Present but Ignored: Physical Condition and Health-Related Quality of Life in College-Aged Females with Generalized Joint Hypermobility
Abstract
1. Introduction
2. Materials and Methods
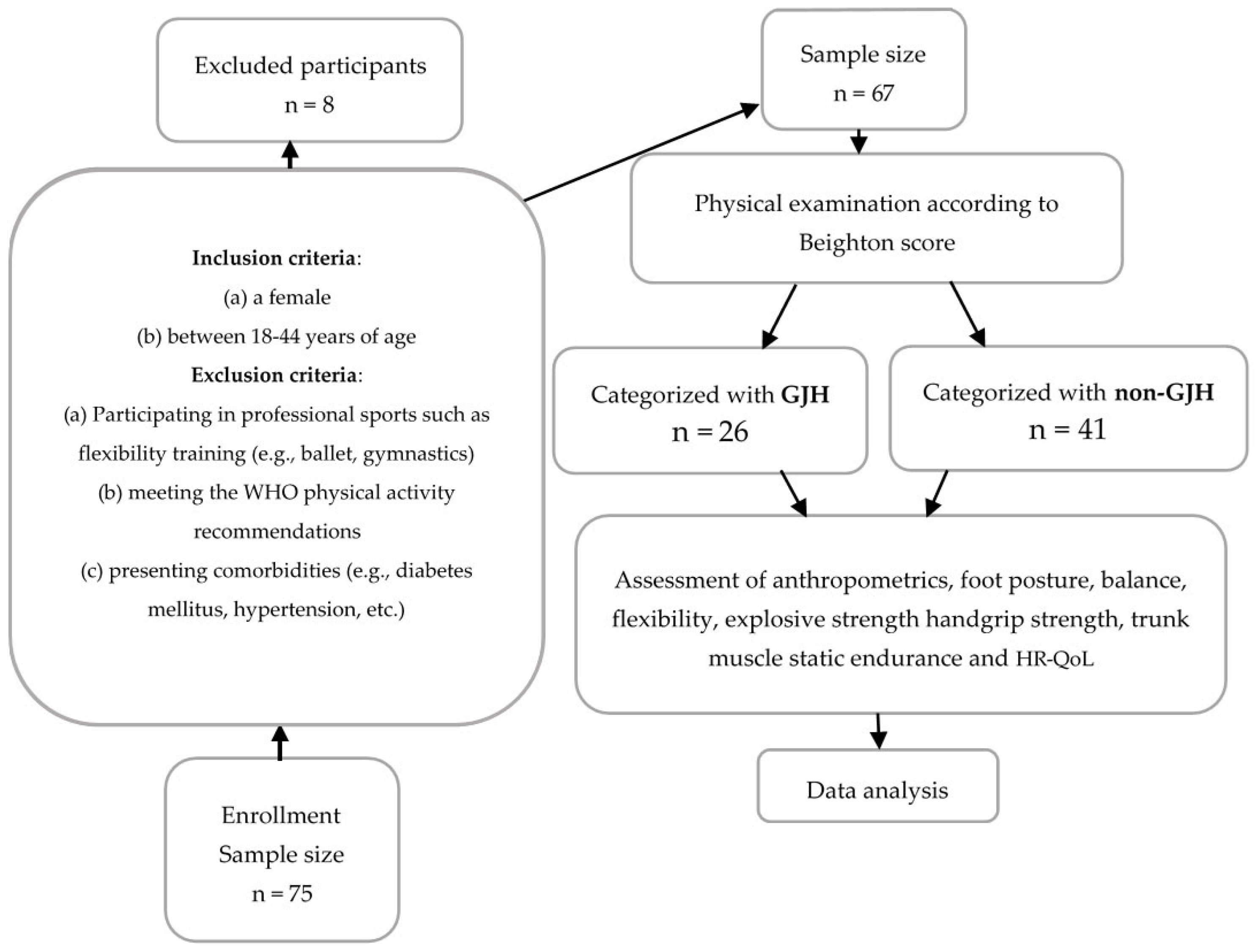
2.1. Participants
2.2. GJH Assessment
2.3. Anthropometric Measurement
2.4. Foot Posture Analysis
2.5. Assessment of Physical Fitness
2.5.1. Balance Assessment
2.5.2. Flexibility
2.5.3. Explosive Strength Assessment
2.5.4. Handgrip Strength Assessment
2.5.5. Trunk Muscle Static Strength Endurance Assessment
2.6. Health-Related Quality of Life
2.7. Data Analysis
3. Results
3.1. Participants’ Data
3.2. Foot Posture
3.3. Physical Fitness
3.4. Health-Related Quality of Life
4. Discussion
4.1. Physical Fitness
4.2. Foot Posture
4.3. Health-Related Quality of Life
4.4. Strengths and Limitations of the Study
4.5. Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Remvig, L.; Flycht, L.; Christensen, K.B.; Juul-Kristensen, B. Lack of Consensus on Tests and Criteria for Generalized Joint Hypermobility, Ehlers-Danlos Syndrome: Hypermobile Type and Joint Hypermobility Syndrome. Am. J. Med. Genet. A. 2014, 164A, 591–596. [Google Scholar] [CrossRef]
- Zhong, G.; Zeng, X.; Xie, Y.; Lai, J.; Wu, J.; Xu, H.; Lin, C.; Li, H.; Cui, C.; Ma, L.; et al. Prevalence and Dynamic Characteristics of Generalized Joint Hypermobility in College Students. Gait Posture 2021, 84, 254–259. [Google Scholar] [CrossRef]
- Malek, S.; Reinhold, E.J.; Pearce, G.S. The Beighton Score as a Measure of Generalised Joint Hypermobility. Rheumatol. Int. 2021, 41, 1707–1716. [Google Scholar] [CrossRef]
- Kumar, B.; Lenert, P. Joint Hypermobility Syndrome: Recognizing a Commonly Overlooked Cause of Chronic Pain. Am. J. Med. 2017, 130, 640–647. [Google Scholar] [CrossRef]
- Morris, S.L.; O’Sullivan, P.B.; Murray, K.J.; Bear, N.; Hands, B.; Smith, A.J. Hypermobility and Musculoskeletal Pain in Adolescents. J. Pediatr. 2017, 181, 213–221.e1. [Google Scholar] [CrossRef]
- Reuter, P.R.; Fichthorn, K.R. Prevalence of Generalized Joint Hypermobility, Musculoskeletal Injuries, and Chronic Musculoskeletal Pain among American University Students. PeerJ 2019, 7, e7625. [Google Scholar] [CrossRef]
- Russek, L.N.; Errico, D.M. Prevalence, Injury Rate and, Symptom Frequency in Generalized Joint Laxity and Joint Hypermobility Syndrome in a “Healthy” College Population. Clin. Rheumatol. 2016, 35, 1029–1039. [Google Scholar] [CrossRef]
- Wolf, J.M.; Cameron, K.L.; Owens, B.D. Impact of Joint Laxity and Hypermobility on the Musculoskeletal System. J. Am. Acad. Orthop. Surg. 2011, 19, 463–471. [Google Scholar] [CrossRef]
- Tuna, F. Prevalence of Joint Hypermobility, Hypermobility Spectrum Disorder and Hypermobile Ehlers-Danlos Syndrome in a University Population: An Observational Study. Eur. Res. J. 2020, 6, 120–129. [Google Scholar] [CrossRef]
- Cohen, A.; Sela, M.C.; Ran, L.Z.; Rushinek, H.; Talisman, S.; Casap, N. Increased Prevalence of Generalized Joint Hypermobility Observed in Patients With Recurrent Temporomandibular Joint Dislocation. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2023, 81, 950–955. [Google Scholar] [CrossRef]
- Zsidai, B.; Piussi, R.; Thomeé, R.; Sundemo, D.; Musahl, V.; Samuelsson, K.; Hamrin Senorski, E. Generalised Joint Hypermobility Leads to Increased Odds of Sustaining a Second ACL Injury within 12 Months of Return to Sport after ACL Reconstruction. Br. J. Sports Med. 2023, 57, 972–978. [Google Scholar] [CrossRef]
- Lamari, N.; Beighton, P. Physiotherapy for Joint Hypermobility Disorders. In Hypermobility in Medical Practice; In Clinical Practice; Springer Nature Switzerland: Cham, Switzerland, 2023; pp. 173–184. [Google Scholar] [CrossRef]
- Juul-Kristensen, B.; Østengaard, L.; Hansen, S.; Boyle, E.; Junge, T.; Hestbaek, L. Generalised Joint Hypermobility and Shoulder Joint Hypermobility-Risk of Upper Body Musculoskeletal Symptoms and Reduced Quality of Life in the General Population. BMC Musculoskelet. Disord. 2017, 18, 226. [Google Scholar] [CrossRef]
- Booshanam, D.S.; Cherian, B.; Joseph, C.P.A.R.; Mathew, J.; Thomas, R. Evaluation of Posture and Pain in Persons with Benign Joint Hypermobility Syndrome. Rheumatol. Int. 2011, 31, 1561–1565. [Google Scholar] [CrossRef]
- Khan, F.R.; Chevidikunnan, M.F.; Mazi, A.F.; Aljawi, S.F.; Mizan, F.H.; BinMulayh, E.A.; Sahu, K.S.; Al-Lehidan, N.S. Factors Affecting Foot Posture in Young Adults: A Cross Sectional Study. J. Musculoskelet. Neuronal Interact. 2020, 20, 216–222. [Google Scholar]
- Biz, C.; Maso, G.; Malgarini, E.; Tagliapietra, J.; Ruggieri, P. Hypermobility of the First Ray: The Cinderella of the Measurements Conventionally Assessed for Correction of Hallux Valgus. Acta Bio Medica Atenei Parm. 2020, 91, 47–59. [Google Scholar] [CrossRef]
- Morgan, O.J.; Hillstrom, R.; Turner, R.; Day, J.; Thaqi, I.; Caolo, K.; Ellis, S.; Deland, J.T.; Hillstrom, H.J. Is the Planus Foot Type Associated With First Ray Hypermobility? Foot Ankle Orthop. 2022, 7, 24730114221081545. [Google Scholar] [CrossRef]
- Santana, C.C.A.; Azevedo, L.B.; Cattuzzo, M.T.; Hill, J.O.; Andrade, L.P.; Prado, W.L. Physical Fitness and Academic Performance in Youth: A Systematic Review. Scand. J. Med. Sci. Sports 2017, 27, 579–603. [Google Scholar] [CrossRef]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Akkaya, K.U.; Burak, M.; Erturan, S.; Yildiz, R.; Yildiz, A.; Elbasan, B. An Investigation of Body Awareness, Fatigue, Physical Fitness, and Musculoskeletal Problems in Young Adults with Hypermobility Spectrum Disorder. Musculoskelet. Sci. Pract. 2022, 62, 102642. [Google Scholar] [CrossRef]
- Scheper, M.; de Vries, J.; Beelen, A.; de Vos, R.; Nollet, F.; Engelbert, R. Generalized Joint Hypermobility, Muscle Strength and Physical Function in Healthy Adolescents and Young Adults. Curr. Rheumatol. Rev. 2014, 10, 117–125. [Google Scholar] [CrossRef]
- Tinkle, B.T. Symptomatic Joint Hypermobility. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101508. [Google Scholar] [CrossRef]
- Liaghat, B.; Juul-Kristensen, B.; Frydendal, T.; Marie Larsen, C.; Søgaard, K.; Ilkka Tapio Salo, A. Competitive Swimmers with Hypermobility Have Strength and Fatigue Deficits in Shoulder Medial Rotation. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2018, 39, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Maestroni, L.; Read, P.; Bishop, C.; Papadopoulos, K.; Suchomel, T.J.; Comfort, P.; Turner, A. The Benefits of Strength Training on Musculoskeletal System Health: Practical Applications for Interdisciplinary Care. Sports Med. 2020, 50, 1431–1450. [Google Scholar] [CrossRef] [PubMed]
- Kocheta, R.; Musale, R.; Andhare, N. Correlation between Joint Hypermobility and Balance in Indian Elite Gymnasts. Arch. Med. Health Sci. 2023, 11, 219. [Google Scholar] [CrossRef]
- Bates, A.V.; McGregor, A.; Alexander, C.M. Adaptation of Balance Reactions Following Forward Perturbations in People with Joint Hypermobility Syndrome. BMC Musculoskelet. Disord. 2021, 22, 123. [Google Scholar] [CrossRef] [PubMed]
- Junge, T.; Henriksen, P.; Hansen, S.; Østengaard, L.; Golightly, Y.M.; Juul-Kristensen, B. Generalised Joint Hypermobility and Knee Joint Hypermobility: Prevalence, Knee Joint Symptoms and Health-related Quality of Life in a Danish Adult Population. Int. J. Rheum. Dis. 2019, 22, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.T.; Snyder, A.R. Health-Related Quality of Life as a Primary Clinical Outcome in Sport Rehabilitation. J. Sport Rehabil. 2011, 20, 17–36. [Google Scholar] [CrossRef]
- WHO. Physical Activity. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 28 March 2024).
- Beighton, P.; Solomon, L.; Soskolne, C.L. Articular Mobility in an African Population. Ann. Rheum. Dis. 1973, 32, 413–418. [Google Scholar] [CrossRef]
- Sanches, S.B.; Oliveira, G.M.; Osório, F.L.; Crippa, J.A.S.; Martín-Santos, R. Hypermobility and Joint Hypermobility Syndrome in Brazilian Students and Teachers of Ballet Dance. Rheumatol. Int. 2015, 35, 741–747. [Google Scholar] [CrossRef]
- Nicholson, L.L.; McKay, M.J.; Baldwin, J.N.; Burns, J.; Cheung, W.; Yip, S.; Chan, C. Is There a Relationship between Sagittal Cervical Spine Mobility and Generalised Joint Hypermobility? A Cross-Sectional Study of 1000 Healthy Australians. Physiotherapy 2021, 112, 150–157. [Google Scholar] [CrossRef]
- Junge, T.; Jespersen, E.; Wedderkopp, N.; Juul-Kristensen, B. Inter-Tester Reproducibility and Inter-Method Agreement of Two Variations of the Beighton Test for Determining Generalised Joint Hypermobility in Primary School Children. BMC Pediatr. 2013, 13, 214. [Google Scholar] [CrossRef]
- Bulbena, A.; Duró, J.C.; Porta, M.; Faus, S.; Vallescar, R.; Martín-Santos, R. Clinical Assessment of Hypermobility of Joints: Assembling Criteria. J. Rheumatol. 1992, 19, 115–122. [Google Scholar]
- Smits-Engelsman, B.; Klerks, M.; Kirby, A. Beighton Score: A Valid Measure for Generalized Hypermobility in Children. J. Pediatr. 2011, 158, 119–123.e4. [Google Scholar] [CrossRef]
- Juul-Kristensen, B.; Rogind, H.; Jensen, D.V.; Remvig, L. Inter-Examiner Reproducibility of Tests and Criteria for Generalized Joint Hypermobility and Benign Joint Hypermobility Syndrome. Rheumatology 2007, 46, 1835–1841. [Google Scholar] [CrossRef]
- Steinberg, N.; Tenenbaum, S.; Zeev, A.; Pantanowitz, M.; Waddington, G.; Dar, G.; Siev-Ner, I. Generalized Joint Hypermobility, Scoliosis, Patellofemoral Pain, and Physical Abilities in Young Dancers. BMC Musculoskelet. Disord. 2021, 22, 161. [Google Scholar] [CrossRef]
- Castori, M.; Tinkle, B.; Levy, H.; Grahame, R.; Malfait, F.; Hakim, A. A Framework for the Classification of Joint Hypermobility and Related Conditions. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 148–157. [Google Scholar] [CrossRef]
- Madden, A.M.; Smith, S. Body Composition and Morphological Assessment of Nutritional Status in Adults: A Review of Anthropometric Variables. J. Hum. Nutr. Diet. 2016, 29, 7–25. [Google Scholar] [CrossRef]
- Heyward, V. ASEP Methods Recommendation: Body Composition Assessment. J. Exerc. Physiol. 2001, 4, 1–12. [Google Scholar]
- Lee, J.S.; Kim, K.B.; Jeong, J.O.; Kwon, N.Y.; Jeong, S.M. Correlation of Foot Posture Index With Plantar Pressure and Radiographic Measurements in Pediatric Flatfoot. Ann. Rehabil. Med. 2015, 39, 10–17. [Google Scholar] [CrossRef]
- Aquino, M.R.C.; Avelar, B.S.; Silva, P.L.; Ocarino, J.M.; Resende, R.A. Reliability of Foot Posture Index Individual and Total Scores for Adults and Older Adults. Musculoskelet. Sci. Pract. 2018, 36, 92–95. [Google Scholar] [CrossRef]
- Redmond, A.C.; Crosbie, J.; Ouvrier, R.A. Development and Validation of a Novel Rating System for Scoring Standing Foot Posture: The Foot Posture Index. Clin. Biomech. 2006, 21, 89–98. [Google Scholar] [CrossRef]
- Vancampfort, D.; Hallgren, M.; Vandael, H.; Probst, M.; Stubbs, B.; Raymaekers, S.; Van Damme, T. Test-Retest Reliability and Clinical Correlates of the Eurofit Test Battery in People with Alcohol Use Disorders. Psychiatry Res. 2019, 271, 208–213. [Google Scholar] [CrossRef]
- Acar, H.; Eler, N. The Effect of Balance Exercises on Speed and Agility in Physical Education Lessons. Univers. J. Educ. Res. 2019, 7, 74–79. [Google Scholar] [CrossRef]
- Karagiannis, C.; Savva, C.; Korakakis, V.; Matheou, I.; Adamide, T.; Georgiou, A.; Xanthos, T. Test–Retest Reliability of Handgrip Strength in Patients with Chronic Obstructive Pulmonary Disease. COPD J. Chronic Obstr. Pulm. Dis. 2020, 17, 568–574. [Google Scholar] [CrossRef]
- Barati, A.; SafarCherati, A.; Aghayari, A.; Azizi, F.; Abbasi, H. Evaluation of Relationship between Trunk Muscle Endurance and Static Balance in Male Students. Asian J. Sports Med. 2013, 4, 34250. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Ewertowska, P.; Trzaskoma, Z.; Sitarski, D.; Gromuł, B.; Haponiuk, I.; Czaprowski, D. Muscle Strength, Muscle Power and Body Composition in College-Aged Young Women and Men with Generalized Joint Hypermobility. PLoS ONE 2020, 15, e0236266. [Google Scholar] [CrossRef]
- Juul-Kristensen, B.; Hansen, H.; Simonsen, E.B.; Alkjær, T.; Kristensen, J.H.; Jensen, B.R.; Remvig, L. Knee Function in 10-Year-Old Children and Adults with Generalised Joint Hypermobility. Knee 2012, 19, 773–778. [Google Scholar] [CrossRef]
- Przymuszała, A.; Gębska, M. Evaluation of Hand Grip Strength and Range of Movement of the Upper Limb in Children with Polyarticular Hypermobility (Ph). J. Educ. Health Sport 2018, 8, 128–138. [Google Scholar] [CrossRef]
- Mitchell, U.H.; Johnson, A.W.; Adams, L.; Kho, J.; Pace, N.; Owen, P.J. Lateral Abdominal Muscles of Adults with Hypermobility May Be Partially Impaired during Contraction. BMJ Open Sport Exerc. Med. 2022, 8, e001343. [Google Scholar] [CrossRef]
- Mebes, C.; Amstutz, A.; Luder, G.; Ziswiler, H.; Stettler, M.; Villiger, P.M.; Radlinger, L. Isometric Rate of Force Development, Maximum Voluntary Contraction, and Balance in Women with and without Joint Hypermobility. Arthritis Care Res. 2008, 59, 1665–1669. [Google Scholar] [CrossRef]
- Aydın, E. Postural Balance Control in Women with Generalized Joint Laxity. Turk. J. Phys. Med. Rehabil. 2017, 63, 259–265. [Google Scholar] [CrossRef]
- Russek, L.N.; Block, N.P.; Byrne, E.; Chalela, S.; Chan, C.; Comerford, M.; Frost, N.; Hennessey, S.; McCarthy, A.; Nicholson, L.L.; et al. Presentation and Physical Therapy Management of Upper Cervical Instability in Patients with Symptomatic Generalized Joint Hypermobility: International Expert Consensus Recommendations. Front. Med. 2023, 9, 1072764. [Google Scholar] [CrossRef]
- Glans, M.; Thelin, N.; Humble, M.B.; Elwin, M.; Bejerot, S. Association between Adult Attention-Deficit Hyperactivity Disorder and Generalised Joint Hypermobility: A Cross-Sectional Case Control Comparison. J. Psychiatr. Res. 2021, 143, 334–340. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Kakaraparthi, V.N.; Reddy, R.S.; Samuel, P.S.; Tedla, J.S.; Rengaramanujam, K.; Ahmad, I.; Sangadala, D.R.; Mukherjee, D. Foot Posture Index Reference Values among Young Adults in Saudi Arabia and Their Association with Anthropometric Determinants, Balance, Functional Mobility, and Hypermobility. BioMed Res. Int. 2021, 2021, 8844356. [Google Scholar] [CrossRef]
- Camerota, F.; Galli, M.; Cimolin, V.; Celletti, C.; Ancillao, A.; Blow, D.; Albertini, G. The Effects of Neuromuscular Taping on Gait Walking Strategy in a Patient with Joint Hypermobility Syndrome/Ehlers–Danlos Syndrome Hypermobility Type. Ther. Adv. Musculoskelet. Dis. 2015, 7, 3–10. [Google Scholar] [CrossRef]
- Barber Foss, K.D.; Ford, K.R.; Myer, G.D.; Hewett, T.E. Generalized Joint Laxity Associated With Increased Medial Foot Loading in Female Athletes. J. Athl. Train. 2009, 44, 356–362. [Google Scholar] [CrossRef]
- Antonio, D.H.; Magalhaes, C.S. Survey on Joint Hypermobility in University Students Aged 18–25 Years Old. Adv. Rheumatol. 2018, 58, 3. [Google Scholar] [CrossRef]
- Karaman, Ç.A.; Zeren, E.; Maral, F.; Parlak, M.; KiRazli, Ö.; Boraci, H.; Zeren, M.; AriFoğlu, Y. The Effect of Hypermobility on Pain and Quality of Life in Young Adults. Bezmialem. Sci. 2022, 10, 749–755. [Google Scholar] [CrossRef]
- Palmer, S.; Macconnell, S.; Willmore, A. Ability of the Bristol Impact of Hypermobility Questionnaire to Discriminate between People with and without Joint Hypermobility Syndrome: A Known-group Validity Study. Musculoskelet. Care 2020, 18, 29–36. [Google Scholar] [CrossRef]

| GJH | Non-GJH | ||||
|---|---|---|---|---|---|
| n = 26 | n = 41 | ||||
| 5.29 (5–7) | 1.8 (0–4) | ||||
| Mean (SD) | Me (IQR) | Mean (SD) | Me (IQR) | U, Z, p Value | |
| Age (years) | 20.06 (1.2) | 20 (19–21) | 20.15 (2.2) | 19.5 (19–21) | 462.5; −0.949; 0.343 |
| Height (cm) | 168.5 (5.2) | 168 (165–172) | 168.4 (6.7) | 169 (165–173) | 500; −0.425; 0.671 |
| Weight (kg) | 59.81 (6.16) | 59.6 (55.2–63.25) | 60.96 (8.76) | 59.3 (56.05–64.2) | 516; −0.219; 0.827 |
| BMI (kg/m2) | 21.1 (1.8) | 20.55 (19.45–22.92) | 21.5 (2.39) | 21 (19.57–22.15) | 520; −0.167; 0.867 |
| GJH | Non-GJH | |||||
|---|---|---|---|---|---|---|
| n = 26 | n = 41 | |||||
| Mean (SD) | Me (IQR) | Mean (SD) | Me (IQR) | U, Z, p Value | r | |
| Sit and reach test (cm) | 33.28 (5.05) | 32.7 (30–37.5) | 26.5 (7.56) | 28 (21–31.5) | 252; −3.62; <0.001 | 0.442 |
| Flamingo balance test (attempts) | 9.73 (5.2) | 9 (6–12) | 6.6 (4.4) | 6 (3–9) | 334.5; −2.562; 0.01 | 0.313 |
| Handgrip strength test (kg) | 29.95 (4.76) | 29.5 (26–33) | 30.85 (5.82) | 31 (26–35.5) | 459; −0.955; 0.34 | 0.117 |
| Standing broad jump test (m) | 1.56 (0.24) | 1.61 (1.35–1.69) | 1.64 (0.2) | 1.7 (1.56–1.77) | 397.5; −1.744; 0.081 | 0.213 |
| Abdomen muscle static strength endurance test (s) | 197.6 (103) | 210 (82–300) | 201 (104.74) | 240 (82–300) | 513.5; −0.262; 0.793 | 0.032 |
| Back muscle static strength endurance test (s) | 208.65 (70.7) | 192.5 (166–300) | 242.66 (76.75) | 300 (205–300) | 368; −2.206; 0.027 | 0.269 |
| GJH | Non-GJH | |||||
|---|---|---|---|---|---|---|
| n = 26 | n = 41 | |||||
| Mean (SD) | Me (IQR) | Mean (SD) | Me (IQR) | U, Z, p Value | r | |
| Physical functioning | 95 (6.48) | 95 (90–100) | 95.6 (6.34) | 95 (95–100) | 483; −0.693; 0.488 | 0.084 |
| Physical limitation | 92 (17.26) | 100 (87.5–100) | 92.1 (14.19) | 100 (75–100) | 513.5; −0.342; 0.741 | 0.04 |
| Bodily pain | 85.54 (19.08) | 89 (78–100) | 82.54 (18.66) | 89 (72.5–100) | 462; −0.951; 0.342 | 0.116 |
| General health | 76.6 (16.38) | 75 (67.5–75) | 72.2 (14.71) | 75 (60–85) | 456.5; −0.991; 0.321 | 0.121 |
| Vitality | 62.31 (17.16) | 65 (53.75–76.25) | 66.7 (12.74) | 65 (57.5–77.5) | 478.5; −0.706; 0.48 | 0.086 |
| Social functioning | 85.92 (22.18) | 94.5 (78–100) | 89.6 (10.1) | 89 (78–100) | 508; −0.342; 0.732 | 0.042 |
| Emotional limitation | 88.48 (23.21) | 100 (94.5–100) | 90 (21.4) | 100 (100–100) | 418; −1.495; 0.135 | 0.182 |
| Mental health | 74.4 (19.46) | 80 (64–82) | 70.15 (14.29) | 76 (60–80) | 504; −0.15; 0.88 | 0.018 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aukštuolytė-Bačienė, E.; Daunoravičienė, A.; Tamulionytė, V.; Berškienė, K.; Narbutaitė, J.; Razon, S.; Slapšinskaitė-Dackevičienė, A. Present but Ignored: Physical Condition and Health-Related Quality of Life in College-Aged Females with Generalized Joint Hypermobility. Healthcare 2024, 12, 1065. https://doi.org/10.3390/healthcare12111065
Aukštuolytė-Bačienė E, Daunoravičienė A, Tamulionytė V, Berškienė K, Narbutaitė J, Razon S, Slapšinskaitė-Dackevičienė A. Present but Ignored: Physical Condition and Health-Related Quality of Life in College-Aged Females with Generalized Joint Hypermobility. Healthcare. 2024; 12(11):1065. https://doi.org/10.3390/healthcare12111065
Chicago/Turabian StyleAukštuolytė-Bačienė, Ernesta, Algė Daunoravičienė, Vilma Tamulionytė, Kristina Berškienė, Jurgita Narbutaitė, Selen Razon, and Agnė Slapšinskaitė-Dackevičienė. 2024. "Present but Ignored: Physical Condition and Health-Related Quality of Life in College-Aged Females with Generalized Joint Hypermobility" Healthcare 12, no. 11: 1065. https://doi.org/10.3390/healthcare12111065
APA StyleAukštuolytė-Bačienė, E., Daunoravičienė, A., Tamulionytė, V., Berškienė, K., Narbutaitė, J., Razon, S., & Slapšinskaitė-Dackevičienė, A. (2024). Present but Ignored: Physical Condition and Health-Related Quality of Life in College-Aged Females with Generalized Joint Hypermobility. Healthcare, 12(11), 1065. https://doi.org/10.3390/healthcare12111065








