Psychological, Pain, and Disability Factors Influencing the Perception of Improvement/Recovery from Physiotherapy in Patients with Chronic Musculoskeletal Pain: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedure
2.4. Variables
2.4.1. Main Variable
- Overall perception of improvement
2.4.2. Secondary Variables
- Disability
- Therapeutic alliance in physiotherapy
- Treatment adherence
- Self-efficacy when dealing with chronic pain
- Fear of movement
- Pain catastrophism
2.5. Sample Size Calculation
2.6. Statistical Analysis
- Homogeneity was evaluated visually using a residual versus fitted values plot. The spread of residuals was random without discernible patterns or funnel shapes, indicating homogeneity of variance.
- The assumption of the Independence of observations was tested using the Durbin–Watson statistic, which helps detect autocorrelation in the residuals of regression analysis. A Durbin–Watson statistic value close to 2.0 suggested no evidence of autocorrelation in our model.
- To assess the Normality of the distribution, Q-Q plots of the residuals were examined. The residuals approximated a straight line, which is consistent with a normal distribution.
- Linearity was verified through an analysis of scatter plots comparing observed versus predicted values, as well as through the examination of normal P-P plots of standardized residuals. These plots demonstrated a linear relationship, affirming the linearity assumption of our model.
3. Results
3.1. Correlation Analysis
3.2. Regression Analysis
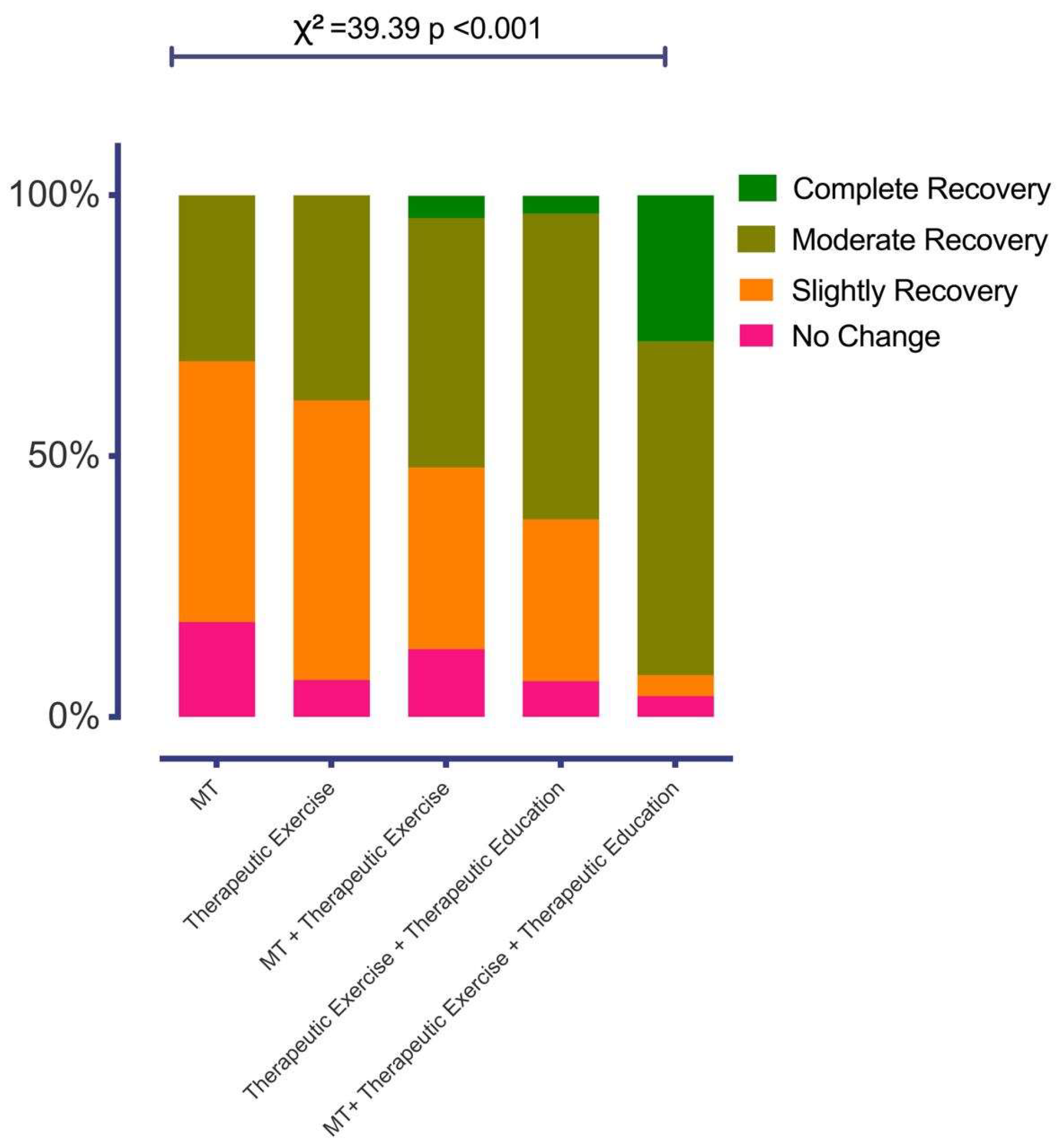
3.3. Contingency Table Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Deshpande, P.R.; Rajan, S.; Sudeepthi, B.L.; Abdul Nazir, C.P. Patient-Reported Outcomes: A New Era in Clinical Research. Perspect. Clin. Res. 2011, 2, 137. [Google Scholar] [CrossRef] [PubMed]
- Bobos, P.; MacDermid, J.; Nazari, G.; Furtado, R. Psychometric Properties of the Global Rating of Change Scales in Patients with Neck Disorders: A Systematic Review with Meta-Analysis and Meta-Regression. BMJ Open 2019, 9, e033909. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Ostelo, R.W.J.G.; Knol, D.L.; Maher, C.G.; de Vet, H.C.W.; Hancock, M.J. Global Perceived Effect Scales Provided Reliable Assessments of Health Transition in People with Musculoskeletal Disorders, but Ratings Are Strongly Influenced by Current Status. J. Clin. Epidemiol. 2010, 63, 760–766.e1. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Maher, C.G.; Mackay, G. Global Rating of Change Scales: A Review of Strengths and Weaknesses and Considerations for Design. J. Man. Manip. Ther. 2009, 17, 163–170. [Google Scholar] [CrossRef]
- Bobos, P.; Ziebart, C.; Furtado, R.; Lu, Z.; MacDermid, J.C. Psychometric Properties of the Global Rating of Change Scales in Patients with Low Back Pain, Upper and Lower Extremity Disorders. A Systematic Review with Meta-Analysis. J. Orthop. 2020, 21, 40–48. [Google Scholar] [CrossRef]
- Garrison, J.C.; Shanley, E.; Thigpen, C.; Hegedus, E.; Cook, C. Between-Session Changes Predict Overall Perception of Improvement but Not Functional Improvement in Patients with Shoulder Impingement Syndrome Seen for Physical Therapy: An Observational Study. Physiother. Theory Pract. 2011, 27, 137–145. [Google Scholar] [CrossRef]
- Swanenburg, J.; Gruber, C.; Brunner, F.; Wirth, B. Patients’ and Therapists’ Perception of Change Following Physiotherapy in an Orthopedic Hospital’s Outpatient Clinic. Physiother. Theory Pract. 2015, 31, 293–298. [Google Scholar] [CrossRef]
- Schmitt, J.; Fabio, R.P.D. The Validity of Prospective and Retrospective Global Change Criterion Measures. Arch. Phys. Med. Rehabil. 2005, 86, 2270–2276. [Google Scholar] [CrossRef]
- Schmitt, J.S.; Abbott, J.H. Patient Global Ratings of Change Did Not Adequately Reflect Change over Time: A Clinical Cohort Study. Phys. Ther. 2014, 94, 534–542. [Google Scholar] [CrossRef]
- Garrison, C.; Cook, C. Clinimetrics Corner: The Global Rating of Change Score (GRoC) Poorly Correlates with Functional Measures and Is Not Temporally Stable. J. Man. Manip. Ther. 2012, 20, 178–181. [Google Scholar] [CrossRef]
- Schmitt, J.; Abbott, J.H. Global Ratings of Change Do Not Accurately Reflect Functional Change Over Time in Clinical Practice. J. Orthop. Sports Phys. Ther. 2015, 45, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Wolfensberger, A.; Vuistiner, P.; Konzelmann, M.; Plomb-Holmes, C.; Léger, B.; Luthi, F. Clinician and Patient-Reported Outcomes Are Associated With Psychological Factors in Patients With Chronic Shoulder Pain. Clin. Orthop. Relat. Res. 2016, 474, 2030. [Google Scholar] [CrossRef] [PubMed]
- Scott, W.; McCracken, L.M. Patients’ Impression of Change Following Treatment for Chronic Pain: Global, Specific, a Single Dimension, or Many? J. Pain 2015, 16, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Vanhaudenhuyse, A.; Gillet, A.; Malaise, N.; Salamun, I.; Grosdent, S.; Maquet, D.; Nyssen, A.-S.; Faymonville, M.-E. Psychological Interventions Influence Patients’ Attitudes and Beliefs about Their Chronic Pain. J. Tradit. Complement. Med. 2018, 8, 296–302. [Google Scholar] [CrossRef] [PubMed]
- da Fonseca Pires, D.A.; Cruz, E.J.C.B.; de Matos Canhão, H.C.; Nunes, C.D.R.D. The Role of Pain and Disability Changes after Physiotherapy Treatment on Global Perception of Improvement in Patients with Chronic Low Back Pain. Musculoskelet. Sci. Pract. 2020, 47, 102139. [Google Scholar] [CrossRef]
- Fischer, D.; Stewart, A.L.; Bloch, D.A.; Lorig, K.; Laurent, D.; Holman, H. Capturing the Patient’s View of Change as a Clinical Outcome Measure. JAMA 1999, 282, 1157–1162. [Google Scholar] [CrossRef]
- Perrot, S.; Lantéri-Minet, M. Patients’ Global Impression of Change in the Management of Peripheral Neuropathic Pain: Clinical Relevance and Correlations in Daily Practice. Eur. J. Pain 2019, 23, 1117–1128. [Google Scholar] [CrossRef]
- Kinney, M.; Seider, J.; Beaty, A.F.; Coughlin, K.; Dyal, M.; Clewley, D. The Impact of Therapeutic Alliance in Physical Therapy for Chronic Musculoskeletal Pain: A Systematic Review of the Literature. Physiother Theory Pract. 2020, 36, 886–898. [Google Scholar] [CrossRef]
- Lawford, B.J.; Bennell, K.L.; Campbell, P.K.; Kasza, J.; Hinman, R.S. Association Between Therapeutic Alliance and Outcomes Following Telephone-Delivered Exercise by a Physical Therapist for People With Knee Osteoarthritis: Secondary Analyses From a Randomized Controlled Trial. JMIR Rehabil. Assist. Technol. 2021, 8, e23386. [Google Scholar] [CrossRef]
- Burns, D.; Boyer, P.; Razmjou, H.; Richards, R.; Whyne, C. Adherence Patterns and Dose Response of Physiotherapy for Rotator Cuff Pathology: Longitudinal Cohort Study. JMIR Rehabil. Assist. Technol. 2021, 8, e21374. [Google Scholar] [CrossRef]
- López-de-Uralde-Villanueva, I.; Beltran-Alacreu, H.; Fernández-Carnero, J.; La Touche, R. Pain Management Using a Multimodal Physiotherapy Program Including a Biobehavioral Approach for Chronic Nonspecific Neck Pain: A Randomized Controlled Trial. Physiother. Theory Pract. 2020, 36, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Grande-Alonso, M.; Suso-Martí, L.; Cuenca-Martínez, F.; Pardo-Montero, J.; Gil-Martínez, A.; La Touche, R. Physiotherapy Based on a Biobehavioral Approach with or Without Orthopedic Manual Physical Therapy in the Treatment of Nonspecific Chronic Low Back Pain: A Randomized Controlled Trial. Pain Med. 2019, 20, 2571–2587. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sanz, J.; Malo-Urriés, M.; Corral-de-Toro, J.; López-de-Celis, C.; Lucha-López, M.O.; Tricás-Moreno, J.M.; Lorente, A.I.; Hidalgo-García, C. Does the Addition of Manual Therapy Approach to a Cervical Exercise Program Improve Clinical Outcomes for Patients with Chronic Neck Pain in Short- and Mid-Term? A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 6601. [Google Scholar] [CrossRef] [PubMed]
- Pires, D.; Cruz, E.B.; Costa, D.; Nunes, C. Beyond Pain and Disability: An Explanatory Mixed Methods Study Exploring Outcomes after Physiotherapy Intervention in Patients with Chronic Low Back Pain. Disabil. Rehabil. 2022, 44, 881–890. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A Classification of Chronic Pain for ICD-11. Pain 2015, 156, 1003. [Google Scholar] [CrossRef]
- Perrot, S.; Cohen, M.; Barke, A.; Korwisi, B.; Rief, W.; Treede, R.-D.; Pain, T.I.T. for the C. of C. The IASP Classification of Chronic Pain for ICD-11: Chronic Secondary Musculoskeletal Pain. Pain 2019, 160, 77. [Google Scholar] [CrossRef]
- Ferrer-Peña, R.; Gil-Martínez, A.; Pardo-Montero, J.; Jiménez-Penick, V.; Gallego-Izquierdo, T.; La Touche, R. Adaptación y Validación de La Escala de Gradación Del Dolor Crónico al Español. Reumatol. Clínica 2016, 12, 130–138. [Google Scholar] [CrossRef]
- Gómez-Pérez, L.; López-Martínez, A.E.; Ruiz-Párraga, G.T. Psychometric Properties of the Spanish Version of the Tampa Scale for Kinesiophobia (TSK). J. Pain 2011, 12, 425–435. [Google Scholar] [CrossRef]
- García Campayo, J.; Rodero, B.; Alda, M.; Sobradiel, N.; Montero, J.; Moreno, S. Validation of the Spanish version of the Pain Catastrophizing Scale in fibromyalgia. Med. Clin. 2008, 131, 487–492. [Google Scholar] [CrossRef]
- Martín-Aragón Gelabert, M.; Pastor-Mira, M.Á.; Rodríguez Marín, J.; March, M.J.; Lledó Boyer, A.; López Roig, S.; Terol Cantero, M. del C. Percepción de autoeficacia en dolor crónico. Adaptación y validación de la chronic pain selfefficacy scale. Rev. De Psicol. De La Salud 1999, 11, 51–75. [Google Scholar]
- Linares-Fernández, M.T.; La Touche, R.; Pardo-Montero, J. Development and Validation of the Therapeutic Alliance in Physiotherapy Questionnaire for Patients with Chronic Musculoskeletal Pain. Patient Educ. Couns. 2021, 104, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Del Corral, T.; La Touche, R.; Cebrià I Iranzo, M.À.; Olmos, R.; Blanco-Royano, F.; López-de-Uralde-Villanueva, I. Development and Validation of the AdT-Physio Scale: A Tool to Assess Adherence and Perception of Physical Therapist Intervention in Patients With Cystic Fibrosis. Phys. Ther. 2020, 100, 2063–2074. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S. Global Rating of Change Scales. Aust. J. Physiother. 2009, 55, 289. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; Steyerberg, E.W. The Number of Subjects per Variable Required in Linear Regression Analyses. J. Clin. Epidemiol. 2015, 68, 627–636. [Google Scholar] [CrossRef]
- Witz, K. Review of Applied Statistics for the Behavioral Sciences. J. Educ. Stat. 1990, 15, 84–87. [Google Scholar] [CrossRef]
- Belsley, D.A. Conditioning Diagnostics: Collinearity and Weak Data in Regression; Wiley: New York, NY, USA, 1991; ISBN 978-0-471-52889-0. [Google Scholar]
- Campbell, P.; Bishop, A.; Dunn, K.M.; Main, C.J.; Thomas, E.; Foster, N.E. Conceptual Overlap of Psychological Constructs in Low Back Pain. Pain 2013, 154, 1783–1791. [Google Scholar] [CrossRef]
- Meisingset, I.; Stensdotter, A.K.; Woodhouse, A.; Vasseljen, O. Predictors for Global Perceived Effect after Physiotherapy in Patients with Neck Pain: An Observational Study. Physiotherapy 2018, 104, 400–407. [Google Scholar] [CrossRef]
- Evans, R.; Bronfort, G.; Maiers, M.; Schulz, C.; Hartvigsen, J. “I Know It’s Changed”: A Mixed-Methods Study of the Meaning of Global Perceived Effect in Chronic Neck Pain Patients. Eur. Spine J. 2014, 23, 888–897. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Tarasuk, V.; Katz, J.N.; Wright, J.G.; Bombardier, C. “Are You Better?” A Qualitative Study of the Meaning of Recovery. Arthritis Rheum 2001, 45, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core Outcome Measures for Chronic Pain Clinical Trials: IMMPACT Recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Rojas, A.E.; González, J.M.; Fuertes, J.N. The Bond of the Working Alliance. In Working Alliance Skills for Mental Health Professionals; Fuertes, J.N., Ed.; Oxford University Press: Oxford, UK, 2019; ISBN 978-0-19-086852-9. [Google Scholar]
- Babatunde, F.; MacDermid, J.; MacIntyre, N. Characteristics of Therapeutic Alliance in Musculoskeletal Physiotherapy and Occupational Therapy Practice: A Scoping Review of the Literature. BMC Health Serv. Res. 2017, 17, 375. [Google Scholar] [CrossRef]
- Ferreira, P.H.; Ferreira, M.L.; Maher, C.G.; Refshauge, K.M.; Latimer, J.; Adams, R.D. The Therapeutic Alliance between Clinicians and Patients Predicts Outcome in Chronic Low Back Pain. Phys. Ther. 2013, 93, 470–478. [Google Scholar] [CrossRef]
| Measures | Mean ± SD/Number (%) | Minimum-Maximum |
|---|---|---|
| Age | 56.9 ± 14.08 | 22–80 |
| BMI | 25.67 ± 4.42 | 18.36–41.24 |
| Number of sessions | 10.33 ± 5.33 | 4–35 |
| Sex | ||
| 115 (76.7) | |
| 35 (23.3) | |
| Educational level | ||
| 10 (6.7) | |
| 45 (30) | |
| 95 (63.3) | |
| Employment status | ||
| 72 (48) | |
| 12 (8) | |
| 33 (22) | |
| 33 (22) | |
| Types of treatment | ||
| 22 (14.7) | |
| 28 (18.7) | |
| 46 (30.7) | |
| 29 (19.3) | |
| 25 (16.7) |
| Measures | Mean ± SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2.45 ± 1.33 | 1 | ||||||||||||||
| 10.33 ± 5.33 | 0.45 *** | ||||||||||||||
| 21.64 ± 6.96 | −0.33 *** | −0.171* | |||||||||||||
| 16.21 ± 9.91 | −0.14 | −0.04 | 0.42 *** | ||||||||||||
| 34.76 ± 9.17 | 0.37 *** | 0.15 | −0.08 | −0.11 | |||||||||||
| 13.14 ± 3.85 | 0.42 *** | 0.15 | −0.09 | −0.03 | 0.58 *** | ||||||||||
| 26.64 ± 4.48 | 0.04 | 0.06 | 0.05 | 0.11 | 0.32 *** | 0.27 *** | |||||||||
| 21 ± 4.8 | 0.48 *** | 0.22 ** | −0.11 | −0.01 | 0.41 *** | 0.39 *** | 0.44 *** | ||||||||
| 57.31 ± 13.83 | 0.14 | 0.07 | −0.04 | −0.22 ** | 0.10 | 0.19 * | 0.19 * | 0.03 | |||||||
| 49.19 ± 12.61 | 0.12 | 0.15 | −0.14 | −0.34 *** | 0.01 | 0.12 | 0.04 | −0.01 | 0.70 *** | ||||||
| 32.77 ± 12.64 | 0.39 *** | 0.21 ** | −0.35 *** | −0.37 *** | 0.19 * | 0.21 * | 0.03 | 0.12 | 0.50 *** | 0.55 *** | |||||
| 10.88 ± 3.14 | −0.17 * | −0.09 | 0.13 | 0.38 *** | −0.07 | −0.09 | 0.06 | −0.07 | −0.20 * | −0.30 *** | −0.12 | ||||
| 17.32 ± 5.44 | −0.15 | −0.11 | 0.18 * | 0.51 *** | 0.09 | −0.01 | 0.17 * | −0.02 | −0.25 ** | −0.42 *** | −0.19 * | 0.70 *** | |||
| 5.35 ± 4.21 | −0.24 * | −0.14 | 0.36 *** | 0.47 *** | −0.05 | −0.15 | −0.01 | −0.02 | −0.30 *** | −0.25 ** | −0.37 *** | 0.17 * | 0.30 *** | ||
| 2.97 ± 2.49 | −0.23 ** | −0.12 | 0.25 ** | 0.42 *** | −0.14 | −0.18 * | −0.17 * | −0.09 | −0.41 *** | −0.24 ** | −0.28 *** | 0.29 *** | 0.31 *** | 0.79 *** | |
| 5.83 ± 5.21 | −0.23 ** | −0.09 | 0.30 *** | 0.50 *** | −0.11 | −0.19 * | −0.17 * | −0.10 | −0.37 *** | −0.28 *** | −0.29 *** | 0.34 *** | 0.33 *** | 0.72 *** | 0.78 *** |
| Criteria Variable: GRPC | ||||
|---|---|---|---|---|
| General Model | ||||
| R2 = 0.52; Adjusted R2 = 0.50; F = 26.32; p < 0.01 | ||||
| Predictor Variables | Regression Coefficient (B) | Standardized Coefficient (B) | p Value | VIF |
| AdT-Physio Beliefs about treatment | 0.13 | −0.48 | <0.001 | 1 |
| Number of sessions | 0.09 | 0.35 | <0.001 | 1.05 |
| CPSS_handling the pain | 0.03 | 0.28 | <0.001 | 1.08 |
| CAF-P_bonding | 0.07 | 0.20 | 0.003 | 1.21 |
| AdT-Physio_compliance | −0.06 | −0.21 | 0.001 | 1.26 |
| GCPS_Intensity of pain | −0.03 | −0.18 | 0.006 | 1.19 |
| Excluded variables | ||||
| CAF-P_collaboration | - | 0.11 | 0.14 | 1.66 |
| TSK_fear of physical activity | - | −0.02 | 0.67 | 1.11 |
| TSK_fear of injury | - | −0.03 | 0.53 | 1.05 |
| CPSS_controlling symptoms | - | −0.01 | 0.9 | 1.44 |
| CPSS_physical activities | - | −0.09 | 0.2 | 1.57 |
| PCS_Rumination | - | −0.01 | 0.82 | 1.32 |
| PCS_magnification | - | −0.05 | 0.41 | 1.19 |
| PCS_hopelessness | - | 0.04 | 0.52 | 1.31 |
| GCPS_Disability | - | 0.11 | 0.09 | 1.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Touche, R.; Pardo-Montero, J.; Grande-Alonso, M.; Paris-Alemany, A.; Miñambres-Martín, D.; Nouvilas-Pallejà, E. Psychological, Pain, and Disability Factors Influencing the Perception of Improvement/Recovery from Physiotherapy in Patients with Chronic Musculoskeletal Pain: A Cross-Sectional Study. Healthcare 2024, 12, 12. https://doi.org/10.3390/healthcare12010012
La Touche R, Pardo-Montero J, Grande-Alonso M, Paris-Alemany A, Miñambres-Martín D, Nouvilas-Pallejà E. Psychological, Pain, and Disability Factors Influencing the Perception of Improvement/Recovery from Physiotherapy in Patients with Chronic Musculoskeletal Pain: A Cross-Sectional Study. Healthcare. 2024; 12(1):12. https://doi.org/10.3390/healthcare12010012
Chicago/Turabian StyleLa Touche, Roy, Joaquín Pardo-Montero, Mónica Grande-Alonso, Alba Paris-Alemany, Diego Miñambres-Martín, and Encarnación Nouvilas-Pallejà. 2024. "Psychological, Pain, and Disability Factors Influencing the Perception of Improvement/Recovery from Physiotherapy in Patients with Chronic Musculoskeletal Pain: A Cross-Sectional Study" Healthcare 12, no. 1: 12. https://doi.org/10.3390/healthcare12010012
APA StyleLa Touche, R., Pardo-Montero, J., Grande-Alonso, M., Paris-Alemany, A., Miñambres-Martín, D., & Nouvilas-Pallejà, E. (2024). Psychological, Pain, and Disability Factors Influencing the Perception of Improvement/Recovery from Physiotherapy in Patients with Chronic Musculoskeletal Pain: A Cross-Sectional Study. Healthcare, 12(1), 12. https://doi.org/10.3390/healthcare12010012









