Investigating Students’ Perceptions towards Artificial Intelligence in Medical Education
Abstract
1. Introduction
2. Methods
2.1. Study Design, Population, and Research Setting
2.2. The Survey Questionnaire
2.3. Ethical Consideration
2.4. Construct Validity of the Questionnaire’s Items
2.4.1. Students’ Perceptions Scale (10 Items)
2.4.2. Impact of AI on Medical Education (Five Items)
2.5. Statistical Analysis
3. Results
3.1. Survey Respondents’ Summary
3.2. Descriptive Statistics
3.3. Students’ Perceptions towards AI
3.4. Student’s Perspective on the Impact of AI on Medical Education and Their Willingness to Use It
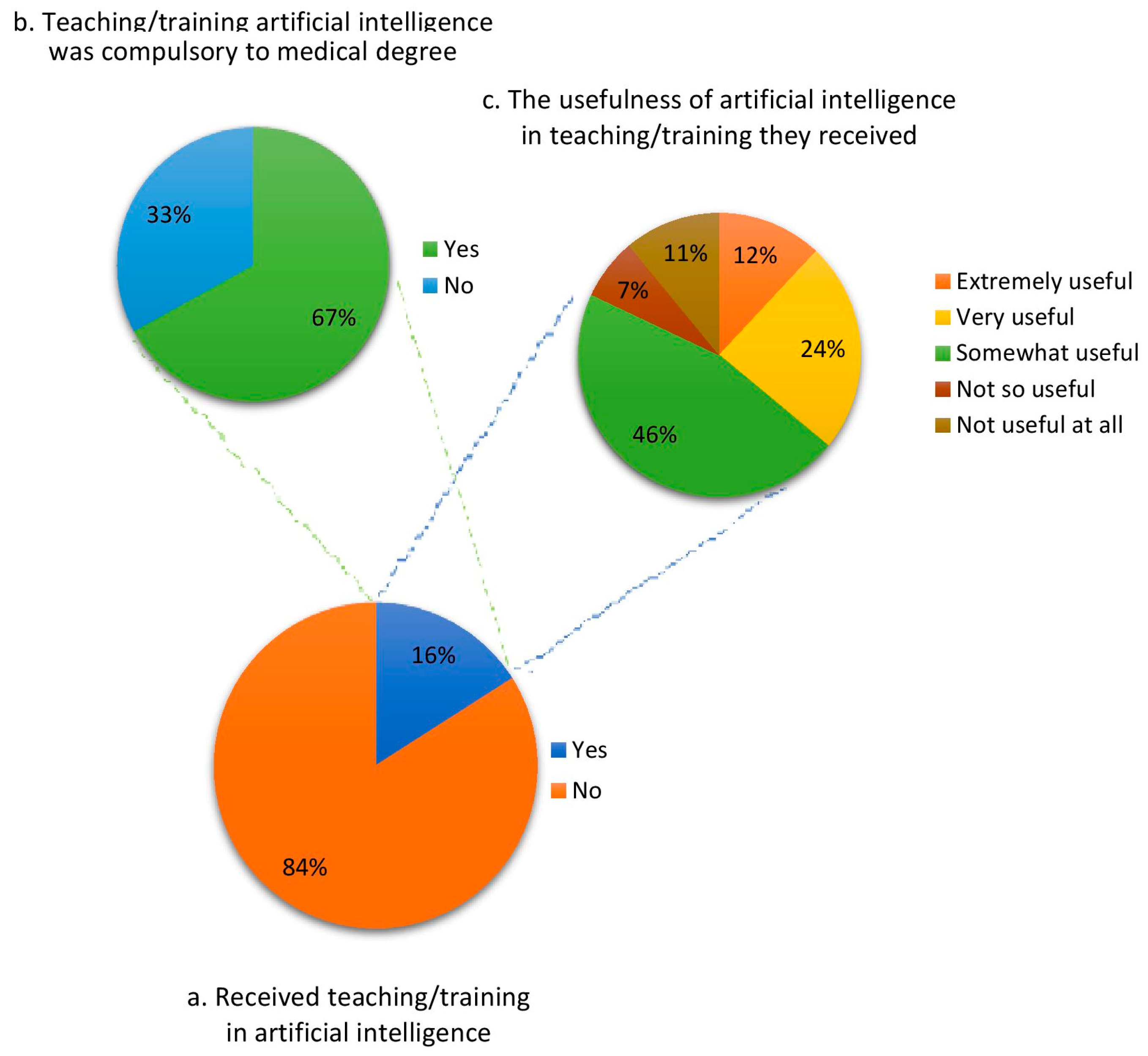
3.5. Students’ Status for Previous Teaching or Training in AI
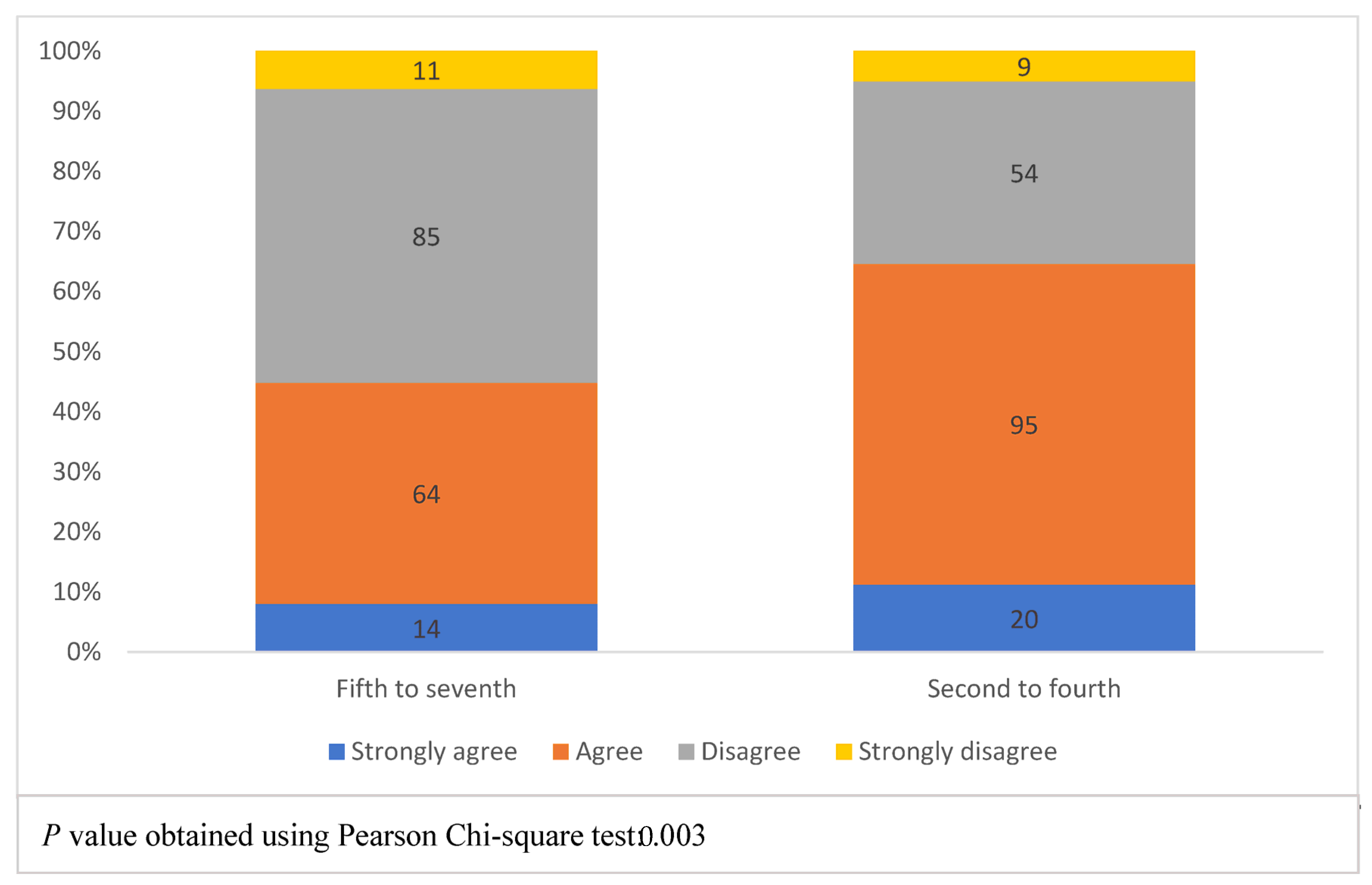
3.6. The Association between Academic Years and the Perceptions towards AI
3.7. The Association between Academic Years and Previous AI Teaching or Training, the Impact of AI on Medical Education and Willingness to Use It
4. Discussion
4.1. Perceptions towards AI among Medical Students
4.2. Teaching or Training in AI among Medical Students
4.3. The Perceived Impact of AI on Medical Education and Willingness to Use It
4.4. Attitudinal Differences among the Students by Academic Phases
4.5. Risks and Ethical/Social Aspects of AI in Healthcare
4.6. The Implications of the Study Findings
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Enholm, I.M.; Papagiannidis, E.; Mikalef, P.; Krogstie, J. Artificial intelligence and business value: A literature review. Inf. Syst. Front. 2022, 24, 1709–1734. [Google Scholar] [CrossRef]
- Elsevier. Description—Artificial Intelligence in Medicine. Available online: https://www.elsevier.com/journals/artificial-intelligence-in-medicine/0933-3657/subscribe (accessed on 25 June 2022).
- Malik, P.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. J. Fam. Med. Prim. Care 2019, 8, 2328. [Google Scholar]
- Pinto dos Santos, D.; Giese, D.; Brodehl, S.; Chon, S.-H.; Staab, W.; Kleinert, R.; Maintz, D.; Baeßler, B. Medical students’ attitude towards artificial intelligence: A multicentre survey. Eur. Radiol. 2019, 29, 1640–1646. [Google Scholar] [CrossRef] [PubMed]
- Sit, C.; Srinivasan, R.; Amlani, A.; Muthuswamy, K.; Azam, A.; Monzon, L.; Poon, D.S. Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: A multicentre survey. Insights Imaging 2020, 11, 14. [Google Scholar] [CrossRef] [PubMed]
- Noguerol, T.M.; Paulano-Godino, F.; Martín-Valdivia, M.T.; Menias, C.O.; Luna, A. Strengths, weaknesses, opportunities, and threats analysis of artificial intelligence and machine learning applications in radiology. J. Am. Coll. Radiol. 2019, 16, 1239–1247. [Google Scholar] [CrossRef]
- Moxley-Wyles, B.; Colling, R.; Verrill, C. Artificial intelligence in pathology: An overview. Diagn. Histopathol. 2020, 26, 513–520. [Google Scholar] [CrossRef]
- Benjamins, J.W.; Hendriks, T.; Knuuti, J.; Juarez-Orozco, L.E.; van der Harst, P. A primer in artificial intelligence in cardiovascular medicine. Neth. Heart J. 2019, 27, 392–402. [Google Scholar] [CrossRef]
- Ting, D.S.W.; Pasquale, L.R.; Peng, L.; Campbell, J.P.; Lee, A.Y.; Raman, R.; Tan, G.S.W.; Schmetterer, L.; Keane, P.A.; Wong, T.Y. Artificial intelligence and deep learning in ophthalmology. Br. J. Ophthalmol. 2019, 103, 167–175. [Google Scholar] [CrossRef]
- Polesie, S.; Gillstedt, M.; Kittler, H.; Lallas, A.; Tschandl, P.; Zalaudek, I.; Paoli, J. Attitudes towards artificial intelligence within dermatology: An international online survey. Br. J. Dermatol. 2020, 183, 159–161. [Google Scholar] [CrossRef]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Future Healthc. J. 2019, 6, 94. [Google Scholar] [CrossRef]
- Rebala, G.; Ravi, A.; Churiwala, S. An Introduction to Machine Learning; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Wang, C.-N.; Yang, F.-C.; Nguyen, V.T.T.; Nguyen, Q.M.; Huynh, N.T.; Huynh, T.T. Optimal design for compliant mechanism flexure hinges: Bridge-type. Micromachines 2021, 12, 1304. [Google Scholar] [CrossRef]
- Wang, C.-N.; Yang, F.-C.; Nguyen, V.T.T.; Vo, N.T. CFD analysis and optimum design for a centrifugal pump using an effectively artificial intelligent algorithm. Micromachines 2022, 13, 1208. [Google Scholar] [CrossRef] [PubMed]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine learning in medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef]
- Singhal, K.; Azizi, S.; Tu, T.; Mahdavi, S.S.; Wei, J.; Chung, H.W.; Scales, N.; Tanwani, A.; Cole-Lewis, H.; Pfohl, S. Large Language Models Encode Clinical Knowledge. arXiv 2022, arXiv:2212.13138. [Google Scholar]
- Lee, P.; Bubeck, S.; Petro, J. Benefits, Limits, and Risks of GPT-4 as an AI Chatbot for Medicine. N. Engl. J. Med. 2023, 388, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. The utility of ChatGPT as an example of large language models in healthcare education, research and practice: Systematic review on the future perspectives and potential limitations. medRxiv 2023. [Google Scholar] [CrossRef]
- Karaca, O.; Çalışkan, S.A.; Demir, K. Medical artificial intelligence readiness scale for medical students (MAIRS-MS)–development, validity and reliability study. BMC Med. Educ. 2021, 21, 112. [Google Scholar] [CrossRef]
- Oh, S.; Kim, J.H.; Choi, S.-W.; Lee, H.J.; Hong, J.; Kwon, S.H. Physician confidence in artificial intelligence: An online mobile survey. J. Med. Internet Res. 2019, 21, e12422. [Google Scholar] [CrossRef] [PubMed]
- van Hoek, J.; Huber, A.; Leichtle, A.; Härmä, K.; Hilt, D.; von Tengg-Kobligk, H.; Heverhagen, J.; Poellinger, A. A survey on the future of radiology among radiologists, medical students and surgeons: Students and surgeons tend to be more skeptical about artificial intelligence and radiologists may fear that other disciplines take over. Eur. J. Radiol. 2019, 121, 108742. [Google Scholar] [CrossRef] [PubMed]
- Edward, H.; Shortliffe, J.J.C.; Chiang, M.F. Biomedical Informatics: Computer Applications in Health Care and Biomedicine, 5th ed.; Springer Nature: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Wartman, S.A.; Combs, C.D. Medical education must move from the information age to the age of artificial intelligence. Acad. Med. 2018, 93, 1107–1109. [Google Scholar] [CrossRef]
- Paranjape, K.; Schinkel, M.; Panday, R.N.; Car, J.; Nanayakkara, P. Introducing artificial intelligence training in medical education. JMIR Med. Educ. 2019, 5, e16048. [Google Scholar] [CrossRef]
- The Association of American Medical Colleges. Effective Use of Educational Technology in Medical Education; The AAMC’s Institute for Improving Medical Education: Washington, DC, USA, 2007. [Google Scholar]
- Lee, J.; Wu, A.S.; Li, D.; Kulasegaram, K.M. Artificial intelligence in undergraduate medical education: A scoping review. Acad. Med. 2021, 96, S62–S70. [Google Scholar] [CrossRef]
- Al Saad, M.M.; Shehadeh, A.; Alanazi, S.; Alenezi, M.; Eid, H.; Alfaouri, M.S.; Aldawsari, S.; Alenezi, R. Medical students’ knowledge and attitude towards artificial intelligence: An online survey. Open Public Health J. 2022, 15, e187494452203290. [Google Scholar] [CrossRef]
- Almaiah, M.A.; Alfaisal, R.; Salloum, S.A.; Hajjej, F.; Thabit, S.; El-Qirem, F.A.; Lutfi, A.; Alrawad, M.; Al Mulhem, A.; Alkhdour, T. Examining the impact of artificial intelligence and social and computer anxiety in e-learning settings: Students’ perceptions at the university level. Electronics 2022, 11, 3662. [Google Scholar] [CrossRef]
- Aljohani, R.A. Teachers and students’ perceptions on the impact of artificial intelligence on English language learning in Saudi Arabia. J. Appl. Linguist. Lang. Res. 2021, 8, 36–47. [Google Scholar]
- Alzahrani, A. A systematic review of artificial intelligence in education in the arab world. Amazon. Investig. 2022, 11, 293–305. [Google Scholar] [CrossRef]
- Holder, C.; Khurana, V.; Watts, M. Artificial Intelligence: Public Perception, Attitude and Trust; Censuswide: London, UK, 2018. [Google Scholar]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar]
- IBM. IBM SPSS Statistics. Available online: https://www.ibm.com/products/spss-statistics (accessed on 11 January 2023).
- Wallis, C. How artificial intelligence will change medicine. Nature 2019, 576, S48. [Google Scholar] [CrossRef]
- Park, C.J.; Paul, H.Y.; Siegel, E.L. Medical student perspectives on the impact of artificial intelligence on the practice of medicine. Curr. Probl. Diagn. Radiol. 2021, 50, 614–619. [Google Scholar] [CrossRef]
- Park, S.H.; Do, K.-H.; Kim, S.; Park, J.H.; Lim, Y.-S. What should medical students know about artificial intelligence in medicine? J. Educ. Eval. Health Prof. 2019, 16, 18. [Google Scholar] [CrossRef]
- Sanal, M.G.; Paul, K.; Kumar, S.; Ganguly, N.K. Artificial Intelligence and Deep Learning: The Future of Medicine and Medical Practice. J. Assoc. Physicians India 2019, 67, 71–73. [Google Scholar] [PubMed]
- Krittanawong, C. The rise of artificial intelligence and the uncertain future for physicians. Eur. J. Intern. Med. 2018, 48, e13–e14. [Google Scholar] [CrossRef] [PubMed]
- Shuaib, A.; Arian, H.; Shuaib, A. The Increasing Role of Artificial Intelligence in Health Care: Will Robots Replace Doctors in the Future? Int. J. Gen. Med. 2020, 13, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Gong, B.; Nugent, J.P.; Guest, W.; Parker, W.; Chang, P.J.; Khosa, F.; Nicolaou, S. Influence of artificial intelligence on Canadian medical students’ preference for radiology specialty: ANational survey study. Acad. Radiol. 2019, 26, 566–577. [Google Scholar] [CrossRef] [PubMed]
- Masters, K. Artificial intelligence in medical education. Med. Teach. 2019, 41, 976–980. [Google Scholar] [CrossRef]
- Goodman, K.; Zandi, D.; Reis, A.; Vayena, E. Balancing risks and benefits of artificial intelligence in the health sector. Bull. World Health Organ. 2020, 98, 230. [Google Scholar] [CrossRef]
- Civaner, M.M.; Uncu, Y.; Bulut, F.; Chalil, E.G.; Tatli, A. Artificial intelligence in medical education: A cross-sectional needs assessment. BMC Med. Educ. 2022, 22, 772. [Google Scholar] [CrossRef]
- EPRS. Artificial Intelligence in Healthcare: Applications, Risks, and Ethical and Societal Impacts; Scientific Foresight Unit, European Parliamentary Research Service, European Parliament: European Union, 2022. [Google Scholar]
- Sunarti, S.; Rahman, F.F.; Naufal, M.; Risky, M.; Febriyanto, K.; Masnina, R. Artificial intelligence in healthcare: Opportunities and risk for future. Gac. Sanit. 2021, 35, S67–S70. [Google Scholar] [CrossRef] [PubMed]
- Bichel-Findlay, J.; Koch, S.; Mantas, J.; Abdul, S.S.; Al-Shorbaji, N.; Ammenwerth, E.; Baum, A.; Borycki, E.M.; Demiris, G.; Hasman, A. Recommendations of the International Medical Informatics Association (IMIA) on Education in Biomedical and Health Informatics: Second Revision. Int. J. Med. Inform. 2023, 170, 104908. [Google Scholar] [CrossRef]


| Items | Common Factor = 32.76% of Variance Loading |
|---|---|
| 1. Artificial intelligence (AI) will play an important role in health care | 0.482 |
| 2. AI will replace some specialties in healthcare during my lifetime | 0.255 |
| 3. I understand basic AI principles | 0.699 |
| 4. I am comfort with AI terminologies | 0.670 |
| 5. I understand AI limitations | 0.437 |
| 6. AI teaching will benefit my career | 0.525 |
| 7. All medical students should receive AI teaching | 0.472 |
| 8. I will be confident using AI tools at the end of my medical degree | 0.691 |
| 9. I will have better understanding of the methods used to assess healthcare AI performance at the end of my medical degree | 0.701 |
| 10. I will possess the knowledge needed to work with AI in routine clinical practice at the end of my medical degree | 0.619 |
| Eigen Value = 3.276 |
| Item No. | Common Factor = 46.64% of Variance Loading |
|---|---|
| 1. AI systems would have a positive impact on medical education | 0.811 |
| 2. Incorporating AI systems in medical education would ease your learning process | 0.810 |
| 3. Use AI systems in medical education would prepare you for real clinical practice | 0.750 |
| 4. Use AI systems in medical practice would replace your future role as a physician | 0.176 |
| 5. The willingness of using AI in medical education system | 0.651 |
| Eigen Value= 2.332 |
| Characteristic | n (%) |
|---|---|
| Age (in years) | |
| Mean ± SD | 22.1 ± 1.8 |
| Gender | |
| Male | 39 (11.1) |
| Female | 313 (88.9) |
| Current academic study year | |
| Second to fourth (Phase II) | 178 (50.6) |
| Fifth to seventh (Phase III) | 174 (49.4) |
| Computer literacy level | |
| Literate | 66 (18.8) |
| Competent | 265 (75.3) |
| Proficient | 21 (5.9) |
| Usage of computer technology for learning | |
| Always | 206 (58.5) |
| Sometimes | 135 (38.4) |
| Never | 11 (3.1) |
| Statement | Strongly Agree n (%) | Agree n (%) | Disagree n (%) | Strongly Disagree n (%) |
|---|---|---|---|---|
| AI will play important role in healthcare | 199 (56.5) | 150 (42.6) | 2 (0.6) | 1 (0.3) |
| AI will replace some specialties in healthcare during my lifetime | 63 (17.9) | 177 (50.3) | 100 (28.4) | 12 (3.4) |
| I understand basic AI principles | 24 (6.8) | 189 (53.7) | 124 (35.2) | 15 (4.3) |
| I am comfortable with AI terminologies | 105 (29.8) | 224 (63.6) | 22 (6.3) | 1 (0.3) |
| I understand AI limitations | 38 (10.8) | 200 (56.8) | 105 (29.8) | 9 (2.6) |
| AI teaching will benefit my career | 105 (29.8) | 224 (63.6) | 22 (6.3) | 1 (0.3) |
| All medical students should receive AI teaching | 111 (31.5) | 178 (50.6) | 63 (17.9) | 0 |
| I will be confident using AI tools at the end of my medical degree | 52 (14.8) | 156 (44.3) | 129 (36.6) | 15 (4.3) |
| I will have better understanding of the methods used to assess healthcare AI performance at the end of my medical degree | 34 (9.7) | 159 (45.2) | 139 (39.5) | 20 (5.7) |
| I will possess the knowledge needed to work with AI in routine clinical practice at the end of my medical degree | 28 (8) | 179 (50.9) | 129 (36.6) | 16 (4.5) |
| Statement | Strongly Agree n (%) | Agree n (%) | Disagree n (%) | Strongly Disagree n (%) |
|---|---|---|---|---|
| AI systems will have a positive impact on medical education | 107 (30.4) | 233 (66.2) | 12 (3.4) | 0 |
| Incorporating AI in medical education would ease the learning process | 122 (34.7) | 203 (57.7) | 23 (6.5) | 4 (1.1) |
| Using AI in medical education will prepare me for real clinical practice | 94 (26.7) | 182 (51.7) | 70 (19.9) | 6 (1.7) |
| AI will replace my future role as a physician | 17 (4.8) | 58 (16.5) | 177 (50.3) | 100 (28.4) |
| Very willing n (%) | Willing n (%) | Not willing n (%) | Not at all willing n (%) | |
| Willingness to use AI in medical education | 120 (34.1) | 202 (57.4) | 27 (7.7) | 3 (0.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buabbas, A.J.; Miskin, B.; Alnaqi, A.A.; Ayed, A.K.; Shehab, A.A.; Syed-Abdul, S.; Uddin, M. Investigating Students’ Perceptions towards Artificial Intelligence in Medical Education. Healthcare 2023, 11, 1298. https://doi.org/10.3390/healthcare11091298
Buabbas AJ, Miskin B, Alnaqi AA, Ayed AK, Shehab AA, Syed-Abdul S, Uddin M. Investigating Students’ Perceptions towards Artificial Intelligence in Medical Education. Healthcare. 2023; 11(9):1298. https://doi.org/10.3390/healthcare11091298
Chicago/Turabian StyleBuabbas, Ali Jasem, Brouj Miskin, Amar Ali Alnaqi, Adel K. Ayed, Abrar Abdulmohsen Shehab, Shabbir Syed-Abdul, and Mohy Uddin. 2023. "Investigating Students’ Perceptions towards Artificial Intelligence in Medical Education" Healthcare 11, no. 9: 1298. https://doi.org/10.3390/healthcare11091298
APA StyleBuabbas, A. J., Miskin, B., Alnaqi, A. A., Ayed, A. K., Shehab, A. A., Syed-Abdul, S., & Uddin, M. (2023). Investigating Students’ Perceptions towards Artificial Intelligence in Medical Education. Healthcare, 11(9), 1298. https://doi.org/10.3390/healthcare11091298






