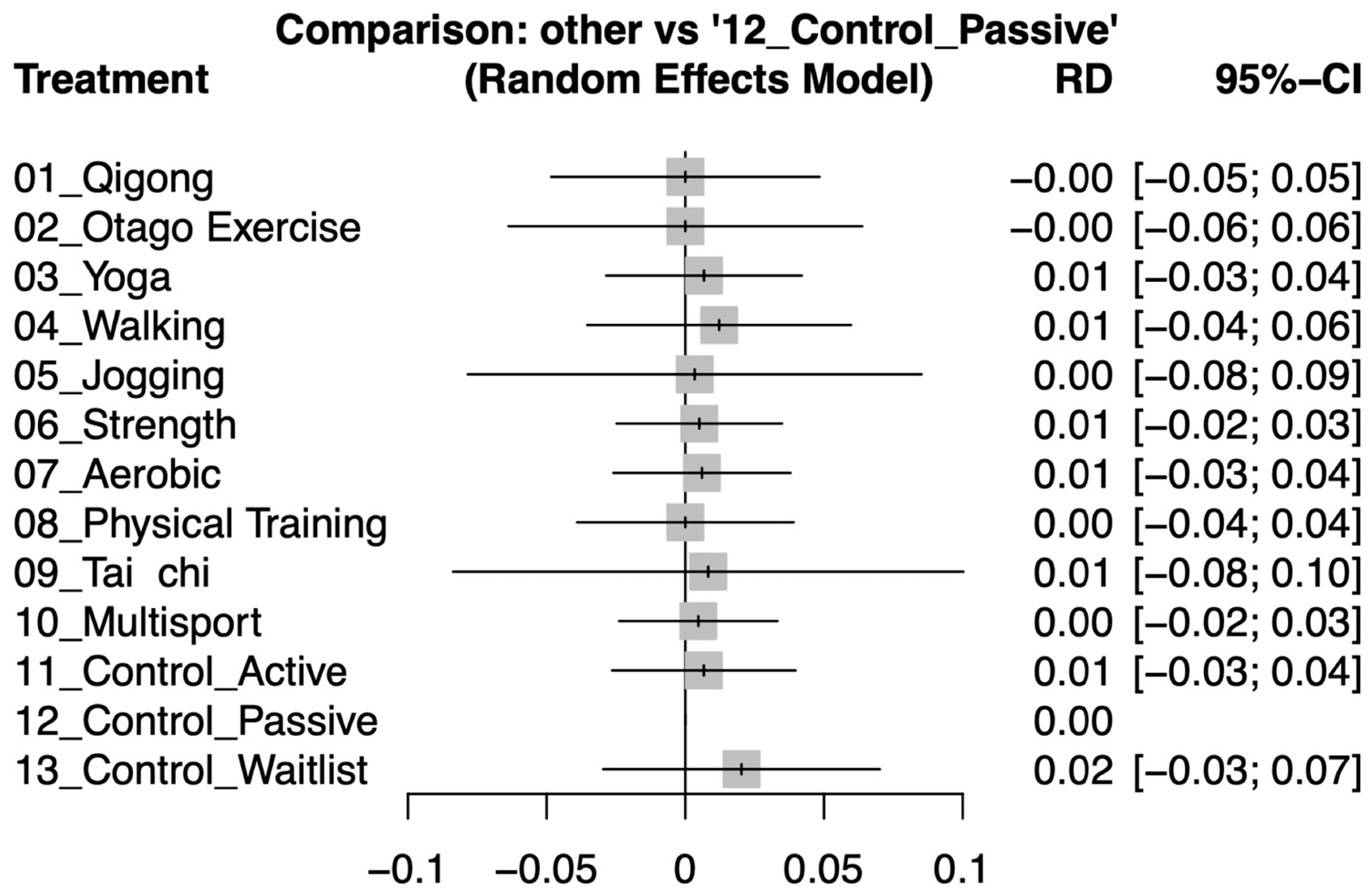
3.4. Secondary Outcome: Differences in Dropout Rates
3.5. Inconsistency Testing
3.6. Sensitivity Analysis
3.7. Publication Bias
4. Discussion
4.1. Main Findings and Clinical Significance
4.2. Significance of Results in the Context of Current Research
4.3. Possible Explanations for the Observed Results
4.4. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Depressive Disorder (Depression); Retrieved from Depressive Disorder (Depression) (Who. Int); World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Tu, C.Y.; Liao, S.C.; Wu, C.S.; Chiu, Y.T.; Huang, W.L. Association of categorical diagnoses and psychopathologies with quality of life in patients with depression, anxiety, and somatic symptoms: A cross-sectional study. J. Psychosom. Res. 2024, 182, 111691. [Google Scholar] [CrossRef] [PubMed]
- Marawi, T.; Zhukovsky, P.; Brooks, H.; Bowie, C.R.; Butters, M.A.; Fischer, C.E.; Flint, A.J.; Herrmann, N.; Lanctôt, K.L.; Mah, L.; et al. Heterogeneity of Cognition in Older Adults with Remitted Major Depressive Disorder: A Latent Profile Analysis. Am. J. Geriatr. Psychiatry 2024, 32, 867–878. [Google Scholar] [CrossRef] [PubMed]
- Invernizzi, S.; Simoes Loureiro, I.; Kandana Arachchige, K.G.; Lefebvre, L. Late-Life Depression, Cognitive Impairment, and Relationship with Alzheimer’s Disease. Dement. Geriatr. Cogn. Disord. 2021, 50, 414–424. [Google Scholar] [CrossRef] [PubMed]
- Patrick, R.E.; Dickinson, R.A.; Gentry, M.T.; Kim, J.U.; Oberlin, L.E.; Park, S.; Principe, J.L.; Teixeira, A.L.; Weisenbach, S.L. Treatment resistant late-life depression: A narrative review of psychosocial risk factors, non-pharmacological interventions, and the role of clinical phenotyping. J. Affect. Disord. 2024, 356, 145–154. [Google Scholar] [CrossRef]
- Weng, W.H.; Wang, Y.H.; Yeh, N.C.; Yang, Y.R.; Wang, R.Y. Effects of physical training on depression and related quality of life in pre-frail and frail older adults: A systematic review and meta-analysis. J. Nutr. Health Aging 2024, 28, 100237. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, X. The effects of physical activity and exercise therapy on frail elderly depression: A narrative review. Medicine 2023, 102, e34908. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, M.; Merchant, R.; Morley, J.; Anker, S.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.; Cesari, M. International exercise recommendations in older adults (ICFSR): Expert consensus guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef]
- Huang, J.; Wang, D.; Wang, J. Clinical evidence of tai chi exercise prescriptions: A systematic review. Evid. Based Complement. Altern. Med. 2021, 2021, 5558805. [Google Scholar] [CrossRef]
- Wehner, C.; Blank, C.; Arvandi, M.; Wehner, C.; Schobersberger, W. Effect of Tai Chi on muscle strength, physical endurance, postural balance and flexibility: A systematic review and meta-analysis. BMJ Open Sport Exerc. Med. 2021, 7, e000817. [Google Scholar] [CrossRef]
- Pascoe, M.C.; J de Manincor, M.; Hallgren, M.; Baldwin, P.A.; Tseberja, J.; Parker, A.G. Psychobiological mechanisms underlying the mental health benefits of yoga-based interventions: A narrative review. Mindfulness 2021, 12, 2877–2889. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, K.; Liu, H.; Qu, J.; Wang, Y.; Chen, P.; Zhang, T.; Luo, J. The impact of Otago exercise programme on the prevention of falls in older adult: A systematic review. Front. Public Health 2022, 10, 953593. [Google Scholar] [CrossRef] [PubMed]
- Carta, M.G.; Cossu, G.; Pintus, E.; Zoccheddu, R.; Callia, O.; Conti, G.; Pintus, M.; Gonzalez, C.I.A.; Massidda, M.V.; Mura, G. Active elderly and health—Can moderate exercise improve health and wellbeing in older adults? Protocol for a randomized controlled trial. Trials 2021, 22, 331. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Soh, K.G.; Omar Dev, R.D.; Talib, O.; Xiao, W.; Cai, H. Effect of brisk walking on health-related physical fitness balance and life satisfaction among the elderly: A systematic review. Front. Public Health 2022, 9, 829367. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, J.M.; Lopes, L.T.; Gonçalves, M.; Machado, J.P. Perceived Health Benefits of Taijiquan and Qigong. Altern. Ther. Health Med. 2023, 29, 222. [Google Scholar] [PubMed]
- Wang, R.; Huang, X.; Wu, Y.; Sun, D. Efficacy of qigong exercise for treatment of fatigue: A systematic review and meta-analysis. Front. Med. 2021, 8, 684058. [Google Scholar] [CrossRef] [PubMed]
- Wingood, M.; Bonnell, L.; LaCroix, A.Z.; Rosenberg, D.; Walker, R.; Bellettiere, J.; Greenwood-Hickman, M.A.; Wing, D.; Gell, N. Community-dwelling older adults and physical activity recommendations: Patterns of aerobic, strengthening, and balance activities. J. Aging Phys. Act. 2021, 30, 653–665. [Google Scholar] [CrossRef] [PubMed]
- Claudino, J.G.; Afonso, J.; Sarvestan, J.; Lanza, M.B.; Pennone, J.; Filho, C.A.C.; Serrão, J.C.; Espregueira-Mendes, J.; Vasconcelos, A.L.V.; de Andrade, M.P. Strength training to prevent falls in older adults: A systematic review with meta-analysis of randomized controlled trials. J. Clin. Med. 2021, 10, 3184. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, A.; Vieta, E.; Correll, C.U.; Nikodem, M.; Baldessarini, R.J. Critical issues on the use of network meta-analysis in psychiatry. Harv. Rev. Psychiatry 2014, 22, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Nevill, C.R.; Cooper, N.J.; Sutton, A.J. A multifaceted graphical display, including treatment ranking, was developed to aid interpretation of network meta-analysis. J. Clin. Epidemiol. 2023, 157, 83–91. [Google Scholar] [CrossRef]
- Chaimani, A.; Caldwell, D.M.; Li, T.; Higgins, J.P.; Salanti, G. Chapter 11: Undertaking Network Meta-Analyses. Cochrane Handbook for Systematic Reviews of Interventions version 6.3. In Cochrane Handbook for Systematic Reviews of Interventions; Cochrane Collaboration: London, UK, 2019; pp. 285–320. [Google Scholar]
- Su, X.; McDonough, D.J.; Chu, H.; Quan, M.; Gao, Z. Application of network meta-analysis in the field of physical activity and health promotion. J. Sport. Health Sci. 2020, 9, 511–520. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Yuan, Y.; Chu, H. The Impact of Excluding Trials from Network Meta-Analyses—An Empirical Study. PLoS ONE 2016, 11, e0165889. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, S.A. The geriatric depression scale (GDS). Best Pract. Nurs. Care Older Adults 2012, 4, 1–2. [Google Scholar]
- Jackson-Koku, G. Beck depression inventory. Occup. Med. 2016, 66, 174–175. [Google Scholar] [CrossRef] [PubMed]
- Bech, P. Fifty years with the Hamilton scales for anxiety and depression: A tribute to Max Hamilton. Psychother. Psychosom. 2009, 78, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Lappan, S.N.; Brown, A.W.; Hendricks, P.S. Dropout rates of in-person psychosocial substance use disorder treatments: A systematic review and meta-analysis. Addiction 2020, 115, 201–217. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G.; Group, C.S.M. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Cochrane Collaboration: London, UK, 2019; pp. 241–284. [Google Scholar]
- Higgins, J.P.; Eldridge, S.; Li, T. Including variants on randomized trials. In Cochrane Handbook for Systematic Reviews of Interventions; Cochrane Collaboration: London, UK, 2019; pp. 569–593. [Google Scholar]
- Page, M.J.; Higgins, J.P.; Sterne, J.A. Assessing risk of bias due to missing results in a synthesis. In Cochrane Handbook for Systematic Reviews of Interventions; Cochrane Collaboration: London, UK, 2019; pp. 349–374. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Fixed-effect versus random-effects models. Introd. Meta-Anal. 2009, 77, 85. [Google Scholar]
- Owen, R.K.; Bradbury, N.; Xin, Y.; Cooper, N.; Sutton, A. MetaInsight: An interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Res. Synth. Methods 2019, 10, 569–581. [Google Scholar] [CrossRef]
- Becker, L.A. Effect Size (ES). 2000. Available online: https://www.uv.es/friasnav/EffectSizeBecker.pdf (accessed on 2 March 2024).
- Higgins, J.P.; Li, T.; Deeks, J.J. Choosing effect measures and computing estimates of effect. In Cochrane Handbook for Systematic Reviews of Interventions; Cochrane Collaboration: London, UK, 2019; pp. 143–176. [Google Scholar]
- Pearson, M.J.; Smart, N.A. Reported methods for handling missing change standard deviations in meta-analyses of exercise therapy interventions in patients with heart failure: A systematic review. PLoS ONE 2018, 13, e0205952. [Google Scholar] [CrossRef]
- Aguiñaga, S.; Ehlers, D.K.; Salerno, E.A.; Fanning, J.; Motl, R.W.; McAuley, E. Home-Based Physical Activity Program Improves Depression and Anxiety in Older Adults. J. Phys. Act. Health 2018, 15, 692–696. [Google Scholar] [CrossRef]
- Belvederi Murri, M.; Amore, M.; Menchetti, M.; Toni, G.; Neviani, F.; Cerri, M.; Rocchi, M.B.; Zocchi, D.; Bagnoli, L.; Tam, E.; et al. Physical exercise for late-life major depression. Br. J. Psychiatry 2015, 207, 235–242. [Google Scholar] [CrossRef]
- Boström, G.; Conradsson, M.; Hörnsten, C.; Rosendahl, E.; Lindelöf, N.; Holmberg, H.; Nordström, P.; Gustafson, Y.; Littbrand, H. Effects of a high-intensity functional exercise program on depressive symptoms among people with dementia in residential care: A randomized controlled trial. Int. J. Geriatr. Psychiatry 2016, 31, 868–878. [Google Scholar] [CrossRef]
- Brittle, N.; Patel, S.; Wright, C.; Baral, S.; Versfeld, P.; Sackley, C. An exploratory cluster randomized controlled trial of group exercise on mobility and depression in care home residents. Clin. Rehabil. 2009, 23, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.J.; Hong, C.H.; Roh, H.W.; Lee, K.S.; Lee, E.H.; Kim, J.; Lim, H.K.; Son, S.J. A 12-Week Multi-Domain Lifestyle Modification to Reduce Depressive Symptoms in Older Adults: A Preliminary Report. Psychiatry Investig. 2018, 15, 279–284. [Google Scholar] [CrossRef]
- Chen, K.M.; Chen, M.H.; Chao, H.C.; Hung, H.M.; Lin, H.S.; Li, C.H. Sleep quality, depression state, and health status of older adults after silver yoga exercises: Cluster randomized trial. Int. J. Nurs. Stud. 2009, 46, 154–163. [Google Scholar] [CrossRef]
- Chen, H.M.; Tsai, C.M.; Wu, Y.C.; Lin, K.C.; Lin, C.C. Randomised controlled trial on the effectiveness of home-based walking exercise on anxiety, depression and cancer-related symptoms in patients with lung cancer. Br. J. Cancer 2015, 112, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhao, L.; Liu, Y.; Zhou, Z.; Zhang, H.; Wei, D.; Chen, J.; Li, Y.; Ou, J.; Huang, J.; et al. Otago exercise programme for physical function and mental health among older adults with cognitive frailty during COVID-19: A randomised controlled trial. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef]
- Chou, K.L.; Lee, P.W.; Yu, E.C.; Macfarlane, D.; Cheng, Y.H.; Chan, S.S.; Chi, I. Effect of Tai Chi on depressive symptoms amongst Chinese older patients with depressive disorders: A randomized clinical trial. Int. J. Geriatr. Psychiatry 2004, 19, 1105–1107. [Google Scholar] [CrossRef] [PubMed]
- Conradsson, M.; Littbrand, H.; Lindelof, N.; Gustafson, Y.; Rosendahl, E. Effects of a high-intensity functional exercise programme on depressive symptoms and psychological well-being among older people living in residential care facilities: A cluster-randomized controlled trial. Aging Ment. Health 2010, 14, 565–576. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.T.; Chow, P.K.; Yu, E.C.; Chan, A.C. Leisure activities alleviate depressive symptoms in nursing home residents with very mild or mild dementia. Am. J. Geriatr. Psychiatry 2012, 20, 904–908. [Google Scholar] [CrossRef]
- Danhauer, S.C.; Miller, M.E.; Divers, J.; Anderson, A.; Hargis, G.; Brenes, G.A. Long-Term Effects of Cognitive-Behavioral Therapy and Yoga for Worried Older Adults. Am. J. Geriatr. Psychiatry 2022, 30, 979–990. [Google Scholar] [CrossRef] [PubMed]
- de Lima, T.A.; Ferreira-Moraes, R.; Alves, W.; Alves, T.G.G.; Pimentel, C.P.; Sousa, E.C.; Abrahin, O.; Cortinhas-Alves, E.A. Resistance training reduces depressive symptoms in elderly people with Parkinson disease: A controlled randomized study. Scand. J. Med. Sci. Sports 2019, 29, 1957–1967. [Google Scholar] [CrossRef] [PubMed]
- Deus, L.A.; Corrêa, H.L.; Neves, R.V.P.; Reis, A.L.; Honorato, F.S.; Silva, V.L.; Souza, M.K.; de Araújo, T.B.; de Gusmão Alves, L.S.; Sousa, C.V.; et al. Are Resistance Training-Induced BDNF in Hemodialysis Patients Associated with Depressive Symptoms, Quality of Life, Antioxidant Capacity, and Muscle Strength? An Insight for the Muscle-Brain-Renal Axis. Int. J. Environ. Res. Public Health 2021, 18, 11299. [Google Scholar] [CrossRef] [PubMed]
- Gary, R.A.; Dunbar, S.B.; Higgins, M.K.; Musselman, D.L.; Smith, A.L. Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. J. Psychosom. Res. 2010, 69, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.T.; Liu, C.B.; Tsai, Y.H.; Chin, Y.F.; Wong, C.H. Physical fitness exercise versus cognitive behavior therapy on reducing the depressive symptoms among community-dwelling elderly adults: A randomized controlled trial. Int. J. Nurs. Stud. 2015, 52, 1542–1552. [Google Scholar] [CrossRef] [PubMed]
- Lavretsky, H.; Milillo, M.M.; Kilpatrick, L.; Grzenda, A.; Wu, P.; Nguyen, S.A.; Ercoli, L.M.; Siddarth, P. A Randomized Controlled Trial of Tai Chi Chih or Health Education for Geriatric Depression. Am. J. Geriatr. Psychiatry 2022, 30, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Lok, N.; Lok, S.; Canbaz, M. The effect of physical activity on depressive symptoms and quality of life among elderly nursing home residents: Randomized controlled trial. Arch. Gerontol. Geriatr. 2017, 70, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Tsutsumimoto, K.; Doi, T.; Makino, K.; Nakakubo, S.; Liu-Ambrose, T.; Shimada, H. Exercise and Horticultural Programs for Older Adults with Depressive Symptoms and Memory Problems: A Randomized Controlled Trial. J. Clin. Med. 2019, 9, 99. [Google Scholar] [CrossRef]
- McMurdo, M.E.; Burnett, L. Randomised controlled trial of exercise in the elderly. Gerontology 1992, 38, 292–298. [Google Scholar] [CrossRef]
- Moraes, H.S.; Silveira, H.S.; Oliveira, N.A.; Matta Mello Portugal, E.; Araújo, N.B.; Vasques, P.E.; Bergland, A.; Santos, T.M.; Engedal, K.; Coutinho, E.S.; et al. Is Strength Training as Effective as Aerobic Training for Depression in Older Adults? A Randomized Controlled Trial. Neuropsychobiology 2020, 79, 141–149. [Google Scholar] [CrossRef]
- Ng, T.P.; Nyunt, M.S.Z.; Feng, L.; Feng, L.; Niti, M.; Tan, B.Y.; Chan, G.; Khoo, S.A.; Chan, S.M.; Yap, P.; et al. Multi-Domains Lifestyle Interventions Reduces Depressive Symptoms among Frail and Pre-Frail Older Persons: Randomized Controlled Trial. J. Nutr. Health Aging 2017, 21, 918–926. [Google Scholar] [CrossRef]
- Seino, S.; Nishi, M.; Murayama, H.; Narita, M.; Yokoyama, Y.; Nofuji, Y.; Taniguchi, Y.; Amano, H.; Kitamura, A.; Shinkai, S. Effects of a multifactorial intervention comprising resistance exercise, nutritional and psychosocial programs on frailty and functional health in community-dwelling older adults: A randomized, controlled, cross-over trial. Geriatr. Gerontol. Int. 2017, 17, 2034–2045. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, M.; Mojtahed, A.; Modabbernia, A.; Mojtahed, M.; Shafiabady, A.; Delavar, A.; Honari, H. Laughter yoga versus group exercise program in elderly depressed women: A randomized controlled trial. Int. J. Geriatr. Psychiatry 2011, 26, 322–327. [Google Scholar] [CrossRef]
- Shahtahmassebi, B.; Hatton, J.; Hebert, J.J.; Hecimovich, M.; Correia, H.; Fairchild, T.J. The effect of the inclusion of trunk-strengthening exercises to a multimodal exercise program on physical activity levels and psychological functioning in older adults: Secondary data analysis of a randomized controlled trial. BMC Geriatr. 2022, 22, 738. [Google Scholar] [CrossRef]
- Singh, N.A.; Clements, K.M.; Fiatarone, M.A. A randomized controlled trial of progressive resistance training in depressed elders. J. Gerontol. A Biol. Sci. Med. Sci. 1997, 52, M27–M35. [Google Scholar] [CrossRef]
- Singh, N.A.; Stavrinos, T.M.; Scarbek, Y.; Galambos, G.; Liber, C.; Fiatarone Singh, M.A. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Sjösten, N.M.; Vahlberg, T.J.; Kivelä, S.L. The effects of multifactorial fall prevention on depressive symptoms among the aged at increased risk of falling. Int. J. Geriatr. Psychiatry 2008, 23, 504–510. [Google Scholar] [CrossRef]
- Tsang, H.W.; Fung, K.M.; Chan, A.S.; Lee, G.; Chan, F. Effect of a qigong exercise programme on elderly with depression. Int. J. Geriatr. Psychiatry 2006, 21, 890–897. [Google Scholar] [CrossRef]
- Underwood, M.; Lamb, S.E.; Eldridge, S.; Sheehan, B.; Slowther, A.; Spencer, A.; Thorogood, M.; Atherton, N.; Bremner, S.A.; Devine, A.; et al. Exercise for depression in care home residents: A randomised controlled trial with cost-effectiveness analysis (OPERA). Health Technol. Assess. 2013, 17, 1–281. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.L.; Tappen, R.M. Exercise training for depressed older adults with Alzheimer’s disease. Aging Ment. Health 2008, 12, 72–80. [Google Scholar] [CrossRef]
- Tang, L.; Zhang, L.; Liu, Y.; Li, Y.; Yang, L.; Zou, M.; Yang, H.; Zhu, L.; Du, R.; Shen, Y.; et al. Optimal dose and type of exercise to improve depressive symptoms in older adults: A systematic review and network meta-analysis. BMC Geriatr. 2024, 24, 505. [Google Scholar] [CrossRef]
- Correia, É.M.; Monteiro, D.; Bento, T.; Rodrigues, F.; Cid, L.; Vitorino, A.; Figueiredo, N.; Teixeira, D.S.; Couto, N. Analysis of the Effect of Different Physical Exercise Protocols on Depression in Adults: Systematic Review and Meta-analysis of Randomized Controlled Trials. Sports Health 2024, 16, 285–294. [Google Scholar] [CrossRef]
- Mahmoudi, A.; Amirshaghaghi, F.; Aminzadeh, R.; Mohamadi Turkmani, E. Effect of Aerobic, Resistance, and Combined Exercise Training on Depressive Symptoms, Quality of Life, and Muscle Strength in Healthy Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Biol. Res. Nurs. 2022, 24, 541–559. [Google Scholar] [CrossRef] [PubMed]
- Piva, G.; Caruso, L.; Gómez, A.C.; Calzolari, M.; Visintin, E.P.; Davoli, P.; Manfredini, F.; Storari, A.; Spinozzi, P.; Lamberti, N. Effects of forest walking on physical and mental health in elderly populations: A systematic review. Rev. Environ. Health 2024, 39, 121–136. [Google Scholar] [CrossRef]
- Milton-Cole, R.; Kazeem, K.; Gibson, A.; Guerra, S.; Sheehan, K.J. Effectiveness of exercise rehabilitation interventions on depressive symptoms in older adults post hip fracture: A systematic review and meta-analysis. Osteoporos. Int. 2024, 35, 227–242. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Mansfield, J.; Marx, M.S.; Biddison, J.R.; Guralnik, J.M. Socio-environmental exercise preferences among older adults. Prev. Med. 2004, 38, 804–811. [Google Scholar] [CrossRef]
- Silva, L.A.d.; Tortelli, L.; Motta, J.; Menguer, L.; Mariano, S.; Tasca, G.; Silveira, G.d.B.; Pinho, R.A.; Silveira, P.C.L. Effects of aquatic exercise on mental health, functional autonomy and oxidative stress in depressed elderly individuals: A randomized clinical trial. Clinics 2019, 74, e322. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.-Y.; Ho, K.-H.; Chen, H.-C.; Chien, M.-Y. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: A systematic review. J. Physiother. 2012, 58, 157–163. [Google Scholar] [CrossRef]
- Liu, F.; Cui, J.; Liu, X.; Chen, K.W.; Chen, X.; Li, R. The effect of tai chi and Qigong exercise on depression and anxiety of individuals with substance use disorders: A systematic review and meta-analysis. BMC Complement. Med. Ther. 2020, 20, 161. [Google Scholar] [CrossRef]
- Voss, S.; Cerna, J.; Gothe, N.P. Yoga impacts cognitive health: Neurophysiological changes and stress regulation mechanisms. Exerc. Sport Sci. Rev. 2023, 51, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Aditi Devi, N.; Phillip, M.; Varambally, S.; Christopher, R.; Gangadhar, B.N. Yoga as a monotherapy alters proBDNF—Mature BDNF ratio in patients with major depressive disorder. Asian J. Psychiatr. 2023, 81, 103429. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.; Ahn, J. The effect of changes in physical self-concept through participation in exercise on changes in self-esteem and mental well-being. Int. J. Environ. Res. Public Health 2021, 18, 5224. [Google Scholar] [CrossRef] [PubMed]
- Craft, L.L. Potential psychological mechanisms underlying the exercise and depression relationship. In Routledge Handbook of Physical Activity and Mental Health; Routledge: London, UK, 2023; pp. 161–168. [Google Scholar]
- Abdulrasool, M.D.; EmadOdaJoda, A.; Abdulrasool, M.D. The effect of psycho-physiological sports proposed in terms of the hormone endorphins serotonin and their relative results on mental fitness in the aged. Ann. Trop. Med. Public Health 2020, 23, 231–369. [Google Scholar] [CrossRef]
- Latino, F.; Tafuri, F. Physical Activity and Cognitive Functioning. Medicina 2024, 60, 216. [Google Scholar] [CrossRef] [PubMed]
- Kazeminia, M.; Salari, N.; Vaisi-Raygani, A.; Jalali, R.; Abdi, A.; Mohammadi, M.; Daneshkhah, A.; Hosseinian-Far, M.; Shohaimi, S. The effect of exercise on anxiety in the elderly worldwide: A systematic review and meta-analysis. Health Qual. Life Outcomes 2020, 18, 363. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Comellas, A.; Valmaña, G.S.; Catalina, Q.M.; Baena, I.G.; Mendioroz Peña, J.; Roura Poch, P.; Sabata Carrera, A.; Cornet Pujol, I.; Casaldàliga Solà, À.; Fusté Gamisans, M. Effects of physical activity interventions in the elderly with anxiety, depression, and low social support: A clinical multicentre randomised trial. Healthcare 2022, 10, 2203. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Su, D.; Chen, Y.; Tan, M.; Chen, X. Effect of socioeconomic status on the physical and mental health of the elderly: The mediating effect of social participation. BMC Public Health 2022, 22, 605. [Google Scholar] [CrossRef] [PubMed]
- Weyerer, S.; Kupfer, B. Physical exercise and psychological health. Sports Med. 1994, 17, 108–116. [Google Scholar] [CrossRef]
- Langoni, C.d.S.; Resende, T.d.L.; Barcellos, A.B.; Cecchele, B.; da Rosa, J.N.; Knob, M.S.; Silva, T.d.N.; Diogo, T.d.S.; da Silva, I.G.; Schwanke, C.H.A. The effect of group exercises on balance, mobility, and depressive symptoms in older adults with mild cognitive impairment: A randomized controlled trial. Clin. Rehabil. 2019, 33, 439–449. [Google Scholar] [CrossRef]
- Singh, N.A.; Clements, K.M.; Singh, M.A.F. The efficacy of exercise as a long-term antidepressant in elderly subjects: A randomized, controlled trial. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M497–M504. [Google Scholar] [CrossRef] [PubMed]
| Sample | Intervention Group | Control Group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors & Year | Country | Comparison | n | Dro- pouts | Age, Mean (SD) | Gender ♀ (%) | IX Type | Dosage | Min. MET/ Week | Ctl. Type | Descriptions | Duration | Outcomes |
| Aguinaga et al., 2018 [38] | USA | Strength Control | 158 149 | 34 26 | 70.62 (5.02) 71.43 (5.25) | 71% 82% | Strength | Freq. of light, mod., & vig. exercise ≥ 15 min/sess., weekly in leisure time. | - | Passive | Educational | 24 w | HADS |
| Belvederi Murri et al., 2015 [39] | Italy | Aerobic Multisport Control | 42 37 42 | 0 0 0 | 75.00 (6.20) 75.00 (6.30) 75.60 (5.60) | 69% 68% 76% | Aerobic Multisport | 60 min/sess., 3 x/w | 2160 | Active | Pharmacological treatment only | 24 w | HADS |
| Boström et al., 2016 [40] | Sweden | HIFE Control | 93 93 | 10 12 | 84.40 (6.20) 85.90 (7.80) | 76% | Strength | 45 min/sess., total 40 sess. | 630 | Passive | Activities of daily living | 16 w | GDS MADRS |
| Brittle et al., 2009 [41] | UK | Exercise Control | 20 18 | 3 5 | 87.00 (6.99) 82.00 (9.98) | 79% 64% | Multisport | 40–60 min/sess., 2 x/w | 480 | Passive | Usual care | 12 w | SADQ |
| Chang et al., 2018 [42] | South Korea | Aerobic Control | 47 46 | 2 3 | 77.80 (6.60) 77.80 (6.60) | 86% 88% | Multisport | 30 min/sess., 3 x/w | 540 | Passive | Social | 12 w | GDS |
| Chen et al., 2009 [43] | Taiwan | Yoga Control | 67 72 | 3 6 | 69.20 (6.23) | 73% | Yoga | 70 min/sess., 3 x/w | 525 | Passive | Usual care | 24 w | TDQ |
| Chen et al., 2015 [44] | Taiwan | Walking exercise Control | 58 58 | 8 7 | 64.76 (11.28) 63.57 (10.54) | 55% 51% | Walking | 40 min/sess., 3 sess./week, and weekly exercise counseling | 300 | Passive | Usual care | 12 w | HADS |
| Chen et al., 2021 [45] | China | OEP Control | 31 31 | 1 2 | 84.59 (4.21) 84.75 (5.41) | 83% 60% | OEP | 30 min/sess., 3 sess./w | 315 | Passive | Activities of daily living | 12 w | GDS-15 |
| Cheng et al., 2012 [48] | China | Tai chi Control | 12 12 | 0 0 | 81.00 (7.70) 82.50 (7.10) | 50% 75% | Tai chi | 60 min/sess., 3 x/w | 540 | Passive | Social | 24 w | GDS |
| Chou et al., 2004 [46] | China | Tai chi Waitlist | 14 | 0 | 72.60 (4.20) | 50% | Tai chi | 45 min/sess., 3 x/w | 405 | Waitlist | Waitlist | 12 w | CES-D |
| Conradsson et al., 2010 [47] | Sweden | Exercise Control | 91 100 | 2 1 | 85.3 (6.1) 84.2 (6.8) | 74% 72% | Strength | 45 min/sess., 5 sess./two weeks (total 29 sess.) | 1142 | Passive | Activities of daily living | 12 w | GDS-15 |
| Danhauer et al., 2022 [49] | USA | Yoga Control—CBT | 110 100 | 0 0 | 66.30 (4.90) 66.70 (5.70) | 82% 90% | Yoga | 75 min/session, 1 x/2 w | 94 | Active | CBT | 11 w | PROMIS-29 Depression |
| de Lima et al., 2019 [50] | Brazil | Resistance training Control | 17 16 | 0 0 | 66.2 (5.5) 67.2 (5.2) | - | Strength | 30–40 min/sess., 2 sess./w | 210 | Active | Pharmacological treatment only | 20 w | HRDS |
| Deus et al., 2021 [51] | Brazil | Strength Control | 101 110 | 20 34 | 67.27 (3.24) 66.33 (3.88) | 43% 47% | Strength | 3 x/w | - | Waitlist | Waitlist | 24 w | BDI |
| Gary et al., 2010 [52] | USA | Home-based exercise Control | 20 17 | 3 3 | 65.80 (13.50) | 57% | Walking | 60 min/sess., 3 x/w | 450 | Active | CBT Usual care | 12 w | HAMD |
| Huang et al., 2015 [53] | Taiwan | Strength Control | 19 20 | 0 0 | 76.53 (5.94) | 53% | Strength | 50 min/sess., 3 x/w | 525 | Active Passive | CBT Usual care | 12 w | GDS |
| Lavretsky et al., 2022 [54] | USA | Tai chi Control | 89 89 | 27 26 | 69.20 (6.90) 69.40 (6.20) | 70% 75% | Tai chi | 60 min/sess., 1 x/w | 180 | Passive | Educational | 12 w | GDS |
| Lok et al., 2017 [55] | Turkey | Mixed aerobic exercises Control | 80 | 0 | 65–90 | 45% | Multisport | 70 min/sess., 4 x/w | 1680 | Waitlist | Waitlist | 10 w | BDI |
| Makizako et al., 2020 [56] | Japan | Strength Control | 27 28 | 3 1 | 73.10 (5.50) | 51% | Strength | 90 min/sess., 1 x/w | 315 | Passive | Educational | 24 w | GDS |
| McMurdo et al., 2001 [57] | UK | Aerobic + Strength Control | 87 | 0 | 65.30 (4.30) | 59% | Aerobic + Strength | 45 min/sess., 3 x/w | 1283 | Passive | Educational | 10 w | GDS |
| Moraes et al., 2020 [58] | Brazil | Aerobic Strength Control | 9 9 7 | 8 8 5 | 70.88 (5.940 72.89 (7.06) 69.28 (5.28) | - | Aerobic + Strength | 5 min warm-up, 20 min exercise; 3 sets of 8–12 reps for major muscle groups | 765 | Passive | Activities of Daily Living | 12 w | HAMD BDI |
| Ng et al., 2017 [59] | Singapore | Physical Training Control | 48 50 | 0 0 | 70.3 (5.25) 70.1 (5.02) | - | Physical Training | 90 min, 2 days/w | 900 | Passive | Usual care | 12 m | GDS |
| Seino et al., 2017 [60] | Japan | IIG DIG | 38 39 | 0 0 | 74.9 ± 5.3 74.3 ± 5.6 | 37% 26% | Strength | 100 min/sess., 2 x/w | 700 | Passive | DIG | 12 w | GDS |
| Shahidi et al., 2011 [61] | Iran | Jogging Laughter Yoga Control | 60 | 0 | 65.70 (4.20) 65.50 (4.80) 68.40 (6.30) | 100% | Jogging yoga | 30 min/sess., 10 | 2100 750 | Waitlist | Waitlist | 10 times | GDS |
| Shahtahmassebi et al., 2022 [62] | Iran | Trunk Strengthening Walking | 32 32 | 0 0 | 70.1 (7.7) 69.4 (7.3) | 57% 63% | Strength | 3 sess./w | - | Passive | Activities of daily living | 18 w | GDS |
| Singh et al., 1997 [63] | USA | Strength Control | 32 | 0 | 70.00 (1.50) 72.00 (2.00) | 71% 53% | Strength | 45 min/sess., 3 x/w | 472.5 | Passive | Educational | 10 w | GDS |
| Singh et al., 2005 [64] | Australia | Strength—high-intensity Strength—low-intensity Control | 18 17 19 | 2 3 1 | 69.00 (5.00) 70.00 (7.00) 69.00 (7.00) | 50% 47% 53% | Strength | 65 min/sess., 3 x/w | 682.5 | Passive | Usual care | 8 w | GDS |
| Sjösten et al., 2008 [65] | Finland | Aerobic + Therapy Control | 293 298 | 32 29 | 72.70 (5.40) 72.80 (5.90) | 76% | Aerobic + Therapy | 2 x/m | - | Passive | Usual care | 12 m | GDS |
| Tsang et al., 2006 [66] | China | Qigong Control | 48 34 | 0 0 | 82.11 (7.19) 82.74 (6.83) | 83% | Qigong | 45 min/sess., 3 x/w | 405 | Passive | Educational | 16 w | GDS |
| Underwood et al., 2013 [67] | The UK | Exercise Depression awareness training | 174 200 | 51 64 | 86.6 (7.4) 86.7 (7.8) | 75% 74% | Multisport | 2 x/week | - | Active | Depression awareness training | 24 w | GDS |
| Williams et al., 2008 [68] | USA | Aerobic + Strength Walking Control | 16 17 12 | 1 6 0 | 87.90 (5.95) | 89% | Aerobic + Strength Walking | 30 min/sess., 5 x/w | 1425 375 | Passive | Social | 16 w | CSDD |
| Qigong | −1.17 [−2.28; −0.06] | |||||||||||
| −0.02 [−1.61; 1.57] | Otago Exercise | −1.15 [−2.29; −0.01] | ||||||||||
| −0.29 [−1.59; 1.00] | −0.27 [−1.60; 1.06] | Yoga | −0.46 [−1.64; 0.72] | −0.13 [−1.17; 0.91] | −1.27 [−2.07; −0.46] | |||||||
| −0.35 [−1.57; 0.88] | −0.32 [−1.58; 0.93] | −0.05 [−0.89; 0.78] | Walking | −0.17 [−1.29; 0.94] | −0.04 [−1.31; 1.23] | −0.82 [−1.41; −0.24] | ||||||
| −0.43 [−1.98; 1.12] | −0.41 [−1.98; 1.16] | −0.14 [−1.21; 0.93] | −0.08 [−1.27; 1.10] | Jogging | −1.08 [−2.27; 0.12] | |||||||
| −0.50 [−1.67; 0.67] | −0.47 [−1.68; 0.73] | −0.20 [−0.94; 0.53] | −0.15 [−0.73; 0.43] | −0.07 [−1.19; 1.06] | Strength | −0.87 [−1.69; −0.06] | −0.69 [−1.12; −0.26] | −0.66 [−1.71; 0.39] | ||||
| −0.55 [−1.86; 0.77] | −0.53 [−1.87; 0.82] | −0.26 [−1.22; 0.71] | −0.20 [−1.06; 0.66] | −0.12 [−1.40; 1.17] | −0.05 [−0.84; 0.74] | Aerobic | −0.35 [−1.45; 0.74] | −0.71 [−1.46; 0.04] | ||||
| −0.63 [−2.18; 0.92] | −0.61 [−2.18; 0.96] | −0.34 [−1.61; 0.93] | −0.29 [−1.48; 0.91] | −0.20 [−1.73; 1.32] | −0.14 [−1.28; 1.01] | −0.08 [−1.37; 1.21] | Physical Training | −0.54 [−1.62; 0.54] | ||||
| −0.66 [−2.00; 0.69] | −0.64 [−2.01; 0.74] | −0.37 [−1.38; 0.65] | −0.31 [−1.23; 0.61] | −0.23 [−1.55; 1.09] | −0.16 [−1.00; 0.68] | −0.11 [−1.15; 0.93] | −0.03 [−1.35; 1.30] | Tai chi | −0.06 [−0.87; 0.76] | −3.99 [−6.06; −1.92] | ||
| −0.85 [−2.06; 0.35] | −0.83 [−2.07; 0.41] | −0.56 [−1.33; 0.21] | −0.51 [−1.16; 0.15] | −0.42 [−1.58; 0.74] | −0.36 [−0.91; 0.19] | −0.31 [−1.08; 0.47] | −0.22 [−1.40; 0.96] | −0.19 [−1.08; 0.69] | Multisport | −0.32 [−1.16; 0.51] | −0.30 [−0.88; 0.28] | −0.66 [−1.75; 0.44] |
| −1.07 [−2.33; 0.19] | −1.05 [−2.34; 0.24] | −0.78 [−1.51; −0.04] | −0.72 [−1.48; 0.03] | −0.64 [−1.81; 0.54] | −0.57 [−1.17; 0.02] | −0.52 [−1.42; 0.37] | −0.44 [−1.67; 0.80] | −0.41 [−1.37; 0.55] | −0.22 [−0.83; 0.40] | Control Active | ||
| −1.17 [−2.28; −0.06] | −1.15 [−2.29; −0.01] | −0.88 [−1.55; −0.21] | −0.82 [−1.34; −0.31] | −0.74 [−1.82; 0.34] | −0.67 [−1.05; −0.30] | −0.62 [−1.33; 0.08] | −0.54 [−1.62; 0.54] | −0.51 [−1.28; 0.25] | −0.32 [−0.79; 0.16] | −0.10 [−0.70; 0.50] | Control Passive | |
| −1.72 [−3.07; −0.37] | −1.70 [−3.08; −0.32] | −1.43 [−2.42; −0.43] | −1.37 [−2.27; −0.47] | −1.29 [−2.60; 0.03] | −1.22 [−1.99; −0.46] | −1.17 [−2.19; −0.15] | −1.09 [−2.42; 0.24] | −1.06 [−2.08; −0.05] | −0.87 [−1.64; −0.09] | −0.65 [−1.55; 0.25] | −0.55 [−1.32; 0.23] | Control Waitlist |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dai, M.-L.; Ting, B.; Malau, I.A.; Wu, S.-K.; Lin, C.-C.; Lin, P.-Y.; Chen, M.-H. Motivational Barriers and Facilitators for Older Adults’ Engagement in Exercise during Depressive Episodes: A Network Meta-Analysis of Randomized Controlled Trials. Healthcare 2024, 12, 1498. https://doi.org/10.3390/healthcare12151498
Dai M-L, Ting B, Malau IA, Wu S-K, Lin C-C, Lin P-Y, Chen M-H. Motivational Barriers and Facilitators for Older Adults’ Engagement in Exercise during Depressive Episodes: A Network Meta-Analysis of Randomized Controlled Trials. Healthcare. 2024; 12(15):1498. https://doi.org/10.3390/healthcare12151498
Chicago/Turabian StyleDai, Mei-Ling, Berne Ting, Ikbal Andrian Malau, Suet-Kei Wu, Chia-Ching Lin, Pan-Yen Lin, and Min-Hsiung Chen. 2024. "Motivational Barriers and Facilitators for Older Adults’ Engagement in Exercise during Depressive Episodes: A Network Meta-Analysis of Randomized Controlled Trials" Healthcare 12, no. 15: 1498. https://doi.org/10.3390/healthcare12151498
APA StyleDai, M.-L., Ting, B., Malau, I. A., Wu, S.-K., Lin, C.-C., Lin, P.-Y., & Chen, M.-H. (2024). Motivational Barriers and Facilitators for Older Adults’ Engagement in Exercise during Depressive Episodes: A Network Meta-Analysis of Randomized Controlled Trials. Healthcare, 12(15), 1498. https://doi.org/10.3390/healthcare12151498







