Can Clinical Assessment of Postural Control Explain Locomotive Body Function, Mobility, Self-Care and Participation in Children with Cerebral Palsy?
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size
2.2. Participants
2.3. Procedure
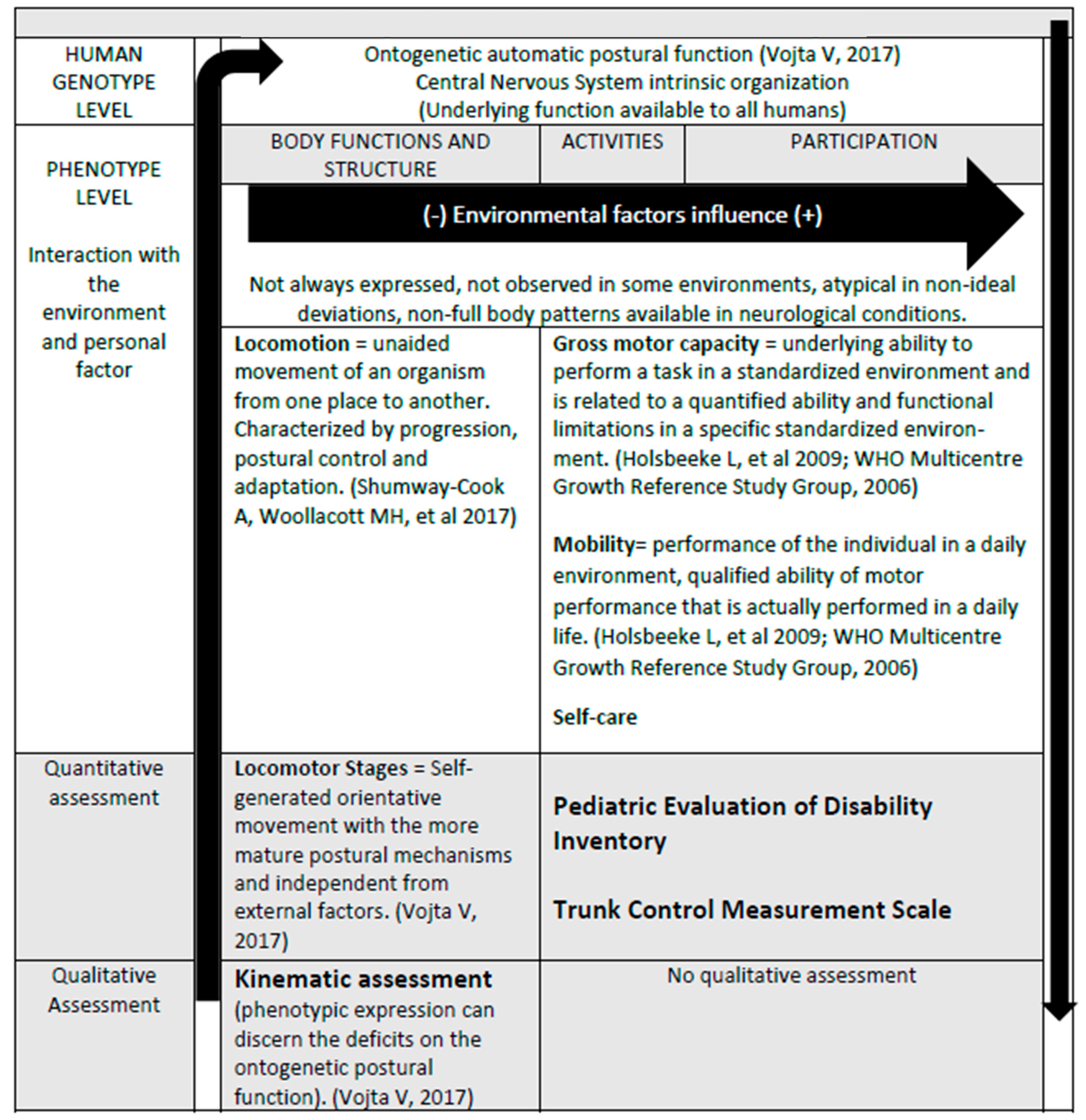
2.4. Outcomes
2.4.1. Locomotor Stages According to Vojta
2.4.2. PEDI
2.4.3. TCMS
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Ontogenetic and Automatic Postural Body Function
4.2. Locomotor Ontogenic Stages vs. Motor Milestones
4.3. Manual Function in Self-Care and Locomotion
4.4. Clinical Implications and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sanz-Mengibar, J.M.; Altschuck, N.; Sanchez-de-Muniain, P.; Bauer, C.; Santonja-Medina, F. Position between trunk and pelvis during gait depending on the gross motor function classification system. Pediatr. Phys. Ther. 2017, 29, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control: Translating Research Into Clinical Practice. Wolters Kluwer: Philadelphia, PA, USA, 2017. [Google Scholar]
- Bosserman, J.; Kelkar, S.; LeBlond, K.D.; Cassidy, J.; McCarty, D.B. Postural Control Measurements to Predict Future Motor Impairment in Preterm Infants: A Systematic Review. Diagnostics 2023, 13, 3473. [Google Scholar] [CrossRef] [PubMed]
- Horak, F.B.; Macpherson, J.M. Postural Orientation and Equilibrium. In Handbook of Physiology, Section 12. Exercise: Regulation and Integration of Multiple Systems; Rowell, L.B., Sheperd, J.T., Eds.; Oxford University Press: New York, NY, USA, 1996; pp. 255–292. [Google Scholar]
- Palisano, R.J.; Hanna, S.E.; Rosenbaum, P.L.; Tieman, B. Probability of walking, wheeled mobility, and assisted mobility in children and adolescents with cerebral palsy. Dev. Med. Child. Neurol. 2010, 52, 66–71. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF); WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Holsbeeke, L.; Ketelaar, M.; Schoemaker, M.M.; Gorter, J.W. Capacity, capability, and performance: Different constructs or three of a kind? Arch. Phys. Med. Rehabil. 2009, 90, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Sanz Mengibar, J.M.; Santonja-Medina, F.; Sanchez-de-Muniain, P.; Canteras-Jordana, M. Can Clinical Assessment of Locomotive Body Function Explain Gross Motor Environmental Performance in Cerebral Palsy? J. Child. Neurol. 2016, 31, 474–480. [Google Scholar] [CrossRef]
- Kim, K.; Kang, J.Y.; Jang, D.H. Relationship Between Mobility and Self-Care Activity in Children With Cerebral Palsy. Ann. Rehabil. Med. 2017, 41, 266–272. [Google Scholar] [CrossRef]
- Bartlett, D.J.; Chiarello, L.A.; McCoy, S.W.; Palisano, R.J.; Jeffries, L.; Fiss, A.L.; Wilk, P. Determinants of self-care participation of young children with cerebral palsy. Dev. Neurorehabil. 2014, 17, 403–413. [Google Scholar] [CrossRef]
- Ostensjø, S.; Carlberg, E.B.; Vøllestad, N.K. Everyday functioning in young children with cerebral palsy: Functional skills, caregiver assistance, and modifications of the environment. Dev. Med. Child. Neurol. 2003, 45, 603–612. [Google Scholar] [CrossRef]
- Voorman, J.M.; Dallmeijer, A.J.; Schuengel, C.; Knol, D.L.; Lankhorst, G.J.; Becher, J.G. Activities and participation of 9- to 13-year-old children with cerebral palsy. Clin. Rehabil. 2006, 20, 937–948. [Google Scholar] [CrossRef]
- Lepage, C.; Noreau, L.; Bernard, P.M. Association between characteristics of locomotion and accomplishment of life habits in children with cerebral palsy. Phys. Ther. 1998, 78, 458–469. [Google Scholar] [CrossRef]
- Palisano, R.J.; Kang, L.J.; Chiarello, L.A.; Orlin, M.; Oeffinger, D.; Maggs, J. Social and community participation of children and youth with cerebral palsy is associated with age and gross motor function classification. Phys. Ther. 2009, 89, 1304–1314. [Google Scholar] [CrossRef] [PubMed]
- van Gorp, M.; Roebroeck, M.E.; Swan Tan, S.; de Groot, V.; Gorter, J.W.; Smits, D.W.; Schmidt, A.K.; Dallmeijer, A.J.; PERRIN DECADE Study Group. Activity Performance Curves of Individuals with Cerebral Palsy. Pediatrics 2018, 142, e20173723. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Boyd, R.N.; Ziviani, J.; Ware, R.S.; Sakzewski, L. Self-care and manual ability in preschool children with cerebral palsy: A longitudinal study. Dev. Med. Child. Neurol. 2019, 61, 570–578. [Google Scholar] [CrossRef]
- James, S.; Ziviani, J.; Ware, R.S.; Boyd, R.N. Relationships between activities of daily living, upper limb function, and visual perception in children and adolescents with unilateral cerebral palsy. Dev. Med. Child. Neurol. 2015, 57, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Öhrvall, A.M.; Eliasson, A.C.; Löwing, K.; Ödman, P.; Krumlinde-Sundholm, L. Self-care and mobility skills in children with cerebral palsy, related to their manual ability and gross motor function classifications. Dev. Med. Child. Neurol. 2010, 52, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
- Gunel, M.K.; Mutlu, A.; Tarsuslu, T.; Livanelioglu, A. Relationship among the Manual Ability Classification System (MACS), the Gross Motor Function Classification System (GMFCS), and the functional status (WeeFIM) in children with spastic cerebral palsy. Eur. J. Pediatr. 2009, 168, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Carnahan, K.D.; Arner, M.; Hägglund, G. Association between gross motor function (GMFCS) and manual ability (MACS) in children with cerebral palsy. A population-based study of 359 children. BMC Musculoskelet. Disord. 2007, 8, 50. [Google Scholar] [CrossRef]
- Sanz-Mengibar, J.M.; Menendez Pardinas, M.; Santonja-Medina, F. Is the implementation of Vojta Therapy associated with faster gross motor development in children with cerebral palsy. Ideggyogy Sz = Clin. Neurosci. 2021, 74, 329–336. [Google Scholar] [CrossRef]
- Sanz-Mengibar, J.M.; Santonja-Medina, F. Role of positioning between trunk and pelvis in locomotor function of ambulant children with and without cerebral palsy. Ideggyogy Sz = Clin. Neurosci. 2019, 72, 343–351. [Google Scholar] [CrossRef]
- Nichols, D.S.; Case-Smith, J. Reliability and Validity of the Pediatric Evaluation of Disability Inventory. Pediatr. Phys. Ther. 1996, 8, 15–24. [Google Scholar] [CrossRef]
- Scott, K.; Lewis, J.; Pan, X.; Heathcock, J. Parent-Reported PEDI-CAT Mobility and Gross Motor Function in Infants With Cerebral Palsy. Pediatr. Phys. Ther. 2021, 33, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.L.; Walter, S.D.; Hanna, S.E.; Palisano, R.J.; Russell, D.J.; Raina, P.; Wood, E.; Bartlett, D.J.; Galuppi, B.E. Prognosis for Gross Motor Function in Cerebral Palsy: Creation of Motor Development Curves. JAMA 2002, 288, 1357–1363. [Google Scholar] [CrossRef] [PubMed]
- Surveillance of Cerebral Palsy in Europe. SCPE: A collaboration of cerebral palsy surveys and registers. Dev. Med. Child. Neurol. 2000, 42, 816–824. [Google Scholar] [CrossRef]
- Bax, M.; Goldstein, M.; Rosenbaum, P.; Leviton, A.; Paneth, N.; Dan, B.; Jacobsson, B.; Damiano, D. Executive Committee for the Definition of Cerebral Palsy. Proposed definition and classification of cerebral palsy. Dev. Med. Child. Neurol. 2005, 47, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Smits, D.W.; Gorter, J.W.; Ketelaar, M.; Van Schie, P.E.; Dallmeijer, A.J.; Lindeman, E.; Jongmans, M.J. Relationship between gross motor capacity and daily-life mobility in children with cerebral palsy. Dev. Med. Child. Neurol. 2010, 52, e60–e66. [Google Scholar] [CrossRef]
- Smits, D.W.; Ketelaar, M.; Gorter, J.W.; van Schie, P.; Dallmeijer, A.; Jongmans, M.; Lindeman, E. Development of daily activities in school-age children with cerebral palsy. Res. Dev. Disabil. 2011, 32, 222–234. [Google Scholar] [CrossRef]
- Ostensjo, S.; Carlberg, E.B.; Vøllestad, N.K. Motor impairments in young children with cerebral palsy: Relationship to gross motor function and everyday activities. Dev. Med. Child. Neurol. 2004, 46, 580–589. [Google Scholar] [CrossRef]
- Kretch, K.S.; Willett, S.L.; Hsu, L.Y.; Sargent, B.A.; Harbourne, R.T.; Dusing, S.C. “Learn the Signs. Act Early.”: Updates and Implications for Physical Therapists. Pediatr. Phys. Ther. 2022, 34, 440–448. [Google Scholar] [CrossRef]
- WHO Multicentre Growth Reference Study Group. WHO Motor Development Study: Windows of achievement for six gross motor development milestones. Acta Paediatr. Suppl. 2006, 450, 86–95. [Google Scholar]
- Vojta, V. Die Zerebralen Bewegungsstörungen im Sug ling-salter: Fruhdiagnose und Frutherapie [Pediatric Motor Disorders: Early Diagnosis and Treatment], 9th ed.; Ferdinand Enke Verlag Editors: Stuttgart, Germany, 2017. (In German) [Google Scholar]
- Maurer-Burkhard, B.; Smoor, I.; von Reumont, A.; Deckstein, G.; Stierle, I.; Rupp, R.; Schuld, C. Validity and reliability of a locomotor stage-based functional rating scale in spinal cord injury. Spinal Cord. 2016, 54, 619–625. [Google Scholar] [CrossRef]
- Iyer, L.V.; Haley, S.M.; Watkins, M.P.; Dumas, H.M. Establishing minimal clinically important differences for scores on the pediatric evaluation of disability inventory for inpatient rehabilitation. Phys. Ther. 2003, 83, 888–898. [Google Scholar] [CrossRef] [PubMed]
| n = 25 | Level | Quantity | % | |
|---|---|---|---|---|
| Gross Motor | I | 7 | 28 | |
| Function | II | 6 | 24 | |
| Classification | III | 6 | 24 | |
| System | IV | 3 | 12 | |
| (GMFCS) | V | 3 | 12 | |
| Locomotor | 0 | 0 | 0 | |
| Stages | 1 | 3 | 12 | |
| 2 | 0 | 0 | ||
| 3 | 0 | 0 | ||
| 4 | 2 | 8 | ||
| 5 | 1 | 4 | ||
| 6 | 4 | 16 | ||
| 7 | 5 | 20 | ||
| 8 | 7 | 28 | ||
| 9 | 3 | 12 | ||
| Cerebral | Bilateral | Quadriparesis | 5 | 20 |
| Palsy | Diparesis | 11 | 44 | |
| Subtypes | Triparesis | 1 | 4 | |
| Unilateral | Hemiparesis | 8 | 32 | |
| TCMS | PEDI | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Subject Number | GMFCS | LS | Static Sitting Balance TCMS (20) | Selective Control TCSM (28) | Dynamic Range TCMS (10) | TCSM Overall Score (58) | Scaled Score Self-Sufficiency | Scaled Score Mobility | Scaled Score Social Features |
| 1. | III | 6 | 11 | 6 | 3 | 20 | 60.5 | 52.2 | 64.1 |
| 2. | IV | 4 | 8 | 4 | 3 | 15 | 59.9 | 30.6 | 82.2 |
| 3. | III | 7 | 13 | 11 | 7 | 31 | 100 | 85.2 | 82.2 |
| 4. | IV | 5 | 6 | 3 | 3 | 12 | 57.4 | 37.1 | 66.2 |
| 5. | I | 6 | 10 | 9 | 6 | 25 | 62.5 | 79.8 | 82.2 |
| 6. | III | 6 | 13 | 17 | 9 | 39 | 85.1 | 63.9 | 89.1 |
| 7. | V | 1 | 0 | 0 | 0 | 0 | 35.1 | 0.0 | 53.2 |
| 8. | V | 1 | 3 | 1 | 4 | 8 | 43.6 | 49.7 | 38.8 |
| 9. | II | 7 | 18 | 9 | 8 | 35 | 60.5 | 79.8 | 77.3 |
| 10. | I | 7 | 13 | 11 | 6 | 30 | 70.8 | 94.2 | 67.4 |
| 11. | II | 7 | 18 | 12 | 5 | 35 | 100.0 | 89.2 | 96.3 |
| 12. | III | 8 | 16 | 9 | 3 | 28 | 59.3 | 54.8 | 73.4 |
| 13. | I | 8 | 13 | 12 | 3 | 28 | 69.1 | 77.3 | 65.1 |
| 14. | V | 1 | 0 | 0 | 0 | 0 | 30.7 | 6.1 | 35.1 |
| 15. | II | 8 | 20 | 11 | 7 | 38 | 68.3 | 94.2 | 82.2 |
| 16. | II | 8 | 20 | 10 | 6 | 36 | 63.2 | 61.9 | 82.2 |
| 17. | IV | 4 | 3 | 2 | 0 | 5 | 43.6 | 46.1 | 49.7 |
| 18. | III | 7 | 20 | 15 | 9 | 44 | 63.2 | 61.9 | 82.2 |
| 19. | II | 8 | 20 | 13 | 6 | 39 | 54.3 | 68.7 | 59.9 |
| 20. | I | 9 | 20 | 18 | 8 | 46 | 100 | 100 | 100 |
| 21. | III | 6 | 14 | 6 | 0 | 20 | 65.2 | 77.3 | 89.1 |
| 22. | I | 9 | 20 | 15 | 9 | 44 | 100 | 100 | 100 |
| 23. | I | 9 | 20 | 16 | 8 | 44 | 100 | 100 | 100 |
| 24. | I | 8 | 20 | 16 | 10 | 46 | 100 | 100 | 100 |
| 25. | II | 8 | 20 | 14 | 9 | 43 | 81.4 | 65.0 | 68.9 |
| LS | TCMS Overall Score | PEDI Self-Care | Mobility | Participation | ||
|---|---|---|---|---|---|---|
| PEDI | ||||||
| Self-Care | 0.68 * | 0.76 * | 0.84 * | |||
| Mobility | 0.75 * | 0.75 * | 0.72 * | |||
| Participation | 0.58 * | 0.72 * | 0.83 * | |||
| TCMS | 0.84 * | |||||
| Static sitting balance | 0.89 * | 0.64 * | 0.69 * | 0.64 * | ||
| Selective control | 0.79 * | 0.82 * | 0.74 * | 0.70 * | ||
| Dynamic range | 0.63 * | 0.69 * | 0.66 * | 0.62 * | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vlčkova, B.; Halámka, J.; Müller, M.; Sanz-Mengibar, J.M.; Šafářová, M. Can Clinical Assessment of Postural Control Explain Locomotive Body Function, Mobility, Self-Care and Participation in Children with Cerebral Palsy? Healthcare 2024, 12, 98. https://doi.org/10.3390/healthcare12010098
Vlčkova B, Halámka J, Müller M, Sanz-Mengibar JM, Šafářová M. Can Clinical Assessment of Postural Control Explain Locomotive Body Function, Mobility, Self-Care and Participation in Children with Cerebral Palsy? Healthcare. 2024; 12(1):98. https://doi.org/10.3390/healthcare12010098
Chicago/Turabian StyleVlčkova, Blanka, Jiří Halámka, Markus Müller, Jose Manuel Sanz-Mengibar, and Marcela Šafářová. 2024. "Can Clinical Assessment of Postural Control Explain Locomotive Body Function, Mobility, Self-Care and Participation in Children with Cerebral Palsy?" Healthcare 12, no. 1: 98. https://doi.org/10.3390/healthcare12010098
APA StyleVlčkova, B., Halámka, J., Müller, M., Sanz-Mengibar, J. M., & Šafářová, M. (2024). Can Clinical Assessment of Postural Control Explain Locomotive Body Function, Mobility, Self-Care and Participation in Children with Cerebral Palsy? Healthcare, 12(1), 98. https://doi.org/10.3390/healthcare12010098


_MD__MPH_PhD.png)



